Abstract
Background
Acetabular dysplasia (AD) is defined as a structurally deficient acetabulum and is a well-recognized cause of hip pain in young adults. While treatment of severe AD with a periacetabular osteotomy has demonstrated good long-term outcomes, a trial of non-operative management is often recommended in this population. This may be especially true in patients with milder deformities. Currently, there is a paucity of research pertaining to non-operative management of individuals with AD.
Purpose
To present expert-driven non-operative rehabilitation guidelines for use in individuals with AD.
Study Design
Delphi study
Methods
A panel of 15 physiotherapists from North America who were identified as experts in non-operative rehabilitation of individuals with AD by a high-volume hip preservation surgeon participated in this Delphi study. Panelists were presented with 16 questions regarding evaluation and treatment principles of individuals with AD. A three-step Delphi method was utilized to establish consensus on non-operative rehabilitation principles for individuals presenting with AD.
Results
Total (100%) participation was achieved for all three survey rounds. Consensus, defined a piori as > 75%, was reached for 16/16 questions regarding evaluation principles, activity modifications, appropriate therapeutic exercise progression, return to activity/sport criteria, and indications for physician referral.
Conclusion
This North American based Delphi study presents expert-based consensus on non-operative rehabilitation principles for use in individuals with AD. Establishing guidelines for non-operative management in this population will help reduce practice variation and is the first step in stratifying individuals who would benefit from non-operative management. Future research should focus on patient-reported outcomes and rate of subsequent surgical intervention to determine the success of the guidelines reported in this study.
Level of Evidence
Level V
Keywords: acetabular dysplasia, rehabilitation, consensus statement, return to sport
BACKGROUND
Acetabular dysplasia (AD) is defined as a structurally deficient acetabulum, both in shape and orientation, resulting in poor coverage of the femoral head and is a well-recognized cause of hip pain in young adults.1–4 As a result of poor acetabular coverage, excessive wear on the acetabular articular cartilage and labrum can occur to potentially produce degenerative changes.5–8 Without appropriate management, AD can lead to severe pain and disability.9,10
Acetabular dysplasia may result in hip osteoarthritis due to the increased shear forces and loading of the acetabulum and labrum.11,12 The labrum attenuates 1-2% of the joint load in a normal hip during gait. However, the labrum is responsible for 4-11% of the total joint load in an individual with AD secondary to increased antero-superior loading of the acetabulum.13,14 Individuals with AD have also been shown to demonstrate muscle strength deficits, as well as iliopsoas and adductor related pain 56%.15 While treatment of severe AD with a periacetabular osteotomy has demonstrated good long-term outcomes, a trial of non-operative management is often recommended in this population.16–18 This is especially true in those with mild deformities. The role of non-operative rehabilitation in an individual with AD is to re-establish strength and functional control of the lumbopelvic and hip musculature to improve dynamic stability of the hip and lower extremity in the setting of osseous instability as well as to provide activity modification strategies to reduce hip joint irritability.
Currently, there is a lack of research pertaining to non-operative management of individuals with AD. Establishing expert-based non-operative rehabilitation recommendations, including initial evaluation principles, activity modifications, therapeutic exercise progression, return to activity criteria, and indications for physician referral, will provide guidance and reduce variation in a practice area where research is lacking. Additionally, this study will set the groundwork to determine those who are most likely to benefit from non-operative rehabilitation. The purpose of this study is to present expert-driven non-operative rehabilitation guidelines for use in individuals with AD.
METHODS
Delphi Panel
The panel of experts who participated in this study consisted of 15 physiotherapists who were identified as experts in the non-operative physiotherapy management of individuals with AD. To avoid bias, panelists were selected from various geographic locations across the United States and Canada. Participants were selected based on the following criteria, including (1) identification as an expert in non-operative management of individuals with AD by a high-volume hip preservation surgeon and (2) treating at least 20 patients diagnosed with AD per year. Participants were blinded for the entirety of the study.
Delphi Structure and Data Collection
A three-step classic Delphi method was used for the current study. Methods are similar to those described by Disantis et al.19 In summary, panelists were presented with three iterative survey rounds via an emailed link. For each survey round, analysis of participants responses was completed by two study members (AD and RM). Any disagreements were resolved by a third team member (MM). Survey responses were deidentified for analysis.
