Abstract
Background
Many patients treated for breast cancer (BC) complain about cognitive difficulties affecting their daily lives. Recently, sleep disturbances and circadian rhythm disruptions have been brought to the fore as potential contributors to cognitive difficulties in patients with BC. Yet, studies on these factors as well as their neural correlates are scarce. The purpose of the ICANSLEEP-1 (Impact of SLEEP disturbances in CANcer) study is to characterize sleep using polysomnography and its relationship with the evolution of cognitive functioning at both the behavioral and the neuroanatomical levels across treatment in BC patients treated or not with adjuvant chemotherapy.
Methods
ICANSLEEP-1 is a longitudinal study including BC patients treated with adjuvant chemotherapy (n = 25) or not treated with adjuvant chemotherapy (n = 25) and healthy controls with no history of BC (n = 25) matched for age (45–65 years old) and education level. The evaluations will take place within 6 weeks after inclusion, before the initiation of chemotherapy (for BC patients who are candidates for chemotherapy) or before the first fraction of radiotherapy (for BC patients with no indication for chemotherapy) and 6 months later (corresponding to 2 weeks after the end of chemotherapy). Episodic memory, executive functions, psychological factors, and quality of life will be assessed with validated neuropsychological tests and self-questionnaires. Sleep quantity and quality will be assessed with polysomnography and circadian rhythms with both actigraphy and saliva cortisol. Grey and white matter volumes, as well as white matter microstructural integrity, will be compared across time between patients and controls and will serve to further investigate the relationship between sleep disturbances and cognitive decline.
Discussion
Our results will help patients and clinicians to better understand sleep disturbances in BC and their relationship with cognitive functioning across treatment. This will aid the identification of more appropriate sleep therapeutic approaches adapted to BC patients. Improving sleep in BC would eventually help limit cognitive deficits and thus improve quality of life during and after treatments.
Trial registration
NCT05414357, registered June 10, 2022.
Protocol version
Version 1.2 dated March 23, 2022.
Keywords: Breast cancer, Adjuvant chemotherapy, Sleep structure, Circadian rhythms, Cognition, White matter integrity
Background
Breast cancer (BC) is the most frequent cancer in women, with 2.26 million cases worldwide in 2020 [1, 2]. Cognitive complaints reported by BC patients [3, 4] have attracted the interest of many researchers, making BC a standard model for studying cognitive decline in non-central nervous system (non-CNS) cancers [5, 6]. These complaints are often reported during and after adjuvant chemotherapy but can also be found before treatment in 20–30% of BC patients [7, 8]. The majority of them refer to memory loss, slowed processing speed, and executive dysfunction [6, 9]. Although subtle in nature, these cognitive difficulties negatively affect the quality of life of BC patients [10, 11] and may persist up to 20 years after chemotherapy [12]. In addition to the effects of treatments, sleep disturbances and circadian rhythm disruptions have been recently brought to the fore as potential contributors to cognitive difficulties in BC patients [13–16]. Sleep is known to play a crucial role in maintaining cognitive functioning, such as episodic memory [17] and executive functioning [18]. However, the association between sleep and cognitive decline in BC still remains largely unknown [14] and thus requires further investigations.
Complaints about troubled sleep before, during, and after chemotherapy are frequent in BC patients, with symptoms of insomnia being the most significant complaint [19, 20]. Moreover, sleep disturbances may be the result of circadian rhythm disruptions that have been highlighted elsewhere in BC patients. Indeed, sleep behavior depends on the interaction of a homeostatic sleep drive with endogenous circadian rhythms [21]. As a side note, both sleep and circadian rhythm disruption have been highlighted before cancer diagnosis and could be predisposing factors for BC incidence, highlighting the need to further identify and address such alterations in BC patients [22–24].
Previous reports have shown alterations of circadian rhythms following chemotherapy, particularly reflected by salivary cortisol profiles and rest-activity rhythms, which are easy to measure and provide reliable information about circadian rhythms. Cortisol is the primary product of the hypothalamic-pituitary-adrenal (HPA) axis [25], and previous reports have shown flattened diurnal cortisol patterns in BC patients following chemotherapy [26, 27]. Moreover, previous studies have shown dysregulation of the rest-activity rhythm using actigraphy in BC patients treated with chemotherapy [28–30]. The results of these studies have shown a lower amplitude of activity levels (difference between the maximum and minimum of the best fitting curve) as well as a lower mesor (the rhythm-adjusted mean of the best fitting curve).
Due to its ease of use, many studies have used actigraphy to assess sleep in BC patients before or during chemotherapy. Some showed a shortened sleep time and more frequent awakenings during chemotherapy compared to the status before the beginning of the treatment [31, 32], whereas others showed no significant difference in terms of frequent awakenings and lower sleep quality before and during chemotherapy [33]. Before chemotherapy, Ancoli-Israel and colleagues [34] showed lower sleep efficiency ([current sleep time/time in bed] × 100) in BC patients while Berger and colleagues [35] showed better sleep efficiency compared to previously established norms. Meanwhile, polysomnography (PSG), the gold-standard method to measure sleep quality and quantity, is rarely used in cancer research [15, 19, 36]. For instance, Silberfab and colleagues [37] did not find any significant difference in sleep patterns between BC patients after chemotherapy and age-matched healthy women. Two studies found sleep structure modifications in BC patients after chemotherapy, notably lower sleep efficiency and higher sleep onset latency [38, 39]. Roscoe and colleagues [36] noted that BC patients slept for longer at the end of chemotherapy than before the start of chemotherapy. Several methodological limitations may have led to these discrepant findings. Although these studies have provided informative results, their main limitation is the lack of control groups. Having a control group of subjects with no history of cancer and even a control group of BC patients without chemotherapy treatment would allow for determining whether sleep modifications are related to cancer per se and/or to chemotherapy. Moreover, the heterogeneity or sample sizes of the groups studied may have also limited the statistical power of the results. New studies are thus needed to further knowledge about sleep modifications in BC patients before and after chemotherapy.
Both sleep quantity and quality are known to contribute to cognitive functioning in both young and old healthy volunteers [18, 40]. Besides characterizing sleep structure, PSG also provides objective quantitative measurements of memory consolidation during sleep through the quantification of sleep spindles (transient 12–15 Hz oscillations generated within thalamocortical loops) and slow waves (cortical < 1 Hz oscillations). Memory consolidation is an active process that integrates newly encoded information into long-term memory networks and is more efficient during sleep [41]. As an example, a reduction in sleep spindle density has been associated with lower memory consolidation in older adults [42–44]. Currently, this topic is rarely addressed in BC patients: only one study has reported a higher spindle frequency and lower slow wave amplitude in BC patients not treated with chemotherapy compared to age-matched healthy women [45]. Given that the link between sleep and cognitive functioning has mostly been assessed using subjective scales and self-report questionnaires in BC [14], new data are required to clarify the relationship between sleep modifications and cognitive deficits in BC patients, both before and after chemotherapy. Moreover, previous reports have shown both white and grey matter alterations in BC patients before and after chemotherapy [46–48]. Given the role of white matter integrity in spindle propagation, as well as the contribution of both white and grey matter alterations in cognitive difficulties in BC patients, one may expect that alterations in grey and white matter could influence both memory consolidation during sleep and cognitive functioning. It is therefore essential to quantify the predictive role of grey and white matter modifications in sleep and its relationship with cognitive functioning. Additionally, some studies have found grey matter reductions among BC patients during and after chemotherapy [49–51] and others have related it to worse neuropsychological performance compared to healthy control groups [52, 53].
In the ICANSLEEP-1 study herein presented, we aim to prospectively assess sleep modifications through PSG among BC patients initiating chemotherapy, as compared to healthy age-matched women and BC patients with no indication to receive chemotherapy.
