Abstract
Background
Dry needling the lumbar multifidi is a technique used by physical therapists to effectively treat low back pain. While studies have examined the safety considerations in the upper lumbar spine related to the kidneys and lungs, none have investigated the possibility of entering the spinal canal in this region.
Purpose
The purpose of this cadaveric ultrasound-guided dry needling exploration was to determine if a dry needle can penetrate the ligamentum flavum at the T12/L1 interspace and enter the spinal canal using a paramedian approach in a fresh-frozen, lightly fixed cadaver in the prone position.
Study Design
Cadaveric study.
Methods
The procedure was performed on a cadaver in the prone position. The needle was advanced under ultrasound guidance to determine if a 0.30 x 50 mm dry needle inserted 1.0 cm lateral to the spinous process of T12 and directed medially at a 22-degree angle could penetrate the ligamentum flavum and enter the spinal canal.
Results
As determined via ultrasound, a dry needle can penetrate the ligamentum flavum and enter the spinal canal at the thoracolumbar junction using this technique.
Conclusion
This interprofessional collaboration demonstrates that a dry needle can penetrate the ligamentum flavum to enter the spinal canal at T12/L1 using a documented technique for dry needling the multifidus. A thorough understanding of human anatomy along with the incorporation of available technology, such as ultrasound, may decrease the risk of adverse events when dry needling the multifidi at the thoracolumbar junction.
Level of Evidence
Level IV.
Keywords: multifidus, ultrasound, cadaver, dry needling, safety considerations
INTRODUCTION
Dry needling is a common technique used by physical therapists to treat musculoskeletal pain,1 and needling the muscles around the lumbar spine has been shown to decrease low back pain in patients post-intervention.2–4 Significant and serious adverse events with dry needling have been published5–7; however, they are likely underreported.8 Documented adverse events from needling interventions in areas around the spine include: acute epidural hematoma,5,6,9 post-dural puncture headache,10,11 infection,12,13 lower extremity weakness,14 and numbness into an extremity.14 Other documented adverse events include bleeding, bruising, pain, aggravation of symptoms, nausea, feeling faint, and headaches.14 Currently, no national or international system is available for tracking data on adverse events related to dry needling.15 While significant and serious events from dry needling are not common, therapists should be aware of all potential risks to improve procedures, safety for the individual patients, and the overall standard of practice.
One potential factor that may contribute to the occurrence of adverse events with dry needling is the lack of a universally accepted intervention methodology. Multiple approaches are used in research and instruction of dry needling techniques, which leads to variability in practice and difficulty determining if adverse events are tied to a specific approach.8,16–18 For example, there are a variety of methods described to dry needle the lumbar multifidi, which include variations in both the location of needle placement as well as the angulation of the needle as it is directed toward the targeted tissue.
When targeting the lumbar multifidi, Rainey describes a needle placement within one finger breadth lateral to the spinous process and a needle direction that is just medial to the vertical axis.19 Wang-Price et al. used a needle placement 2.0 cm lateral to the spinous process and angled 20° medially toward the spinous process, as well as a needle placement 4.0 cm lateral to the spinous process with a 45° medial angulation, with both techniques resulting in successful placement of the needle in the lumbar multifidi confirmed on ultrasound imaging.20
Other authors report an inferomedial needle angulation when targeting the lumbar multifidi but are not consistent with all parameters. Variations in parameters include needle placements at 1.0 cm lateral to the spinous process with a 15° inferomedial angulation21 as well as 1.0 cm, or 1 finger breadth lateral placement with an inferomedial angulation without specific information related to the degree of angulation, thereby leaving the technique open to interpretation.18,22 Hannah et al. describe a 1.5 cm needle placement lateral to the spinous process with a 45° inferior and 45° medial angulation of the needle.23 In addition to the medial and inferomedial needle angulation techniques, other techniques include placing the needle 1.0-1.5 cm lateral to the spinous process with no angulation, but rather a straight posterior to anterior direction.23,24 Table 1 outlines the variability that exists related to needle position, needle length, needle angulation, depth of penetration, and patient position for dry needling the lumbar multifidus.