Panelists were presented with 16 free-response questions on 9 topics regarding non-operative rehabilitation principles for AD. The topic areas are listed below:
Initial evaluation principles
Activity limitations
Therapeutic exercise progression
Lumbopelvic and lower extremity neuromuscular control
Rehabilitation of the hip flexor complex
Muscle stretching principles
Cardiovascular fitness
Return to recreational activity/sports
Referral back to a hip specialist
During the first survey round, responses were coded for common thematic content. Common responses reported by > 50% of panelists were considered modal, while common responses reported by >35% of panelists formed a second tier of responses. During the second survey round, panelists received nine topic related questions and were asked to agree or disagree with the modal response. Those who disagreed were provided a response including the second-tier items as well as the option for free text. The same process was repeated for round three. Consensus for 15/16 questions was reached in survey round two. Consensus for 16/16 questions was reached in survey round three.
RESULTS
The expert panel in the current study consisted of 15 physiotherapists who were identified as experts in the non-operative physiotherapy management of individuals with AD. All 15 therapists (100%) participated in the three Delphi rounds. Consensus was achieved for 100% of the 16 questions provided to the expert panel regarding non-operative rehabilitation principles for AD.
Initial Evaluation Principles (Range of Motion, Muscle Strength, Special Tests, and Functional Tests)
14/15 (93%) of panelists agreed that hip flexion and hip internal (IR) and external rotation ER, in supine and prone, ROM measurements are the most important. One dissenting panelist felt that hip abduction should also be measured.
14/15 (93%) of panelists agreed that muscle strength measures for the hip abductors, hip extensors, deep rotators, and core are the most important. One dissenting panelist felt that the quadriceps strength should also be measured.
15/15 (100%) of panelists agreed that a battery of special tests, including flexion/adduction/internal rotation (FADIR), flexion/abduction/external rotation (FABER), log roll, and apprehension testing should be utilized.
15/15 (100%) of panelists agreed that SL activities should be utilized to assess functional control. Examples of functional tests included a SL stance, SL squat, and SL step down.
Activity Modifications
15/15 (100%) of panelists agreed that activities that do not increase pain should be permitted and painful activities should be modified or discontinued.
Therapeutic Exercise Progression
15/15 (100%) of panelists agreed that progression from local to global exercise should be based upon quality of movement and irritability of the hip joint. Examples of quality of movement parameters included adequate muscle activation and minimal compensatory strategies.
14/15 (93%) of panelists agreed that progression from isometric to concentric exercises should be based on reported pain level and progression from concentric to eccentric exercises should be based on quality of movement. Examples of quality of movement included adequate muscle activation through palpation and minimal compensatory strategies. One dissenting panelist thought that progression from isometrics should be initiated as soon as possible, incorporating these exercises with concentric exercises to fatigue.
Lumbopelvic and Lower extremity Neuromuscular Control
15/15 (100%) of panelists agreed these tasks should challenge both the pelvis and lower quarter with a focus on SL control. These tasks should include both static and multidirectional tasks and be progressed based on quality of movement, beginning in low level positions progression to high level positions. Exercise examples to facilitate lumbopelvic neuromuscular control should include transversus abdominis firing in various positions while exercises to facilitate lower extremity neuromuscular control should include double and SL activities. All panelists (100%) agreed progression from double to SL activities are appropriate when the patient exhibits no trunk or pelvic compensations during double leg activities and the patient can maintain pelvic and lower extremity control during a basic SL task.
Rehabilitation of the Hip Flexor Complex
15/15 (100%) of panelists agreed therapeutic exercise should begin only after the patient has demonstrated an improvement in posterolateral hip muscle strength and a reduction of hip joint irritability. These exercises should begin in a short lever (knee flexed) position, when appropriate.
14/15 (93%) of panelists agreed that these exercises may only be necessary based on sporting demands and be used only in the setting of tolerance to short lever hip flexion exercises and reduced hip irritability. Examples of sports that may require prescription of long lever exercises including dancers. One dissenting panelist thought that long lever exercises should be utilized with all patients if there is no pain with hip flexor muscle activation.
