Abstract
In 2022, Bruce Willis’ family released a statement saying that he had been diagnosed with aphasia (an acquired language impairment) and would no longer be acting. Ten months later, the Willis family released another statement indicating that he received a more specific diagnosis of frontotemporal degeneration (FTD). This resulted in an explosion of media coverage, as prominent news outlets scrambled to produce stories describing FTD to a public largely unfamiliar with the disease. The quality of these stories varied widely, and in many cases the relationship between aphasia and FTD was misrepresented, as were basic descriptions and facts about FTD. FTD refers to a class of protein-misfolding diseases that are a common cause of aphasias due to neurodegeneration, or primary progressive aphasias (PPA). Rather than describing how FTD was discovered to be the underlying source of Mr. Willis’ aphasia, many reports described his aphasia as “progressing into” FTD, implying they are two different disorders. Furthermore, these reports used the terminology of frontotemporal “dementia” rather than “degeneration”, a term that invokes many stereotypes in the public imagination and may have contributed to misrepresentations in coverage. Instead of focusing on the language symptoms of PPA, reports often emphasized the personality and behavioral changes more closely associated with other variants of FTD. The substance of various facts, such as how common FTD is and how it can be treated, varied widely across reports. In sum, the media coverage of Mr. Willis’ diagnosis reveals the extent to which the media and general public are uninformed about FTD and PPA. The remedy for this problem is to promote greater awareness of FTD, in both the public and the medical provider class. The Willis family’s disclosure was a courageous act that helped bring much-needed attention to this disease.
Keywords: Celebrity, Dementia, FTD, Primary progressive aphasia, Stigma
Translational Significance: Although frequently seen in specialized neurological and memory clinics, frontotemporal degeneration (FTD) remains less well known by the public compared to other neurodegenerative diseases such as Alzheimer’s and Parkinson’s disease. We highlight the extent of this problem via an analysis of media coverage, fact-checking aspects of various print, internet, television, and cable reports. It is our hope that such interactive dialog between the media and scientific/medical communities may help to promote public awareness and clear up misconceptions. Greater awareness of FTD in the public and medical provider class may allow affected individuals to be diagnosed more accurately and faster.
On March 30, 2022, Bruce Willis’ family released a statement, saying that “… Bruce has been experiencing some health issues and has recently been diagnosed with aphasia, which is impacting his cognitive abilities. As a result of this and with much consideration Bruce is stepping away from the career that has meant so much to him” (Moore, 2022). Aphasias are disorders of language, typically resulting from either a brain lesion (e.g., stroke, tumor) or from neurodegenerative disease. None of the media reports or the family’s subsequent statements suggested the presence of a lesion, which would have likely been detected with brain imaging. In combination with Mr. Willis’ age (67 at the time of diagnosis), it seemed more than likely that his language symptoms were a result of neurodegeneration.
This syndrome is known as primary progressive aphasia (PPA), in reflection of the unfortunate fact that neurodegeneration and language symptoms become worse over time (Gorno-Tempini et al., 2011; Mesulam, 1987). Confusingly, PPA is a cognitive syndrome rather than a neuropathological diagnosis, which means it can be caused by multiple underlying diseases. One of the most common causes of PPA is a class of diseases is called frontotemporal degeneration (FTD; a.k.a. frontotemporal dementia, frontotemporal lobar degeneration), based on the misfolding of certain tau or transactive response DNA binding protein 43 (TDP-43) proteins (Borghesani et al., 2020; Mesulam et al., 2023; Snowden et al., 2007). Most of the remaining PPA cases are an atypical manifestation of the plaques and tangles of Alzheimer’s disease (Bergeron et al., 2018; Spinelli et al., 2017). As such, the most likely sources of Mr. Willis’ aphasia would be FTD or Alzheimer’s disease pathology.
People familiar with PPA were thus unsurprised 10 months later (on February 16, 2023) when Mr. Willis’ family released a statement saying: “Since we announced Bruce’s diagnosis of aphasia in spring 2022, Bruce’s condition has progressed and we now have a more specific diagnosis: frontotemporal dementia (known as FTD)” (Willis et al., 2023). The resultant flurry of media reports, however, portrayed Mr. Willis’ FTD diagnosis as a surprising further development, rather than confirmation of the most likely scenario given the known underlying pathobiology of PPA.
Examination of the previous media coverage in March of 2022, in response to the family’s initial aphasia announcement, shows a perplexing lack of journalistic memory. The morning after the family’s aphasia statement, the NBC Today Show (Gaines & Miller, 2022), ABC’s Good Morning America (Schindler, 2022), and the CBS Mornings show (Fripp, 2022) all described how aphasia could be caused by a progressive dementia/neurological disease. People Magazine quoted the Mayo Clinic, noting that aphasia “typically occurs suddenly after a stroke or a head injury. But it can also come on gradually from a slow-growing brain tumor or a disease that causes progressive, permanent damage (degenerative)” (Juneau, 2022). And yet, following the family’s FTD statement 10 months later, NBC News NOW reported that Mr. Willis “… has been diagnosed with something called frontotemporal dementia. It comes a year after the actor’s family revealed he suffered from a different cognitive disease known as aphasia” (Hopper, 2023).
Media Misrepresentation of Mr. Willis’ FTD Diagnosis
The family’s FTD statement was released on the website for the Association for Frontotemporal Degeneration (AFTD) on February 16 (2023), and was carefully crafted (Willis et al., 2023). Their description of the relationship between aphasia and FTD was, as one would expect, clear and accurate, saying that FTD was a more specific diagnosis of the cause of the aphasia suffered by Mr. Willis. When paraphrased by news anchors on multiple television shows that evening, however, the relationship was reworded in a way that may have misled the lay public.
As reported by Norah O’Donnell on the CBS evening news, “His family says that has progressed into frontotemporal dementia, which impacts personality, behavior, and language” (Nalesnik & Hawley, 2023). Similarly, Entertainment Tonight reported that the family “… revealed that his brain disease has progressed to frontotemporal dementia” (Campbell, 2023). An article in Variety said that “… the 67-year-old actor had been diagnosed with aphasia and would retire from acting, his condition has now progressed into frontotemporal dementia” (Moreau, 2023). The half-spoken connotation here is that aphasia can develop into the more serious condition of FTD, failing to recognize that the former is a manifestation of the latter. As an analogy, it would be harder to imagine cognition and neuropathology being conflated in this way if a patient had instead been diagnosed with tremor, and it was later revealed the underlying source was Parkinson’s disease. In such a scenario, given the public’s greater familiarity with this syndrome, it seems unlikely that the media would report tremor “progressing into” Parkinson’s disease.