Table 1. Variability of Techniques used by Physical Therapists when Dry Needling the Lumbar Multifidus.
| Reference | Target Muscle | Needle diameter | Needle length | Insertion Depth | Pt position | Needle approach | Needle angle |
|---|---|---|---|---|---|---|---|
| Loizidis et al., 20202 | L2-5 Para-vertebral musclesa | 0.30 mm | 50-75 mm | To lamina | Prone over pillowb | 2 cm lateral to SPc | Inferomedial (~20°) |
| Wang-Price et al., 202016 | L4-S2 multifidi | 0.30 mm | 60-100 mm | To laminad | Prone over pillowb,e | On or near tender point | Inferomedial (~20-30°) |
| Hannah et al., 201623 | L4 multifidi | 0.25-0.30 mmf | N/A | To lamina | Prone | 1.5 cm lateral to SP | 45° inferior & 45° medial |
| 1 cm lateral to SP | 0° | ||||||
| Clark et al., 202122 | T12-L1 multifidi | 0.30 mm | 60 mm | To lamina | Not stated | 1 cm lateral to SP | Inferomedial |
| Koppenhaver et al., 201525 | L3-L5 multifidi | 0.30 mm | 50-60 mm | To lamina | Prone | 1.5 cm lateral to SP | Inferomedial (~20°) |
| Puentedura et al., 201726 | L4 multifidi | 0.30 mm | 40-50 mm | To lamina | Prone | 1.5 cm lateral to SP | Inferomedial (~20°) |
| Wang-Price et al., 202220 | L4-L5 multifidi | 0.30 mm | 100 mm | Bony backdropg | Prone over pillowb | 2.0 cm lateral to SP | 20° medial |
| 4.0 cm lateral to SP | 45° medial | ||||||
| Rainey 201319 | L3 & L5 multifidi | 0.25 mm | 60 mm | To lamina | Prone over pillowb | Within 1 finger breadth from midline | Just medial to vertical axis |
| Koppenhaver 201521 | L3-L5 multifidi | .30mm | 50-60 mm | To multifidus | Prone | 1 cm lateral to SP | Inferomedial 15° |
aParavertebral muscles included: multifidus, erector spinae, iliocostalis lumborum, thoracolumbar fascia
bThe pillow is under the patient’s abdomen
cSP = Spinous Process
d Not specified but mentioned standardizing depth by stopping at bony lamina of vertebrae
e Not specifically stated in dry needling procedure, but was the position for other testing procedures
fResearchers used craft needle for dissection purposes but stated the typical dry needling procedure would be with 0.25-0.30mm
gTo bony backdrop or until entire shaft of needle is completely subcutaneous
Despite the variability that exists in needling technique, dry needling of the multifidi has been considered a safe technique due to the ability of the vertebral lamina to serve as a protective barrier for the spinal canal, preventing inadvertent needling into the spinal canal. Several studies have examined the accuracy of needle placement in the lumbar multifidi at L4-518,21 and the safety considerations related to nearby structures, such as the kidneys and lungs,24 but none have investigated the possibility of entering the spinal canal in the upper lumbar region. Spinal canal perforation is a risk and has been demonstrated in the upper cervical spine.27 Additionally, acute cervical epidural hematoma has occurred following dry needling5,6 and may occur in other areas as well. The cadaveric dry needling technique described in this commentary highlights one of the multiple, documented approaches for the lumbar multifidi and sought to determine if a significant safety vulnerability exists.
The idea for this collaboration between physical therapy and certified registered nurse anesthetist (CRNA) faculty originated during a discussion on the distinctions between lumbar punctures performed by anesthesia providers and dry needling techniques executed by physical therapists on the multifidi. While the classic approaches and needle types for these two procedures differ, it raises the question of whether a dry needling procedure, when conducted in a manner described as safe and effective, can potentially breach the spinal canal.19,20 Table 2 compares a lumbar puncture technique and dry needling techniques targeting the lumbar multifidi.
Table 2. Comparison of Techniques Used in a Lumbar Puncture Performed by an Anesthesia Provider and Dry Needling the Lumbar Multifidi Performed by a Physical Therapist.
| Lumbar Puncture | Dry Needling Multifidi | |
|---|---|---|
| Needle diameter (gauge) | 20-22 gauge | 0.25-0.30 mm |
| Needle length | 9 cm | 40-100 mm |
| Patient position | Sitting or side-lying with flexion of the spine | Prone or prone over pillow |
| Needle approach | Midline (in the interspinous space) In some cases, a paramedian (off midline) approach is useda |
1-4 cm lateral to spinous process |
| Needle angle | Slightly cephalad. In some cases, medially and superiorlya |
0-45 degrees Medial or inferomedial |
| Use of imaging to ensure proper placement | Ultrasound-assisted techniquesb | Not a standard practice |
a In certain instances, such as increased age and spinal deformity, providers may employ a paramedian approach in which the spinal needle is placed off midline and directed medially and superiorly to avoid the interspinous space
b Authors have also described ultrasound-assisted techniques to determine the interspinous level, midline, and depth to the ligamentum flavum28
The purpose of this collaborative cadaveric ultrasound-guided examination of dry needling was to determine if a dry needle can penetrate the ligamentum flavum at T12/L1 interspace and enter the spinal canal using a paramedian approach in a fresh-frozen, lightly fixed cadaver in the prone position.