Muscle Stretching Principles
13/15 (87%) of panelists agreed muscle stretching should not be a focus of rehabilitation as hip dysplasia is a diagnosis related to joint instability. Two dissenting panelists thought that muscle stretching should be incorporated based upon findings of physical examination.
Cardiovascular Fitness
15/15 (100%) of panelists agreed low impact activities should be encouraged when pain-free. Examples of such activities include cycling and swimming (with a pool buoy if necessary). Higher impact cardiovascular activities may be initiated as strength improves and hip joint irritability decreases.
Return to Recreational Activity/Sports
14/15 (93%) of panelists agreed individuals may begin running when they demonstrate a decrease in hip joint irritability, appropriate pelvic and lower extremity neuromuscular control during SL activities, and a normal gait pattern with ambulation. One dissenting panelist recommended the use of functional testing including the Vail Sport Test and the Selective Functional Movement Assessment (SFMA) should be utilized in conjunction with these measures.
15/15 (100%) of panelists agreed individuals may begin plyometric exercises when they report minimal to no pain and appropriate pelvic and LE neuromuscular control during all running and low-level agility tasks.
15/15 (100%) of panelists agreed individuals may be cleared for full return to sports when they demonstrate adequate pelvic and LE neuromuscular control during all SL tasks, normalized strength, and tolerance to all sport specific tasks, including running and plyometrics.
Referral to a Physician Hip Specialist
13/15 panelists agreed a patient should be referred to a physician specializing in hip-related injuries if they are exhibiting no decrease in symptoms despite improved strength and neuromuscular control after 4-8 weeks of physiotherapy. Two dissenting panelists felt that individuals should undergo at least 12 weeks of therapy before referring to a physician hip specialist. The patient may be referred to a physician hip specialist for an initial or return consultation depending on the route physical therapy management was initiated.
DISCUSSION
A trial of physiotherapy to improve strength and neuromuscular control is often recommended before surgical intervention in individuals presenting with AD. Currently, there is no consensus regarding non-operative rehabilitation principles, including evaluation, therapeutic exercise and neuromuscular control recommendations, return to activity criteria, and criteria for referral back to a hip specialist, for individuals with AD. This Delphi study was conducted to establish expert-based rehabilitation principles for individuals presenting to physiotherapy for management of AD.
Initial Evaluation Principles
Range of Motion
Consensus Point: During an initial evaluation for an individual presenting for non-operative management of AD, hip flexion and hip IR and ER, in supine and prone, are the most important ranges of motion to measure.
Assessment of hip ROM is an important element of an initial physiotherapy evaluation. The panelists recommend a through side-to-side comparison of hip ROM, with a focus on hip flexion and hip IR and ER ROM. Individuals with AD have been shown to demonstrate normal or increased hip ROM.20,21 Careful attention should be paid the end of physiologic hip flexion ROM, ensuring that there are no compensatory movements of the lumbar spine during this measurement. Additionally, hip IR and ER ROM should be measured in both the supine with the hip and knee flexed to 90 degrees as well as in prone with the hip in neutral flexion/extension. Screening of hip rotation in the prone position reduces possibility of ROM restriction due to femoral head neck offset and therefore may allow for better assessment of the bony structure of the femoroacetabular articulation, specifically the presence of femoral version.22 Increased hip IR may indicate the presence of femoral anteversion, while increased hip ER may indicate the presence of femoral retroversion.23,24 Holm et al.25 reported hip rotation ROM has good reliability in screening for femoral version. Additionally, Uding et al.26 report a 20 degree difference between hip IR and ER ROM when measured prone may be suggestive of abnormal femoral version.26 Femoral anteversion in the presence of AD may further decrease the stability of the hip joint and progression of symptoms. Li et al.27 reported individuals with AD and concomitant femoral anteversion demonstrate a significantly greater incidence of OA.
Strength
Consensus Point: During an initial evaluation for an individual presenting for non-operative management of AD, the hip abductors, hip extensors, deep rotators, and core musculature are the most important muscle groups to strength test.