So why did several news outlets change the family’s statement in nearly the same way, by stating that aphasia progressed into FTD? One possibility is that it made for a better narrative: an esoteric and complicated story about diagnostic clarification is not nearly as interesting as a story of one of the world’s largest stars suffering further misfortune Reporters may also have been encouraged along that path by the ways in which we describe FTD. The family’s statement included the terminology of “frontotemporal dementia,” and the latter word invokes many connotations in the public imagination.
In common practice, the term dementia is used to refer to any neurodegenerative disease affecting older adults. This term has been in use since the 1600s, derived from Latin, meaning “madness” or “being out of one’s mind.” The implication is that someone with dementia is mentally ill and suffering from pervasive cognitive impairments. The reality, however, is that many neurodegenerative diseases target a small number of brain networks in initial stages, resulting in isolated domains of cognitive and behavioral impairments.
The most common form of neurodegeneration targets the medial temporal lobes first, resulting in the amnestic syndrome of Alzheimer’s disease. Although memory is affected in early stages, other cognitive faculties such as language, visuoperception, and motor skills (praxis) may remain relatively intact during that time (Davidson et al., 2010; Stopford et al., 2008). The distribution of FTD pathology is more variable and is often first apparent in the frontal and/or temporal lobes (hence the “frontotemporal” monicker) but may concentrate in other regions in variants such as corticobasal degeneration and progressive supranuclear palsy. This results in a bouquet of symptoms, sometimes resulting in language impairments (i.e., PPA), other times in personality and behavioral changes, and other times in motor impairments. Other domains of cognition such as memory and visuoperception may be relatively spared in early stages (Gorno-Tempini et al., 2011; Mesulam et al., 2012; Rascovsky et al., 2011).
The specific domain of impairment often determines the specific limitations a person with FTD might face in daily life. Far from the stereotype of dementia with confusion and lack of insight, an individual in the early stages of PPA may live a relatively normal life, experiencing difficulty mainly when having to translate thoughts through the filter of language. Having said that, the everyday experiences and quality of life vary widely across individuals with PPA (Davies & Howe, 2020; Ruggero et al., 2019, 2023).
When the term dementia was applied to Mr. Willis, this likely evoked a set of stereotypes among reporters that influenced the coverage. By subtly changing the family’s statement such that Mr. Willis’ aphasia “progressed into” FTD, news outlets created a digestible, if potentially inaccurate, narrative for public consumption: Mr. Willis had language impairments, but now he has developed dementia. It reduces a complicated and diverse set of interrelated cognitive, anatomical, and pathological processes into a single term that every American is familiar with and can be equally applied to any individual with neurodegenerative disease, regardless of their specific circumstances. This was most clearly distilled in the chyron on the bottom of the screen during the next-day CBS Mornings coverage, which simply read “Bruce Willis diagnosed with dementia” (Fripp, 2023).
In 2008, a caregiver whose partner had neurodegenerative disease teamed up with an expert clinician/researcher, and together they published a paper calling for the term dementia to be eliminated from medical diagnoses altogether (Trachtenberg & Trojanowski, 2008). In 2011, AFTD changed its name from the “Association for Frontotemporal Dementia” to the “Association for Frontotemporal Degeneration.” At the time, the association noted that “A significant portion of families do not identify with the term ‘dementia’ and some are offended by it” (Association for Frontotemporal Degeneration, 2011). They further described why they chose the alternative term of degeneration: “The term ‘degeneration’ emphasizes some of the critical characteristics of FTD—the gradual and progressive nature of the degeneration in brain cells, as well as variable degrees of the degeneration in cognitive, behavior, language, and motor functioning.” It is possible that the media coverage of Bruce Willis’ FTD diagnosis would have had a different tone, and perhaps have been subject to less distortion, if his diagnosis been described as “frontotemporal degeneration” rather than “frontotemporal dementia.”
Fact-Checking Other Aspects of the Media Coverage
After stating the headline that Mr. Willis had been diagnosed with FTD, most of the news stories then expanded by providing fundamental facts about FTD. The accuracy in reporting these facts varied widely across media outlets. The most egregiously inaccurate reports were published on the same day as the family’s FTD statement (February 16, 2023), suggesting that a rush to report same day led to errors. There were also clear distinctions in the quality of reporting between the nation’s premier newspapers (The New York Times and The Washington Post), who produced impressive same-day reports, versus the same-day and next-day coverage on television, cable, and internet news outlets. Factual coverage almost universally focused on addressing the following questions, all of which would be valuable for the public to know: (1) what is FTD?, (2) how common is FTD?, and (3) are there any treatments for FTD?
What Is FTD?
The same-day New York Times story described FTD as “… a form of dementia that occurs most commonly when nerve cells in the frontal and temporal lobes of the brain decrease in number,” which is a reasonable enough description (Blum, 2023). The story described how “There are two main variants of FTD: primary progressive aphasia, which hampers a patient’s ability to communicate, and behavioral variant frontotemporal dementia, which manifests as personality and behavioral changes.” Importantly, this description acknowledges that there are two common syndromes of FTD with different cognitive symptoms (although motor variants also exist).
Many individuals with FTD pathology display the syndrome of behavioral variant FTD (bvFTD; Hogan et al., 2016; Knopman & Roberts, 2011; Logroscino et al., 2023). Atrophy in these individuals is most intense in the frontal lobes, resulting in changes to personality and comportment. Specific symptoms may include impulsivity, socially inappropriate behaviors, apathy, eating changes, and loss of empathy (Rascovsky et al., 2011). These changes may drive individuals to engage in criminal behavior for the first time in their lives, so bvFTD is sometimes identified via interactions with the criminal justice system rather than the healthcare system (Diehl-Schmid et al., 2013).
Another common manifestation of FTD is the PPA syndrome (Hogan et al., 2016; Knopman & Roberts, 2011; Logroscino et al., 2023). The Washington Post same-day report had the most thorough and accurate description of PPA, describing the language symptoms, the underlying proteinopathy, and the relationships between the two. “There are two major subtypes of aphasia—the agrammatic type or the semantic type—that are caused by FTD, said Brad Dickerson, Director of the Frontotemporal Disorders Unit at Massachusetts General Hospital, neurologist and professor of neurology at Harvard Medical School. ‘The agrammatic type is more of a problem with producing grammatically constructed sentences, syntax, whereas the semantic type is really the meanings of words,’ he said. ‘The agrammatic type tends to be due to the tau problem in the brain, which affects the frontal lobe, mostly. Whereas the semantic type tends to be due to the TDP-43 type, which tends to affect the temporal lobe of the brain’” (Sima et al., 2023). Symptoms in the semantic subtype of PPA center on inability to comprehend the meaning of individual words, particularly nouns (Hurley et al., 2012).
