To the Editor,
We have read with interest the published article entitled "Lower versus higher oxygen targets for out-of-hospital cardiac arrest: a systematic review and meta-analysis" by Cheng et al. [1]. The article is well written, and I have two concerns as explained below.
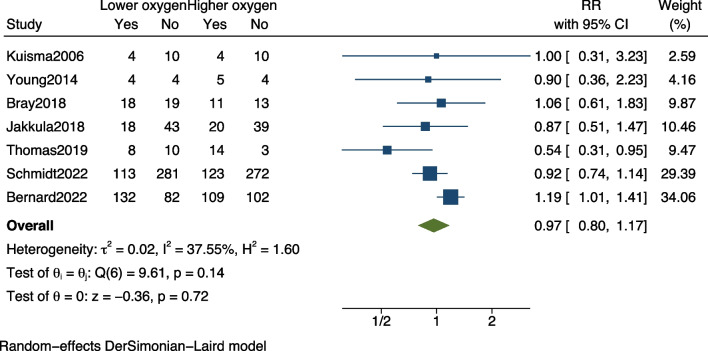
First, there may be a need for some data to be revised. The numbers in Table 1 [1] for sample size in the study by Bernard et al. [2] differ from those in the forest plot of Fig. 2 [1] (425 vs. 401). In the original text, Bernard et al. mentioned that hospital mortality should be 132 deaths in the lower oxygen saturation targets group (n = 214) and 109 deaths in the higher oxygen saturation targets group (n = 211), which is different from what the authors mentioned in the article. After correcting this error, the combined mortality rate should be RR, 0.97; 95% CI 0.80–1.17; p = 0.72 (Fig. 1).
Fig. 2.
Forest plot of hospital mortality. Lower oxygen target versus higher oxygen target among out-of-hospital cardiac arrest patients. The points and the bars represent the relative risk (RR) and 95% confidence interval (CI). RR, relative risk; CI, confidence interval
Fig. 1.
Forest plot of pooled mortality. Lower oxygen target versus higher oxygen target among out-of-hospital cardiac arrest patients. The points and the bars represent the relative risk (RR) and 95% confidence interval (CI). RR, relative risk; CI, confidence interval
Second, this study used 90-day mortality as its primary outcome. In cases where data for 90-day mortality were unavailable, the study also considered mortality at 30 days or in-hospital mortality for the pooled analysis. It is worth noting that among the seven included randomized controlled trials (RCTs), only two studies reported 90-day mortality [3, 4], one reported 30-day mortality [5], and the remaining four studies reported hospital mortality [2, 6–8]. Combining these different time points for mortality outcomes may increase the overall sample size and statistical power. Nevertheless, it could also introduce heterogeneity, affect the interpretation of the findings, and impact the reliability of the conclusion drawn.
I reanalyzed the data, excluding three studies, and performed a new analysis on the remaining four studies with the endpoint of hospital mortality [2, 6–8]. The results indicate that a higher oxygen target significantly reduces hospital mortality among out-of-hospital cardiac arrest patients (RR, 1.17; 95% CI 1.00–1.37; p = 0.05) (Fig. 2). Although the results did not demonstrate significant heterogeneity, the substantial weight of the Bernard study suggests that further studies are urged to offer more definitive answers.
Acknowledgements
Not applicable.
Author contributions
YZ, BZ, and QW participated in the discussion and wrote the manuscript.
Funding
None.
Availability of data and materials
Not applicable.
Declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Qian Wang, Email: wq0376@hotmail.com.
Bin Zang, Email: zangbin_66@163.com.
References
- 1.Cheng X, Zhang Y, Deng H, Feng Y, Chong W, Hai Y, et al. Lower versus higher oxygen targets for out-of-hospital cardiac arrest: a systematic review and meta-analysis. Crit Care. 2023;27(1):401. doi: 10.1186/s13054-023-04684-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernard SA, Bray JE, Smith K, Stephenson M, Finn J, Grantham H, et al. Effect of lower vs higher oxygen saturation targets on survival to hospital discharge among patients resuscitated after out-of-hospital cardiac arrest: the EXACT randomized clinical trial. JAMA. 2022;328(18):1818–1826. doi: 10.1001/jama.2022.17701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmidt H, Kjaergaard J, Hassager C, Molstrom S, Grand J, Borregaard B, et al. Oxygen targets in comatose survivors of cardiac arrest. N Engl J Med. 2022;387(16):1467–1476. doi: 10.1056/NEJMoa2208686. [DOI] [PubMed] [Google Scholar]
- 4.Thomas M, Voss S, Benger J, Kirby K, Nolan JP. Cluster randomised comparison of the effectiveness of 100% oxygen versus titrated oxygen in patients with a sustained return of spontaneous circulation following out of hospital cardiac arrest: a feasibility study. PROXY: post ROSC OXY genation study. BMC Emerg Med. 2019;19(1):16. doi: 10.1186/s12873-018-0214-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jakkula P, Reinikainen M, Hastbacka J, Loisa P, Tiainen M, Pettila V, et al. Targeting two different levels of both arterial carbon dioxide and arterial oxygen after cardiac arrest and resuscitation: a randomised pilot trial. Intensive Care Med. 2018;44(12):2112–2121. doi: 10.1007/s00134-018-5453-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bray JE, Hein C, Smith K, Stephenson M, Grantham H, Finn J, et al. Oxygen titration after resuscitation from out-of-hospital cardiac arrest: a multi-centre, randomised controlled pilot study (the EXACT pilot trial) Resuscitation. 2018;128:211–215. doi: 10.1016/j.resuscitation.2018.04.019. [DOI] [PubMed] [Google Scholar]
- 7.Kuisma M, Boyd J, Voipio V, Alaspaa A, Roine RO, Rosenberg P. Comparison of 30 and the 100% inspired oxygen concentrations during early post-resuscitation period: a randomised controlled pilot study. Resuscitation. 2006;69(2):199–206. doi: 10.1016/j.resuscitation.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 8.Young P, Bailey M, Bellomo R, Bernard S, Dicker B, Freebairn R, et al. HyperOxic therapy OR NormOxic therapy after out-of-hospital cardiac arrest (HOT OR NOT): a randomised controlled feasibility trial. Resuscitation. 2014;85(12):1686–1691. doi: 10.1016/j.resuscitation.2014.09.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.