Decreased strength of the lumbopelvic and posterolateral hip complex may lead to a reduction in hip stability. In the setting of osseous insufficiency secondary to AD, muscular strength may plan an even larger role by providing dynamic stability to the hip joint. The gluteus medius, gluteus maximus, deep rotators, and core musculature are key stabilizers of the hip joint and should be assessed during an initial physiotherapy evaluation in an individual with AD.28
In conjunction with the gluteus maximus and deep rotators, the gluteus medius muscle controls transverse and frontal plane motion of the femur, preventing femoral adduction and internal rotation, while the core musculature assists with maintaining neutral pelvic and spinal alignment.29,30
Given their role in lumbopelvic stability, the panelists recommend strength testing of the hip abductor, hip extensor, and deep rotator muscles through manual muscle testing or handheld dynamometry. Core musculature may be evaluated through performance of a plank and side plank, assessing for inability to maintain proper form over 45-seconds. The plank and side plank exercises were chosen as they are a widely utilized measure of isometric core strength. While the strength deficits associated with other non-arthritic hip disorders, such as femoroacetabular impingement, has been shown in the literature, there is little research assessing the strength deficits associated with AD.31,32 In a study of 46 men and 49 women with symptomatic AD, Wang et al.33 reported hip abductor muscle strength was decreased compared to the contralateral, asymptomatic hip during isokinetic strength testing.
Special Tests
Consensus Point: During an initial evaluation for an individual presenting for non-operative management of AD, special tests including FADIR, FABER, log roll, and apprehension testing should be utilized.
While no single special test exists to evaluate for the presence of AD, a cluster of examination findings, along with the individuals subjective report, may indicate the presence of intra-articular hip pain and concomitant hip instability associated with AD. The FADIR and FABER tests are commonly utilized to assess for the presence of intra-articular hip pain in this population. A systematic review by Caliesch et al.34 assessed the diagnostic accuracy of clinical tests for femoroacetabular impingement and found the FADIR test had a sensitivity of 0.96 (0.91-0.99) and a specificity of 0.11 (0.06-0.02) and the authors also reported a sensitivity of 0.6 (0.15 to 0.95) and a specificity of 0.2 (0.10 to 0.35). Therefore, these tests should be utilized to screen for the presence of intra-articular pain, not identify a specific pathology. Following identification of intra-articular hip pain, the use of apprehension testing may assist clinicians in identifying the presence of hip joint instability. Hoppe et al.35 analyzed three physical examination maneuvers to detect the presence of instability and found the abduction-hyperextension-external rotation test was the most accurate with a sensitivity and specificity of 80.6% and 89.4%, respectively. A systematic review by Cohen et al.36 found 65% of patients with a diagnosis of hip instability reported the presence of anterior apprehension in a position of combined hip extension and external rotation.
Functional Control
Consensus Point: During an initial evaluation for an individual presenting for non-operative management of AD, SL activities such as a SL stance, SL squat, an/or step down should be utilized to assess functional control.
The relationship between lumbopelvic and postero-lateral hip muscle function and lower extremity injury has been well documented in the literature.37–42 Frontal plane pelvic motion is controlled mainly by the gluteus medius muscle, providing not only dynamic stabilization of the hip joint, but also assists with control of knee adduction moment during SL activities.43,44 The deep hip external rotators and core musculature also play a role providing control of femoral internal rotation and dynamic stability of the trunk, respectively.45 Along with muscle activation, the presence of abnormal femoral version may impact an individual’s performance during functional testing. In order to appropriately assess functional control of these muscles, the panelists recommend evaluating an individual’s performance during SL tasks, including but not limited to a SL stance, SL squat, and or/step down maneuver. Observation of static SL stance can be useful to assess for gluteus medius dysfunction through the presence of a Trendelenburg sign, defined as a contralateral pelvic drop or a shift in the trunk to keep the pelvis level.46,47 McGovern et al.48 found the SL squat and the step-down test can help identify kinematic and biomechanical deficiencies and are useful in the evaluation of an individual with non-arthritic hip pain.
Activity Modifications
Consensus Point: Recreational activities that do not increase pain should be permitted, however, activities that increase pain should be modified (ie. reduced intensity or frequency) as needed to remain symptom free.
