Abstract
Cervical artery dissection is an uncommon condition for which pregnancy and postpartum states confer increased risk. Although the majority of patients with this condition fully recover, including resolution of the dissection on imaging, long-term sequelae include a variety of cardiovascular conditions that may be associated with high rates of morbidity and mortality. Here, we review 2 cases of vertebral artery dissection in relation to pregnancy. Our first case will review the management of a pregnant patient with a history of vertebral artery dissection; whereas our second case reviews a presentation of postpartum vertebral artery dissection. Providers should maintain a high suspicion of cervical artery dissection in pregnant and postpartum patients presenting with headache and neck pain.
Key words: cervical artery dissection and pregnancy, complications of preeclampsia, postpartum cervical artery dissection, postpartum vertebral artery dissection, vascular events in pregnancy, vertebral artery dissection and pregnancy
Introduction
Cervical artery dissection is an uncommon phenomenon; although the exact incidence has not been determined, it is estimated to be 2.6 to 5 per 100,000 patients per year.1, 2, 3 A retrospective review of electronic medical record data found that pregnancy is associated with a 2-fold increased incidence rate ratio (IRR) of cervical artery dissection, with the postpartum period accounting for a 5.5 IRR.4 In this study, 45% of patients with postpartum cervical artery dissection had a hypertensive disorder.4 Cervical artery dissection is more common in men; however, women of reproductive-age experience a higher incidence than men of the same age.5 Given this increased incidence in women of reproductive-age, 29 cases reports of cervical artery dissection in relation to pregnancy and postpartum have been described.6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22
To date, no reported cases of viable intrauterine pregnancy diagnosed within 6 months of a primary cervical artery dissection have been described. Herein, we report our management of a pregnancy starting 4 months after primary cervical artery dissection and a case of a vertebral artery dissection initially presumed to be postpartum preeclampsia with severe features.
Cases
Case 1
A 30-year-old gravida-3-para-0020 initiated her prenatal care in the first trimester with a past medical history notable for left vertebral artery dissection. Her past medical and surgical history were otherwise uncomplicated. The vertebral artery dissection was diagnosed following presentation for 1 day of neurologic symptoms, including bifrontal headache, scintillating scotoma of the left eye, and transient numbness of her left face and hand. She reported that 3 weeks earlier, while lifting weights, she experienced an immediate onset of severe posterior neck pain lasting 3 to 5 days. She subsequently underwent chiropractic manipulation for neck pain and stated that the neck pain initially resolved and denied additional neurologic symptoms. Evaluation during her presentation to the emergency department included a head and neck computer tomography angiography (CTA) that demonstrated a 6 mm filling defect in the distal V2 representing a vertebral artery dissection. Further imaging with brain magnetic resonance imaging demonstrated no evidence of ischemia. She was followed-up with in the outpatient setting by neurology and 2 months later, repeat head and neck CTA demonstrated improved patency with minimal narrowing of the affected segment of the left vertebral artery with no evidence of pseudoaneurysm.
The patient subsequently presented at 11 weeks gestation for initial prenatal management and was started on daily low-dose aspirin given her history of vertebral artery dissection. She received a neurology consultation at 24 weeks gestation. A repeat head and neck CTA was pursued that demonstrated improved findings of the left vertebral artery at the V2 segment with no significant stenosis. Given these imaging findings, the clinical consensus was that the patient was at a low cerebrovascular risk with vaginal delivery and was neurologically cleared to valsalva, as would be required during the second stage of labor.
At 41 weeks gestation, the patient was admitted to labor and delivery for augmentation in the setting of prelabor rupture of membranes, with anticipation of a vaginal delivery. Cesarean delivery would be considered for routine obstetrical indications or should clinical suspicion of redissection arise.
The patient reached the second stage of labor with intravenous oxytocin. After 45 minutes of pushing, the fetus had a category II fetal heart rate tracing characterized by variable decelerations and reflex fetal tachycardia. Repeat cervical examination demonstrated an asynclitic and occiput-posterior presentation at +1 station despite excellent maternal efforts. Given fetal position and the persistent category II fetal heart tracing, the recommendation was made to proceed to cesarean delivery. The cesarean delivery and patient's postpartum course were uncomplicated with no signs or symptoms of cerebrovascular events and the patient was discharged to home on postoperative day 2. The patient was seen and evaluated for her 6-week postpartum appointment then seen 4 months postpartum for a well woman examination. During this time, she denied any recurrence of pain and neurologic symptoms.