Methods
The ICANSLEEP-1 study is a single-center longitudinal study where sleep will be prospectively assessed using PSG among three groups: BC patients treated with chemotherapy, BC patients without chemotherapy, and cancer-free women. Self-report questionnaires and neuropsychological tests will be used to assess participants’ complaints and quality of life as well as their cognitive profiles. Rest-activity and cortisol rhythms will be assessed using actigraphy and saliva recollection, respectively. Polysomnography will serve to quantify sleep structure, that is, sleep quantity and quality. Neuropsychological tests will evaluate participants’ cognitive functioning. Structural magnetic resonance imaging (MRI) will be used to quantify both grey and white matter integrities, respectively. The ICANSLEEP-1 protocol and this manuscript have been written in accordance with standard protocol items, following recommendations for interventional trials (SPIRIT).
Study objectives
The main objective is to longitudinally quantify sleep modifications associated with BC and chemotherapy using PSG.
The secondary objectives are to:
Assess the relationship between the presence of sleep disturbances and poor cognitive performance, both before and after chemotherapy.
Quantify the predictive role of white matter integrity alterations in explaining such a relationship.
Determine whether the presence of sleep disturbances is associated with circadian disruptions in BC patients both before and after chemotherapy.
Participants
Three groups of women aged between 45 and 65 years will be recruited: 25 BC patients scheduled to receive adjuvant chemotherapy (CHE), 25 BC patients treated with radiotherapy alone with no indication of chemotherapy (NCH), and 25 healthy female controls (CTL). BC patients in the NCH group will be matched for age and level of education to BC patients from the CHE group. Similarly, the female volunteers enrolled in the CTL group will be matched to BC patients for age and level of education. Both pre- and postmenopausal women will be included, and information regarding menopausal status as well as the date of the beginning of menopause will be collected for all participants.
Eligible BC patients will be asked to participate in the ICANSLEEP-1 study by the medical and/or radiation oncologists. An explanation of the study and an information note will be given to them. Eligibility criteria are indicated in Table 1. Patients will be enrolled in the study once they provide their written informed consent.
Table 1.
ICANSLEEP-1 inclusion and non-inclusion criteria
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Breast cancer patients and Healthy individuals |
Age between 45–65 yo French native speakers At least on level 3 (end of primary schools) of the Barbizet scale Insomnia Sleep Index (ISI > 7) Women who don’t work on night shifts Women who signed the consent form to participate in the study |
Neurological sequelae Personality disorders and progressive psychiatric disorder Drug use and/or heavy drinking Women with contraindication to MRI Women with uncorrected vision problem Women with treated sleep apnea syndrome Women with a treatment that hasn’t been stabilized for at least 3 months (hypnotics, antidepressants, anxiolytics) |
| Healthy individuals | Women with no history of cancer | - |
| Breast cancer patients |
Operated for local breast cancer Treated with adjuvant Chemotherapy +/- Radiotherapy Absence of pre-existing cognitive impairment at cancer diagnosis |
Metastatic cancer |
Healthy volunteers will be recruited from the general population through associations, an advertisement in Centre François Baclesse, or by acquaintance, for example. Eligible women will be asked to participate by the physicians from our laboratory and will receive an information file. Women who meet all eligibility criteria (Table 1) will be asked to sign the consent form to be enrolled in the study.
Study sites
The study will be conducted in the comprehensive cancer center François Baclesse (Caen, France) for BC patients and in our laboratory at Normandie University (Caen, France) for healthy women, as indicated on https://clinicaltrials.gov/ct2/show/NCT05414357.
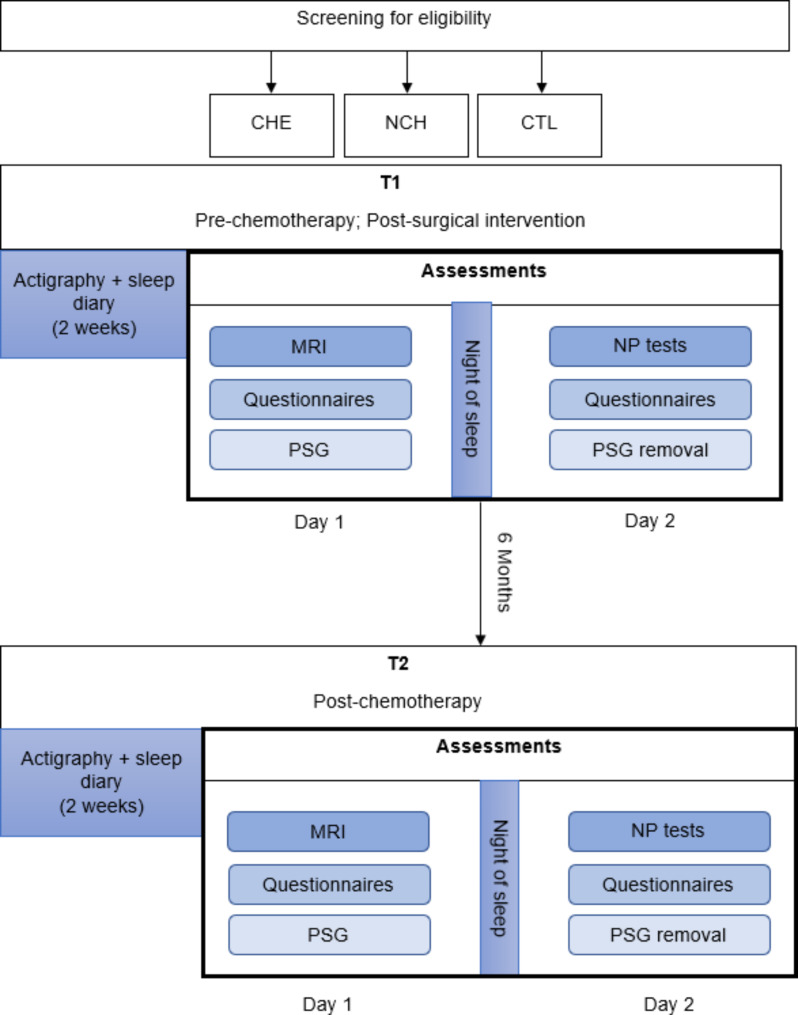
Modalities of participation
The modalities of participation for each of the three groups are summarized in Fig. 1. The overview of study assessments is given in Table 2.
Fig. 1.
ICANSLEEP-1 trial design. CHE: group of patients treated with chemotherapy; NCH: group of patients not treated with chemotherapy; CTL: control group; MRI: magnetic resonance imaging; PSG: polysomnography; NP tests: neuropsychological tests
Table 2.