METHODS
The procedure was performed at Middle Tennessee School of Anesthesia on an 88 y/o female donor by a certified registered nurse anesthetist with over 20 years of diagnostic ultrasound imaging experience and 15 years performing and teaching regional anesthesia. The fresh/lightly embalmed donor was received via the Willed Body Program at The University of North Texas Health Science Center. Exemption from Institutional Review Board approval was granted by Advarra IRB (Pro00070509).
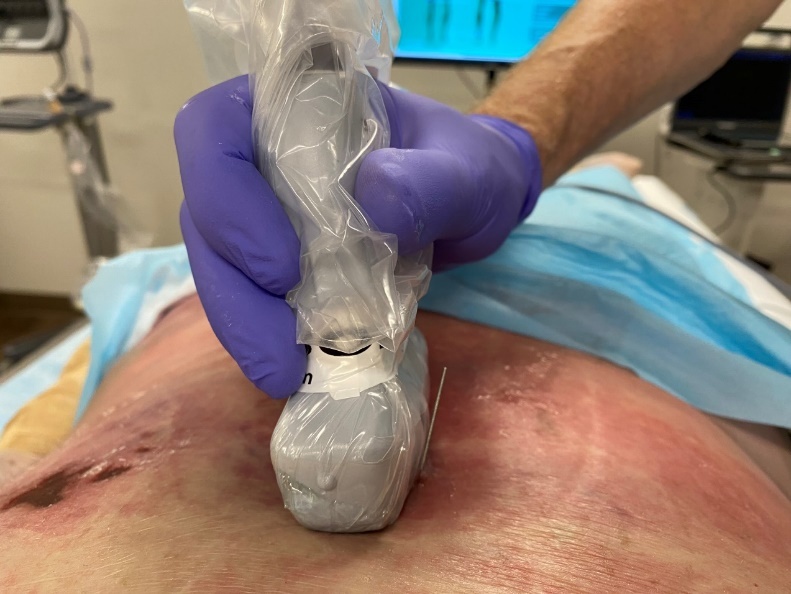
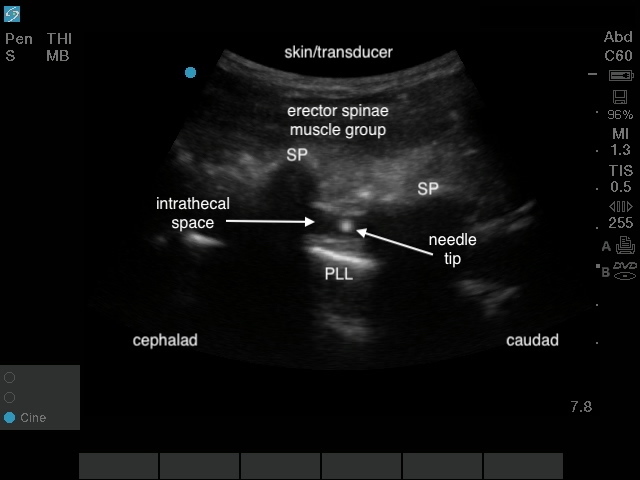
The cadaver was placed in a prone position. A Sonosite Edge II ultrasound system with an rC60xi 5-2 MHz curvilinear array transducer (Bothell, WA) was placed in a parasagittal orientation with the orientation indicator facing cephalad. The sacrum, L5-S1 interspace, and L5 spinous process were identified. The transducer was slid cephalad until the interspace between T12 and L1 was identified. An AGUPUNT APS 0.30 x 50 mm dry needle was inserted approximately 1.0 cm lateral to the spinous process of T12 (Figure 1) and was directed medially at a 22-degree angle (Figure 2). The needle was advanced under ultrasound guidance to determine if it could penetrate the ligamentum flavum to enter the spinal canal.