Individuals presenting with AD are generally young and active, therefore, activity modifications while undergoing a trial of supervised physiotherapy may be indicated. The panelists recommend all recreational activities should be pain-free as a common short-term goal of non-operative physiotherapy is a reduction in pain. Continuing activities that are painful may hinder the individual’s ability to perform the necessary strength and control exercises which are crucial to improving dynamic joint stability in this population. These activities often include prolonged upright activities or activities incorporating large ranges of hip motion, especially into flexion and rotation. Therefore, activities that are painful should be modified as needed. Modifications may include discontinuation of the activity or simply a reduction in the intensity or frequency. Tolerance to these activities should be reassessed as strength and functional control improves and can be reinitiated when the individuals report improved tolerance to these activities.
Therapeutic Exercise Progression
Local to Global Exercise Progression
Consensus Point: Progression from local to globally-focused exercise should be based upon quality of movement (ie. adequate muscle activation with minimal compensatory actions) and irritability of the hip joint.
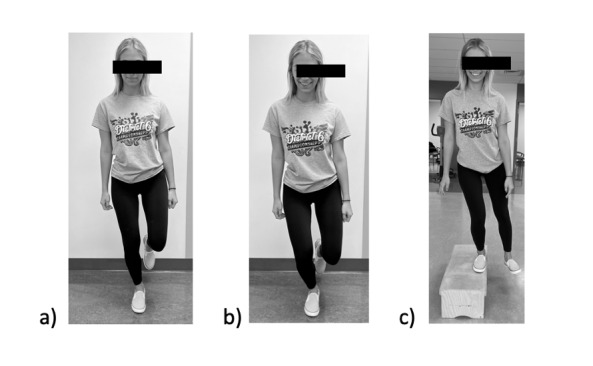
Appropriate functional control relies on coordinated activation of muscles across multiple joints. To establish functional control, however, an individual needs to first demonstrate competency in local muscle control (deep rotators, etc) as activation of global muscles in the presence of local dysfunction may reduce the ability of the local musculature to assist with basic stability tasks. Local muscle control should be assessed through an individual’s ability to perform low-load isometric exercises in varying non-weight bearing positions without compensation. Examples of these activities include gluteal bridges, clamshells, and transverse abdominis firing (Figure 1). The importance of local muscular control has been well established in patients with low back pain as the local muscles promote segmental stabilization and are superior to controlling unwanted load through the spine.49 Once an individual demonstrates adequate muscle activation with minimal compensatory actions during local exercise, the panelists recommend progression to global exercise, which may include weight bearing tasks (Figure 2). Global exercises should challenge the control of multiple muscle groups across multiple joints and should mimic an individual’s activity goals.
Figure 1. Examples of local muscle control exercises including a) supine transverse abdominis contraction with palpation, b) gluteal bridge, and c) sidelying hip abduction with resistance band.
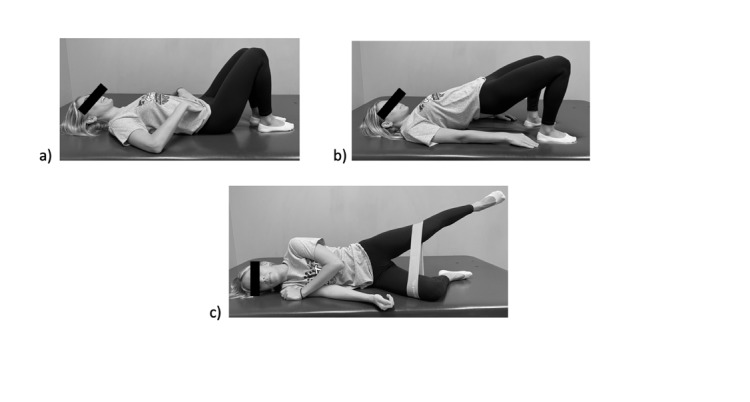
Figure 2. Examples of global exercises including a) SL stance, b) SL squat, and c) lateral step down.
Isometric to Eccentric Exercise Progression
Consensus Point: Progression from isometric to concentric exercise should be based on the individuals reported pain level during exercise. Progression from concentric to eccentric exercise should be based upon quality of movement (ie. adequate muscle activation with minimal compensatory actions).