Questionnaires and neuropsychological test battery included in the ICANSLEEP-1 study with their outcome measures
| Domains | Assessment tests | Outcome measures | Range | Evaluated time frame |
|---|---|---|---|---|
| Sleep Questionnaires | ||||
| Insomnia | ISI | Total Score | 0–28 (> 7) | Over the last two weeks |
| Sleep Quality | PSQI | Total score | 0–21 | Over the last month |
| Circadian Typology | MEQ | Total score | 16–86 | - |
| Quality of Life Questionnaires | ||||
| Cognitive complaint | Fact-Cog | PCI | 0–72 | Over the last seven days |
| PCA | 0–28 | |||
| QoL | 0–16 | |||
| Oth | 0–16 | |||
| Quality of life | FACT-G (patients) | Total score | 0–108 | Over the last seven days |
| Pain | BPI | Severity of pain | 0–10 | Over the last eight days |
| Interference of pain | 0–10 | |||
| Fatigue | FACIT-F (patients) | Total score | 0–52 | Over the last seven days |
| MFI-20 | General and physical fatigue | 9–45 | - | |
| Reduced activity | 3–15 | |||
| Reduced motivation | 2–10 | |||
| Mental fatigue | 6–30 | |||
| Anxiety | STAI-Y | State score | 20–80 | At the time being |
| Trait score | 20–80 | Generally speaking, | ||
| Depression | BDI-II | Total score | 0–63 | Over the last two weeks |
| Neuropsychological tests | ||||
| Global functioning | MoCA | Total Score | 0–30 | |
| Episodic Memory | HVLT | Total free recall score | 0–36 | |
| Delayed recall score | 0–12 | |||
| Working Memory | WMS-III subset of spatial memory | Total number of correct trials forward | 0–16 | |
| Total number of correct trials backward | 0–16 | |||
| Baddeley dual Task | Digit span: number of correct sequences | 3–10 | ||
| Motor Task: number of boxes checked in 2 min | 0–332 | |||
| Dual task: number of correct sequences; number of boxes checked | 0–332 | |||
| Attention | D2-R | Number of target characters processed | 0–513 | |
| E %: [(EO + EC)/PTO] x100 | 0–100 | |||
| Executive Functions | N-Back | Number of correct responses | 0–48 | |
| TMT (A – B) | Time in seconds of part A | ≥ 0s | ||
| Time in seconds part B – A | ≥ 0s | |||
| Stroop | Naming | ≥ 0s | ||
| Reading | ≥ 0s | |||
| Interference Time | ≥ 0s | |||
| Verbal Fluency | Letters P & R | |||
ISI: Insomnia Severity Index, PSQI: Pittsburgh Sleep quality Index, MEQ: Morningness-Eveningness Questionnaire, FACT-COG: Functional Assessment of Cancer Therapy – Cognitive Function, PCI: Perceived Cognitive Impairment, PCA: Perceived Cognitive Abilities, QOL: impact on Quality of Life, Oth: Comments from Others, FACT-G: The Functional Assessment of Cancer Therapy – General, BPI: Brief Pain Inventory, FACIT-F: Functional Assessment of Chronic Illness Therapy – Fatigue, MFI-20: Multidimensional Fatigue Inventory, STAI-Y: State-Trait Anxiety Inventory, BDI-II: Beck’s Depression Inventory-2nd edition, MoCA: Montreal Cognitive Assessment; HVLT: Hopkins Verbal Learning Test; WMS-III: Wechsler Memory Scale – 3rd edition, D2-R: d2 Test of Attention-Revised, E%: percent of Errors, EO: Errors of Omission, EC: Errors of Commission, PTO: Processed Target Objects, TMT: Trail Making Test
Once signed consent is obtained, the inclusion evaluation will aim to assess sleep complaints and sleep apnea. After inclusion, patients from the CHE group will be evaluated in two sessions spaced 6 months apart: before the first administration of adjuvant chemotherapy (baseline or T1) and 2 weeks after the end of adjuvant chemotherapy (T2). The same will apply to patients in the NCH group and healthy controls.
Each session will be conducted over two half-days separated by a night of sleep. On the afternoon of day 1, structural MRI assessments will be realized, and the participants will be asked to complete self-report questionnaires related to psychological factors, after which PSG will be placed to measure sleep patterns during one full night of sleep at home. Self-report questionnaires on quality of sleep and quality of life will be filled in by participants at home. On the morning of day 2, PSG will be removed, and the participants will undergo neuropsychological tests and fill in the other questionnaires.
Assessments tools
An overview of tools to be used in the study is given in Table 2.
Self-reported questionnaires
The Insomnia Severity Index (ISI) [54] is a self-report questionnaire assessing the nature, severity, and impact of insomnia. It evaluates the following dimensions: severity of sleep onset, sleep maintenance, early morning awakening problems, sleep dissatisfaction, interference of sleep difficulties with daytime functioning, noticeability of sleep problems by others, and distress caused by the sleep difficulties. A score ≥ 7 will be considered to indicate the presence of insomnia.
The Berlin questionnaire [55] will be used to assess sleep complaints and sleep apnea factors such as snoring behavior, waketime sleepiness or fatigue, and the presence of obesity or hypertension.
The Pittsburgh Sleep Quality Index (PSQI) [56] is a self-report questionnaire that will be used to assess efficiency and quality of sleep over a 1-month time interval. It measures the following components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. A score > 5 is considered to indicate a significant sleep disturbance.
The Morningness-Eveningness Questionnaire [57] will be used to assess chronotype given that it can influence the ambulatory measurement of rest-activity rhythm in healthy volunteers [58]. The questionnaire contains 19 questions to assess morningness-eveningness. At the end, the sum of the scores will be converted to a 5-point morningness-eveningness scale, with a score of 70–86 meaning that the person is “definitely morning type,” a score of 59–69 meaning that the person is “moderately morning type,” a score of 42–58 meaning that the person is “neither type,” a score of 31–41 meaning “moderately morning type,” and a score of 16–30 meaning “definitely evening type.” The Functional Assessment of Cancer Therapy Cognitive Scale (FACT-Cog) [59] in its French version will be used to assess subjective cognitive complaints and their impact on the quality of life. Memory, attention, concentration, language, and thinking abilities will be assessed with 37 items on a 5-point Likert scale (from 0 = not at all to 4 = very much).
The Functional Assessment of Cancer Therapy – General (FACT-G) [60] will assess general quality of life using 27 items categorized under the following components: physical, social/family, emotional, and functional well-being. The score range is 0–108, noted on a 5-point Likert scale (from 0 = not at all to 4 = very much).
The Brief Pain Inventory (BPI) [61] is a self-assessment pain questionnaire. It evaluates pain intensity on a sensory dimension and the level of interference of pain in the participant’s life. It assesses the following components: pain relief, pain quality, and patient’s perception of the cause of pain. A score of 1–4 = mild pain, 5–6 = moderate pain, and 7–10 = severe pain.
Fatigue will be assessed using the Functional Assessment of Chronic Illness Therapy (FACIT-F) [62] and the Multidimensional Fatigue Inventory (MFI-20) [63]. The first is used in its short form as a 13-item self-report questionnaire that aims to assess participants’ perception of fatigue and how it might affect their daily activities and functioning. All items are noted on a 5-point Likert scale (from 0 = not at all to 4 = very much). The second is also a self-report questionnaire designed to measure five fatigue components (general fatigue, physical fatigue, reduced activity, reduced motivation, and mental fatigue). Each question is noted from 1 = no, it is not true to 5 = yes, it is true. The score ranges from 4 to 20. A higher score indicates greater fatigue. The specificity of this questionnaires is that it can be administered to both healthy controls and BC patients. This will allow us to compare both groups.
The State-Trait Anxiety Inventory for Adults (STAI-Y) [64] will be used to evaluate anxiety. It contains two separate scales to measure the state (where participants describe how they feel in the moment) and the trait (where participants describe how they generally feel) of anxiety. Each scale contains 20 statements. To measure the state of anxiety, the 20 statements evaluate how the subject feels “right now,” while the trait is measured by asking the subject how they feel “generally”. The statements are scored on a 4-point Likert scale from 1 = no to 4 = yes for the state component and from 1 = never to 4 = almost always. The total score for both scales ranges from 20 to 80, with higher scores indicating more severe anxiety.
The Beck’s Depression Inventory (BDI-II) [65] will be used to evaluate depression using a 21-item scale that provides information about the severity and nature of depression in the participants. The items range from 0 = the absence of symptoms to 3 = an intense level. The sum of the score will define the presence and severity of depression. A score of 1–10 = absence of depression, 11–16 = mild mood disturbance, 17–20 = borderline clinical depression, 21–30 = moderate depression, 31–40 = severe depression, and finally, a score over 40 = extreme depression.
