Abstract
Background
With the advent of the COVID-19 pandemic, in-person social interactions and opportunities for accessing resources that sustain health and well-being have drastically reduced. We therefore designed the pan-Canadian prospective COVID-19: HEalth and Social Inequities across Neighbourhoods (COHESION) cohort to provide a deeper understanding of how the COVID-19 pandemic context affects mental health and well-being, key determinants of health, and health inequities.
Methods
This paper presents the design of the two-phase COHESION Study, and descriptive results from the first phase conducted between May 2020 and September 2021. During that period, the COHESION research platform collected monthly data linked to COVID-19 such as infection and vaccination status, perceptions and attitudes regarding pandemic-related measures, and information on participants’ physical and mental health, well-being, sleep, loneliness, resilience, substances use, living conditions, social interactions, activities, and mobility.
Results
The 1,268 people enrolled in the Phase 1 COHESION Study are for the most part from Ontario (47%) and Quebec (33%), aged 48 ± 16 years [mean ± standard deviation (SD)], and mainly women (78%), White (85%), with a university degree (63%), and living in large urban centers (70%). According to the 298 ± 68 (mean ± SD) prospective questionnaires completed each month on average, the first year of follow-up reveals significant temporal variations in standardized indexes of well-being, loneliness, anxiety, depression, and psychological distress.
Conclusions
The COHESION Study will allow identifying trajectories of mental health and well-being while investigating their determinants and how these may vary by subgroup, over time, and across different provinces in Canada, in varying context including the pandemic recovery period. Our findings will contribute valuable insights to the urban health field and inform future public health interventions.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-17297-w.
Keywords: COVID-19, Mental health, Prospective cohort, Social interactions, Study design, Well-being
Background
On January 10, 2020, World Health Organization announced the identification of a new strain of coronavirus, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causing a mild to severe respiratory illness – which may progress to pneumonia and respiratory failure – named coronavirus disease 2019 (COVID-19) [1]. The first positive case of COVID-19 in Canada was reported on January 25, 2020 and a state of health emergency was declared across the country between March 13 and March 22, 2020, depending on the province [2, 3]. Mid-August 2021, there were just over 1.4 million cases in Canada and more than 26,700 deaths [2].
Public health measures to control transmission have brought vast sectors of economic activity to a halt, leading to massive unemployment and reductions in income, while reducing people’s daily movements and opportunities for in-person social interactions [4]. This has affected people’s opportunities and access to resources that sustain mental health and well-being. The COVID-19 conditions reinforce the role of various social and environmental health determinants, with differential impacts on the mental health and well-being of populations, depending on age [5], gender [6], housing conditions [7], education [8], job type [9], income [10], or ethnic background [11–13] and, more generally, social and environmental contexts [14, 15].
COVID-19 conditions including lockdown, curfew and physical distancing measures reduce social contacts, increase social isolation and feelings of loneliness, and decrease levels of social support; these dimensions directly influence well-being and mental health [16, 17]. Canadian data shows pandemic-related increases in social isolation, domestic violence and anxiety [18], with certain groups such as teens, older adults, women and racialized communities particularly at-risk [19]. Daily mobility and related physical activity are reduced through confinement measures and reduced activity spaces have been linked to depressive symptoms [20, 21] and sleep troubles [22]. Walkable environments and access to green space are key environmental conditions linked to positive health outcomes including physical activity and well-being [23]. With shrinking activity spaces and policy constraints curbing daily mobility, the role of residential living conditions is further amplified.
Marginalized populations often bear the burden of poor social and environmental living conditions and have been shown to be disproportionately affected by the socio-economic impacts COVID-19 [24, 25]. Overcrowding or living in inadequate dwellings are important determinants of mental health and well-being; moreover, prolonged exposure to home environments during lockdown conditions further exacerbate these impacts [26, 27]. Economic hardship, which is linked to income reduction and job instability, has heavily contributed to the mental health burden of Canadians, and is also related to housing instability and food insecurity [28, 29]. In turn, detrimental health behavior such as alcohol or other substance use are increasing and are linked to poorer mental health outcomes [30].
In total, there is an urgent need to better understand, in particular, how the unintended long-term consequences of COVID-19 pandemic and mitigation measures, contextual conditions (e.g., housing conditions, neighborhood characteristics), and behavior (e.g., mobility, social interaction, sleep) are linked to mental health and well-being trajectories. Furthermore, impacts are likely to vary between population groups (for instance, according to gender, age, racialized communities, or deprivation level).
We developed the pan-Canadian COVID-19: HEalth and Social Inequities across Neighbourhoods (COHESION) Study to better understand how the COVID-19 pandemic affects health, key determinants of health, and health inequities, with a focus on mental health and well-being. This study will provide longitudinal evidence of how these change over time and across different provinces in Canada.
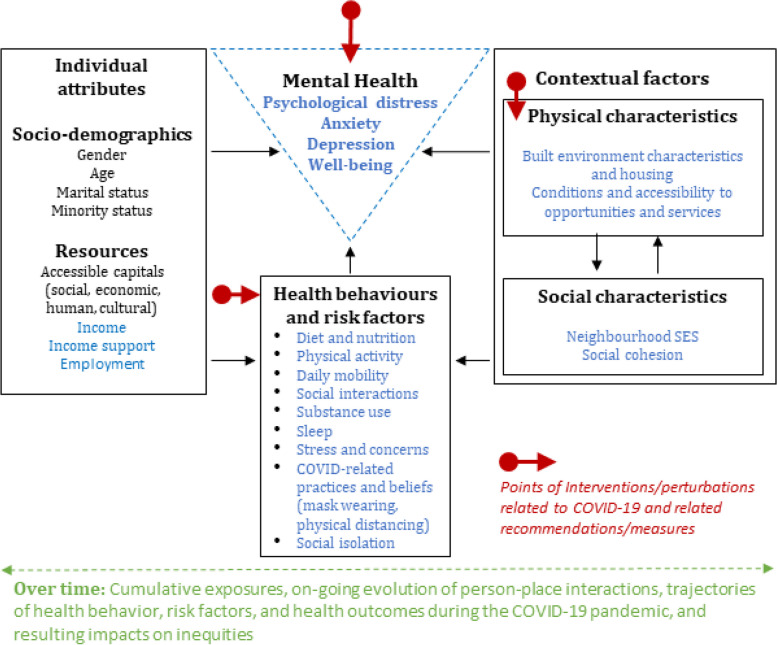
COHESION adopts a built environment and health framework (Fig. 1) recently published by its team members [31]. This framework positions mental health at the intersection of individual level attributes, health behaviours, and contextual factors. Contextual, or neighbourhood factors include physical (e.g. accessibility to green space, transportation infrastructure, and other health-promoting resources), and social characteristics (e.g. social deprivation, social cohesion). These factors directly influence mental health, but their primary impact is indirect, mediated through behavioural pathways. Figure 1 highlights the critical disruption points triggered by the COVID-19 pandemic.
Fig. 1.
Conceptual model of the COHESION Study. Adapted from Wasfi & Kestens (2021) [32]
In the context of the COVID-19 pandemic, the COHESION Study aims:
evaluating the direct impact of physical and social neighborhood characteristics on mental health and well-being trajectories, while controlling for individual-level health behaviors and socio-demographics;
evaluating if and how physical and social neighborhood characteristics may modify the associations between individual-level predictors and mental health and well-being trajectories.
The current paper has two main objectives: (i) to present the design and methods used in the two phases of the COHESION study, and (ii) to present descriptive statistics from the longitudinal follow-up of the study’s first phase, as a basis to discuss cohort characteristics and methodological issues.
Methods
Study design and recruitment
The two-phase COHESION Study is a pan-Canadian prospective cohort study. COHESION Phase 1 was conducted between May 2020 and September 2021. COHESION Phase 2 will be launched in May 2022. All Phase 1 participants will be invited to participate in Phase 2, and additional recruitments (n = 10,000) will be done.
After consenting to participate to the study, participants are invited to fill a short eligibility questionnaire. Inclusion criteria are being aged 15 years or above, currently residing in Canada, and reading or speaking English or French. Eligible participants are then invited to complete a baseline questionnaire.
The recruitment for COHESION Phase 1 was launched on May 11 2020. We used a combination of methods that have proven successful from previous experience in recruiting population-based research project samples [33], including media communication (e.g., newspaper articles, radio interviews), social media promotion (e.g., Facebook, Twitter, Instagram, and LinkedIn), and outreach through partners’ local networks (e.g., local health authorities that relayed the study on their website or through their newsletters).
For COHESION Phase 2, we will further use quota sampling at the health region level, based on 2016’s Census data (i.e., age composition, gender, income, educational attainment, and ethnic background). We engaged Potloc Inc., a tech-enabled consumer research company that conducts survey sampling through social networks (Facebook, Twitter, Instagram, LinkedIn), for geo-targeting of respondents based on the sampling quotas. Potloc Inc.’s algorithm will push sociodemographic and geographically targeted online ads to our study until local quotas are attained (targets are monitored daily) and that 10,000 participants have thereby been enrolled. Furthermore, a geographical oversampling (n = 1,000) will be conducted in Nord-de-l’Île-de-Montréal (NIM) territory (Quebec), in partnership with the NIM’s integrated health and social services center (CIUSSS-NIM).
Enrollment and participation in the two-phase COHESION Study are voluntary, and a raffle of three prizes ($100 gift cards) is drawn every month for active participants for the duration of the study.
Data collection
In the subsequent paragraphs, we will explicitly indicate whether the information discussed pertains to Phase 1, Phase 2, or both phases to provide clarity for the reader.