Isometric muscle activation increases muscle tension without changing muscle length or joint range of motion and these types of contractions assist with dynamic joint stability.50 Not only do isometric contractions assist with maintaining a stable posture during dynamic movements, but they have been shown to benefit both acute and chronic pain and allow for increased joint stability and strength in the presence of pain.50–54 The panelists recommend use of isometric exercise in the presence of acute pain in the hip joint to improve muscle activation and joint stability. When the individual demonstrates less irritability in the hip joint as well as adequate muscle activation during isometric exercise, clinicians should progress to concentric exercises to further assist with muscle strengthening.
Lumbopelvic and Lower Extremity Neuromuscular Control
Therapeutic Exercise for Lumbopelvic and Lower Extremity Neuromuscular Control
Consensus Point: Exercises to facilitate lumbopelvic and lower extremity neuromuscular control should challenge both the pelvis and lower quarter with a focus on SL control when appropriate. Exercises should begin in low demand positions (ie. supine, quadruped, or tall kneeling) and progress to high demand positions (ie. double and SL) as tolerated. These tasks should include both static and multidirectional tasks and be progressed based on quality of movement.
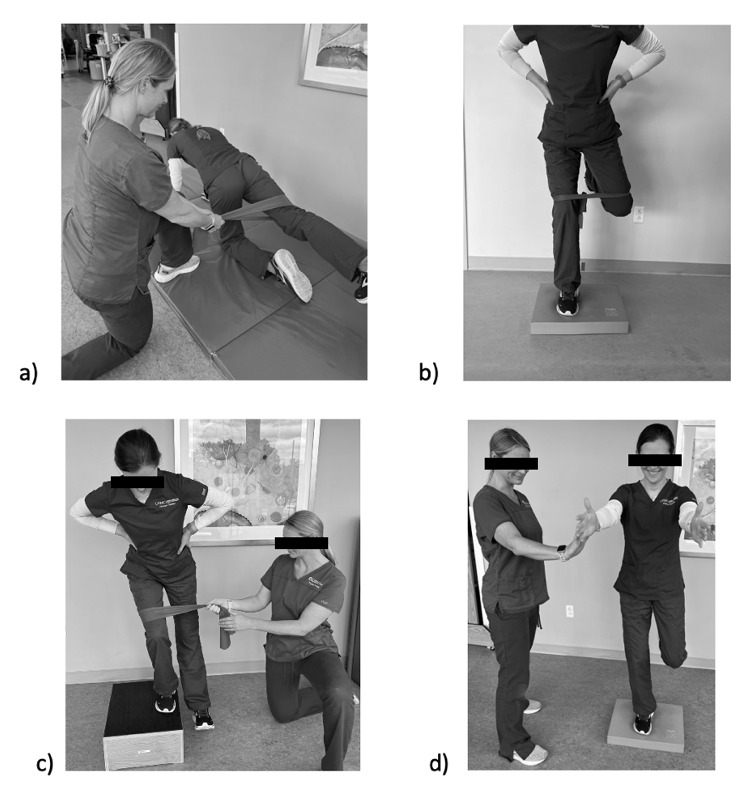
The association between adequate lumbopelvic control and lower extremity injury has been well established in the literature.30,55 The lumbopelvic region serves as the foundation for the trunk and lower extremity and poor lumbopelvic neuromuscular control can result in uncontrolled trunk movement as well as lower extremity valgus.56,57 The gluteus medius, gluteus maximus, deep external rotator, and core musculature play an important role in lumbopelvic neuromuscular control and exercises should be prescribed to challenge functional control these muscles.58–60 The panelists recommend beginning lumbopelvic control exercises in low demand positions of supine, quadruped, and tall kneeling incorporating lower and upper extremity movement based on quality of movement (Figure 3). Once adequate lumbopelvic control has been established in low demand positions, exercises should be progressed to double and SL weight bearing activities. Weight bearing exercises should begin with static tasks, progressing to dynamic, multidirectional tasks based on quality of movement (Figure 4).
Figure 3. Examples of low demand lumbopelvic control exercises including a) supine march, b) supine lower extremity isometric hold with alternating upper extremity flexion, c) alternating upper extremity flexion in supine, and d) bird dog.