In contrast to The New York Times and The Washington Post same-day reports, which emphasized that bvFTD and PPA are two different syndromes, most television news coverage conflated the two very different sets of cognitive symptoms, and implied that Mr. Willis was suffering from both. To be clear, a given individual with FTD may show a mixture of language and behavioral symptoms, particularly in late stages of disease when atrophy spreads to multiple brain networks (Modirrousta et al., 2013), but in earlier stages cognitive impairments can be relatively isolated to a single domain (e.g., language; Mesulam et al., 2012). Given the family’s statements it was clear enough that Mr. Willis has been suffering from PPA, so it is unclear why many news outlets focused on the more flamboyant symptoms of bvFTD.
For example, on ABC News Live Prime’s same-day coverage, they described how FTD “… can be very tricky to diagnose because its most prominent symptoms are actually behavioral. So, in addition to cognitive impairment, these patients may develop dramatic personality changes, they may develop compulsive or impulsive behaviors, they may be inappropriate at times, they may be apathetic, there’s so many different ways this can look. And, of course, in some cases language can be a major presenting symptom” (Kavanaugh, 2023). The language symptoms of PPA were also listed after the behavioral symptoms of bvFTD on the CBS Evening News, when Nora O’Donnell said that FTD “… impacts personality, behavior, and language” (Nalesnik & Hawley, 2023). In drawing analogies to other medical conditions, it would be hard to imagine a report on an early lung cancer diagnosis beginning with a description of late-stage metastatic brain cancer symptoms.
How Common Is FTD?
Given most people’s unfamiliarity with FTD, it is natural to wonder how common the condition is. This issue is the most difficult to fact check, and we may have more sympathy for errors in reporting. FTD is often misdiagnosed as Alzheimer’s disease (Beber & Chaves, 2013; Mouton et al., 2022), for example, when clinicians mistake problems with word finding (associated with PPA) as being a problem with memory. Likewise, the symptoms of bvFTD are easily mistaken for a psychiatric disorder (Ducharme et al., 2015; Zapata-Restrepo et al., 2021). Individuals are more likely to receive an accurate diagnosis if they are receiving upper-tier specialized medical care in urban centers (Besser & Galvin, 2020), and it typically takes over 3 years to arrive at that diagnosis (Draper et al., 2016).
The overlapping relationships between PPA and FTD are a further source of confusion, as there would be fewer of the former at any given time (because many FTD cases are bvFTD or motor variants), and not everyone who has PPA also has FTD. Keep in mind that FTD at least nominally refers to the underlying pathology, which can ultimately only be confirmed via autopsy or biomarker studies. It may thus be that an individual has PPA and the presence of FTD may be inferred but not confirmed. A third subtype of PPA we have not mentioned so far, known as the logopenic variant, is often caused by Alzheimer’s pathology rather than FTD pathology (Rogalski et al., 2016). The odds of finding a clinician who understands these complexities are extremely low, particularly for people being treated in community clinics rather than specialized centers.
Keeping all those issues in mind, which would collectively serve to underestimate the true frequency of FTD in the population, one would then need to examine the few scientific reports attempting to construct population estimates. This quickly leads to esoteric distinctions such as prevalence (the total number of cases in the population in a given time period) versus incidence (the number of new cases diagnosed during a period of time). For those unversed in epidemiological methods (such as reporters), this is a daunting challenge.
Given these issues, most new investigators understandably turned to trusted sources such as the AFTD and Alzheimer’s Association (AA) websites for information. The New York Times (Blum, 2023), The Washington Post (Sima et al., 2023), Time Magazine (Park, 2023), and the NBC Today Show (D’Incecco et al., 2023) and all quoted prevalence estimates from the AFTD (Association for Frontotemporal Degeneration, 2023b). The AFTD estimates that 50,000–60,000 Americans currently have FTD, based on the prevalence estimate from Knopman and Roberts’ (2011). The AFTD readily acknowledges, however, that this is likely an underestimate. The Knopman and Roberts’ study did not include all FTD variants, such as corticobasal degeneration, progressive supranuclear palsy, and other motor variants, which may represent an appreciable proportion of cases (Leroy et al., 2021; Logroscino et al., 2023).
Rather than getting into the complexities of prevalence, other reporters tried to summarize the frequency of FTD in terms of the percentage of neurodegenerative disease cases. ABC News Live Prime’s same-day coverage mentioned that FTD “represents 10% of dementia cases” (Kavanaugh, 2023). CNN’s next-day coverage described FTD as being about 20% of neurodegenerative cases (Sheetrit, 2023). These numbers would appear to be vastly at odds with Knopman and Roberts’ numbers, suggesting FTD is far more prevalent. These rates may have come from the AA website, which mentions that “FTD, once considered rare, is now thought to account for up to 10 to 15 percent of all dementia cases” (Alzheimer’s Association, 2023b). Likewise, the Mayo Clinic website says that “FTD is the cause of approximately 10% to 20% of dementia cases.” The 10% figure may have come from Hogan et al. (2016), who estimated that FTD represents about 10% of neurodegenerative cases younger than 65 and about 3% of cases older than 65. While there may be good reasons for separating figures according to specific age ranges, this causes further confusion in trying to identify how common FTD is.
So how do these rates line up with the also widely cited Knopman and Roberts figures? First off one would need to determine how many total cases of neurodegenerative disease there are in the United States, which is also surprisingly difficult. The AA provides figures each year on the number of Alzheimer’s cases, which would be a smaller subset of the total neurodegenerative cases. In 2023 they estimated that 6.7 million Americans over the age of 65 had Alzheimer’s disease (Alzheimer’s Association, 2023a). Many people with FTD are diagnosed younger than 65, and it is difficult to make comparisons based on different age ranges. The AA estimates that about 200,000 American’s currently have a younger onset neurodegenerative disease (onset prior to age 65 years). Taking these numbers along with those from the Hogan study, if one assumed that 3% of 6.7 million American’s over 65 had FTD, and 10% of the 200,000 Americans with younger onset diseases had FTD, you would arrive at a figure of 221,000 total Americans with FTD, roughly four times greater than estimated in the Knopman and Roberts study.
The apparent contradiction here was overlooked in the next-day coverage on the CBS Mornings show, which stated both that FTD was 20% of neurodegenerative cases, and that there were 50,000–60,000 Americans with FTD (Fripp, 2023).