Case 2
A 35-year-old gravida-3 para-3 presented to labor and delivery triage 11 days postoperatively following a repeat low transverse cesarean delivery at an outside facility. On presentation, she reported a headache for 3 days prior and had not resolved with ibuprofen or acetaminophen, in addition to right sided neck pain and shortness of breath. Vital signs were significant for systolic blood pressures in the 180’s with diastolic pressures in the 100’s. She was treated with 10 mg of oral nifedipine and started on magnesium sulfate for seizure prophylaxis in the setting of presumed postpartum preeclampsia with severe features. Following a standard course of magnesium sulfate therapy, she reported her headache persisted. Consultation with a certified registered nurse anesthetist was obtained and the headache was determined to be unlikely due to previous spinal catheter placement. Laboratory values had remained within normal limits on a complete blood count and comprehensive metabolic panel.
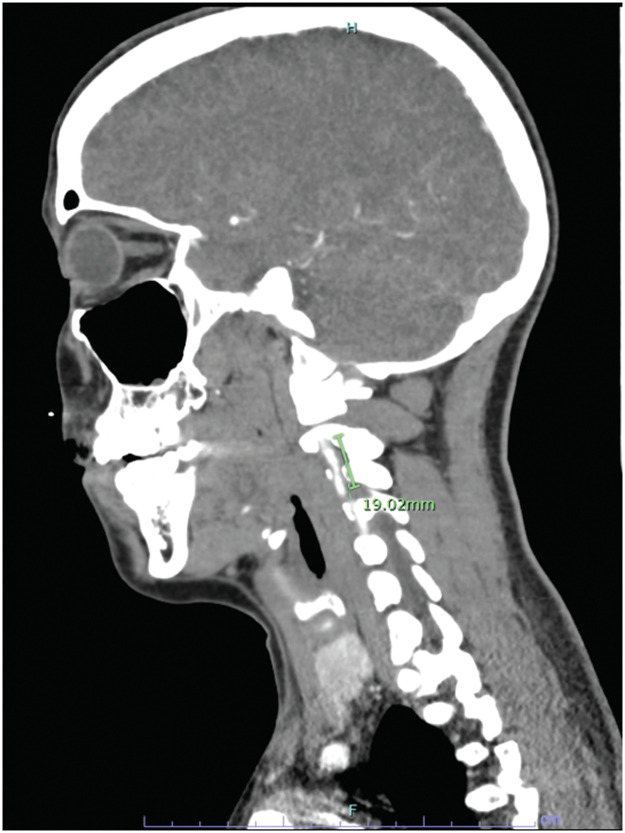
On hospital day 4, she was started on 30 mg of nifedipine daily owing to persistently elevated blood pressures. Notably, her headache remained unresolved, with transient relief secondary to cyclobenzaprine. The persistence of the headache prompted imaging with CTA of the head and neck. Imaging revealed bilateral vertebral artery dissections with the right defect measuring 2 cm and the left measuring 1 to 2 mm (Figure 1). Further history revealed that the patient had received chiropractic manipulation for her ongoing headache in the postpartum period before her presentation and hospitalization. Vascular surgery consultation was obtained, in conjunction with neurosurgery at an outside facility. The neurosurgeon consulted recommended against patient transfer for intervention because there was no evidence of stroke. Magnetic resonance imaging was obtained which revealed no intracranial process. The patient was ultimately discharged home on hospital day 6 with hard copies of her medical imaging and recommendation for continued treatment with 325 mg aspirin daily and repeat imaging and neurology follow-up in 2 to 3 months.
Figure.
Computed tomography demonstrating dissection of the distal portion of the V2 segment of the vertebral artery
Rosalik. Vertebral artery dissection and pregnancy. Am J Obstet Gynecol Glob Rep 2023.
The patient moved and was subsequently remote from our facility. She presented to the emergency room approximately 6 weeks following discharge with similar symptoms of headache and neck pain. Because she had no signs of stroke on examination, she was discharged from the emergency room. Repeat magnetic resonance imaging was then performed outpatient 2 weeks later and demonstrated resolution of the dissections.
Comments
To the best of our knowledge, 29 cases of pregnancy and postpartum associated cervical artery dissection have been described as demonstrated in Table.6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22 Within these cases, 23 cases of postpartum cervical artery dissection have been described, with only 1 of these patients not describing headache or neck pain.6, 7, 8, 9, 10, 11,13,17, 18, 19, 20, 21, 22 Antepartum cases ranged in gestational age, from first trimester to term, including 1 patient whose symptoms began intrapartum, though no consistent symptomatology was present in these patients.10,12,14,16,19
Table.