Involvement options
For both study’s phases, two levels of involvement are proposed. Participants can opt for: (i) participating in the online self-administered questionnaires only (baseline + invitation to follow up questionnaires); or (ii) participating in the questionnaires and downloading a mobile phone application to provide additional active and passive data (cf. 3.2.5).
Baseline questionnaires
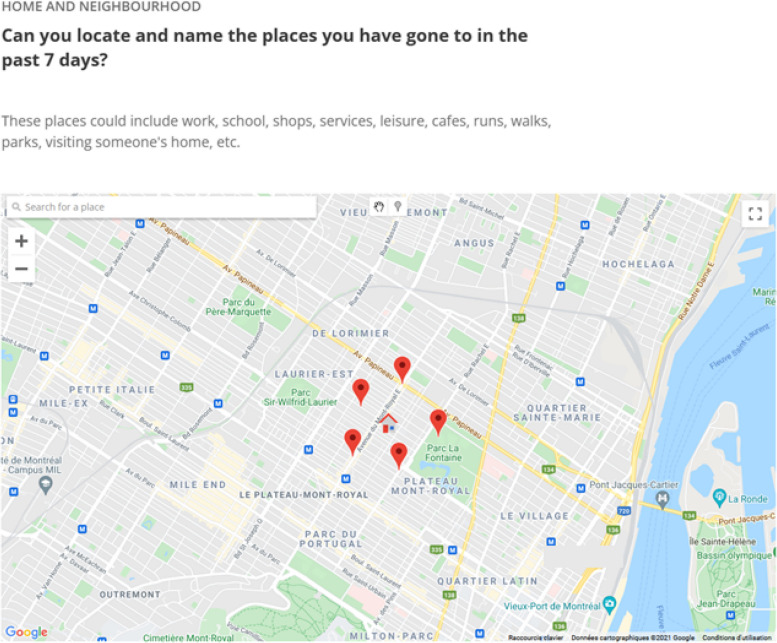
Through the COHESION Study Phase 1 baseline questionnaire (35–45 min), participants report on: their sociodemographic characteristics (e.g., gender, ethnic or cultural background, education level, employment status, income, relationship status, and household composition); housing condition (e.g., house tenure, dwelling type and size, outdoor space) and satisfaction; physical (e.g., chronic disease diagnosis) and mental health conditions (e.g., anxiety and depression), and substance use (alcohol, tobacco, vape, and cannabis); COVID-19 infection status, vulnerability towards COVID-19, perception of- and compliance with COVID-19 mitigation measures, and pre-pandemic employment, income, substances use, loneliness, resilience, and social interactions. Additionally, a map-based questionnaire collects data on activity locations and social contacts (cf. Fig. 2). For parents, a supplementary module on mental health and perceptions of COVID-19 mitigation measures concerning adolescents and children who live in the household is administered (participants answer on behalf of children in their household).
Fig. 2.
Collecting data on living and activity places with VERITAS-Social. Screenshot from the VERITAS application (map-based survey tool – permission given from Polygon Inc.) for a fictional participant; the house icon locates the participant’s residential address and the pin icons symbolize the visited places located by the participant
The COHESION Study Phase 2 baseline questionnaire will consist in one core (10 min) and two optional complementary Sect. (15 min each). The core baseline questionnaire includes: sociodemographic characteristics and key housing conditions; COVID-19 vaccination status, perceptions of COVID-19 pandemic and related mitigation measures; standardized modules assessing general health (first item of the 12-item Short-Form Health Survey) [34], well-being (5-item World Health Organization Well-Being Index, WHO-5 Index) [35], sleep credit (Pittsburgh Sleep Quality Index, PSQI, 4 items only) [36], and psychological distress (Psychological Distress Scale, Kessler-6) [37]; and an outdoor mobility and social interactions module. Optional complementary baseline sections include the map-based questionnaire on activity locations and social contacts (cf. 3.2.4) and additional in-depth questions on relevant themes: additional items retrieved from the Phase 1 baseline questionnaire (it means all items not already included in the Phase 2 core baseline questionnaire); standardized modules on loneliness (University of California Los Angeles, UCLA, 3-item loneliness score) [38], anxiety symptoms (7-item Generalized Anxiety Disorder, GAD-7) [39], depression symptoms (9-item Patient Health Questionnaire, PHQ-9) [40], resilience (6-item Brief Resilience Scale) [41], sense of belonging (Canada Community Health Survey, CCHS) [42], and physical activity (Godin Leisure-Time Exercise) [43]; items for assessing conspiracy beliefs.
Slightly shorten versions of the Phase 2 baseline questionnaires (i.e., excluding questions about birth, cultural background, etc.) have been provided for participants coming from Phase 1 and wishing going on Phase 2.
Follow-up questionnaires
Follow-up questionnaires of the COHESION Study are short questionnaires (15 min). For Phase 1, they were first offered biweekly until August 2020, then monthly. COVID-19-related topics cover infection and/or vaccination status, perceived vulnerability, perception of and compliance with mitigation measures, position regarding vaccination, and conspiracy beliefs. Health-related questions focus on general health (SF-12, first item) [34], well-being (WHO-5 Index) [35], sleep credit (PSQI, 4 items only) [36], loneliness (UCLA 3-item loneliness score) [38], anxiety symptoms (GAD-7) [39], depression symptoms (PHQ-9) [40], psychological distress (Kessler-6) [37], and sense of belonging (CCHS) [42] (Table 1). Employment status, household income, and substance use are also documented. Additionally, participants are asked at each follow-up about any changes concerning their place of residence and housing conditions. Supplementary module on mental health and perception of COVID-19 mitigation measures concerning children or adolescents living at home is administered when applicable.
Table 1.
Main information collected in the framework of the COHESION Study Phase 1 prospective follow-up (June 2020 to July 2021)
| Survey (year/week) | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Theme | Assessment tool | Assessment period | 20/26 | 20/30 | 20/32 | 20/34 | 20/36 | 20/38 | 20/40 | 20/44 | 20/48 | 20/52 | 21/03 | 21/07 | 21/11 | 21/15 | 21/19 | 21/23 | 21/27 |
| COVID-19 | |||||||||||||||||||
| COVID-19 infection status | At the questionnaire administration point | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |
| COVID-19-pandemic-related perceptions | At the questionnaire administration point | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |
| Anti-COVID-19 measures compliance | At the questionnaire administration point | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| Position towards anti-COVID-19 vaccine | At the questionnaire administration point | X | X | X | X | X | X | ||||||||||||
| Anti-COVID-19 vaccination status | At the questionnaire administration point | X | X | X | X | X | |||||||||||||
| Health / Well-being | |||||||||||||||||||
| General health | SF-12 (first item only) | During the past 2 weeks | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Well-being | WHO-5 Index | During the past 2 weeks | X | X | X | X | X | ||||||||||||
| Loneliness | UCLA 3-item loneliness score | During the past 2 weeks | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| Anxiety symptoms | 7-item Generalized Anxiety Disorder (GAD-7) | During the past 2 weeks | X | X | X | X | X | X | X | X | |||||||||
| Depression symptoms | 9-item Patient Health Questionnaire (PHQ-9) | During the past 2 weeks | X | X | X | X | X | X | X | X | |||||||||
| Psychological distress symptoms | 6-item Psychological Distress Scale (Kessler-6) | During the past 2 weeks | X | X | X | X | X | X | X | X | X | X | X | ||||||
| Behaviors | |||||||||||||||||||
| Outdoor mobility | VERITAS | During the past 7 days | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Social interactions | VERITAS | During the past 7 days | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Sleep credit | Pittsburgh Sleep Quality Index | During the past month | X | X | X | X | X | X | X | X | X | ||||||||
| Substance use a | Frequency questionnaire | During the past 2 weeks | X | X | X | X | X | X | X | X | X | X | |||||||
aFour items: alcohol, cigarettes, vape, and cannabis.
Follow-up questionnaire waves are named according to their week and year of release (for instance, “20/26” for the follow-up questionnaire proposed to participants in the 26th week of 2020).
For Phase 2, follow-up questionnaires will be split in a core (‘light’) and an optional complementary (‘complete’) sections, and will be offered every two months. It will include the same questions as for Phase 1, adding a standardized module for assessing physical activity (Godin Leisure-Time Exercise Questionnaire) [43].
Questions can vary between follow-ups, depending on the situation and priorities raised by the research team and our public health partners. Thus, these additional themes can focus on health insecurity (i.e., access to health care, prescriptions and medicine) [44], sleep troubles (PSQI) [36], food insecurity (10-item Health Canada Household Food Security Module) [45], and children’s difficulties (if any) [45].
For Phase 1, follow-up questionnaire waves are named according to their week and year of release (for instance, “20/26” for the follow-up questionnaire proposed to participants in the 26th week of 2020).
Use of VERITAS-Social to collect daily mobility and social interaction data
One of the specificities of COHESION is that it integrates, in baseline and follow-up questionnaires of the two phases, the Visualization and Evaluation of Route Itineraries, Travel destinations, Activity spaces and Social interactions (VERITAS-Social) questionnaire. For COHESION, it was adapted to locate a possible list of up to 20 activities carried out during the past seven days (Fig. 2). As previously described, VERITAS-Social is an interactive map-based questionnaire that jointly collects an individual’s social network and activity locations [46]; it is an adaptation of the VERITAS tool, an interactive questionnaire for geo-locating places, and related information of interest (e.g., frequency of visit, transportation modes used) [47]. It uses a Google Map module to facilitate the location of activity places. The social module asks if an activity location is generally visited alone or with someone else; participants can identify one or more individuals, or a group of people (see S1a-b Figs). In other words, it is a name generator that identifies network members based on their co-presence at reported destinations [48]. Data on network members include age, gender, type of relationship (e.g., friend, acquaintance), frequency of interactions, and duration of the relationship; for groups, data includes the number of people in the group, and the duration of the relationship.