So, are the actual numbers of Americans with FTD closer to 50,000 or 221,000, or even greater? No one knows for sure, and the existing prevalence and incidence estimates are just that: rough estimates, each depending on a huge number of assumptions. There are currently no convincing prevalence studies in the United States. Researchers in other countries have taken advantage of comprehensive medical registries and sophisticated experimental designs to estimate that FTD represents about 2%–5% of all neurodegenerative cases, regardless of age (Feldman et al., 2003; Leroy et al., 2021; Nilsson et al., 2014). These numbers seem reasonable (face valid), but more information is needed before we can state specific numbers in the United States with confidence. Regardless of such specifics, FTD appears to be an appreciable portion of neurodegenerative cases, and the public’s unfamiliarity with FTD is out of sync with its prevalence.
Are There Any Treatments for FTD?
Most of the news stories about Mr. Willis ended with a description of how FTD can be treated. The answers provided by medical experts for these stories varied widely, with some more realistic than others. As accurately noted in The Washington Post’s same-day story, “There is no cure for FTD. ‘Just like Alzheimer’s, at this time, there is no disease-modifying therapy, no curative therapy,’ said Chi-Ying ‘Roy’ Lin, a neurology professor at Baylor College of Medicine” (Sima et al., 2023). Sadly, this is currently the case for most neurodegenerative diseases. As noted by Dr. Ian Grant, an assistant professor of neurology at the Northwestern University Feinberg School of Medicine, in The New York Times’ same-day coverage, however, “… there’s a difference between a disease not having a cure and saying, ‘There’s nothing we can do’” (Blum, 2023). Although there are no cures for FTD, a wider notion of a “treatment” could also refer to any therapeutic that will make life more comfortable for someone with FTD, for example, by ameliorating individual symptoms.
For someone with PPA, speech therapy as delivered by a speech language pathologist can be extremely valuable, sometimes leading to language gains (reacquiring lost words), other times helping to manage decline in language (Savage et al., 2021; Taylor-Rubin et al., 2021; Volkmer et al., 2020). A speech language pathologist can also help promote alternative communication techniques when word finding failures or speech deficits make oral communication too difficult (Robinaugh & Henry, 2022). The New York Times, The Washington Post, and ABC News Live Prime were the only news outlets to mention speech therapy as an option in their coverage (Blum, 2023; Kavanaugh, 2023; Sima et al., 2023). The New York Times also mentioned occupational therapy, which can be useful for other symptoms in FTD (Kortte & Rogalski, 2013; Tsai & Boxer, 2014).
The Washington Post story included an in-depth description of pharmaceutical drugs prescribed for FTD. They noted that many of the drugs administered to help with cognitive symptoms (e.g., Donepezil, Memantine) were developed for Alzheimer’s disease, and that there is no solid evidence they are effective for FTD in terms of treating cognitive or behavioral changes. The New York Times and Time Magazine also noted that medications are available to treat mood and behavior symptoms (e.g., depression, anxiety, delusions), which are sometimes noted in people diagnosed with neurodegenerative diseases (Collins et al., 2023).
Other news outlets included a description of therapeutics for which the evidence is unclear. On Fox & Friends’ next-day coverage (Florentin, 2023), they described how staying mentally active via activities such as crossword puzzles could be beneficial. There is some evidence that individuals with FTD who are more cognitively engaged may have better outcomes, but the use of correlational methods makes it difficult to know whether this engagement actually slows cognitive decline or is merely a correlated factor (Casaletto et al., 2020). Studies employing cognitive training can overcome correlational limitations, but the literature on the efficacy of such trainings is mixed and difficult to interpret. Gains may be made in some neurodegenerative populations, but they tend to be subtle and task-specific, rather than slowing cognitive decline in general (National Academies of Sciences, Engineering, and Medicine [NASEM] et al., 2017). Putative benefits appear to be greatest in older adults prior to developing a neurodegenerative disease, or in the earliest stages of disease (Hill et al., 2017; Lasaponara et al., 2021).
There have been few cognitive interventions for FTD, with successful trainings instead tending to focus on specific behaviors seen in bvFTD (Shinagawa et al., 2015). In the case of PPA it may make more sense to focus on speech therapy, which directly targets the relevant language symptoms and communication partner-focused therapies, rather than attempting to train other domains of cognition (Robinaugh & Henry, 2022; Taylor-Rubin et al., 2021; Volkmer et al., 2020). Individuals may also benefit from interventions for specific symptoms than tend to emerge in later stages of disease, such as difficulties with swallowing (dysphagia) or motor coordination. Evaluation of caregiver stress and proving support is a key pillar of management, given the dangers of caregiver burnout to the family members providing close care in FTD (Karnatz et al., 2021).
In their coverage Fox & Friends also mentioned “healthy lifestyle” as being protective (Florentin, 2023), which is a general term for engaging in regular exercise, having good nutrition, avoiding substance abuse, obtaining quality sleep, and other such factors. Most of the components of a healthy lifestyle have been supported scientifically, in terms of delaying the onset and improving outcomes for FTD and other neurodegenerative diseases (Casaletto et al., 2020; Dhana et al., 2020; Sabia et al., 2021). A general rule of thumb is that any type of behavior that improves cardiovascular function will also benefit the brain (NASEM et al., 2017). NBC News NOW’s coverage also emphasized healthy lifestyle (Hopper, 2023), but included the consumption of organic foods as part of a healthy lifestyle, for which we could find no scientific evidence. Mediterranean diets such as MIND, however, have been shown to be beneficial in Alzheimer’s disease (Agarwal et al., 2023), and may plausibly be of benefit in other younger onset diseases such FTD (Filippini et al., 2020).
Conclusion
The public and the medical provider class remains relatively unfamiliar with FTD, compared to Alzheimer’s disease. This unfamiliarity contributes to FTD being under and misdiagnosed and many patients being misinformed. Misdiagnosed individuals may be given medications with potential side effects and no established benefits in FTD (e.g., Alzheimer drugs), and conversely may not be referred to therapeutics of proven benefit such as speech therapy. The news coverage of Mr. Willis’ FTD diagnosis, which included significant distortions and mistruths, revealed the extent of this unfamiliarity. The extensive coverage of Mr. Willis was a net positive, however, as it has drawn attention to FTD, and has enhanced the public’s knowledge of this disease.
Public figures have great power to draw attention to medical conditions, as was the case when Lou Gehrig disclosed his diagnosis of amyotrophic lateral sclerosis (Cavicke & O’Leary, 2001). Mr. Willis and his family have been courageous in sharing the details of his path to being diagnosed with aphasia (PPA) and FTD. Mr. Willis is one of the world’s largest stars, resulting in worldwide media coverage of his diagnosis. The AFTD noted that the month after the Willis family’s announcement, the number of visitors to their website increased by more than 18 times, resulting in 1.9 million visitors in March of 2023 (Association for Frontotemporal Degeneration, 2023a). Also, during that time, phone calls to the AFTD HelpLine (866-507-7222) more than doubled, and the number of followers of @theAFTD on Instagram almost doubled.
