Abstract
Radioactive iodine (RAI) accumulation is commonly used for the detection of metastatic disease posttotal thyroidectomy. However, false-positive results have been reported due to abnormal RAI accumulation in some benign pathologies apart from metastatic sites. Here, we present one such case where false-positive I-131 uptake in the pelvis which localized to the cervix and was attributed to menstruation.
Keywords: Cervix, false positive, radioiodine, thyroid cancer
Introduction
Radioactive iodine (RAI) or I-131 has been used since the 1940s, for the treatment of both benign and malignant thyroid conditions. In differentiated thyroid cancer, it is mainly used in the diagnosis of remnant thyroid tissue, detection of metastatic sites, treatment of RAI avid disease as well as follow-up of the cases. Any focal area of RAI accumulation outside its physiological distribution is considered pathological and needs evaluation.[1] However, certain benign pathologies may show increased RAI accumulation, making their correct identification important to avoid futile interventions.[2] Hereby, we present one such case with abnormal RAI accumulation localizing to the cervix.
Case Report
A 39 -year-old female presented with swelling on the right side of her neck for the last 10 months. The swelling was insidious in onset and slowly progressive. Ultrasonography (USG) neck was done which revealed solid cystic lesion measuring 2.4 cm × 2.2 cm with increased internal vascularity and microcalcification. Subsequently, USG-guided fine-needle aspiration cytology was performed and revealed metastasis from papillary carcinoma of thyroid. The patient then underwent total thyroidectomy with bilateral modified radical neck dissection. Postoperative histopathology revealed pT1aN1b disease. The patient was then referred for I-131 whole body iodine scan 1-month postsurgery. On laboratory evaluation, the patient had serum thyroid-stimulating hormone-68.6 µIU/ml, serum thyroglobulin levels-31.2 ng/ml, and anti-thyroglobulin antibodies was 17.6 U/ml (n < 60). I-131 whole body scan performed 48 h postadministration of 2 mCi of I-131 revealed a focal area of RAI uptake in the thyroid bed, suggestive of thyroid remnant. The patient then underwent remnant ablation with 30 mCi of I-131. Post-therapy scan performed after 5 days revealed a focal area of increased uptake in the pelvic region in addition to the uptake in the thyroid bed [Figure 1a and b]. Single-photon emission computed tomography/computed tomography (SPECT/CT) was done to rule out pelvic metastasis and revealed localization of uptake to the cervix with no corresponding abnormality on CT [Figure 1c-e]. The patient was found to be actively menstruating at the time of posttherapy scan and the uptake was thus attributed to the accumulated I-131 in the menstrual blood. The presence of any lesion was also ruled out with pelvic USG, thus confirming the hypothesis.
Figure 1:
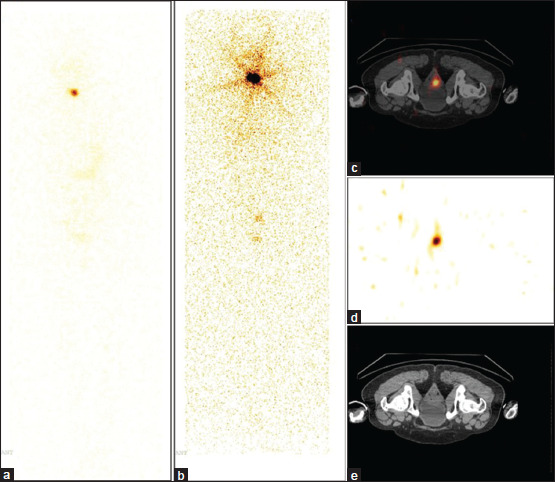
A 39-year-old female case of papillary carcinoma thyroid, posttotal thyroidectomy with bilateral modified radical neck dissection. (a) I-131 WBS anterior view image showing RAI uptake in the thyroid bed, suggestive of thyroid remnant. (b) Posterior view image showing uptake in thyroid remnant, and a focal area of increased uptake in the pelvis. Axial cross-sectional slices (c) Coregistered SPECT/CT (d) SPECT only, and (e) Computed tomography images showing I-131 uptake localizing to the cervix with no corresponding anatomical abnormality. SPECT/CT: Single-photon emission computed tomography/computed tomography, WBS: Whole-body scans, RAI: Radioactive iodine
Discussion
Thyrotropes have high iodine concentration capacity owing to secondary active transport of iodine by sodium iodide symporter and can maintain a thyrotrope: Plasma concentration gradient of up to 100:1.[3] This concentration capacity is the rationale behind the use of RAI for visualization as well as ablation of functioning thyroid tissue (remnant as well as metastatic) in differentiated thyroid cancer.