Once all activities, corresponding locations, and all people with whom these activities are carried out have been reported, participants are asked to identify members of their social network from whom they receive support or with whom they enjoy spending time with, including members who may not have been reported among the people seen at usual activity venues. Finally, participants were able to indicate interpersonal relationships between network members (i.e., who knows whom), and whether some specific individuals belonged to documented groups.
In Phase 1, the VERITAS-Social questionnaire was mandatory for all participants. To optimize the representativeness of our sample, we adapted our approach in Phase 2 by making this questionnaire optional.
Optional mobile application
Participants enrolling in the mobile phone arm of the study were invited to download Ethica Data mobile application (cf. 3.2.1), used successfully in previous research projects [49]. Once installed and launched, the application passively monitors location and mobility (e.g., stationary, in vehicle, walking, or biking) using GPS data (1 min of data collected every 5 min), physical activity (step counter), and social contacts (other smartphones), derived from listings of other Bluetooth discoverable devices in the participant’s surroundings (for more details see [50]). The app further prompts participants to complete Ecological Momentary Assessment (EMA) questionnaires three times a day for one week every month. EMA questionnaires include short self-reports (< 1 min) on well-being, sleep, mood (Short Mood Scale, 6 items) [51], and social interactions (see S2 Fig).
Environmental data
Because some of the data collected is spatial (e.g. place of residence, VERITAS-Social locations, mobile app GPS data), we are able to add area-level environmental data to our dataset. This allows to explore links between individual-level measures and social and environmental contextual conditions. Numerous environmental datasets covering Canada are available through the Canadian Urban Environmental Health Research Consortium (CANUE), which can be linked to our dataset using the 6-position postal code – a key identifier for all participants.
Contextual variables of interest include measures of neighborhood deprivation, such as the Material and Social Deprivation Indices (MSDI; data 2016) available at the Canadian Census dissemination area level (i.e., the smallest Canadian standard geographic area, with a population of 400 to 700 persons) [52]. These two composite indexes combine Census data on educational attainment, employment ratio, average income, and household composition.
The urbanization degree is measured using Statistics Canada classification (at the four-digit code area level; data 2016), based on the number of inhabitants in population centers [53]. “Small”, “medium” and “large” urban population centers correspond to areas embracing between 1,000 and 29,999, between 30,000 and 99,999, and 100,000 and more inhabitants, respectively, while “rural area” is a residual value gathering all areas located outside population centers.
Greenness is evaluated using the growing season Normalized Difference Vegetation Index (NDVI) (at the six-digit code area level; data 2019), based on Landsat 8 satellite data [54, 55].
Area-level walkability is measured using the Canadian Active Living Environments (CAN-ALE) database [56].
Additional localized and temporalized data on COVID-19 pandemic conditions, including lockdowns, curfews, vaccination plan, number of cases, and emergence of variants is also available through the Canadian Institute for Health Information (CIHI) compilation [57].
Ethics and data management plan
Before completing the eligibility questionnaire, potential participants are first invited to read the consent form and provide an electronic written consent to participate in the study. Informed consent was then obtained from all subjects and/or their legal guardian(s). In Phase 2, a second consent will be required from participant wishing to register for the prospective follow-ups after having completed baseline questionnaire. Phase 1 COHESION was approved by the ethics board of the Centre de Recherche du Centre Hospitalier de l’Université de Montréal (CRCHUM; MP-02-2021-8924) and by the Public Health Agency of Canada (PHAC) ethical review board (REB 2020-016P). Phase 2 COHESION was approved by both the ethics board of the Centre Intégré Universitaire de Santé et de Services Sociaux du Nord-de-l’Île-de-Montréal (CIUSSS-NIM ; 2022–2327) and PHAC (REB 2020-016P). All methods used in the project were carried out in accordance with relevant guidelines and regulations.
For data security and privacy proposal, all data are hosted on Compute Canada servers with secondary backups on hospital-grade internal servers. All data has been stripped from any personally identifying information, with only the principal investigator being able to track the records back to one participant. Researchers can access anonymized individual level records by connecting directly through a Secure Shell (SSH) to the database hosted on Compute Canada (a SSH allows remote machines accessing data in a secure way since the connection is encrypted). They can also access aggregated data for analysis through a secure online platform hosted by Tableau [58]. A document listing all the data management policies governing data access and storage has been submitted to the ethic board for approval.
Results
Recruitment and participants
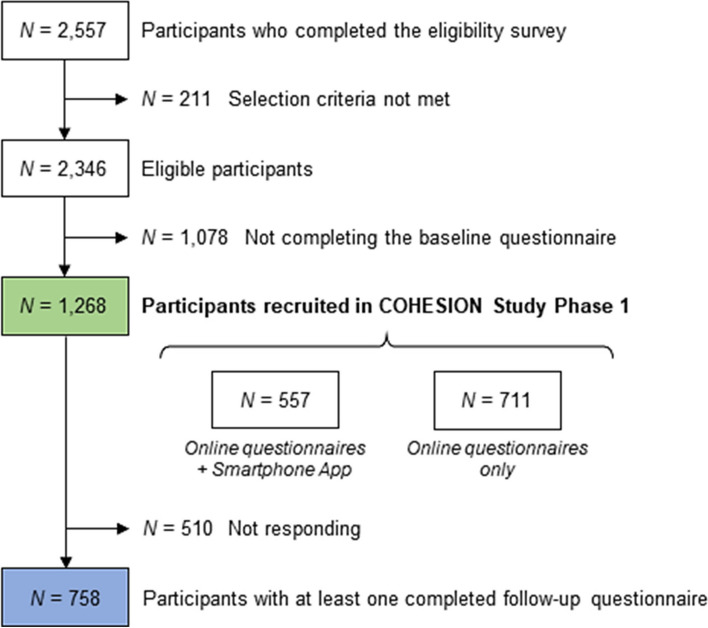
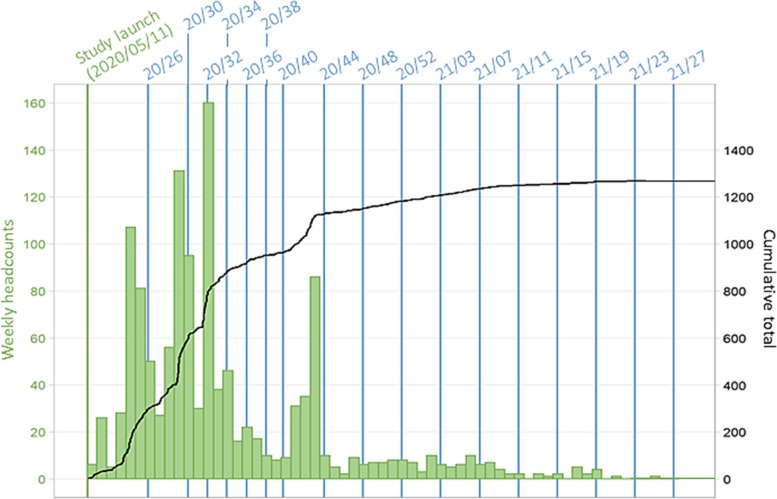
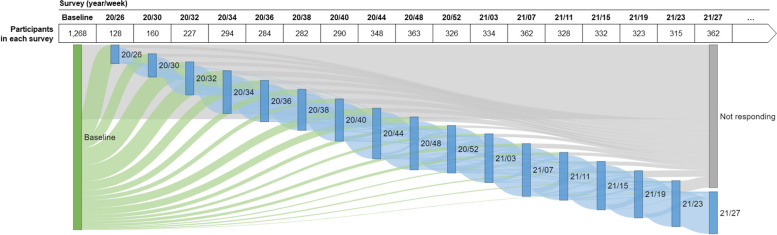
Among the 2,557 people who completed the COHESION Phase 1 eligibility questionnaire, 2,346 (92%) met the selection criteria (Fig. 3). Among these ones, 1,268 (54%) completed the baseline questionnaire and have been enrolled in the COHESION Study, and among the latter, 557 (44%) opted for the Ethica mobile application in addition to the online self-administered questionnaires. Although recruitment was continuously open during the Phase 1 timespan, the major part of participants joined the study during the first months following the study launch: 832 (66%) recruitments after three months of follow-up, 1,136 (90%) after six months (Fig. 4).
Fig. 3.
Flow chart of participants’ recruitment to the COHESION Study Phase 1 (June 2020 to July 2021)
Fig. 4.