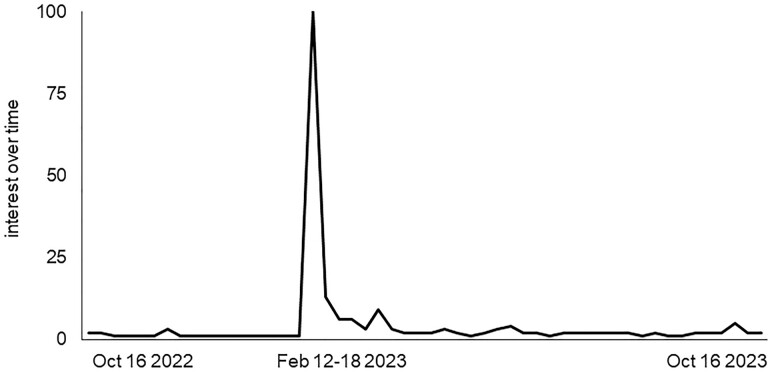
Similarly, the interest in FTD stimulated by the Willis family’s disclosure is apparent in the history of internet searches on Google Trends (https://www.google.com/trends). We queried Google Trends to see “interest over time” in the United States for the term “frontotemporal dementia” throughout the past year, from October 16, 2022, to October 16, 2023 (Figure 1). The interest over time metric reflects the number of internet searches on a given topic, normalized over time such that the scale ranges from 0 (least relative interest) to 100 (greatest relative interest). Interest peaked at 100 during the week of February 12–18, 2023, when the Willis family’s statement on FTD was released, demonstrating the impact of their disclosure. Although interest has declined rapidly since that peak, levels remain over double what they were predisclosure (average of 2.9 postdisclosure vs 1.2 predisclosure).
Figure 1.
Interest over time for the term “frontotemporal dementia” on Google Trends. Interest over time reflects the number of internet searches for “frontotemporal dementia” across a 1-year time period, normalized on scale from 0 to 100. Interest peaked the week of the Willis family’s frontotemporal degeneration disclosure (February 16, 2023), and has remained elevated since then compared to the preceding period. Data source: Google Trends (https://www.google.com/trends).
Given its frequency in the population, other public figures throughout the ages must have had FTD as well. We could only identify one other famous individual to disclose an FTD diagnosis. In 2015 Terry Jones, the comedian, director, and Monty Python member, was also diagnosed with PPA and FTD. Like Mr. Willis, Mr. Jones shared his diagnoses with the public, before passing away in 2020.
It is striking how often individuals with neurodegenerative disease and their families put efforts into helping others, even when they know those efforts will not directly benefit themselves. We see this sort of altruism every day, when participants with neurodegenerative diseases volunteer for research studies that may 1 day lead to treatments, when they and their families engage in fundraising, and when they share their experiences with the press and social media. The transparency of Mr. Willis and his family is in this same spirit of altruism, and the FTD community and general public have benefitted from their graciousness.
Acknowledgments
We would like to thank Dr. Jennifer Stanley at the University of Akron for encouraging and facilitating the writing of this article.
Contributor Information
Robert S Hurley, Department of Psychology, Cleveland State University, Cleveland, Ohio, USA.
Jagan A Pillai, Lou Ruvo Center for Brain Health, Neurological Institute, Cleveland Clinic, Cleveland, Ohio, USA.
James B Leverenz, Lou Ruvo Center for Brain Health, Neurological Institute, Cleveland Clinic, Cleveland, Ohio, USA.
Funding
This work was supported by the National Institute on Aging (P30-AG062428).
Conflict of Interest
None.
References
- Agarwal, P., Leurgans, S. E., Agrawal, S., Aggarwal, N. T., Cherian, L. J., James, B. D., Dhana, K., Barnes, L. L., Bennett, D. A., & Schneider, J. A. (2023). Association of Mediterranean–DASH intervention for neurodegenerative delay and Mediterranean diets with Alzheimer disease pathology. Neurology, 100(22), e2259–e2268. 10.1212/WNL.0000000000207176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzheimer’s Association. (2023a). 2023 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia, 19(4), 1598–1695. 10.1002/alz.13016 [DOI] [PubMed] [Google Scholar]
- Alzheimer’s Association. (2023b). Differential diagnosis of frontotemporal dementia. https://www.alz.org/professionals/health-systems-medical-professionals/dementia-diagnosis/differential-diagnosis/differential_diagnosis_of_frontotemporal_dementia
- Association for Frontotemporal Degeneration. (2011). AFTD adopts new name, renews mission. AFTD Newsletter, 8(1), 1–4. https://www.theaftd.org/wp-content/uploads/2018/03/AFTD-News-Spring-2011.pdf [Google Scholar]
- Association for Frontotemporal Degeneration. (2023a). Bruce Willis announcement brings FTD awareness to millions worldwide. AFTD Newsletter, 20(1), 1–7. https://www.theaftd.org/aftd-news/spring-2023/ [Google Scholar]
- Association for Frontotemporal Degeneration. (2023b). What is FTD? Disease overview. Author. https://www.theaftd.org/what-is-ftd/disease-overview/ [Google Scholar]
- Beber, B. C., & Chaves, M. L. F. (2013). Evaluation of patients with behavioral and cognitive complaints: Misdiagnosis in frontotemporal dementia and Alzheimer’s disease. Dementia & Neuropsychologia, 7(1), 60–65. 10.1590/S1980-57642013DN70100010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergeron, D., Gorno-Tempini, M. L., Rabinovici, G. D., Santos-Santos, M. A., Seeley, W., Miller, B. L., Pijnenburg, Y., Keulen, M. A., Groot, C., van Berckel, B. N. M., van der Flier, W. M., Scheltens, P., Rohrer, J. D., Warren, J. D., Schott, J. M., Fox, N. C., Sanchez-Valle, R., Grau-Rivera, O., Gelpi, E., & Ossenkoppele, R. (2018). Prevalence of amyloid-beta pathology in distinct variants of primary progressive aphasia. Annals of Neurology, 84(5), 729–740. 10.1002/ana.25333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besser, L. M., & Galvin, J. E. (2020). Diagnostic experience reported by caregivers of patients with frontotemporal degeneration. Neurology Clinical Practice, 10(4), 298–306. 10.1212/CPJ.0000000000000738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blum, D. (2023, February 16). Bruce Willis has frontotemporal dementia, his family announces. The New York Times. https://www.nytimes.com/2023/02/16/well/mind/bruce-willis-frontotemporal-dementia-aphasia.html