Case reports of peripartum cervical artery disease
| Study ID, Case# | Maternal age | Timing | Hypertension | Comorbidities | Headache | Neck Pain | Diagnosis, outcome |
|---|---|---|---|---|---|---|---|
| Kelly et al,7 2014, 1 | 39 | Postpartum, 11 d | Absent | None | Present | Present | ICAD and VAD, recovery |
| Kelly et al,7 2014, 2 | 29 | Postpartum, 53 d | Present | Migraines | Present | Present | ICAD and VAD, recovery |
| Kelly et al,7 2014, 3 | 32 | Postpartum, 0 d | Absent | Migraines | Present | Present | ICAD and stroke, residual weakness |
| Kelly et al,7 2014, 4 | 39 | Postpartum, 24 d | Present | Hypertension, hyperlipidemia | Present | Present | VAD, recovery |
| Kelly et al,7 2014, 5 | 28 | Postpartum, 4 d | Present | None | Present | Present | ICAD and subarachnoid hemorrhage, recovery |
| Finley et al,8 2015 | 35 | Postpartum, 3 wk | Present | Migraines, smoking history | Present | Not specified | VAD, stroke, minor deficits |
| Drazin et al,20 2012 | 37 | Postpartum, 1 h | Present | Migraine | Present | Present | VAD, recovery |
| Shanmugalingam et al,10 2016 | 32 | Intrapartum, delivery 2/2 eclampsia | Present | Undiagnosed SLE | Present | Present | VAD, recovery |
| Shanmugalingam et al,10 2016 | 33 | Antepartum, admit for preeclampsia | Present | None | Present | Present | VAD, recovery |
| Shanmugalingam et al,10 2016 | 30 | Postpartum, 6 d | Present | Obesity | Present | Not specified | VAD, recovery |
| Shanmugalingam et al,10 2016 | 30 | Postpartum, <24 h | Present | None | Not specified | Present | Vertebral thrombus, recovery |
| Brantley et al,11 2012 | 32 | Postpartum, 13 d | Present | Thyroid cancer | Not specified | Present | VAD, dissecting to left anterior descending coronary artery, CABG, recovery |
| Cenkowski et al,17 2012 | 35 | Postpartum, 8 mo | Absent | CAD one month before | Not specified | Not specified | VAD, recovery |
| Manasewitsch et al,9 2020 | 31 | Postpartum, 10 d | Present | Smoking | Present | Not specified | VAD, stroke, recovery |
| Arnold et al,18 2008, 1 | 41 | Postpartum, 18 d | Not specified | Migraine | Present | Present | VAD, TIA |
| Arnold et al,18 2008, 2 | 35 | Postpartum, 5 d | Present | Migraines, smoking | Present | Not specified | ICAD, VAD, stroke |
| Arnold et al,18 2008, 3 | 38 | Postpartum, 8 d | Present | Migraines | Present | Not specified | ICAD, SAH |
| Arnold et al,18 2008, 4 | 27 | Postpartum, 11 d | Not specified | Migraines | Present | Present | VAD, RPLS |
| Arnold et al,18 2008, 5 | 38 | Postpartum, 7 d | Present | Migraines | Present | Not specified | VAD, SAH, RPLS |
| Arnold et al,18 2008, 6 | 34 | Postpartum, 7 d | Not specified | Chiropractic manipulation | Preset | Present | VAD |
| Nishimura et al,21 2015 | 35 | Postpartum, 5 d | Present | None | Present | Present | VAD, seizure, recovery |
| Tuluc et al,16 2006 | 39 | Antepartum, unresponsive | Unknown, presumed | None | Present | Not specified | VAD, SAH, death |
| McKinney et al,6 2010 | 41 | Postpartum, 5 d | present | None | Present | Not specified | Basilar artery dissection, seizure, significant motor and neurologic deficit |
| Morton,14 2012 | 31 | Antepartum, 16 wk | Present | SLE, chiropractic manipulation | Not specified | Present | ICAD, persistent Horner syndrome |
| Mas et al,19 1987, 1 | 32 | Antepartum | Present | None | Present | Present | VAD, Wallenberg syndrome, recovery |
| Mas et al,19 1987, 2 | 27 | Postpartum, 2 wk | Not specified | Chiropractic manipulation | Not specified | Present | VAD, TIA, recovery |
| Baffour et al,13 2012 | 34 | Postpartum, 14 d | Present | None | Present | Present | ICAD, stroke, recovery |
| Mohammed et al,12 2014 | 31 | Antepartum, 11 wk | Not specified | None | Present | Present | ICAD, persistent Horner syndrome |
| Borelli et al,22 2012 | 32 | Postpartum, 10 d | Present | HELLP | Present | Not specified | VAD, stroke |
CABG, coronary artery bypass graft surgery; CAD, coronary artery disease; HELLP, hemolysis, elevated liver enzymes, low platelets; ICAD, internal carotid artery dissection; RPLS, reversible posterior leukoencephalopathy syndrome; SAH, subarachnoid hemorrhage; SLE, systemic lupus erythematosus; TIA, transient ischemic attack; VAD, vertebral artery dissection.