Timeline of recruitment of the COHESION Study Phase 1 participants (N = 1,268). Follow-up questionnaire waves are named according to their week and year of release (for instance, “20/26” for the follow-up questionnaire proposed to participants in the 26th week of 2020)
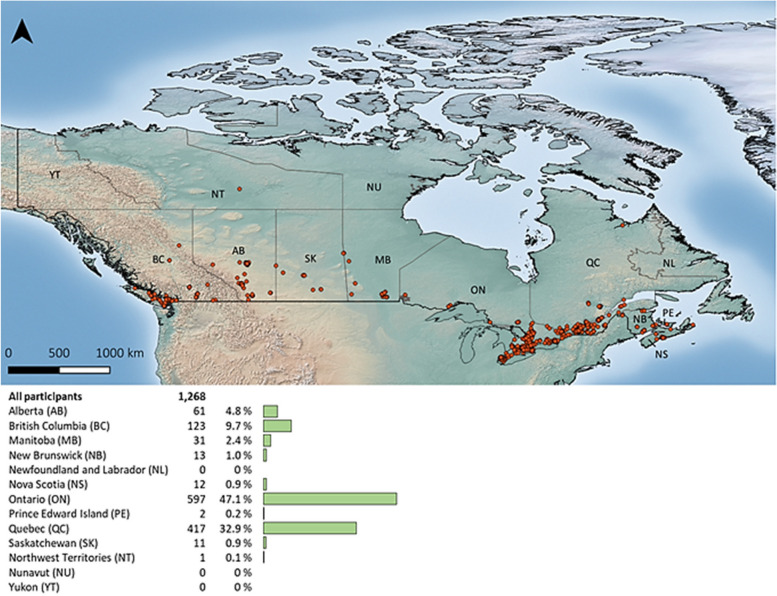
COHESION Phase 1 participants are distributed all across Canada; they live mainly in Ontario (597, 47%) and Quebec (417, 33%) (Fig. 5), and 910 (72%) declared English as their first language. They are in average 48 ± 16 years (mean ± standard deviation, SD) and are mainly women (78% [vs. 50% in the total Canadian population]), White (85% [vs. 72%]), born in Canada (85% [vs. 78%]), with university or post-graduate level degree (63% [vs. 28.5%]), and in a relationship (67% [vs. 58%]) (Table 2). The majority of participants are homeowners (62%) and reside in a house (66%), living with their partner or family (74%). Most do not have children living at home (72%), have access to private outside space (97%), and own pets (56%), and are located in large urban centers (i.e., areas with over 100,000 inhabitants). However,ugh participants exhibit considerable contrasts in the greenness of their home surroundings and the level of material and social deprivation in their neighborhoods (Table 3). In descending order, participants employed (58%), retired (19%), unemployed (14%), on leave or disabled (5%), or students (2%). The majority are satisfied with their household annual income (77%) (Table 2). Regarding their health, 44% have been affected by at least one physical chronic disease (i.e., heart disease, lung disease, cancer, high blood pressure, diabetes, severe obesity, and/or autoimmune disease), and 35% have been affected by at least one mental chronic disease (i.e., depressive disorder and/or anxiety disorder). A monthly consumption of alcohol, cigarettes and/or vape, and cannabis was reported by 72%, 14%, and 18% of participants at baseline, respectively. Lastly, they are 27% and 38% considering their selves and/or someone in their household at a high risk of being infected by- or of complications of COVID-19, respectively.
Fig. 5.
Geographical distribution of COHESION Study Phase 1 participants across Canada (N = 1,268). Figure obtained from “maps” R package
Table 2.
Description of COHESION Study Phase 1 participants, at recruitment (N = 1,268)
| Characteristics | N | Percent |
|---|---|---|
| Demographics | ||
| Age category | ||
| 15-24 | 103 | 8.1 % |
| 25-34 | 231 | 18.2 % |
| 35-44 | 227 | 17.9 % |
| 45-54 | 230 | 18.1 % |
| 55-64 | 282 | 22.2 % |
| ≥65 | 195 | 15.4 % |
| Gender | ||
| Woman | 985 | 77.7 % |
| Man | 243 | 19.2 % |
| Other identity | 40 | 3.2 % |
| Ethnic or cultural group | ||
| White | 1,080 | 85.2 % |
| Other group | 188 | 14.8 % |
| Born in Canada | ||
| Yes | 1,073 | 84.6 % |
| No | 195 | 15.4 % |
| Education level | ||
| School degree | 179 | 14.1 % |
| College degree | 278 | 21.9 % |
| University degree | 408 | 32.2 % |
| Post-graduate degree | 393 | 31.0 % |
| Unknown / Not answered | 10 | 0.8 % |
| Employment | ||
| Employed, full-time | 545 | 43.0 % |
| Employed, part-time | 148 | 11.7 % |
| Self-employed | 36 | 2.8 % |
| Unemployed | 183 | 14.4 % |
| Retired | 245 | 19.3 % |
| On leave / Disabled | 59 | 4.7 % |
| Student | 24 | 1.9 % |
| Other | 28 | 2.2 % |
| Relationship | ||
| In a relationship / Married | 847 | 66.8 % |
| Single | 282 | 22.2 % |
| Separated / Divorced / Widowed | 135 | 10.6 % |
| Other | 4 | 0.3 % |
| Household characteristics | ||
| Household composition | ||
| Alone | 274 | 21.6 % |
| With my family | 482 | 38.0 % |
| With my partner | 451 | 35.6 % |
| Other | 61 | 4.8 % |
| Children (living at home) | ||
| 0 | 918 | 72.4 % |
| 1 | 155 | 12.2 % |
| 2 | 137 | 10.8 % |
| ≥3 | 58 | 4.6 % |
| Household annual income | ||
| <$21,000 | 153 | 12.1 % |
| $21,000-$36,000 | 173 | 13.6 % |
| $36,000-$48,000 | 141 | 11.1 % |
| $48,000-$96,000 | 337 | 26.6 % |
| ≥$96,000 | 279 | 22.0 % |
| Unknown / Not answered | 185 | 14.6 % |
| Characteristics | N | Percent |
| Satisfaction regarding income/needs | ||
| Very well | 453 | 35.7 % |
| Well | 522 | 41.2 % |
| Not well | 271 | 21.4 % |
| Unknown / Not answered | 22 | 1.7 % |
| Pet ownership | ||
| Yes | 693 | 56.4 % |
| No | 536 | 43.6 % |
| Housing | ||
| House tenure | ||
| Owner | 786 | 62.0 % |
| Renter | 382 | 30.1 % |
| Other | 69 | 5.4 % |
| Unknown / Not answered | 31 | 2.4 % |
| Dwelling type | ||
| House | 833 | 65.7 % |
| Apartment / Condo | 419 | 33.0 % |
| Other | 12 | 0.9 % |
| Unknown / Not answered | 4 | 0.3 % |
| Private outside space | ||
| Yard or nature | 963 | 78.4 % |
| Balcony or terrace | 225 | 18.3 % |
| No | 41 | 3.3 % |
| General health | ||
| Chronic physical disease | ||
| Yes | 557 | 43.9 % |
| No | 688 | 54.3 % |
| Unknown / Not answered | 23 | 1.8 % |
| Chronic mental disease | ||
| Yes | 441 | 34.8 % |
| No | 794 | 62.6 % |
| Unknown / Not answered | 33 | 2.6 % |
| Substance use | ||
| Alcohol a | ||
| No | 352 | 27.8 % |
| At least once a month | 245 | 19.3 % |
| At least once a week | 465 | 36.7 % |
| At least once a day | 206 | 16.2 % |
| Cigarettes and/or vape a | ||
| No | 1,095 | 86.4 % |
| At least once a month | 16 | 1.3 % |
| At least once a week | 11 | 0.9 % |
| At least once a day | 146 | 11.5 % |
| Cannabis a | ||
| No | 1,036 | 81.7 % |
| At least once a month | 88 | 6.9 % |
| At least once a week | 57 | 4.5 % |
| At least once a day | 87 | 6.9 % |
| COVID-19 b | ||
| At a high risk of being infected | ||
| Yes | 327 | 26.6 % |
| No | 902 | 73.4 % |
| At a high risk of complications | ||
| Yes | 465 | 37.8 % |
| No | 764 | 62.2 % |
aDuring the month before completing baseline questionnaire.
bParticipant and/or someone in his/her household.
Table 3.
Residential social and environmental measures (N = 1,268)
| Indexes | N | Percent |
|---|---|---|
| Urbanization degree =a | ||
| Large center | 891 | 70.4 % |
| Medium center | 102 | 8.1 % |
| Small center | 138 | 10.9 % |
| Rural | 135 | 10.7 % |
| Surrounding greenness (NDVI) b | ||
| <0.28 | 254 | 20.1 % |
| 0.28-0.36 | 259 | 20.5 % |
| 0.36-0.43 | 266 | 21.0 % |
| 0.43-0.51 | 233 | 18.4 % |
| ≥0.51 | 253 | 20.0 % |
| Material deprivation index c | ||
| Quintile 1 | 295 | 24.5 % |
| Quintile 2 | 279 | 23.2 % |
| Quintile 3 | 257 | 21.4 % |
| Quintile 4 | 203 | 16.9 % |
| Quintile 5 | 169 | 14.0 % |
| Social deprivation index c | ||
| Quintile 1 | 162 | 13.5 % |
| Quintile 2 | 162 | 13.5 % |
| Quintile 3 | 199 | 16.5 % |
| Quintile 4 | 251 | 20.9 % |
| Quintile 5 | 429 | 35.7 % |
aAccording to Statistics Canada classification, “small”, “medium” and “large” centers correspond to areas including between 1,000 and 29,999, between 30,000 and 99,999, and 100,000 and more inhabitants, respectively, while “rural area” is a residual value gathering all areas located outside population centers (at the four-digit code area level; data 2016) [52].
bQuintiles of the growing season Normalized Difference Vegetation Index (NDVI) in the COHESION Study cohort (at the six-digit code area level; data 2019) [53, 54].
cQuintiles of the distribution over the whole Canadian territory (at the Canadian Census dissemination area level; data 2016) [51].
Prospective follow-up and attrition
Throughout the first year of follow-up, i.e., from May 2020 to July 2021, up to 17 follow-up questionnaires were administered to participants (Fig. 4), and 758 (60%) participants completed at least one (Fig. 3). Depending on their date of recruitment, participants were contacted between one and seventeen times as part of the prospective follow-up waves (Fig. 4), and they filled out in average 29% ± 36% (mean ± SD) of the follow-up questionnaires they received. Among the first year of follow-up, in average 298 ± 68 participants completed the follow-up questionnaire by wave (Fig. 6, see S1 Table).