Sleep and circadian rhythm assessments
Salivary cortisol to assess diurnal cortisol rhythm
Saliva collection will be performed to measure levels of salivary cortisol, one of the markers of circadian rhythms. The procedure involves inserting a cotton ball into the mouth and soaking it with saliva for 2–3 min, then putting it back into the storage tube. Participants will be invited to perform these saliva extractions at home as follows: before sleep, at awakening, and 30 and 45 min after awakening.
Actigraphy to assess rest-activity rhythm
Two weeks before each assessment time point, participants will place an actigraph MotionWatch® 8, (CamNtech Ltd, UK) on their non-dominant wrist (Fig. 1). Actigraphy will provide information related to parametric and non-parametric measures of rest-activity rhythm, as previously published in BC patients [29, 66, 67]. The actigraphs contain a triaxial sensor detecting acceleration in a 0.01–8 g range. They will set to 30-second epochs to allow sleep parameter analysis (validated using 30-second epochs by the manufacturer) and record light intensity to aid the analysis of sleep episodes. During these 2 weeks, participants will also be asked to fill in a sleep diary that will be used to analyze actigraph data for better accuracy. Participants will subjectively indicate their sleep quality and duration, including hours in bed, sleep quality, number and duration of nocturnal awakenings, and naps and their duration. Moreover, the actigraphs allow the tracking of both the diurnal physical activity and the nighttime activity of participants, given that physical activity could also influence sleep in BC patients and being active or not could influence the results [68, 69].
Polysomnography to assess sleep structure
During the night, sleep will be recorded using ambulatory PSG (Siesta, Compumedics) at home or at the hotel where some participants will stay. Recordings of brain activity using electroencephalography (EEG), eye movements, heart rate, respiratory rate, and oxygen saturation will be performed simultaneously. These measures will offer us quantitative data on sleep onset latency, sleep efficiency, number of nocturnal awakenings after sleep onset, total sleep time, and the relative percentages of sleep stages. Twenty EEG electrodes will be placed on the scalp, over prefrontal (FP1/FP2), frontal (F3/F4/F7/F8/Fz), central (C3/C4/Cz), temporal (T3/T4), parietal (P3/P4/Pz), and occipital (O1/O2) sites, according to the international 10–20 system, using Ag/Au electrodes with a ground and a bi-mastoids reference. The impedance for all electrodes will be kept below 5 kΩ. The hardware EEG filter band pass will be 0.15–121 Hz and the sample rate will be 256 Hz. Two electrodes will be placed above and below the eyes to record eye movements, along with two electrodes on the chin to measure muscle tone. An electrocardiogram will also be recorded by placing two electrodes under each clavicle. To detect potential sleep apneas or hypopneas, thoracic and abdominal belts will be placed to record respiratory movements, a microphone to detect snoring, nasal pressure, nasal and oral thermistors to measure respiratory airflow, and a finger pulse oximeter to measure oxygen saturation. In addition, analyses of spindles and slow waves will be performed using the open-source SpiSOP (www.spisop.org; RRID: SCR_015673) based on MATLAB 2017b (MathWorks, Natick, USA; RRID: SCR_001622). For this work, the standard settings of SpiSOP will be used based on previously published algorithms [70]; SpiSOP documentation is available here: www.spisop.org/documentation/.
Neuropsychological test Battery
Global cognitive functioning will be assessed with the Montreal Cognitive Assessment (MoCA) [71] at baseline only (T1). During each session, cognition will be assessed for all participants using standardized neuropsychological tests, all while accounting for the test-retest effect (Table 2). Episodic memory will be assessed using the Hopkins Verbal Learning Test (HVLT) [72], standardized and adapted for French populations. Working memory will be assessed using the subtest of Spatial Memory forward and backward (Wechsler Memory Scale-III) and by the dual task of Baddeley [73]. Attention will be assessed using d2-R [74]. Finally, executive function will be assessed by the Stroop test [75], the Trail Making Test (B-A) [64], lexical fluency (letters P & R) [76], and by a modified version of the N-Back task specifically developed for the AGING protocol [77]. Sleep-dependent memory consolidation will be evaluated using a computer-based memory task performed both before and after sleep (i.e., learning in the afternoon and recall the next morning) in order to measure associated grapho-elements [78].
Brain structural magnetic resonance imaging assessments
Structural MRI will be obtained using a 3T GE (Signa Premier). The whole procedure will be described to all participants before beginning the acquisitions. Volumetric T1-weighted images will be acquired at a 1 mm3 isotropic resolution to measure grey matter density and volume using a three-dimensional (3D) fast field echo sequence (sagittal acquisition; repetition time, 2.2 s; echo time, 2.7 ms; flip angle, 8°; 180 slices; slice thickness, 1 mm; matrix size, 256 × 256). Then, diffusion tensor imaging (DTI) (2D) will be used to measure white matter microstructural integrity (128 directions, multi-shell; repetition time, 4.8 s; echo time, 71 ms; flip angle, 90°; slice thickness, 2 mm; matrix size, 108 × 108). Moreover, a T2-FLAIR (2D) will be acquired to make sure that the participants do not have any brain lesions (axial; repetition time, 8.5 s; echo time, 90 ms; inversion time, 2.4 s; flip angle, 160°; slice thickness, 4 mm).
Statistical considerations
This study was designed to control an error risk α of 0.05 and a power of 80%. Assuming sleep alterations for 30% of patients following chemotherapy compared to a theoretical proportion of 10% [31], the required sample size is 24 patients per group. We thus planned to enroll a total of 75 participants (25 BC patients receiving chemotherapy, 25 BC patients without an indication for chemotherapy, and 25 healthy women).
Statistical analyses will be performed using R® software. Exploratory data analyses will provide, for qualitative variables, the frequencies and their exact 95% confidence intervals, and for quantitative variables, the mean, the standard deviation of the mean, the median, and the quartiles.
Repeated measures analyses of variance (ANOVA) will be applied to longitudinally compare BC patients and healthy controls, with p < 0.05. The relationship between sleep parameters and scores on cognitive tests and quality of life assessments will be assessed at any time using a linear mixed model (accounting for the correlation between repeated measures of the same subject). SPM12 software (https://www.fil.ion.ucl.ac.uk/spm/software/spm12) will be used to assure a whole-brain voxel-based analysis and FSL 6.0.5 software will be used to preprocess white matter data (https://fsl.fmrib.ox.ac.uk/fsl/fslwiki). The relationships between white matter integrity, sleep parameters, and scores on cognitive tests will be assessed at any time using a linear mixed model (considering the correlation between repeated measures of the same subject). Similarly, relationships between sleep disturbances and circadian disruptions will be assessed at any time using a linear mixed model.
Data management
A web-based data capture (WBDC) system will be used for data collection and query handling. The investigator will ensure that data are recorded on the eCRFs as specified in the study protocol and in accordance with the instructions provided.
The investigator ensures the accuracy, completeness, and timeliness of the data recorded and of the provision of answers to data queries according to the Clinical Study Agreement. The investigator will sign the completed eCRFs. A copy of the completed eCRFs will be archived at the study site [79].
Withdrawal from study
The reasons a participant may discontinue participation in the study include the following circumstances:
Intercurrent event, not compatible with the pursuit of the study.
Woman’s decision (the data already collected during the search can be kept and exploited unless she opposes it).
Participant lost of view.
Investigator’s decision.
Discussion
Recent research in BC patients has associated the presence of cognitive deficits with the occurrence of sleep complaints [80–82] but the findings remain inconclusive [14] and further investigations on this topic are needed.