Figure 1. Needle inclination demonstrates ~22-degree medial angle.

Figure 2. Ultrasound guidance set up.
RESULTS
As Figure 3 and Figure 4 illustrate, a 0.30 x 50 mm dry needle inserted approximately 1.0 cm lateral to the spinous process of T12 and directed medially at a 22-degree angle can pass between adjacent vertebral laminae and penetrate the ligamentum flavum to enter the spinal canal. Please reference Supplemental File 1 for video evidence.
Figure 3. Ultrasound image of the spine in parasagittal orientation; SP - spinous process, PLL – posterior longitudinal ligament.
CONCLUSION
While adverse effects resulting from entering the spinal canal during a dry needling procedure are rare, this interprofessional collaboration demonstrates some important considerations for the clinician when performing dry needling. First, there is significant variability in the techniques described for dry needling the multifidus with no clear consensus regarding which technique is most effective and safe. Many techniques described also lack specific information regarding needle angulation, thereby leaving the exact technique open to interpretation, and this ambiguity has the potential to lead to variations in clinician needling technique and a resulting decrease in the certainty of a safe needle path and placement. This cadaveric study demonstrates that a 0.30 x 50 mm dry needle is able to penetrate the ligamentum flavum and enter the spinal canal at T12/L1 using a dry needling technique described for the multifidus, and therefore, either purposeful or inadvertent deviations in needle placement in this area of the spine have the potential to cause neurologic injury. While a comprehensive understanding of human anatomy is crucial for dry needling, the utilization of ultrasound has the potential to enhance the precision of dry needling techniques in vulnerable areas, such as the thoracolumbar junction, and may contribute to further risk reduction. The authors recommend that future studies explore various needle lengths and positions, as well as other regions of the spine and patient positions to explore the risk of a dry needle entering the spinal canal under these conditions.
Conflicts of interest
The authors declare no conflicts of interest.
Supplementary Material
US Imaging
References
- Dry needling in the management of musculoskeletal pain. Kalichman L., Vulfsons S. Sep 1;2010 The Journal of the American Board of Family Medicine. 23(5):640–646. doi: 10.3122/jabfm.2010.05.090296. doi: 10.3122/jabfm.2010.05.090296. [DOI] [PubMed] [Google Scholar]
- The effects of dry needling on pain relief and functional balance in patients with sub-chronic low back pain. Loizidis Theodoros, Nikodelis Thomas, Bakas E., Kollias I. Nov 11;2020 Journal of Back and Musculoskeletal Rehabilitation. 33(6):953–959. doi: 10.3233/bmr-181265. doi: 10.3233/bmr-181265. [DOI] [PubMed] [Google Scholar]
- Is dry needling effective for low back pain?: A systematic review and PRISMA-compliant meta-analysis. Hu Han-Tong, Gao Hong, Ma Rui-Jie, Zhao Xiao-Feng, Tian Hong-Fang, Li Lu. Jun;2018 Medicine. 97(26):e11225. doi: 10.1097/md.0000000000011225. doi: 10.1097/md.0000000000011225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evidence for dry needling in the management of myofascial trigger points associated with low back pain: A systematic review and meta-analysis. Liu Lin, Huang Qiang-Min, Liu Qing-Guang, Thitham Nguyen, Li Li-Hui, Ma Yan-Tao, Zhao Jia-Min. Jan;2018 Archives of Physical Medicine and Rehabilitation. 99(1):144–152.e2. doi: 10.1016/j.apmr.2017.06.008. doi: 10.1016/j.apmr.2017.06.008. [DOI] [PubMed] [Google Scholar]
- An acute cervical epidural hematoma as a complication of dry needling. Lee Jun-Hwan, Lee Hyangsook, Jo Dae-Jean. Jun;2011 Spine. 36(13):E891–E893. doi: 10.1097/brs.0b013e3181fc1e38. doi: 10.1097/brs.0b013e3181fc1e38. [DOI] [PubMed] [Google Scholar]