Fig. 6.
Participation in Phase 1 of the COHESION Study, baseline and follow-ups (June 2020 to July 2021; N = 1,268). Follow-up questionnaire waves are named according to their week and year of release (for instance, “20/26” for the follow-up questionnaire proposed to participants in the 26th week of 2020). Green flow shows participants responding for the first time to a follow-up questionnaire, blue flow shows participants responding again to a follow-up questionnaire, and grey flow shows participants not responding to follow-ups
Attrition rate throughout the Phase 1 follow-up appeared statistically distinct in some specific groups (Table 4). The older the participants were and the higher the education level was, the less the attrition was (p < 0.001 and p = 0.069, respectively); average age was 50 ± 16 years and 45 ± 16 years (mean ± SD) in people participating or not in the longitudinal follow-up, respectively (p < 0.001). Attrition appeared higher in employed people and lower in retired ones (p < 0.001) (Table 4), and also higher in people living in family (p = 0.005), with children (p = 0.013), with pets (p = 0.001), in a house (p = 0.001), and not owner (p = 0.001) (see S2a Table). Lastly, people with a chronic physical disease (p = 0.039) or at a high risk of being infected by the COVID-19 (p = 0.001) were less prone to participate to the follow-up. No contrast was noticed according to substance use or residential social and environmental components (see S2a-b Tables).
Table 4.
Attrition in the COHESION Study Phase 1, and comparison of participants enrolling or not in the prospective follow-up according to demographics (N = 1,268)
| Participating in follow-ups (N = 758) | Participated in baseline only (N = 510) | ||||
|---|---|---|---|---|---|
| Characteristics | N | Percent | N | Percent | p -value a |
| Age category | <0.001 | ||||
| 15-24 | 47 | 6.2 % | 56 | 11.0 % | |
| 25-34 | 120 | 15.8 % | 111 | 21.8 % | |
| 35-44 | 134 | 17.7 % | 93 | 18.2 % | |
| 45-54 | 131 | 17.3 % | 99 | 19.4 % | |
| 55-64 | 183 | 24.1 % | 99 | 19.4 % | |
| ≥65 | 143 | 18.9 % | 52 | 10.2 % | |
| Gender | 0.63 | ||||
| Woman | 591 | 78.0 % | 394 | 77.3 % | |
| Man | 146 | 19.3 % | 97 | 19.0 % | |
| Other identity | 21 | 2.8 % | 19 | 3.7 % | |
| Ethnic or cultural group | 0.64 | ||||
| White | 649 | 85.6 % | 431 | 84.5 % | |
| Other group | 109 | 14.4 % | 79 | 15.5 % | |
| Born in Canada | 0.12 | ||||
| Yes | 631 | 83.2 % | 442 | 86.7 % | |
| No | 127 | 16.8 % | 68 | 13.3 % | |
| Education level | 0.069 | ||||
| School degree | 94 | 12.4 % | 85 | 16.7 % | |
| College degree | 169 | 22.3 % | 109 | 21.4 % | |
| University degree | 235 | 31.0 % | 173 | 33.9 % | |
| Post-graduate degree | 254 | 33.5 % | 139 | 27.3 % | |
| Unknown / Not answered | 6 | 0.8 % | 4 | 0.8 % | |
| Employment | <0.001 | ||||
| Employed, full-time | 300 | 39.6 % | 245 | 48.0 % | |
| Employed, part-time | 85 | 11.2 % | 63 | 12.4 % | |
| Self-employed | 23 | 3.0 % | 13 | 2.5 % | |
| Unemployed | 99 | 13.1 % | 84 | 16.5 % | |
| Retired | 192 | 25.3 % | 53 | 10.4 % | |
| On leave / Disabled | 29 | 3.8 % | 30 | 5.9 % | |
| Student | 13 | 1.7 % | 11 | 2.2 % | |
| Other | 17 | 2.2 % | 11 | 2.2 % | |
| Relationship | 0.59 | ||||
| In a relationship / Married | 511 | 67.4 % | 336 | 65.9 % | |
| Single | 160 | 21.1 % | 122 | 23.9 % | |
| Separated / Divorced / Widowed | 85 | 11.2 % | 50 | 9.8 % | |
| Other | 2 | 0.3 % | 2 | 0.4 % | |
aChi-square test (or Fisher exact test for low numbers).
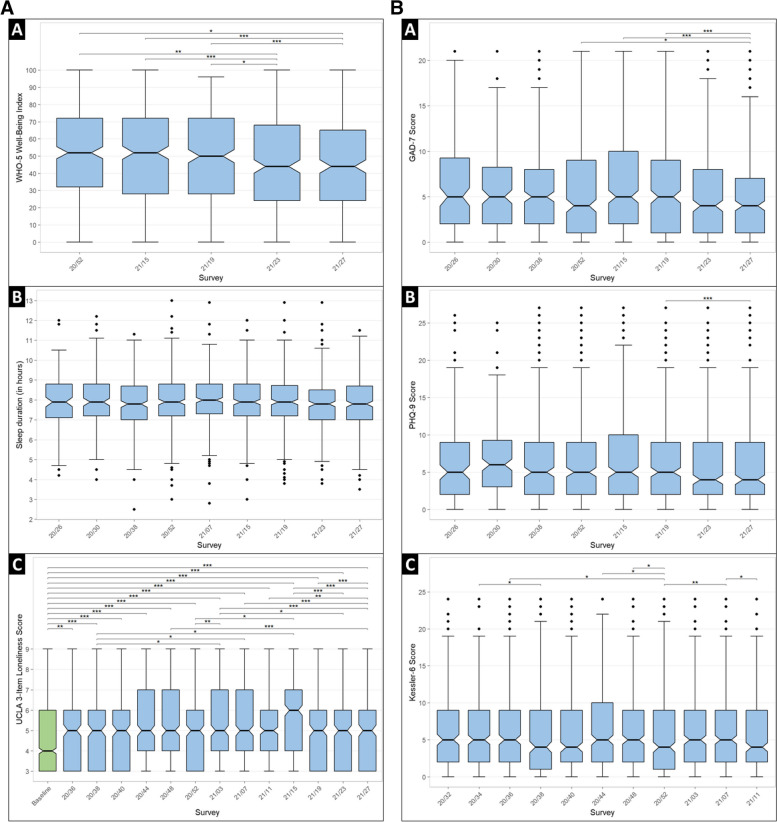
Well-being and mental health
From June 2020 to July 2021, we administered to participants well-being, sleep credit, loneliness, anxiety, depression and psychological distress -related standardized modules 5, 9, 13, 8, 8, and 11 times, respectively (Table 1). During this period, each thematic module was completed at least once by 481 (38%), 630 (50%), 658 (52%), 612 (48%), 612 (48%), and 692 (55%) Phase 1 participants, respectively (see S3a-b Tables).
The median of the 5-WHO well-being Index ranged from 44% (interval interquartile, IQR: 24–65; wave 21/27) to 52% (IQR: 32–72; wave 20/52) depending on the wave. Well-being appeared decreasing waves after waves, the median index value from the last two administered waves (21/23 and 21/27, corresponding to June and July 2021), being significantly lower than those from the initial three waves (20/52, 21/15, and 21/19, corresponding to December 2020, April, and May 2021, respectively) (Fig. 7a; see S4a Table). Sleep duration remained stable throughout the first year of the Phase 1 follow-up (mean ± SD: from 7.9 ± 1.3 to 8.0 ± 1.4 h; waves 21/23 and 20/30, respectively), with no statistically changes observed. During the prospective follow-up, the median of the UCLA 3-item loneliness score oscillated between 5 (IQR: 3–6; wave 21/27) and 6 (IQR: 4–7; wave 21/15). These variations were statistically significant, with heightened feeling of loneliness occurring from October 2020 (wave 20/44) to April 2021 (wave 21/15), except for wave 20/52, which coincided with the holiday season. Moreover, all UCLA 3-item loneliness scores during the follow-up were significantly higher than the retrospectively assessed median score for the pre-pandemic period (4; IQR: 3–6).
Fig. 7.
a (A) Well-being (WHO-5 Index) level, (B) sleep duration, and (C) feeling of loneliness (UCLA 3-item loneliness score) throughout the first year of prospective follow-up of the COHESION Study Phase 1. Significance of comparison tests, after Bonferroni correction: * <0.05, ** <0.01, *** <0.001. Green: baseline questionnaire; blue: follow-up questionnaire. Follow-up questionnaire waves are named according to their week and year of release (for instance, “20/26” for the follow-up questionnaire proposed to participants in the 26th week of 2020). b. Symptoms of (A) anxiety (7-item Generalized Anxiety Disorder, GAD-7, score), (B) depression (9-item Patient Health Questionnaire, PHQ-9, score), and (C) psychological distress (6-item Kessler Psychological Distress Scale) throughout the first year of prospective follow-up of the COHESION Study Phase 1. Significance of comparison tests, after Bonferroni correction: * <0.05, ** <0.01, *** <0.001. Follow-up questionnaire waves are named according to their week and year of release (for instance, “20/26” for the follow-up questionnaire proposed to participants in the 26th week of 2020
Concerning mental health, the first year of Phase 1 follow-up showed statistically significant changes between questionnaire waves in reporting of anxiety symptoms, depression symptoms, and psychological distress (Fig. 7b; see S4b Table). The GAD-7 median score ranged from 4 (IQR: 1–7; wave 21/27) to 5 (IQR: 2–10; wave 21/15), while the PHQ-9 median score varied between 4 (IQR: 1–7; wave 21/27) and 6 (IQR: 3-9.3; wave 20/30). For both composite indexes, the lowest median value was observed in wave 21/27 (2021, July), with some statistically significant differences noted among the waves. Lastly, the Kessler-6 psychological distress median score oscillated between 4 (IQR: 1–9; wave 20/52) and 5 (IQR: 2–10; wave 20/44); numerous comparisons of the psychological distress median scores from wave 20/52 (2020, December) to other waves showed statistically significant contrasts.