Although sleep disturbances are thought to be a side effect of cancer treatment, notably chemotherapy [13, 83], multiple studies showed that sleep complaints in BC exist even in BC patients who did not receive chemotherapy [84, 85] and their presence has detrimental effects on patients’ quality of life [86]. Sleep is intrinsically linked to circadian rhythms and a recent review highlighted the presence of circadian disruptions in BC, more specifically of cortisol and rest-activity rhythms [13]. These disruptions are, in most cases, associated with chemotherapy in this disease but were also found outside chemotherapy [67] and may contribute to the development and persistence of sleep disturbances—among other symptoms—leading many women with BC to complain about their quality of sleep [83, 87].
Longitudinal studies comparing sleep disturbances in BC patients before and after receiving chemotherapy are thus needed to better understand their influence on cognitive functioning in this pathology. Thus, our study is designed to assess sleep before and after adjuvant chemotherapy using PSG in BC patients treated or not with adjuvant chemotherapy compared to healthy controls. The use of PSG will bring us deeper knowledge of sleep structures (i.e., sleep stages, quality, and quantity) as well as memory consolidation processes during sleep using EEG-derived indices. In addition, PSG will allow us to assess sleep apnea in all participants [45]. Moreover, using DTI, we will be able to provide information related to white matter integrity and its association with both sleep disturbances and memory deficits [88–90].
Accordingly, the characterization of sleep disturbances as contributors to cognitive decline in BC will increase awareness among clinicians to focus on these underdiagnosed symptoms, leading to the development of more appropriate interventions. Improving sleep in BC will lead to the enhancement of patients’ cognitive functioning and possibly their daily lives. A better understanding of sleep disturbances in BC will pave the way for future studies dedicated to improving both sleep and cognitive functioning in BC patients. For now, previous reports have shown the beneficial effects of cognitive behavioral therapy and physical activity on sleep complaints, self-esteem, and quality of life [69, 91].
This study has some limitations. For example, participants may be uncomfortable in the MRI machine due to the narrow space and acoustic noise, which will be reduced using methods such as the passive absorption of acoustic noise by earplugs and helmets. Time will also be dedicated to installing participants comfortably and explaining the MRI protocol to reduce stress in the machine. PSG installation could also bother participants. However, our experience has shown that participants accept PSG well, especially because it will be implemented in ambulatory form at the participant’s home for most participants. Measuring sleep in a familiar environment can help reduce the bother and anxiety caused by PSG examination, as well as the first-night effect.
Conclusion
Using a longitudinal approach, the ICANSLEEP-1 study is expected to provide information on sleep structure modifications in BC patients both before and after chemotherapy. Thanks to the objective evaluation of sleep together with measures of two circadian rhythms, associated with a neuropsychological test battery and structural MRI acquisition, this study is intended to generate advanced knowledge on the altered sleep processes in BC and their impact on cognition and cerebral structures. In the long term, we expect that our results will be useful to both patients and clinicians, allowing a better understanding of patient complaints and thus improving their supportive care and quality of life.
Acknowledgements
Not applicable.
Abbreviations
- BC
breast cancer
- PSG
polysomnography
- EEG
electroencephalography
- MRI
magnetic resonance imaging
- DTI
diffusion tensor imaging
- CNS
central nervous system
- HPA
hypothalamic-pituitary-adrenal
Author Contributions
CE drafted and edited the manuscript. JP, FJ, BG, GQ and FE conceptualized the ICANSLEEP-1 trial. LdG and JP wrote the protocol for ethical approval. CE, MG, BG and FE edited the protocol for ethical approval. LdG, SR, PC, FD, OE, TM contributed to trial design (respectively neuropsychological and sleep parts). SS, ND, MN contributed towards the neuroimaging designs. JL contributed to the formulation of the analytical plan of the design. JMG, and BC performed the administrative procedures. CSD and FV are the medical referents for the protocol and will include patients and controls.
Funding
This work is supported by the Normandie Region, within the framework of a RIN Research 2020 “Chair of Excellence,” doctoral funding from the Ecole Doctorale N° 556 – HSRT (Homme, Sociétés, Risque, Territoire), and the Fondation ARC pour la recherche sur le cancer.
Data Availability
Not applicable.
Declarations
Ethics approval and consent to participate
This study has received ethical approval from the ethics committee of Comité de Protection des Personnes Ile de France IV on 19th of April 2022 (N° ID-RCB: 2022-A00437-36). Eligible patients will be asked to participate by the medical and/or radiation oncologists, and eligible women free of disease will be asked to participate by the physicians from the U1077 University team. All eligible participants (patients and healthy women) will receive an information file. All participants will give their informed consent before any study-related assessment starts. All methods will be performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ferlay J, Colombet M, Soerjomataram I, Parkin DM, Piñeros M, Znaor A, et al. Cancer statistics for the year 2020: An overview. Int J Cancer. 15 août 2021;149(4):778–89. [DOI] [PubMed]
- 2.International Agency for Research on Cancer 2023, from https://gco.iarc.fr/today/online-analysis-multi-bars
- 3.Boykoff N, Moieni M, Subramanian SK. Confronting chemobrain: an in-depth look at survivors’ reports of impact on work, social networks, and health care response. J Cancer Surviv. 2009;3(4):223–32. doi: 10.1007/s11764-009-0098-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lange M, Licaj I, Clarisse B, Humbert X, Grellard J, Tron L et al. Cognitive complaints in cancer survivors and expectations for support: Results from a web–based survey. Cancer Med. 18 mars 2019;8(5):2654–63. [DOI] [PMC free article] [PubMed]
- 5.Giffard B, Lange M, Léger I. Les troubles cognitifs légers liés Au cancer: comment Et à quelles fins les évaluer en consultation neuropsychologique ? Rev Neuropsychol. 2015;7(2):127. [Google Scholar]
- 6.Wefel JS, Kesler SR, Noll KR, Schagen SB. Clinical characteristics, pathophysiology, and management of noncentral nervous system cancer-related cognitive impairment in adults: Cancer-related cognitive impairment. CA Cancer J Clin mars. 2015;65(2):123–38. doi: 10.3322/caac.21258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahles TA, Saykin AJ, McDonald BC, Furstenberg CT, Cole BF, Hanscom BS, et al. Cognitive function in Breast cancer patients prior to adjuvant treatment. Breast Cancer Res Treat Juill. 2008;110(1):143–52. doi: 10.1007/s10549-007-9686-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wefel JS, Lenzi R, Theriault R, Buzdar AU, Cruickshank S, Meyers CA. Chemobrain’ in breast carcinoma? Cancer. 2004;101(3):466–75. doi: 10.1002/cncr.20393. [DOI] [PubMed] [Google Scholar]