Physiologically, RAI accumulation in post-thyroidectomy patients is seen in salivary glands, gastric mucosa, liver, and intestine as well as in its excretory pathway, i.e., kidneys, ureter, and bladder. Any focal accumulation of RAI beyond these physiological sites is considered suspicious for the presence of metastatic disease. However, certain benign pathological conditions such as thymic cysts, Meckel's diverticula, nasolacrimal duct obstruction, renal cysts, hepatic cysts, vascular aneurysms, and nabothian cysts can show increased tracer accumulation, leading to unnecessary evaluation.[4,5] Thus, recognition of these pathologies and their differentiation from metastatic disease is essential.
Increased tracer accumulation in the cervix is mainly seen during mensuration as in the case presented. It is attributed to the pooling of menstrual blood containing high concentrations of I-131.[6,7] Although scarce, some literature also suggests there is an increased concentration of iodine (and thus RAI) in the cervical mucus during the progestogenic phase of the menstrual cycle.[8] This increased accumulation of RAI in the cervical mucus can mimic metastatic disease. In the present case, the patient was actively menstruating at the time of posttherapy scan, and thus tracer accumulation can be attributed to the accumulation of blood-containing RAI. The presence of any metastatic disease was ruled out with SPECT/CT of the pelvis and the same was also confirmed with pelvic USG. Thus, I-131 whole-body scans should be reported with the background of histological features as well as tumor markers to avoid unnecessary invasive procedures (diagnostic as well as therapeutic).
Conclusion
I-131 uptake outside the physiological distribution, although considered specific for functional thyroid tissue, may also be seen in certain benign conditions. Correct differentiation of these benign sites from metastatic disease is essential to avoid unnecessary intervention in cases of benign pathologies and to provide appropriate management in cases with metastatic disease. Thus, the interpretation of I-131 scans should be done in an integrated manner taking histological features as well as tumor markers into consideration.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Oh JR, Ahn BC. False-positive uptake on radioiodine whole-body scintigraphy: Physiologic and pathologic variants unrelated to thyroid cancer. Am J Nucl Med Mol Imaging. 2012;2:362–85. [PMC free article] [PubMed] [Google Scholar]
- 2.Wu K, Ozomaro U, Flavell R, Pampaloni M, Liu C. Causes of false-positive radioactive iodine uptake in patients with differentiated thyroid cancer. Curr Radiol Rep. 2021;9:1–11. [Google Scholar]
- 3.Ravera S, Nicola JP, Salazar-De Simone G, Sigworth FJ, Karakas E, Amzel LM, et al. Structural insights into the mechanism of the sodium/iodide symporter. Nature. 2022;612:795–801. doi: 10.1038/s41586-022-05530-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blum M, Tiu S, Chu M, Goel S, Friedman K. I-131 SPECT/CT elucidates cryptic findings on planar whole-body scans and can reduce needless therapy with I-131 in post-thyroidectomy thyroid cancer patients. Thyroid. 2011;21:1235–47. doi: 10.1089/thy.2011.0010. [DOI] [PubMed] [Google Scholar]
- 5.Hannoush ZC, Palacios JD, Kuker RA, Casula S. False positive findings on I-131 WBS and SPECT/CT in patients with history of thyroid cancer: Case series. Case Rep Endocrinol. 2017;2017:8568347. doi: 10.1155/2017/8568347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu L, Chen Y, Tian T, Huang R, Liu B. Physiologic uterine uptake of radioiodine during menstruation demonstrated by SPECT/CT. Clin Nucl Med. 2019;44:975–7. doi: 10.1097/RLU.0000000000002754. [DOI] [PubMed] [Google Scholar]
- 7.Rachinsky I, Driedger A. Iodine-131 uptake in a menstruating uterus: Value of SPECT/CT in distinguishing benign and metastatic iodine-positive lesions. Thyroid. 2007;17:901–2. doi: 10.1089/thy.2007.0084. [DOI] [PubMed] [Google Scholar]
- 8.Parisier HE, Houssay AB, Zapata AC, Valerga AC, Funes JF. I-131-uptake in cervical mucus during the menstrual cycle. Fertil Steril. 1964;15:433–9. doi: 10.1016/s0015-0282(16)35288-8. [DOI] [PubMed] [Google Scholar]