Discussion
Overview of findings
More than 1,200 people enrolled in the Phase 1 of the pan-Canadian COHESION cohort, and about 60% of them participated in the prospective follow-up. The COHESION Study overrepresents women, White and graduated people. The first year of follow-up reveals significant temporal variations in standardized indices of well-being, loneliness, anxiety, depression, and psychological distress.
Challenges. Lessons learned from phase 1, and proposed adaptations for phase 2
Addressing attrition
Loss to follow-up is an issue in any longitudinal study. In Phase 1, attrition was related to age, education level, employment, housing conditions, and some health conditions, similar to other longitudinal studies [59, 60]. To try to reduce attrition in Phase 2 and better retain those that are at greatest risk of loss to follow-up, we have devised the following strategies: (1) Reminders: Our questionnaire platform provides automated reminders for online follow-up survey completion including for EMA; (2) Flexibility: Phase 2 will offer easier participation options, relying on a multi-stage on-boarding process, which includes a short initial 10-min questionnaire and easy-to-sign-up longitudinal follow-ups, with possible ‘light’ or ‘complete’ choices. To increase accessibility, participation and retention (notably with younger participants), we have also optimized the online questionnaire for ease of use through smartphones. (3) Gifts: While enrollment and participation to the COHESION Study are free and voluntary, a lottery of 3 monthly prizes ($100 gift cards) is organized for active participants. In Phase 2, participants who choose the full participation (by completing the optional follow-up questionnaire modules) will be entered twice in the raffle to increase their chance of winning. (4) Improved feedback: In December 2020, an opinion survey was sent to participants to gather feedback on the experience of COHESION Study Phase 1, including on perceived complexity, length, and usability of the questionnaires, interest in surveyed topics, interactions with the mobile application. Suggestions for improvement included better messaging on the purpose of the study, including through regular updates and better recognition of their contribution, and sharing stories to increase the sense of belonging. These elements were considered when re-designing the study for Phase 2, in collaboration with the Center of Excellence on Partnership with Patients and the Public [61]. As suggested by Fumagalli et al. (2013), promising approaches based on persona principles as those used in marketing strategies might help. Thus, we plan to tailor the content of newsletters, to strengthen the sense of belonging of those most at risk of dropping out, a strategy that has proved effective for re-engaging young and busy people [62]. Despite all these methodological efforts to minimize it, the risk of attrition can hardly be eliminated. One way to account for the potential effect of residual attrition bias is through various analytical strategies, including the use of inverse probability weights for trajectory analyses (e.g., growth curve models) on mental health and well-being. Beyond these measures, to further understand and adjust for any potential biases in our results, we have planned analyses stratified by age, gender, and specific individual socio-demographic characteristics.
Inclusion of marginalized populations
It is important to include marginalized populations better. We have worked in collaboration with public health partners to identify best recruitment strategies, including by building connections with local partners (e.g., Médecins du Monde, Red Cross, Food banks) that are working directly with various priority groups and have established trust with these individuals and communities [63]. The use of high-precision targeted social media campaigns, provided by partnering consumer research company Potloc Inc., along with continuous monitoring of stratified targets by region, age and gender, should also contribute to optimize sample representation. Now, because the survey uses online technologies that may be a barrier for participation in remote communities and for more marginalized groups, we will also offer computer-assisted phone interviews (CAPI) during working hours through our study helpline. CAPI refers to a data collection method in which an interviewer conducts a structured survey over the phone while using a computer or digital device to guide the interview process and record responses [32].
Addressing the lack of pre-pandemic baseline
One critical issue with our cohort that was launched in mid-spring 2020 is the lack of a true pre-pandemic baseline. This can partly be circumvented with retrospective questions, but as time goes by, the recall bias increases, particularly for subjective mental health measures [64]. In response to this, starting in fall 2020, we employed a two-fold strategy to reduce cognitive effort and bias. First we asked broader questions about psychological changes since the pandemic’s onset (improvement, deterioration, no change). Second, we incorporated more factual questions with a lower likelihood of recall bias, such as the use of mental health services and substance use in the pre-pandemic year, which will be factored into our trajectory analyses. Despite these adaptations, the risk of recall bias remains, meaning that interpretation about change from pre-pandemic measures should be done with caution.
Adapting surveys and advantages of prospective cohort design
An advantage of a prospective cohort design is the potential for adapting surveys to new or unforeseen circumstances, including evolving priorities of public health authorities. As months passed by and the situation evolved, we developed and administered new modules to address such needs, including on substance use, a priority identified by our partner the Public Health Agency of Canada, or on parent-related stress during the back-to-school periods. Repeated surveys also provide the opportunity for timely dissemination of findings. To facilitate dissemination and use of data by our public health partners, we developed an online dashboard for real-time monitoring of key indicators (www.cohesionstudy.ca/dashboard). Throughout phase 2 of COHESION, we will continue adapting our survey content with timely themes, helping uncovering key pathways linking individual trajectories, environmental contexts, and health and equity outcomes.
Local adaptations and contributions to public health policies
An important contribution of this project is to offer both a pan-Canadian portrait while allowing local oversampling and providing very contextualized information. An example of local adaptation is planned for public health territory of CIUSSS Nord-de-l’Île-de-Montréal (NIM) in Québec [65], with a target local sample of 1,000 participants. Data will be used to support the co-construction of tailored local intersectoral interventions towards mental health and more broadly to support activities towards health equity as part of a longer-term pandemic recovery strategy. While COHESION Study Phase 1 aimed to understand the mechanisms linking residential living conditions (built environment, surrounding greenness, neighborhood deprivation) to differential trajectories of mental health and well-being since the outbreak of the pandemic, Phase 2 is designed to offer decision support for public health authorities across Canada in varying context, including the pandemic recovery period. This period presents a valuable opportunity to apply the lessons learned from the peak of the pandemic and to examine how the social and physical environments continue to influence mental health in a post-pandemic context. By conducting our study across two distinct phases, we aim to capture a comprehensive understanding of these relationships in different pandemic contexts. This contextualized information on a potential representative sample of general population would be particularly important for policy makers as they address health inequities related to income, housing, daily mobility and social interactions, intimate partner violence, childhood, access to food and health care, and racism that have been exacerbated over the past two years. Ultimately, our findings will contribute valuable insights to the urban health field and inform future public health interventions.
Limitations
Regarding limitations, our recruitment methods and sample characteristics might compromise generalizability, even though Phase 2 intensified efforts to bolster representativeness. In this phase, we employed quota sampling across Canadian provinces and territories, anchoring our selection to demographics such as age, gender, and education. This aimed to align our results more closely with the national population’s makeup. Moreover, using elements from standardized tools, while tailored to ease participant burden and refine assessments, may bring potential uncertainties. However, we commit to thoroughly assessing the reliability and validity of these measures during our data analysis phase, striving for robust conclusions. Furthermore, our method of collecting pre-pandemic mental health data, while providing essential comparative value, might not fully portray our participants’ pre-pandemic mental health scenarios.
Transitioning from these lessons, Phase 2 includes refined strategies in response to our Phase 1 experiences, particularly the challenges posed by the mandatory VERITAS-Social data collection. In COHESION 2.0, we have adapted by making VERITAS optional. This adaptation enables us to strike a balance. While numerous studies predominantly zero in on residential determinants, we envisage a broader canvas – capturing the intricacies of individual activities and the wider environmental influences. This approach, naturally, poses its representativeness challenges, but we remain vigilant and proactive in addressing them.
Conclusions
Recognizing the interconnected nature of various factors impacting mental health, real-time monitoring and evaluation of the unintended consequences on mental health and health inequities of the pandemic is essential for shaping and adapting effective public health policies and programs targeting contextual living conditions (e.g., pedestrianization of streets, securing access to parks, housing renovation programs, permanent supportive housing programs, neighborhood greening program) [32, 66]. We will benefit from the support of the Uni-Cité Collaboratory [67] which specializes in science-to-policy approaches – to equip research teams and cities with tools for better incorporation of scientific findings into urban public policy. Our study aims to provide valuable insights into the key pathways of the COVID-19 impacts on mental health and well-being across Canada while acknowledging potential limitations. Our flexible infrastructure ensures adaptability to local needs and the evolving situation as we transition from the pandemic to the post-pandemic recovery period, ultimately contributing to informed public health interventions.
Supplementary Information
Additional file 1: Table S1. Participation in the COHESION Study Phase 1 throughout the first year of prospective follow-up (June 2020 to July 2021): detailed statistics (N = 1,268). Table S2a. To be continued. Table S2b. Comparison of participants enrolling or not in the prospective follow-up according to residential social and environmental measures (N = 1,268). Table S3a. Participation to the thematic questionnaire modules on well-being, sleep credit, and loneliness in the COHESION Study Phase 1 throughout the first year of prospective follow-up (June 2020 to July 2021, N= 1,268). Table S3b. Participation to the thematic questionnaire modules on anxiety symptoms, depression symptoms, and psychological distress in the COHESION Study Phase 1 throughout the first year of prospective follow-up (June 2020 to July 2021, N = 1,268). a I.e., headcount and percentage of participants having completed at least the corresponding number of follow-ups. Table S4a. WHO-5 Index, sleep duration, and UCLA 3-item loneliness score throughout the first year of prospective follow-up of the COHESION Study Phase 1: detailed statistics. Table S4b. GAD-7 score, PHQ-9 score, and Kessler-6 score throughout the first year of prospective follow-up of the COHESION Study Phase 1: detailed statistics. Figure S1a. Collecting data on each activity place with VERITAS-Social. There is the example of a fictional participant. Screenshot from the VERITAS application (map-based survey tool – permission given from Polygon Inc.). Figure S1b. Identifying people related to each activity place with VERITAS-Social. There is the example of a fictional participant. Figure S2. Examples of Ecological Momentary Assessment (EMA) questionnaires proposed by Ethica Data mobile application.