- 9.Janelsins MC, Kesler SR, Ahles TA, Morrow GR. Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int Rev Psychiatry févr. 2014;26(1):102–13. doi: 10.3109/09540261.2013.864260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hurria A, Goldfarb S, Rosen C, Holland J, Zuckerman E, Lachs MS, et al. Effect of adjuvant Breast cancer chemotherapy on cognitive function from the older patient’s perspective. Breast Cancer Res Treat août. 2006;98(3):343–8. doi: 10.1007/s10549-006-9171-6. [DOI] [PubMed] [Google Scholar]
- 11.Lange M, Heutte N, Noal S, Rigal O, Kurtz J, Lévy C, et al. Cognitive changes after adjuvant treatment in older adults with early-stage Breast Cancer. The Oncologist janv. 2019;24(1):62–8. doi: 10.1634/theoncologist.2017-0570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koppelmans V, Breteler MMB, Boogerd W, Seynaeve C, Gundy C, Schagen SB. Neuropsychological performance in survivors of Breast Cancer more than 20 years after adjuvant chemotherapy. J Clin Oncol 1 avr. 2012;30(10):1080–6. doi: 10.1200/JCO.2011.37.0189. [DOI] [PubMed] [Google Scholar]
- 13.Amidi A, Wu LM. Circadian disruption and cancer- and treatment-related symptoms. Front Oncol 28 oct. 2022;12:1009064. doi: 10.3389/fonc.2022.1009064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duivon M, Giffard B, Desgranges B, Perrier J. Are Sleep complaints related to cognitive functioning in non-central nervous System Cancer? A systematic review. Neuropsychol Rev [Internet] 5 août 2021 [cité 30 nov 2021]; Disponible sur: https://link.springer.com/10.1007/s11065-021-09521-4. [DOI] [PubMed]
- 15.Perrier J, Duivon M, Rauchs G, Giffard B. Le Sommeil dans les cancers non cérébraux: revue de la littérature, mécanismes potentiels et perspectives pour mieux comprendre les troubles cognitifs associés. Médecine Sommeil juin. 2021;18(2):90–103. doi: 10.1016/j.msom.2020.12.002. [DOI] [Google Scholar]
- 16.Ancoli-Israel S, Liu L, Natarajan L, Rissling M, Neikrug AB, Youngstedt SD, Mills PJ, Sadler GR, Dimsdale JE, Parker BA, Palmer BW. Reductions in sleep quality and circadian activity rhythmicity predict longitudinal changes in objective and subjective cognitive functioning in women treated for Breast cancer. Supportive care in cancer: Official Journal of the Multinational Association of Supportive Care in Cancer. 2022;30(4):3187–200. doi: 10.1007/s00520-021-06743-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diekelmann S, Born J. The memory function of sleep. Nat Rev Neurosci févr. 2010;11(2):114–26. doi: 10.1038/nrn2762. [DOI] [PubMed] [Google Scholar]
- 18.Wilckens KA, Woo SG, Kirk AR, Erickson KI, Wheeler ME. The role of sleep continuity and total sleep time in executive function across the adult lifespan. Psychol Aging Sept. 2014;29(3):658–65. doi: 10.1037/a0037234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Costa AR, Fontes F, Pereira S, Gonçalves M, Azevedo A, Lunet N. Impact of Breast cancer treatments on sleep disturbances – A systematic review. The Breast déc. 2014;23(6):697–709. doi: 10.1016/j.breast.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Savard J, Ivers H, Villa J, Caplette-Gingras A, Morin CM. Natural course of Insomnia Comorbid with Cancer: an 18-Month Longitudinal Study. J Clin Oncol 10 sept. 2011;29(26):3580–6. doi: 10.1200/JCO.2010.33.2247. [DOI] [PubMed] [Google Scholar]
- 21.Deboer T. Sleep homeostasis and the circadian clock: do the circadian pacemaker and the sleep homeostat influence each other’s functioning? Neurobiol Sleep Circadian Rhythms 1 mars. 2018;5:68–77. doi: 10.1016/j.nbscr.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Montaruli A, Castelli L, Mulè A, Scurati R, Esposito F, Galasso L, et al. Biological Rhythm and Chronotype: New perspectives in Health. Biomolecules Avr. 2021;11(4):487. doi: 10.3390/biom11040487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mogavero MP, DelRosso LM, Fanfulla F, Bruni O, Ferri R. Sleep disorders and cancer: state of the art and future perspectives. Sleep Med Rev 1 avr. 2021;56:101409. doi: 10.1016/j.smrv.2020.101409. [DOI] [PubMed] [Google Scholar]
- 24.Samuelsson LB, Bovbjerg DH, Roecklein KA, Hall MH. Sleep and circadian disruption and incident Breast cancer risk: an evidence-based and theoretical review. Neurosci Biobehav Rev janv. 2018;84:35–48. doi: 10.1016/j.neubiorev.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adam EK, Quinn ME, Tavernier R, McQuillan MT, Dahlke KA, Gilbert KE. Diurnal Cortisol Slopes and Mental and Physical Health outcomes:a systematic review and Meta-analysis. Psychoneuroendocrinology sept. 2017;83:25–41. doi: 10.1016/j.psyneuen.2017.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abercrombie HC, Giese-Davis J, Sephton S, Epel ES, Turner-Cobb JM, Spiegel D. Flattened cortisol rhythms in metastatic Breast cancer patients. Psychoneuroendocrinology sept. 2004;29(8):1082–92. doi: 10.1016/j.psyneuen.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 27.Hsiao FH, Jow GM, Kuo WH, Wang MY, Chang KJ, Lai YM, et al. A longitudinal study of diurnal cortisol patterns and associated factors in Breast cancer patients from the transition stage of the end of active cancer treatment to post-treatment survivorship. The Breast déc. 2017;36:96–101. doi: 10.1016/j.breast.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 28.Liu L, Rissling M, Neikrug A, Fiorentino L, Natarajan L, Faierman M, et al. Fatigue and circadian activity rhythms in Breast Cancer patients before and after chemotherapy: a controlled study. Fatigue Abingdon Eng Print. 2013;1(1–2):12–26. doi: 10.1080/21641846.2012.741782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roveda E, Bruno E, Galasso L, Mulè A, Castelli L, Villarini A, et al. Rest-activity circadian rhythm in Breast cancer survivors at 5 years after the primary diagnosis. Chronobiol Int 3 août. 2019;36(8):1156–65. doi: 10.1080/07420528.2019.1621330. [DOI] [PubMed] [Google Scholar]
- 30.Savard J, Liu L, Natarajan L, Rissling MB, Neikrug AB, He F, et al. Breast Cancer patients have progressively impaired sleep-wake activity rhythms during chemotherapy. Sleep 1 sept. 2009;32(9):1155–60. doi: 10.1093/sleep/32.9.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beck SL, Berger AM, Barsevick AM, Wong B, Stewart KA, Dudley WN. Sleep quality after initial chemotherapy for Breast cancer. Support Care Cancer juin. 2010;18(6):679–89. doi: 10.1007/s00520-009-0662-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li W, Kwok CCH, Chan DCW, Ho AWY, Ho CS, Zhang J, et al. Disruption of sleep, sleep-wake activity rhythm, and nocturnal melatonin production in Breast cancer patients undergoing adjuvant chemotherapy: prospective cohort study. Sleep Med mars. 2019;55:14–21. doi: 10.1016/j.sleep.2018.11.022. [DOI] [PubMed] [Google Scholar]
- 33.Kuo HH, Chiu MJ, Liao WC, Hwang SL. Quality of Sleep and related factors during chemotherapy in patients with stage I/II Breast Cancer. J Formos Med Assoc. 2006;105(1):64–9. doi: 10.1016/S0929-6646(09)60110-8. [DOI] [PubMed] [Google Scholar]