Rosalik. Vertebral artery dissection and pregnancy. Am J Obstet Gynecol Glob Rep 2023.
Our second case strengthens the breadth of reports detailing postpartum cervical artery dissection's association with hypertensive disorders in pregnancy, their presentation with headache and neck pain, and the management of these events following the event and in subsequent pregnancies. As with 16 of the cases reported in the Table, both of our patients demonstrated resolution of symptoms following aspirin therapy, and resolution of dissection was demonstrated on follow-up imaging.
Recommendations for treatment of cervical artery dissection remain unclear and largely up to provider discretion. The Cervical Artery Dissection in Stroke Study provided the first randomized control trial examining the impact of treatment of cervical artery dissection to prevent stroke and decrease the risk of recurrent stroke. This study found no difference in outcome, including recurrent stroke and residual artery occlusion in the treatment of cervical artery dissection with antiplatelet or anticoagulation, though there was 1 instance of anticoagulation therapy leading to subarachnoid hemorrhage.23 Our patients were treated with antiplatelet therapy, a therapeutic choice which may be a more appropriate for those without neurologic symptoms. In subsequent pregnancies, recommendations include counseling for risk of stroke, and use of aspirin to reduce the risk of preeclampsia in future pregnancies.7,10
Overall, cervical artery dissection is a rare cardiovascular event for which pregnancy and hypertensive states confer increased risks. Imaging of the head and neck should be considered for patients who present with symptoms associated with cervical artery dissection during pregnancy or in the immediate postpartum period. Although this condition is relatively rare, and the majority of patients recover fully, failure to recognize the etiology and delay in diagnosis could lead to severe morbidity and mortality, and care should be taken in future pregnancies to minimize risk of recurrence.
Footnotes
The authors report no conflict of interest.
Written and verbal consent was provided by both patients included in this article.
Patient cases were previously presented at the 2022 annual meeting of the American College of Obstetricians and Gynecologists Armed Forces District, Las Vegas, NV, October 17, 2022.
The views expressed herein are those of the authors and do not reflect the official policy of the Department of the Army, Department of Defense, or US Government.
References
- 1.Schievink W, Roiter V. Epidemiology of cervical artery dissection. Front Neurol Neurosci. 2005;20:12–15. doi: 10.1159/000088125. [DOI] [PubMed] [Google Scholar]
- 2.Béjot Y, Daubail B, Debette S, Durier J, Giroud M. Incidence and outcome of cerebrovascular events related to cervical artery dissection: the Dijon Stroke Registry. Int J Stroke. 2014;9:879–882. doi: 10.1111/ijs.12154. [DOI] [PubMed] [Google Scholar]
- 3.Lee VH, Brown RD, Jr, Mandrekar JN, Mokri B. Incidence and outcome of cervical artery dissection: a population-based study. Neurology. 2006;67:1809–1812. doi: 10.1212/01.wnl.0000244486.30455.71. [DOI] [PubMed] [Google Scholar]
- 4.Salehi Omran S, Parikh NS, Poisson S, et al. Association between pregnancy and cervical artery dissection. Ann Neurol. 2020;88:596–602. doi: 10.1002/ana.25813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Metso AJ, Metso TM, Debette S, et al. Gender and cervical artery dissection. Eur J Neurol. 2012;19:594–602. doi: 10.1111/j.1468-1331.2011.03586.x. [DOI] [PubMed] [Google Scholar]