Acknowledgements
The authors would like to warmly thank Dre. Kate Zinszer (Centre de Recherche en Santé Publique, Montreal, QC, Canada) for her crucial involvement in the foundation of this project; Dr. Margaret De Groh for securing the funds from PHAC; Alexandra Otis (CIUSSS Nord-de-l’Ile-de-Montréal, Montreal, QC, Canada) and Marina Najjar (Centre de Recherche en Santé Publique, Montreal, QC, Canada) for their decisive coordination work in the Phase 1 COHESION study; Alexie Kim, Salma Sahil, and Andréanne Fortin for their assistance in study’s communication; Alexandre Naud for his help with the VERITAS questionnaire; and Catherine Grenon for her help in analyzing the verbatims of the completed surveys. NDVI and MSDI metrics, indexed to DMTI Spatial Inc. postal codes, were provided by the Canadian Urban Environmental Health Research Consortium (CANUE).
Abbreviations
- COHESION
COVID-19: HEalth and Social Inequities across Neighbourhoods
Authors' contributions
GM and YK contributed to the study conception. SG performed data analyses. GM, YK and BT performed the project administration. GM, YK and BT supervised data collection. SG wrote the initial draft of the manuscript. GM, YK, BT, RW, GS, CH, LL, ED and BN did critical review and revision of the draft. GM and YK supervised the research project. GM and YK obtained funding for the study.
Funding
The COHESION Study is supported by the Public Health Agency of Canada (PHAC, Ref # 4500416825–450041483) and the Fonds de Recherche du Québec en Santé (FRQ-S) and the Ministère de l’Économie et de l’Innovation du Québec (Ref # 52266), and has benefited from infrastructure support from the Canadian Foundation for Innovation (CFI, Ref # 41072). These governmental organizations were not involved in the study design, data collection, or decision to publish this manuscript. The content and views expressed in this article are those of the authors and do not necessarily reflect these organizations.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available because they contain highly detailed individual location data about participants, but are available from the corresponding author on request. Sharing of location data will also require ethics approval from the requesting author’s institution.
Declarations
Ethics approval and consent to participate
Before completing the eligibility questionnaire, potential participants are first invited to read the consent form and provide an electronic written consent to participate in the study. Informed consent was obtained from all the participants and/or their legal guardians. In Phase 2, a second consent will be required from participant wishing to register for the prospective follow-ups after having completed baseline questionnaire. Phase 1 COHESION was approved by the ethics board of the Centre de Recherche du Centre Hospitalier de l’Université de Montréal (CRCHUM; MP-02-2021-8924) and by the Public Health Agency of Canada (PHAC) ethical review board (REB 2020-016P). Phase 2 COHESION was approved by both the ethics board of the Centre Intégré Universitaire de Santé et de Services Sociaux du Nord-de-l’Île-de-Montréal (CIUSSS-NIM ; 2022–2327) and PHAC (REB 2020-016P).
Consent for publication
Not applicable.
Competing interests
YK holds shares in Polygon Research Inc., the data collection platform that is used for the COHESION study. Other authors have no competing interests to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Rolling updates on coronavirus disease (COVID-19). 2020 [cited 25 Aug 2021]. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.
- 2.Government of Canada. COVID-19 daily epidemiology update. 2021 [cited 25 Aug 2021]. Available: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html.
- 3.Bernier C-A, Boire-Schwab D, Bélanger C, Castonguay J-S, Fimiani M, Fitz-Simon N et al. COVID-19: Emergency Measures Tracker. 2021 [cited 25 Aug 2021]. Available: https://www.mccarthy.ca/fr/node/63791.
- 4.Statistics Canada. Canadian Economic Dashboard and COVID-19. 2021 [cited 30 Mar 2021]. Available: https://www150.statcan.gc.ca/n1/pub/71-607-x/71-607-x2020009-eng.htm.
- 5.Bruine de Bruin W. Age Differences in COVID-19 Risk Perceptions and Mental Health: Evidence From a National U.S. Survey Conducted in March 2020. Isaacowitz D, editor. The Journals of Gerontology: Series B. 2021;76: e24–e29. 10.1093/geronb/gbaa074. [DOI] [PMC free article] [PubMed]
- 6.Wenham C, Smith J, Morgan R. COVID-19: the gendered impacts of the outbreak. The Lancet. 2020 doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. The Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jenkins EK, McAuliffe C, Hirani S, Richardson C, Thomson KC, McGuinness L, et al. A portrait of the early and differential mental health impacts of the COVID-19 pandemic in Canada: findings from the first wave of a nationally representative cross-sectional survey. Prev Med (Baltim) 2021;145:106333. doi: 10.1016/j.ypmed.2020.106333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The New York Times. The Workers Who Face the Greatest Coronavirus Risk. 2020. https://www.nytimes.com/interactive/2020/03/15/business/economy/coronavirus-worker-risk.html.
- 10.Chen JT, Krieger N. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US county versus zip code analyses. J Public Health Manage Pract. 2021;27:46–S56. doi: 10.1097/PHH.0000000000001263. [DOI] [PubMed] [Google Scholar]
- 11.Van Lancker W, Parolin Z. COVID-19, school closures, and child poverty: a social crisis in the making. The Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yancy CW. COVID-19 and African americans. JAMA - Journal of the American Medical Association. 2020 doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 13.Pareek M, Bangash MN, Pareek N, Pan D, Sze S, Minhas JS, et al. Ethnicity and COVID-19: an urgent public health research priority. The Lancet. 2020 doi: 10.1016/S0140-6736(20)30922-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Samuelsson K, Barthel S, Colding J, Macassa G. Urban nature as a source of resilience during social distancing amidst the coronavirus pandemic. 2020. 10.31219/osf.io/3wx5a.
- 15.Varshney LR, Socher R. COVID-19 Growth Rate Decreases with Social Capital. 2020. 10.1101/2020.04.23.20077321.
- 16.Courtet P, Olie E, Debien C, Vaiva G. Keep socially (but not physically) connected and carry on: preventing Suicide in the age of COVID-19. J Clin Psychiatry. 2020 doi: 10.4088/JCP.20com13370. [DOI] [PubMed] [Google Scholar]
- 17.Monteith LL, Holliday R, Brown TL, Brenner LA, Mohatt NV. Preventing Suicide in Rural Communities During the COVID-19 Pandemic. Journal of Rural Health. Blackwell Publishing Ltd; 2021. pp. 179–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dawkins G. Mental health survey shows manitobans feeling more anxious due to social isolation. Winn Sun. 2020. https://winnipegsun.com/news/news-news/mental-health-survey-shows-manitobans-feeling-more-anxious-due-to-social-isolation.
- 19.Mcmaster G. Why COVID-19 loneliness can be especially hard on teens. 2020. https://www.ualberta.ca/folio/2020/05/why-covid-19-loneliness-can-be-especially-hard-on-teens.html.
- 20.Vallée J, Cadot E, Roustit C, Parizot I, Chauvin P. The role of daily mobility in mental health inequalities: the interactive influence of activity space and neighbourhood of residence on depression. Soc Sci Med. 2011;73:1133–44. doi: 10.1016/j.socscimed.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 21.Chung MH, Leung SF, Välimäki M. Use of tracking technology to examine life-space mobility among people with depression: a systematic review protocol. BMJ Open. 2020;10:e034208. doi: 10.1136/bmjopen-2019-034208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Astell-Burt T, Feng X, Kolt GS. Does access to neighbourhood green space promote a healthy duration of sleep? Novel findings from a cross-sectional study of 259 319 australians. BMJ Open. 2013;3:e003094. doi: 10.1136/bmjopen-2013-003094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Public Health Agency of Canada. The Chief Public Health Officer’s Report on the State of Public Health in Canada 2017 – Designing Healthy Living. 2017. https://www.canada.ca/en/public-health/services/publications/chief-public-health-officer-reports-state-public-health-canada/2017-designing-healthy-living.html.
- 24.Abedi V, Olulana O, Avula V, Chaudhary D, Khan A, Shahjouei S, et al. Racial, economic, and Health Inequality and COVID-19 Infection in the United States. J Racial Ethn Health Disparities. 2021;8:732–42. doi: 10.1007/s40615-020-00833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Turcotte M, Hango D. Incidence des conséquences économiques de la COVID-19 sur les préoccupations sociales des Canadiens. 2020. https://publications.gc.ca/site/fra/9.887808/publication.html.
- 26.Pevalin DJ, Reeves A, Baker E, Bentley R. The impact of persistent poor housing conditions on mental health: a longitudinal population-based study. Prev Med (Baltim). 2017;105. 10.1016/j.ypmed.2017.09.020. [DOI] [PubMed]
- 27.Schellenberg G, Fonberg J. Housing characteristics and staying at home during the COVID-19 pandemic. 2020. https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00009-eng.htm.
- 28.Deaton J, Deaton B. Food security and Canada’s agricultural system challenged by COVID-19. Can J Agric Econ. 2020;68. 10.1111/cjag.12227.