- Borghesani, V., Battistella, G., Mandelli, M. L., Welch, A., Weis, E., Younes, K., Neuhaus, J., Grinberg, L. T., Seeley, W. M., Spina, S., Miller, B., Miller, Z., & Gorno-Tempini, M. L. (2020). Regional and hemispheric susceptibility of the temporal lobe to FTLD–TDP type C pathology. NeuroImage: Clinical, 28, 102369. 10.1016/j.nicl.2020.102369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, B. D. (2023, February 16). (Season 42, Episode 136) [TV series episode]. In Johnson E. (Executive Producer), Entertainment Tonight. CBS. [Google Scholar]
- Casaletto, K. B., Staffaroni, A. M., Wolf, A., Appleby, B., Brushaber, D., Coppola, G., Dickerson, B., Domoto-Reilly, K., Elahi, F. M., Fields, J., Fong, J. C., Forsberg, L., Ghoshal, N., Graff-Radford, N., Grossman, M., Heuer, H. W., Hsiung, G. Y., Huey, E. D., Irwin, D., … The ARTFL/LEFFTDS Study. (2020). Active lifestyles moderate clinical outcomes in autosomal dominant frontotemporal degeneration. Alzheimer’s & Dementia, 16(1), 91–105. 10.1002/alz.12001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavicke, D., & O’Leary, J. P. (2001). Lou Gehrig’s death. The American Surgeon, 67(4), 393–395. 10.1177/000313480106700420 [DOI] [PubMed] [Google Scholar]
- Collins, J. D., Henley, S. M. D., & Suarez-Gonzalez, A. (2023). A systematic review of the prevalence of depression, anxiety, and apathy in frontotemporal dementia, atypical and young-onset Alzheimer’s disease, and inherited dementia. International Psychogeriatrics, 35(9), 457–476. 10.1017/S1041610220001118 [DOI] [PubMed] [Google Scholar]
- D’Incecco, J. (Director), Gaines, J. (Director), & Miller, L. (Director). (2023, February 17). (Season 2023, Episode 41) [TV Series Episode]. In Mazzarelli T. & Parkinson T. (Executive Producers), Today. NBC. [Google Scholar]
- Davidson, J. E., Irizarry, M. C., Bray, B. C., Wetten, S., Galwey, N., Gibson, R., Borrie, M., Delisle, R., Feldman, H. H., Hsiung, G. Y., Fornazzari, L., Gauthier, S., Guzman, D., Loy-English, I., Keren, R., Kertesz, A., George-Hyslop, P. S., Wherrett, J., & Monsch, A. U. (2010). An exploration of cognitive subgroups in Alzheimer’s disease. Journal of the International Neuropsychological Society, 16(2), 233–243. 10.1017/S1355617709991160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies, K., & Howe, T. (2020). Experiences of living with primary progressive aphasia: A scoping review of qualitative studies. American Journal of Alzheimer's Disease and Other Dementias, 35, 1533317519886218. 10.1177/1533317519886218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhana, K., Evans, D. A., Rajan, K. B., Bennett, D. A., & Morris, M. C. (2020). Healthy lifestyle and the risk of Alzheimer dementia: Findings from 2 longitudinal studies. Neurology, 95(4), e374–e383. 10.1212/WNL.0000000000009816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl-Schmid, J., Perneczky, R., Koch, J., Nedopil, N., & Kurz, A. (2013). Guilty by suspicion? Criminal behavior in frontotemporal lobar degeneration. Cognitive and Behavioral Neurology, 26(2), 73–77. 10.1097/WNN.0b013e31829cff11 [DOI] [PubMed] [Google Scholar]
- Draper, B., Cations, M., White, F., Trollor, J., Loy, C., Brodaty, H., Sachdev, P., Gonski, P., Demirkol, A., Cumming, R. G., & Withall, A. (2016). Time to diagnosis in young-onset dementia and its determinants: The INSPIRED study. International Journal of Geriatric Psychiatry, 31(11), 1217–1224. 10.1002/gps.4430 [DOI] [PubMed] [Google Scholar]
- Ducharme, S., Price, B. H., Larvie, M., Dougherty, D. D., & Dickerson, B. C. (2015). Clinical approach to the differential diagnosis between behavioral variant frontotemporal dementia and primary psychiatric disorders. The American Journal of Psychiatry, 172(9), 827–837. 10.1176/appi.ajp.2015.14101248 [DOI] [PubMed] [Google Scholar]
- Feldman, H., Levy, A. R., Hsiung, G. Y., Peters, K. R., Donald, A., Black, S. E., Bouchard, R. W., Gauthier, S. G., Guzman, D. A., Hogan, D. B., Kertesz, A., Rockwood, K., & Group, A. S. (2003). A Canadian cohort study of cognitive impairment and related dementias (ACCORD): Study methods and baseline results. Neuroepidemiology, 22(5), 265–274. 10.1159/000071189 [DOI] [PubMed] [Google Scholar]
- Filippini, T., Adani, G., Malavolti, M., Garuti, C., Cilloni, S., Vinceti, G., Zamboni, G., Tondelli, M., Galli, C., Costa, M., Chiari, A., & Vinceti, M. (2020). Dietary habits and risk of early-onset dementia in an Italian case–control study. Nutrients, 12(12), 3682. 10.3390/nu12123682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florentin, P. (Director). (2023, February 17). (Season 2023, Episode 48) [TV series episode]. In R. R. E. (Producer), Fox & Friends. Fox News. [Google Scholar]
- Fripp, S. (Director). (2022, March 31). [TV series episode]. In Thomas S. (Executive Producer), CBS Mornings. CBS. [Google Scholar]
- Fripp, S. (Director). (2023, February 17). (Season 3, Episode 35) [TV series episode]. In Thomas S. (Executive Producer), CBS Mornings. CBS. [Google Scholar]
- Gaines, J. (Director), & Miller, L. (Director). (2022, March 31). (Season 2022, Episode 77) [TV series episode]. In Mazzarelli T. & Parkinson T. (Executive Producers), Today. NBC. [Google Scholar]
- Gorno-Tempini, M. L., Hillis, A. E., Weintraub, S., Kertesz, A., Mendez, M., Cappa, S. F., Ogar, J. M., Rohrer, J. D., Black, S., Boeve, B. F., Manes, F., Dronkers, N. F., Vandenberghe, R., Rascovsky, K., Patterson, K., Miller, B. L., Knopman, D. S., Hodges, J. R., Mesulam, M. M., & Grossman, M. (2011). Classification of primary progressive aphasia and its variants. Neurology, 76(11), 1006–1014. 10.1212/WNL.0b013e31821103e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill, N. T., Mowszowski, L., Naismith, S. L., Chadwick, V. L., Valenzuela, M., & Lampit, A. (2017). Computerized cognitive training in older adults with mild cognitive impairment or dementia: A systematic review and meta-analysis. The American Journal of Psychiatry, 174(4), 329–340. 10.1176/appi.ajp.2016.16030360 [DOI] [PubMed] [Google Scholar]