- Acute spinal epidural hematoma as a complication of dry needling: A case report. Berrigan William A., Whitehair Curtis L., Zorowitz Richard D. Feb 22;2019 PM&R. 11(3):313–316. doi: 10.1016/j.pmrj.2018.07.009. doi: 10.1016/j.pmrj.2018.07.009. [DOI] [PubMed] [Google Scholar]
- Pneumothorax complication of deep dry needling demonstration. Cummings M, Ross-Marrs R, Gerwin R. Dec;2014 Acupuncture in Medicine. 32(6):517–519. doi: 10.1136/acupmed-2014-010659. doi: 10.1136/acupmed-2014-010659. [DOI] [PubMed] [Google Scholar]
- Lack of standardization in dry needling dosage and adverse event documentation limits outcome and safety reports: a scoping review of randomized clinical trials. Kearns Gary A., Brismée Jean-Michel, Riley Sean P., Wang-Price Sharon, Denninger Thomas, Vugrin Margaret. 2023Journal of Manual & Manipulative Therapy. 31(2):72–83. doi: 10.1080/10669817.2022.2077516. doi: 10.1080/10669817.2022.2077516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acute spinal epidural hematoma after acupuncture: Personal case and literature review. Domenicucci Maurizio, Marruzzo Daniele, Pesce Alessandro, Raco Antonino, Missori Paolo. Jun;2017 World Neurosurgery. 102:695.e11–695.e14. doi: 10.1016/j.wneu.2017.03.125. doi: 10.1016/j.wneu.2017.03.125. [DOI] [PubMed] [Google Scholar]
- Development of postdural puncture headache following therapeutic acupuncture using a long acupuncture needle. Jo Dae-Jean, Lee Bong Jae, Sung Joon Kyung, Yi Jae-Woo. 2010Journal of Korean Neurosurgical Society. 47(2):140. doi: 10.3340/jkns.2010.47.2.140. doi: 10.3340/jkns.2010.47.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post-dural puncture headache following acupotomy using "Wonli-acupuncture needle" - A case report. Kim Hyungtae, Lee Cheol-Hyeong, Kim Yeon-Dong. Jul 31;2018 Anesthesia and Pain Medicine. 13(3):314–318. doi: 10.17085/apm.2018.13.3.314. doi: 10.17085/apm.2018.13.3.314. [DOI] [Google Scholar]
- Deep spine infection after acupuncture in the setting of spinal instrumentation. Callan Alexandra K., Bauer Jennifer M., Martus Jeffrey E. Mar;2016 Spine Deformity. 4(2):156–161. doi: 10.1016/j.jspd.2015.09.045. doi: 10.1016/j.jspd.2015.09.045. [DOI] [PubMed] [Google Scholar]
- Paraplegia caused by spinal infection after acupuncture. Bang M S, Lim S H. 2006Spinal Cord. 44(4):258–259. doi: 10.1038/sj.sc.3101819. doi: 10.1038/sj.sc.3101819. [DOI] [PubMed] [Google Scholar]
- Adverse events associated with therapeutic dry needling. Boyce David, Wempe Hannah, Campbell Courtney, Fuehne Spencer, Zylstra Edo, Smith Grant, Wingard Christopher, Jones Richard. Feb;2020 International Journal of Sports Physical Therapy. 15(1):103–113. doi: 10.26603/ijspt20200103. doi: 10.26603/ijspt20200103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dry needling in physical therapy practice: Adverse events. Valdes Vanessa. Nov 1;2019 International Journal of Physical Therapy & Rehabilitation. 5(2) doi: 10.15344/2455-7498/2019/157. doi: 10.15344/2455-7498/2019/157. [DOI] [Google Scholar]
- Short-term effects of two deep dry needling techniques on pressure pain thresholds and electromyographic amplitude of the lumbosacral multifidus in patients with low back pain - a randomized clinical trial. Wang-Price Sharon, Zafereo Jason, Couch Zach, Brizzolara Kelli, Heins Taylor, Smith Lindsey. Jan 17;2020 Journal of Manual & Manipulative Therapy. 28(5):254–265. doi: 10.1080/10669817.2020.1714165. doi: 10.1080/10669817.2020.1714165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The effect of dry needling compared to lumbar spine mobilization on pain, functional disability, quadratus lumborum and lumbar multifidus function, lumbar range of motion and pain pressure threshold in patients with non-specific chronic low back pain: Study protocol for a randomized controlled trial. Mirzaie Hamide, Pourahmadi Mohammad Reza, Ayoubpour Mohamad Reza, Firouze Bahare. Dec 5;2022 Research Square. doi: 10.21203/rs.3.rs-2153991/v1. doi: 10.21203/rs.3.rs-2153991/v1. [DOI]