- 29.Loopstra R. Vulnerability to food insecurity since the COVID-19 lockdown. 2020. https://api.semanticscholar.org/CorpusID:216094696.
- 30.Rotermann M. Canadians who report lower self-perceived mental health during the COVID-19 pandemic more likely to report increased use of cannabis, alcohol and tobacco. 2020. https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00008-eng.htm.
- 31.Wasfi R, Kestens Y. Built environment and health. Urban Form and Accessibility. Elsevier; 2021. pp. 187–205. [Google Scholar]
- 32.Housing. and Social Inequalities in Health in Times of COVID-19: Strategies for Promoting Affordable Quality Housing | INSPQ. [cited 20 Apr 2023]. Available: https://www.inspq.qc.ca/en/publications/3152-housing-social-ineqaulitiies-health-covid-19.
- 33.Wasfi R, Poirier Stephens Z, Sones M, Laberee K, Pugh C, Fuller D, et al. Recruiting Participants for Population Health Intervention Research: effectiveness and costs of recruitment methods for the INTERACT (INTErventions, Research, and Action in Cities Team) study. J Med Internet Res. 2021 doi: 10.2196/21142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Turner-Bowker D, Hogue SJ. Short form 12 Health Survey (SF-12). Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer Netherlands; 2014. pp. 5954–7. [Google Scholar]
- 35.Bech P. Measuring the dimension of psychological general well-being by the WHO-5. In: Quality of life newsletter. 2004.
- 36.Smyth C. The Pittsburgh Sleep Quality Index (PSQI) J Gerontol Nurs. 1999;25:10–0. doi: 10.3928/0098-9134-19991201-10. [DOI] [PubMed] [Google Scholar]
- 37.Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, et al. Screening for serious mental Illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19:4–22. doi: 10.1002/mpr.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- 39.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166. 10.1001/archinte.166.10.1092. [DOI] [PubMed]
- 40.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16. 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed]
- 41.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15:194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 42.Statistics Canada. Canadian Community Health Survey (CCHS) - Mental Health. [cited 1 May 2020]. Available: https://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=assembleInstr&a=1&〈=en&Item_Id=119788.
- 43.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10:141–6. [PubMed] [Google Scholar]
- 44.Canadian Income Survey. – 2019 Questionnaire [Unmet health care needs module]. [cited 16 Mar 2022]. Available: https://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=assembleInstr&a=1&〈=en&Item_Id=1270841.
- 45.Office of Nutrition Policy and Promotion, Health Products and Food Branch. Canadian Community Health Survey, Cycle 2.2, Nutrition (2004) - Income-Related Household Food Security in Canada. Ottawa, CA; 2007.
- 46.Naud A, Sueur C, Basile C, Kestens Y. Combining social network and activity space data for health research: tools and methods. Health Place. 2020;66:102454. doi: 10.1016/j.healthplace.2020.102454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chaix B, Kestens Y, Perchoux C, Karusisi N, Merlo J, Labadi K. An interactive mapping tool to assess individual mobility patterns in neighborhood studies. Am J Prev Med. 2012;43. 10.1016/j.amepre.2012.06.026. [DOI] [PubMed]
- 48.Campbell KE, Lee BA. Name generators in surveys of personal networks. Soc Networks. 1991;13:203–21. doi: 10.1016/0378-8733(91)90006-F. [DOI] [Google Scholar]
- 49.Fuller D, Bell S, Firth CL, Muhajarine N, Nelson T, Stanley K, et al. Wave 1 results of the INTerventions, Research, and Action in cities Team (INTERACT) cohort study: examining spatio-temporal measures for urban environments and health. Health Place. 2021 doi: 10.1016/j.healthplace.2021.102646. [DOI] [PubMed] [Google Scholar]
- 50.Qian W. 0000-0001-8580-5235. Transmission Modeling with Smartphone-based Sensing. 2022 [cited 20 Apr 2023]. Available: https://harvest.usask.ca/handle/10388/14060.
- 51.Wilhelm P, Schoebi D. Assessing Mood in Daily Life. Eur J Psychol Assess. 2007;23:258–67. doi: 10.1027/1015-5759.23.4.258. [DOI] [Google Scholar]
- 52.Pampalon R, Hamel D, Gamache P, Philibert MD, Raymond G, Simpson A. An area-based Material and Social Deprivation Index for Public Health in Québec and Canada. Can J Public Health. 2012;103:17–S22. doi: 10.1007/BF03403824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Statistics Canada. Population centre size class values by province and territory., 2016 Census. [cited 2 Aug 2021]. Available: https://www12.statcan.gc.ca/census-recensement/2016/ref/dict/tab/t1_13-eng.cfm.
- 54.Gorelick N, Hancher M, Dixon M, Ilyushchenko S, Thau D, Moore R. Google Earth Engine: planetary-scale geospatial analysis for everyone. Remote Sens Environ. 2017;202:18–27. doi: 10.1016/j.rse.2017.06.031. [DOI] [Google Scholar]
- 55.Google Earth Engine. USGS Landsat 8 TOA Reflectance (Orthorectified) – 2013 to 2017. 2017. Available: https://explorer.earthengine.google.com/detail/LANDSAT/LC8_L1T_TOA.
- 56.Herrmann T, Gleckner W, Wasfi RA, Thierry B, Kestens Y, Ross NA. A pan-canadian measure of active living environments using open data. Health Rep. 2019;30. 10.25318/82-003-x201900500002-eng. [DOI] [PubMed]
- 57.Canadian Institute for Health Information. COVID-19 Intervention Timeline in Canada. 2021. [cited 3 Aug 2021]. Available: https://www.cihi.ca/en/covid-19-intervention-timeline-in-canada.
- 58.Fields E. Tableau Online Security in the Cloud. 2021.
- 59.Jacobsen E, Ran X, Liu A, Chang CCH, Ganguli M. Predictors of attrition in a longitudinal population-based study of aging. Int Psychogeriatr. 2021;33:767–78. doi: 10.1017/S1041610220000447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Young AF, Powers JR, Bell SL. Attrition in longitudinal studies: who do you lose? Aust N. Z J Public Health. 2006;30:353–61. doi: 10.1111/J.1467-842X.2006.TB00849.X. [DOI] [PubMed] [Google Scholar]
- 61.CEPPP – Center of Excellence for Patient and Public Partnership. [cited 4 Apr 2022]. Available: https://ceppp.ca/en/.
- 62.Fumagalli L, Laurie H, Lynn P. Experiments with methods to reduce attrition in longitudinal surveys. J R Stat Soc Ser a Stat Soc. 2013;176:499–519. doi: 10.1111/J.1467-985X.2012.01051.X. [DOI] [Google Scholar]
- 63.Wasfi R, Stephens ZP, Sones M, Laberee K, Pugh C, Fuller D, et al. Recruiting Participants for Population Health Intervention Research: effectiveness and costs of recruitment methods for a Cohort Study. J Med Internet Res. 2021;23. 10.2196/21142. [DOI] [PMC free article] [PubMed]
- 64.Hipp L, Bünning M, Munnes S, Sauermann A. Problems and pitfalls of retrospective survey questions in COVID-19 studies. Surv Res Methods. 2020;14:109–14. doi: 10.18148/SRM/2020.V14I2.7741. [DOI] [Google Scholar]
- 65.CIUSSS du Nord. -de-l’île-de-Montréal | Portrait de l’établissement. [cited 4 Apr 2022]. Available: https://www.ciusssnordmtl.ca/a-propos/qui-sommes-nous/portrait-de-letablissement/.
- 66.COVID-19. : Safe Use of Urban Parks and Green Spaces During Gradual Lockdown Lifting | INSPQ. [cited 20 Apr 2023]. Available: https://www.inspq.qc.ca/en/publications/3043.
- 67.Home — Collaboratoire Uni-Cité. [cited 4 Apr 2022]. Available: https://www.uni-cite.ca/home.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Participation in the COHESION Study Phase 1 throughout the first year of prospective follow-up (June 2020 to July 2021): detailed statistics (N = 1,268). Table S2a. To be continued. Table S2b. Comparison of participants enrolling or not in the prospective follow-up according to residential social and environmental measures (N = 1,268). Table S3a. Participation to the thematic questionnaire modules on well-being, sleep credit, and loneliness in the COHESION Study Phase 1 throughout the first year of prospective follow-up (June 2020 to July 2021, N= 1,268). Table S3b. Participation to the thematic questionnaire modules on anxiety symptoms, depression symptoms, and psychological distress in the COHESION Study Phase 1 throughout the first year of prospective follow-up (June 2020 to July 2021, N = 1,268). a I.e., headcount and percentage of participants having completed at least the corresponding number of follow-ups. Table S4a. WHO-5 Index, sleep duration, and UCLA 3-item loneliness score throughout the first year of prospective follow-up of the COHESION Study Phase 1: detailed statistics. Table S4b. GAD-7 score, PHQ-9 score, and Kessler-6 score throughout the first year of prospective follow-up of the COHESION Study Phase 1: detailed statistics. Figure S1a. Collecting data on each activity place with VERITAS-Social. There is the example of a fictional participant. Screenshot from the VERITAS application (map-based survey tool – permission given from Polygon Inc.). Figure S1b. Identifying people related to each activity place with VERITAS-Social. There is the example of a fictional participant. Figure S2. Examples of Ecological Momentary Assessment (EMA) questionnaires proposed by Ethica Data mobile application.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available because they contain highly detailed individual location data about participants, but are available from the corresponding author on request. Sharing of location data will also require ethics approval from the requesting author’s institution.