- Hogan, D. B., Jetté, N., Fiest, K. M., Roberts, J. I., Pearson, D., Smith, E. E., Roach, P., Kirk, A., Pringsheim, T., & Maxwell, C. J. (2016). The prevalence and incidence of frontotemporal dementia: A systematic review. The Canadian Journal of Neurological Sciences, 43(S1), S96–S109. 10.1017/cjn.2016.25 [DOI] [PubMed] [Google Scholar]
- Hopper, M. (Director). (2023, February 16). [TV series episode]. In Crivelli L. (Executive Producer), NBC News NOW. NBC. [Google Scholar]
- Hurley, R. S., Paller, K. A., Rogalski, E. J., & Mesulam, M. M. (2012). Neural mechanisms of object naming and word comprehension in primary progressive aphasia. The Journal of Neuroscience, 32(14), 4848–4855. 10.1523/JNEUROSCI.5984-11.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juneau, J. (2022). Bruce Willis has aphasia and as ‘stepping away’ from acting, family reveals. People Magazine. https://people.com/health/bruce-willis-has-aphasia-stepping-away-from-acting/
- Karnatz, T., Monsees, J., Wucherer, D., Michalowsky, B., Zwingmann, I., Halek, M., Hoffmann, W., & Rene Thyrian, J. (2021). Burden of caregivers of patients with frontotemporal lobar degeneration—A scoping review. International Psychogeriatrics, 33(9), 891–911. 10.1017/S1041610219000176 [DOI] [PubMed] [Google Scholar]
- Kavanaugh, M. (Director). (2023, February 16). [TV series episode]. In Tienabeso S. (Executive Producer), ABC News Live Prime. ABC. [Google Scholar]
- Knopman, D. S., & Roberts, R. O. (2011). Estimating the number of persons with frontotemporal lobar degeneration in the US population. Journal of Molecular Neuroscience, 45(3), 330–335. 10.1007/s12031-011-9538-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kortte, K. B., & Rogalski, E. J. (2013). Behavioural interventions for enhancing life participation in behavioural variant frontotemporal dementia and primary progressive aphasia. International Review of Psychiatry, 25(2), 237–245. 10.3109/09540261.2012.751017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasaponara, S., Marson, F., Doricchi, F., & Cavallo, M. (2021). A scoping review of cognitive training in neurodegenerative diseases via computerized and virtual reality tools: What we know so far. Brain Sciences, 11(5), 528. 10.3390/brainsci11050528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leroy, M., Bertoux, M., Skrobala, E., Mode, E., Adnet-Bonte, C., Le Ber, I., Bombois, S., Cassagnaud, P., Chen, Y., Deramecourt, V., Lebert, F., Mackowiak, M. A., Sillaire, A. R., Wathelet, M., Pasquier, F., Lebouvier, T., Abied, R., Adnet, C., Barois, A., … The Méotis Network. (2021). Characteristics and progression of patients with frontotemporal dementia in a regional memory clinic network. Alzheimer’s Research & Therapy, 13(1), 19. 10.1186/s13195-020-00753-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logroscino, G., Piccininni, M., Graff, C., Hardiman, O., Ludolph, A. C., Moreno, F., Otto, M., Remes, A. M., Rowe, J. B., Seelaar, H., Solje, E., Stefanova, E., Traykov, L., Jelic, V., Rydell, M. T., Pender, N., Anderl-Straub, S., Barandiaran, M., Gabilondo, A., … The FRONTIERS Group. (2023). Incidence of syndromes associated with frontotemporal lobar degeneration in 9 European countries. JAMA Neurology, 80(3), 279–286. 10.1001/jamaneurol.2022.5128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesulam, M. M. (1987). Primary progressive aphasia—Differentiation from Alzheimer’s disease. Annals of Neurology, 22(4), 533–534. 10.1002/ana.410220414 [DOI] [PubMed] [Google Scholar]
- Mesulam, M. M., Gefen, T., Flanagan, M., Castellani, R., Jamshidi, P., Barbieri, E., Sridhar, J., Kawles, A., Weintraub, S., Geula, C., & Rogalski, E. (2023). Frontotemporal degeneration with transactive response DNA-binding protein type C at the anterior temporal lobe. Annals of Neurology, 94(1), 1–12. 10.1002/ana.26677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesulam, M. M., Wieneke, C., Thompson, C., Rogalski, E., & Weintraub, S. (2012). Quantitative classification of primary progressive aphasia at early and mild impairment stages. Brain, 135(Pt 5), 1537–1553. 10.1093/brain/aws080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modirrousta, M., Price, B. H., & Dickerson, B. C. (2013). Neuropsychiatric symptoms in primary progressive aphasia: Phenomenology, pathophysiology, and approach to assessment and treatment. Neurodegenerative Disease Management, 3(2), 133–146. 10.2217/nmt.13.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore, D. G. [@demimoore]. (2022, March 30). To Bruce’s amazing supporters, as a family we wanted to share that our beloved Bruce has been experiencing some health [Photograph]. Instagram. https://www.instagram.com/p/Cbu-mD7LMPg/
- Moreau, J. (2023). Bruce Willis diagnosed with dementia after retiring due to aphasia. Variety Magazine. https://variety.com/2023/film/news/bruce-willis-dementia-aphasia-retire-1235525599/
- Mouton, A., Plonka, A., Fabre, R., Tran, T. M., Robert, P., Macoir, J., Manera, V., & Gros, A. (2022). The course of primary progressive aphasia diagnosis: A cross-sectional study. Alzheimer’s Research & Therapy, 14(1), 64. 10.1186/s13195-022-01007-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalesnik, B. (Director), & Hawley, A. (Director). (2023, February 16). (Season 1, Episode 942). In Verdugo A. (Executive Producer), CBS Evening News with Norah O’Donnell. CBS. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Health Sciences Policy, Committee on Preventing Dementia and Cognitive Impairment, Downey, A., Stroud, C., Landis, S., & Leshner, A. I. (Eds.). (2017). Preventing cognitive decline and dementia: A way forward. National Academies Press (US). 10.17226/24782 [DOI] [PubMed] [Google Scholar]