- Dommerholt J., de las Penas C.F. Trigger Point Dry Needling E-Book: Trigger Point Dry Needling E-Book. Elsevier Health Sciences; [Google Scholar]
- The use of trigger point dry needling and intramuscular electrical stimulation for a subject with chronic low back pain: a case report. Rainey C.E. 2013Int J Sports Phys Ther. 8(2):145–161. [PMC free article] [PubMed] [Google Scholar]
- Validity and reliability of dry needle placement in the deep lumbar multifidus muscle using ultrasound imaging: an in-vivo study. Wang-Price Sharon S., Etibo Kristen N., Short Alicia P., Brizzolara Kelli J., Zafereo Jason A. Mar 22;2022 Journal of Manual & Manipulative Therapy. 30(5):284–291. doi: 10.1080/10669817.2022.2051239. doi: 10.1080/10669817.2022.2051239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baseline examination factors associated with clinical improvement after dry needling in individuals with low back pain. Koppenhaver Shane L., Walker Michael J., Smith Ryan W., Booker Jacquelynn M., Walkup Isaac D., Su Jonathan, Hebert Jeffrey J., Flynn Timothy. Aug;2015 Journal of Orthopaedic & Sports Physical Therapy. 45(8):604–612. doi: 10.2519/jospt.2015.5801. doi: 10.2519/jospt.2015.5801. [DOI] [PubMed] [Google Scholar]
- The effects of dry needling to the thoracolumbar junction multifidi on measures of regional and remote flexibility and pain sensitivity: A randomized controlled trial. Clark Nicole G., Hill Cheryl J., Koppenhaver Shane L., Massie Thomas, Cleland Joshua A. Jun;2021 Musculoskeletal Science and Practice. 53:102366. doi: 10.1016/j.msksp.2021.102366. doi: 10.1016/j.msksp.2021.102366. [DOI] [PubMed] [Google Scholar]
- Comparison of two angles of approach for trigger point dry needling of the lumbar multifidus in human donors (cadavers) Hannah Mary C., Cope Janet, Palermo Alec, Smith Walker, Wacker Valerie. Dec;2016 Manual Therapy. 26:160–164. doi: 10.1016/j.math.2016.08.008. doi: 10.1016/j.math.2016.08.008. [DOI] [PubMed] [Google Scholar]
- Safety of dry needling to the upper lumbar spine: a pilot cadaver study. Mansfield C J, Harr M, Briggs M, Onate J, Boucher L C. 2020Journal of Manual & Manipulative Therapy. 28(2):111–118. doi: 10.1080/10669817.2019.1708593. doi: 10.1080/10669817.2019.1708593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Changes in lumbar multifidus muscle function and nociceptive sensitivity in low back pain patient responders versus non-responders after dry needling treatment. Koppenhaver Shane L., Walker Michael J., Su Jonathan, McGowen Jared M., Umlauf Lindsey, Harris Kevin D., Ross Michael D. Dec;2015 Manual Therapy. 20(6):769–776. doi: 10.1016/j.math.2015.03.003. doi: 10.1016/j.math.2015.03.003. [DOI] [PubMed] [Google Scholar]
- Immediate changes in resting and contracted thickness of transversus abdominis after dry needling of lumbar multifidus in healthy participants: A randomized controlled crossover trial. Puentedura Emilio J., Buckingham Sarah J., Morton Daniella, Montoya Crystal, Fernandez de las Penas Cesar. Oct;2017 Journal of Manipulative and Physiological Therapeutics. 40(8):615–623. doi: 10.1016/j.jmpt.2017.06.013. doi: 10.1016/j.jmpt.2017.06.013. [DOI] [PubMed] [Google Scholar]
- Influence of clinical experience on accuracy and safety of obliquus capitus inferior dry needling in unembalmed cadavers. Kearns Gary A., Hooper Troy L., Brismée Jean-Michel, Allen Brad, Lierly Micah, Gilbert Kerry K., Pendergrass Timothy J., Edwards Deborah. 2022Physiotherapy Theory and Practice. 38(12):2052–2061. doi: 10.1080/09593985.2021.1901326. doi: 10.1080/09593985.2021.1901326. [DOI] [PubMed] [Google Scholar]
- Ultrasound-facilitated epidurals and spinals in obstetrics. Carvalho Jose Carlos Almeida. Mar;2008 Anesthesiology Clinics. 26(1):145–158. doi: 10.1016/j.anclin.2007.11.007. doi: 10.1016/j.anclin.2007.11.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
US Imaging