- 34.Ancoli-Israel S, Liu L, Marler MR, Parker BA, Jones V, Sadler GR, Dimsdale J, Cohen-Zion M, Fiorentino L. Fatigue, sleep, and circadian rhythms prior to chemotherapy for Breast cancer. Supportive care in cancer: Official Journal of the Multinational Association of Supportive Care in Cancer. 2006;14(3):201–9. doi: 10.1007/s00520-005-0861-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berger AM, Farr LA, Kuhn BR, Fischer P, Agrawal S. Values of Sleep/Wake, Activity/Rest, circadian rhythms, and fatigue prior to adjuvant Breast Cancer Chemotherapy. J Pain Symptom Manag. 2007;33(4):398–409. doi: 10.1016/j.jpainsymman.2006.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roscoe JA, Perlis ML, Pigeon WR, O’Neill KH, Heckler CE, Matteson-Rusby SE, et al. Few changes observed in Polysomnographic-assessed sleep before and after completion of Chemotherapy. J Psychosom Res déc. 2011;71(6):423–8. doi: 10.1016/j.jpsychores.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Silberfarb PM, Hauri PJ, Oxman TE, Schnurr P. Assessment of sleep in patients with Lung cancer and Breast cancer. J Clin Oncology: Official J Am Soc Clin Oncol. 1993;11(5):997–1004. doi: 10.1200/JCO.1993.11.5.997. [DOI] [PubMed] [Google Scholar]
- 38.Eldin ET, Younis SG, Aziz L, Eldin AT, Erfan ST. Evaluation of sleep pattern disorders in Breast cancer patients receiving adjuvant treatment (chemotherapy and/or radiotherapy) using polysomnography. J BUON. 2019;24(2):529–34. [PubMed] [Google Scholar]
- 39.Parker KP, Bliwise DL, Ribeiro M, Jain SR, Vena CI, Kohles-Baker MK, et al. Sleep/Wake patterns of individuals with Advanced Cancer measured by Ambulatory Polysomnography. J Clin Oncol 20 mai. 2008;26(15):2464–72. doi: 10.1200/JCO.2007.12.2135. [DOI] [PubMed] [Google Scholar]
- 40.Scullin MK, Bliwise DL. Sleep, cognition, and normal aging: integrating a half century of Multidisciplinary Research. Perspect Psychol Sci Janv. 2015;10(1):97–137. doi: 10.1177/1745691614556680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Born J. Slow-wave sleep and the consolidation of long-term memory. World J Biol Psychiatry janv. 2010;11(sup1):16–21. doi: 10.3109/15622971003637637. [DOI] [PubMed] [Google Scholar]
- 42.Bryant NB, Nadel L, Gómez RL. Associations between sleep and episodic memory updating. Hippocampus août. 2020;30(8):794–805. doi: 10.1002/hipo.23178. [DOI] [PubMed] [Google Scholar]
- 43.Mander BA, Winer JR, Walker MP. Sleep and Human Aging Neuron 5 avr. 2017;94(1):19–36. doi: 10.1016/j.neuron.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Petzka M, Chatburn A, Charest I, Balanos GM, Staresina BP. Sleep spindles track cortical learning patterns for memory consolidation. Curr Biol juin. 2022;32(11):2349–2356e4. doi: 10.1016/j.cub.2022.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Duivon M, Perrier J, Segura-Djezzar C, Joly F, Rehel S, Berthomier C, et al. Sleep-dependent memory consolidation in Breast cancer: use of a virtual reality prospective memory task. Front Neurosci 7 sept. 2022;16:908268. doi: 10.3389/fnins.2022.908268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abraham J, Haut MW, Moran MT, Filburn S, Lemiuex S, Kuwabara H. Adjuvant chemotherapy for Breast Cancer: effects on Cerebral White Matter seen in Diffusion Tensor Imaging. Clin Breast Cancer févr. 2008;8(1):88–91. doi: 10.3816/CBC.2008.n.007. [DOI] [PubMed] [Google Scholar]
- 47.Deprez S, Amant F, Smeets A, Peeters R, Leemans A, Van Hecke W, et al. Longitudinal Assessment of Chemotherapy-Induced Structural changes in Cerebral White Matter and its correlation with impaired cognitive functioning. J Clin Oncol 20 janv. 2012;30(3):274–81. doi: 10.1200/JCO.2011.36.8571. [DOI] [PubMed] [Google Scholar]
- 48.Tong T, Lu H, Zong J, Lv Q, Chu X. Chemotherapy-related cognitive impairment in patients with Breast cancer based on MRS and DTI analysis. Breast Cancer sept. 2020;27(5):893–902. doi: 10.1007/s12282-020-01094-z. [DOI] [PubMed] [Google Scholar]
- 49.de Ruiter MB, Reneman L, Boogerd W, Veltman DJ, Caan M, Douaud G, et al. Late effects of high-dose adjuvant chemotherapy on white and gray matter in Breast cancer survivors: converging results from multimodal magnetic resonance imaging. Hum Brain Mapp déc. 2012;33(12):2971–83. doi: 10.1002/hbm.21422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Inagaki M, Yoshikawa E, Matsuoka Y, Sugawara Y, Nakano T, Akechi T, et al. Smaller regional volumes of brain gray and white matter demonstrated in Breast cancer survivors exposed to adjuvant chemotherapy. Cancer 1 janv. 2007;109(1):146–56. doi: 10.1002/cncr.22368. [DOI] [PubMed] [Google Scholar]
- 51.Koppelmans V, de Ruiter MB, van der Lijn F, Boogerd W, Seynaeve C, van der Lugt A, et al. Global and focal brain volume in long-term Breast cancer survivors exposed to adjuvant chemotherapy. Breast Cancer Res Treat 1 avr. 2012;132(3):1099–106. doi: 10.1007/s10549-011-1888-1. [DOI] [PubMed] [Google Scholar]
- 52.Lange M, Joly F, Vardy J, Ahles T, Dubois M, Tron L, et al. Cancer-related cognitive impairment: an update on state of the art, detection, and management strategies in cancer survivors. Ann Oncol déc. 2019;30(12):1925–40. doi: 10.1093/annonc/mdz410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lepage C, Smith AM, Moreau J, Barlow-Krelina E, Wallis N, Collins B, et al. A prospective study of grey matter and cognitive function alterations in chemotherapy-treated Breast cancer patients. SpringerPlus 19 août. 2014;3:444. doi: 10.1186/2193-1801-3-444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 1 mai. 2011;34(5):601–8. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the Sleep Apnea Syndrome. Ann Intern Med. oct 1999;5(7):485. [DOI] [PubMed]
- 56.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res mai. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 57.Horne JA, Östberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976. [PubMed]
- 58.Martinez-Nicolas A, Martinez-Madrid MJ, Almaida-Pagan PF, Bonmati-Carrion MA, Madrid JA, Rol MA. Assessing chronotypes by ambulatory circadian monitoring. Front Physiol. nov 2019;20:10:1396. [DOI] [PMC free article] [PubMed]
- 59.Joly F, Lange M, Rigal O, Correia H, Giffard B, Beaumont JL, et al. French version of the Functional Assessment of Cancer therapy–cognitive function (FACT-Cog) version 3. Support Care Cancer déc. 2012;20(12):3297–305. doi: 10.1007/s00520-012-1439-2. [DOI] [PubMed] [Google Scholar]
- 60.Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol mars. 1993;11(3):570–9. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 61.Cleeland CS, Ryan K. The brief pain inventory. Pain Res Group. 1991;20:143–7. [Google Scholar]
- 62.Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes. 16 déc 2003;1:79. [DOI] [PMC free article] [PubMed]
- 63.Smets EMA, Garssen B, Bonke B, De Haes JCJM. The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res avr. 1995;39(3):315–25. doi: 10.1016/0022-3999(94)00125-O. [DOI] [PubMed] [Google Scholar]
- 64.Spielberger C, Goruch R, Lushene R, Vagg P, Jacobs G. Manual for the state-trait inventory STAI (form Y). Mind Gard Palo Alto CA USA; 1983.