- Nilsson, C., Landqvist Waldö, M., Nilsson, K., Santillo, A., & Vestberg, S. (2014). Age-related incidence and family history in frontotemporal dementia: Data from the Swedish Dementia Registry. PLoS One, 9(4), e94901. 10.1371/journal.pone.0094901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, A. (2023). Bruce Willis has frontotemporal dementia. Here’s what it is. Time Magazine. https://time.com/6256435/bruce-willis-frontotemporal-dementia/
- Rascovsky, K., Hodges, J. R., Knopman, D., Mendez, M. F., Kramer, J. H., Neuhaus, J., van Swieten, J. C., Seelaar, H., Dopper, E. G., Onyike, C. U., Hillis, A. E., Josephs, K. A., Boeve, B. F., Kertesz, A., Seeley, W. W., Rankin, K. P., Johnson, J. K., Gorno-Tempini, M. L., Rosen, H., & Miller, B. L. (2011). Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain, 134(Pt 9), 2456–2477. 10.1093/brain/awr179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinaugh, G., & Henry, M. L. (2022). Behavioral interventions for primary progressive aphasia. Handbook of Clinical Neurology, 185, 221–240. 10.1016/B978-0-12-823384-9.00011-6 [DOI] [PubMed] [Google Scholar]
- Rogalski, E., Sridhar, J., Rader, B., Martersteck, A., Chen, K., Cobia, D., Thompson, C. K., Weintraub, S., Bigio, E. H., & Mesulam, M. M. (2016). Aphasic variant of Alzheimer disease: Clinical, anatomic, and genetic features. Neurology, 87(13), 1337–1343. 10.1212/WNL.0000000000003165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggero, L., Croot, K., & Nickels, L. (2023). Quality of life ratings and proxy bias in primary progressive aphasia: Two sides to the story? American Journal of Alzheimer’s Disease & Other Dementias, 38, 15333175231177668. 10.1177/15333175231177668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggero, L., Nickels, L., & Croot, K. (2019). Quality of life in primary progressive aphasia: What do we know and what can we do next? Aphasiology, 33(5), 498–519. 10.1080/02687038.2019.1568135 [DOI] [Google Scholar]
- Sabia, S., Fayosse, A., Dumurgier, J., van Hees, V. T., Paquet, C., Sommerlad, A., Kivimäki, M., Dugravot, A., & Singh-Manoux, A. (2021). Association of sleep duration in middle and old age with incidence of dementia. Nature Communications, 12(1), 2289. 10.1038/s41467-021-22354-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage, S. A., Lampe, L. F., & Nickels, L. (2021). No negative impact of word retraining on vocabulary use or clarity of communication in semantic dementia. Neuropsychological Rehabilitation, 33(2), 1–33. 10.1080/09602011.2021.1993934 [DOI] [PubMed] [Google Scholar]
- Schindler, M. (Director). (2022, March 31). (Season 2022, Episode 63) [TV Series Episode]. In McGirl Kieran (Producer), Good morning America. ABC. [Google Scholar]
- Sheetrit, S. (Director). (2023, February 16). (Season 2023, Episode 76). In Spinella M. (Executive Producer), CNN Tonight. CNN. [Google Scholar]
- Shinagawa, S., Nakajima, S., Plitman, E., Graff-Guerrero, A., Mimura, M., Nakayama, K., & Miller, B. L. (2015). Non-pharmacological management for patients with frontotemporal dementia: A systematic review. Journal of Alzheimer’s Disease, 45(1), 283–293. 10.3233/JAD-142109 [DOI] [PubMed] [Google Scholar]
- Sima, R., Soong, K., Gilbert, C., & Cimons, M. (2023). Bruce Willis has frontotemporal dementia: What are the symptoms of FTD? The Washington Post. https://www.washingtonpost.com/wellness/2023/02/16/bruce-willis-frontotemporal-dementia-ftd-symptoms/
- Snowden, J., Neary, D., & Mann, D. (2007). Frontotemporal lobar degeneration: Clinical and pathological relationships. Acta Neuropathologica, 114(1), 31–38. 10.1007/s00401-007-0236-3 [DOI] [PubMed] [Google Scholar]
- Spinelli, E. G., Mandelli, M. L., Miller, Z. A., Santos-Santos, M. A., Wilson, S. M., Agosta, F., Grinberg, L. T., Huang, E. J., Trojanowski, J. Q., Meyer, M., Henry, M. L., Comi, G., Rabinovici, G., Rosen, H. J., Filippi, M., Miller, B. L., Seeley, W. W., & Gorno-Tempini, M. L. (2017). Typical and atypical pathology in primary progressive aphasia variants. Annals of Neurology, 81(3), 430–443. 10.1002/ana.24885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stopford, C. L., Snowden, J. S., Thompson, J. C., & Neary, D. (2008). Variability in cognitive presentation of Alzheimer’s disease. Cortex, 44(2), 185–195. 10.1016/j.cortex.2005.11.002 [DOI] [PubMed] [Google Scholar]
- Taylor-Rubin, C., Croot, K., & Nickels, L. (2021). Speech and language therapy in primary progressive aphasia: A critical review of current practice. Expert Review of Neurotherapeutics, 21(4), 419–430. 10.1080/14737175.2021.1897253 [DOI] [PubMed] [Google Scholar]
- Trachtenberg, D. I., & Trojanowski, J. Q. (2008). Dementia: A word to be forgotten. Archives of Neurology, 65(5), 593–595. 10.1001/archneur.65.5.593 [DOI] [PubMed] [Google Scholar]
- Tsai, R. M., & Boxer, A. L. (2014). Treatment of frontotemporal dementia. Current Treatment Options in Neurology, 16(11), 319. 10.1007/s11940-014-0319-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkmer, A., Rogalski, E., Henry, M., Taylor-Rubin, C., Ruggero, L., Khayum, R., Kindell, J., Gorno-Tempini, M. L., Warren, J. D., & Rohrer, J. D. (2020). Speech and language therapy approaches to managing primary progressive aphasia. Practical Neurology, 20(2), 154–161. 10.1136/practneurol-2018-001921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis, E. H., Moore, D. G., Willis, S. L., Willis, T. B., Willis, M. R., & Willis, E. P. (2023). A statement from the Willis Family. Association for Frontotemporal Degeneration. https://www.theaftd.org/mnlstatement23/ [Google Scholar]
- Zapata-Restrepo, L., Rivas, J., Miranda, C., Miller, B. L., Ibanez, A., Allen, I. E., & Possin, K. (2021). The psychiatric misdiagnosis of behavioral variant frontotemporal dementia in a Colombian sample. Frontiers in Neurology, 12, 729381. 10.3389/fneur.2021.729381 [DOI] [PMC free article] [PubMed] [Google Scholar]