- 6.McKinney JS, Messé SR, Pukenas BA, et al. Intracranial vertebrobasilar artery dissection associated with postpartum angiopathy. Stroke Res Treat. 2010;2010 doi: 10.4061/2010/320627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelly JC, Safain MG, Roguski M, Edlow AG, Malek AM. Postpartum internal carotid and vertebral arterial dissections. Obstet Gynecol. 2014;123:848–856. doi: 10.1097/AOG.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 8.Finley A, Rogers B, Richards T, Jr, Vogel H. Postpartum vertebral artery dissection. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-211872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manasewitsch NT, Hanfy AA, Beutler BD, et al. Postpartum vertebral artery dissection: case report and review of the literature. Thromb J. 2020;18:30. doi: 10.1186/s12959-020-00243-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shanmugalingam R, Reza Pour N, Chuah SC, et al. Vertebral artery dissection in hypertensive disorders of pregnancy: a case series and literature review. BMC Pregnancy Childbirth. 2016;16:164. doi: 10.1186/s12884-016-0953-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brantley HP, Cabarrus BR, Movahed A. Spontaneous multiarterial dissection immediately after childbirth. Tex Heart Inst J. 2012;39:683–686. [PMC free article] [PubMed] [Google Scholar]
- 12.Mohammed I, Aaland M, Khan N, Crossley I. A young pregnant woman with spontaneous carotid artery dissection–unknown mechanisms. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2013-202541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baffour FI, Kirchoff-Torres KF, Einstein FH, Karakash S, Miller TS. Bilateral internal carotid artery dissection in the postpartum period. Obstet Gynecol. 2012;119:489–492. doi: 10.1097/AOG.0b013e318242d8d4. [DOI] [PubMed] [Google Scholar]
- 14.Morton A. Internal carotid artery dissection following chiropractic treatment in a pregnant woman with systemic lupus erythematosus. Chiropr Man Therap. 2012;20:38. doi: 10.1186/2045-709X-20-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mass SB, Cardonick E, Haas S, Gopalani S, Leuzzi RA. Bilateral vertebral artery dissection causing a cerebrovascular accident in pregnancy. A case report. J Reprod Med. 1999;44:887–890. [PubMed] [Google Scholar]
- 16.Tuluc M, Brown D, Goldman B. Lethal vertebral artery dissection in pregnancy: a case report and review of the literature. Arch Pathol Lab Med. 2006;130:533–535. doi: 10.5858/2006-130-533-LVADIP. [DOI] [PubMed] [Google Scholar]
- 17.Cenkowski M, daSilva M, Bordun KA, Hussain F, Kirkpatrick ID, Jassal DS. Spontaneous dissection of the coronary and vertebral arteries post-partum: case report and review of the literature. BMC Pregnancy Childbirth. 2012;12:122. doi: 10.1186/1471-2393-12-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arnold M, Camus-Jacqmin M, Stapf C, et al. Postpartum cervicocephalic artery dissection. Stroke. 2008;39:2377–2379. doi: 10.1161/STROKEAHA.107.510107. [DOI] [PubMed] [Google Scholar]
- 19.Mas JL, Bousser MG, Hasboun D, Laplane D. Extracranial vertebral artery dissections: a review of 13 cases. Stroke. 1987;18:1037–1047. doi: 10.1161/01.str.18.6.1037. [DOI] [PubMed] [Google Scholar]
- 20.Drazin D, Rosner J, Shirzadi A, Phuphanich S. Postpartum extracranial bilateral vertebral artery dissection mimicking subarachnoid hemorrhage. Neurologist. 2012;18:149–151. doi: 10.1097/NRL.0b013e318247bb59. [DOI] [PubMed] [Google Scholar]
- 21.Nishimura M, Hiraoka E, Kanazawa K, Akita H. Postpartum vertebral artery dissection with posterior reversible encephalopathy syndrome. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2014-207332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Borelli P, Baldacci F, Vergallo A, et al. Bilateral thalamic infarct caused by spontaneous vertebral artery dissection in pre-eclampsia with HELLP syndrome: a previously unreported association. J Stroke Cerebrovasc Dis. 2012;21 doi: 10.1016/j.jstrokecerebrovasdis.2012.01.007. 914.e9–10. [DOI] [PubMed] [Google Scholar]
- 23.Markus HS, Levi C, King A, Madigan J, Norris J. Cervical Artery Dissection in Stroke Study (CADISS) Investigators. Antiplatelet therapy vs anticoagulation therapy in cervical artery dissection: the Cervical Artery Dissection in Stroke Study (CADISS) randomized clinical trial final results. JAMA Neurol. 2019;76:657–664. doi: 10.1001/jamaneurol.2019.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]