- 65.Beck AT. An inventory for Measuring Depression. Arch Gen Psychiatry 1 juin. 1961;4(6):561. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 66.Galasso L, Montaruli A, Mulè A, Castelli L, Bruno E, Pasanisi P, et al. Rest-activity rhythm in Breast cancer survivors: an update based on non-parametric indices. Chronobiol Int 2 juin. 2020;37(6):946–51. doi: 10.1080/07420528.2020.1756839. [DOI] [PubMed] [Google Scholar]
- 67.Martin T, Duivon M, Bessot N, Grellard JM, Emile G, Polvent S, et al. Rest activity rhythms characteristics of Breast cancer women following endocrine therapy. Sleep 11 avr. 2022;45(4):zsab248. doi: 10.1093/sleep/zsab248. [DOI] [PubMed] [Google Scholar]
- 68.Bernard P, Savard J, Steindorf K, Sweegers MG, Courneya KS, Newton RU, et al. Effects and moderators of exercise on sleep in adults with cancer: individual patient data and aggregated meta-analyses. J Psychosom Res 1 sept. 2019;124:109746. doi: 10.1016/j.jpsychores.2019.109746. [DOI] [PubMed] [Google Scholar]
- 69.Kreutz C, Schmidt ME, Steindorf K. Effects of physical and mind–body exercise on sleep problems during and after Breast cancer treatment: a systematic review and meta-analysis. Breast Cancer Res Treat Juill. 2019;176(1):1–15. doi: 10.1007/s10549-019-05217-9. [DOI] [PubMed] [Google Scholar]
- 70.Mölle M, Marshall L, Gais S, Born J. Grouping of spindle activity during slow oscillations in human Non-rapid Eye Movement Sleep. J Neurosci 15 déc. 2002;22(24):10941–7. doi: 10.1523/JNEUROSCI.22-24-10941.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief Screening Tool for mild cognitive impairment: MOCA: a BRIEF SCREENING TOOL FOR MCI. J Am Geriatr Soc avr. 2005;53(4):695–9. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 72.Rieu D, Bachoud-Lévi AC, Laurent A, Jurion E, Dalla Barba G. Adaptation française Du « Hopkins verbal learning test ». Rev Neurol (Paris) juin. 2006;162(6–7):721–8. doi: 10.1016/S0035-3787(06)75069-X. [DOI] [PubMed] [Google Scholar]
- 73.Godefroy O. Fonctions exécutives et pathologies neurologiques et psychiatriques: évaluation en pratique clinique. Groupe de Boeck; 2008.
- 74.Brickenkamp R, Schmidt-Atzert L, Liepmann D. D2-R: test d’attention concentrée. Éditions Hogrefe France.; 2015.
- 75.Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18(6):643. doi: 10.1037/h0054651. [DOI] [Google Scholar]
- 76.Cardebat D, Doyon B, Puel M, Goulet P, Joanette Y. Evocation lexicale Formelle et sémantique chez des sujets normaux. Performances et dynamiques de production en fonction du sexe, de l’âge et du niveau d’étude. Acta Neurol Belg. 1990;90(4):207–17. [PubMed] [Google Scholar]
- 77.Gauthier K, Morand A, Dutheil F, Alescio-Lautier B, Boucraut J, Clarys D, et al. Ageing stereotypes and prodromal Alzheimer’s Disease (AGING): study protocol for an ongoing randomised clinical study. BMJ Open. oct 2019;7(10):e032265. [DOI] [PMC free article] [PubMed]
- 78.Hilliard D, Passow S, Thurm F, Schuck NW, Garthe A, Kempermann G, et al. Noisy galvanic vestibular stimulation modulates spatial memory in young healthy adults. Sci Rep 27 juin. 2019;9(1):9310. doi: 10.1038/s41598-019-45757-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lange M, Clarisse B, Leconte A, Dembélé KP, Lequesne J, Nicola C, et al. Cognitive assessment in patients treated by immunotherapy: the prospective Cog-Immuno trial. BMC Cancer 13 déc. 2022;22:1308. doi: 10.1186/s12885-022-10384-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Caplette-Gingras A, Savard J, Savard MH, Ivers H. Is Insomnia Associated with cognitive impairments in Breast Cancer patients? Behav Sleep Med sept. 2013;11(4):239–57. doi: 10.1080/15402002.2012.672940. [DOI] [PubMed] [Google Scholar]
- 81.Liou KT, Ahles TA, Garland SN, Li QS, Bao T, Li Y, et al. The relationship between Insomnia and cognitive impairment in Breast Cancer survivors. JNCI Cancer Spectr 7 juin. 2019;3(3):pkz041. doi: 10.1093/jncics/pkz041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Xu S, Thompson W, Ancoli-Israel S, Liu L, Palmer B, Natarajan L. Cognition, quality-of-life, and symptom clusters in Breast cancer: using bayesian networks to elucidate complex relationships. Psychooncology mars. 2018;27(3):802–9. doi: 10.1002/pon.4571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lowery-Allison AE, Passik SD, Cribbet MR, Reinsel RA, O’Sullivan B, Norton L, et al. Sleep problems in Breast cancer survivors 1–10 years posttreatment. Palliat Support Care juin. 2018;16(3):325–34. doi: 10.1017/S1478951517000311. [DOI] [PubMed] [Google Scholar]
- 84.Fleming L, Randell K, Stewart E, Espie CA, Morrison DS, Lawless C et al. Insomnia in Breast cancer: a prospective observational study. Sleep [Internet]. 1 mars 2019 [cité 24 Nov 2022];42(3). Disponible sur: https://academic.oup.com/sleep/article/doi/10.1093/sleep/zsy245/5231798. [DOI] [PubMed]
- 85.Perrier J, Duivon M, Clochon P, Rehel S, Doidy F, Grellard JM, et al. Sleep macro- and microstructure in Breast cancer survivors. Sci Rep 15 févr. 2022;12(1):2557. doi: 10.1038/s41598-022-06664-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Schmidt ME, Chang-Claude J, Vrieling A, Heinz J, Flesch-Janys D, Steindorf K. Fatigue and quality of life in Breast cancer survivors: temporal courses and long-term pattern. J Cancer Surviv mars. 2012;6(1):11–9. doi: 10.1007/s11764-011-0197-3. [DOI] [PubMed] [Google Scholar]
- 87.Palesh O, Peppone, Innominato J, Jeong M, Sprod L et al. Prevalence, putative mechanisms, and current management of sleep problems during chemotherapy for cancer. Nat Sci Sleep déc 2012;151. [DOI] [PMC free article] [PubMed]
- 88.Sousa H, Almeida S, Bessa J, Pereira MG. The Developmental Trajectory of Cancer-related cognitive impairment in Breast Cancer patients: a systematic review of Longitudinal Neuroimaging studies. Neuropsychol Rev 1 sept. 2020;30(3):287–309. doi: 10.1007/s11065-020-09441-9. [DOI] [PubMed] [Google Scholar]
- 89.Vien C, Boré A, Boutin A, Pinsard B, Carrier J, Doyon J, et al. Thalamo-cortical White Matter underlies motor memory consolidation via modulation of Sleep spindles in Young and older adults. Neurosci 15 mars. 2019;402:104–15. doi: 10.1016/j.neuroscience.2018.12.049. [DOI] [PubMed] [Google Scholar]
- 90.Piantoni G, Poil SS, Linkenkaer-Hansen K, Verweij IM, Ramautar JR, Van Someren EJW, et al. Individual Differences in White Matter Diffusion affect sleep oscillations. J Neurosci 2 janv. 2013;33(1):227–33. doi: 10.1523/JNEUROSCI.2030-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Garland SN, Johnson JA, Savard J, Gehrman P, Perlis M, Carlson L, et al. Sleeping well with cancer: a systematic review of cognitive behavioral therapy for insomnia in cancer patients. Neuropsychiatr Dis Treat. 2014;10:1113. doi: 10.2147/NDT.S47790. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.