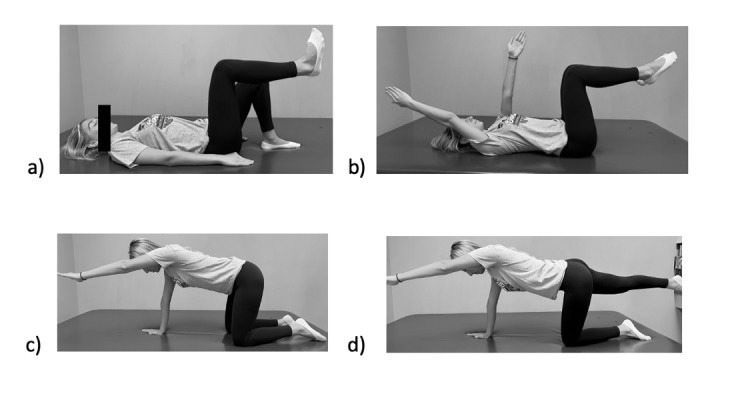
Figure 4. High demand lumbopelvic exercise progression including a) quadruped hip extension with medial resistance, b) standing hip abduction with resistance band on unstable surface, c) lateral step down with medial resistance, and d) SL stance on unstable surface with upper extremity perturbations.
Progression from Double to SL Activities
Consensus Point: Progression from double to SL activities is appropriate when an individual exhibits no trunk or pelvic compensation during double leg activities and can maintain pelvic and lower extremity control during a basic SL stance.
Double leg activities, such as a squat, should be utilized to establish basic static and dynamic control of the pelvis in a weight bearing position. While Lubahn et al.61 found the double leg squat with a load may be effective strategy to activate the gluteus maximus, it has been well established that electromyographic (EMG) activity of the gluteus medius and gluteus maximus muscles are highest in a SL position.62 However, a study of 22 healthy females with a mean age of 22.6 + 2.5 years found the magnitude of anticipatory gluteus medius activity before toe off of the contralateral limb during a SL squat was significantly correlated with the knee abduction moment (p < .001).63 This study highlights importance of establishing appropriate gluteus medius muscle recruitment in a double leg position before progressing to SL activities.63 Therefore, the panelists recommend progression from double to SL activities only when the individual can maintain appropriate pelvic and trunk control during double leg activities and can maintain pelvic and lower extremity control during a basic SL stance. Thorough attention should also be given to sagittal plane control, specifically pelvic tilt. Individuals with AD may increase their anterior pelvic tilt to improve functional acetabular retroversion, providing improved coverage anterior-superior femoral head.64,65 Therefore, creating increased anterior pelvic tilt may be a helpful compensatory motion to encourage in this population when transitioning from double to SL activities.
Rehabilitation of the Hip Flexor Complex
Consensus Point: Therapeutic exercise directed at the hip flexor complex should begin only after the patient has demonstrated an improvement in posterolateral hip strength and a reduction in hip joint irritability. These exercises should begin in a short lever position, when/if appropriate. Long lever hip flexion exercises may only be necessary based on sporting demands (i.e. dancers). They should be incorporated only when the patient has reduced hip joint irritability and is tolerating all short lever hip flexion exercises without an increase in pain.
The iliopsoas muscle complex sits anterior to the hip joint and may compensate for the lack of osseous stability associated with AD.66–68 As a result, the iliopsoas tendon is susceptible to inflammation, overload, and/or pain. Furthermore, Philippon et al.69 reported a link between gluteus medius muscle weakness and iliopsoas tendonitis. It has been shown that gluteal weakness is present in individuals with AD and therefore may increase the likelihood of developing iliopsoas tendonitis. More recently, Jacobsen et al.70 performed an ultrasound evaluation of the iliopsoas in 100 individuals with symptomatic AD. The authors reported that 50% of individuals demonstrated abnormalities in the iliopsoas tendon, hypothesizing that these abnormalities were a result of insufficient anterior acetabular coverage and the resulting increased load placed through the iliopsoas.70 Therefore, the expert panel recommends avoiding hip flexor muscle strengthening until improved dynamic hip joint stability has been established through increased posterolateral hip strength. When appropriate, these exercises should begin in a short lever position to minimize the chance of further irritation to the iliopsoas tendon. If long lever hip flexion is a required sporting demand, strengthening of the iliopsoas in a long lever should be prescribed, but only after adequate tolerance to short lever strengthening has been established. Both short and long lever hip flexion exercises should be discontinued if the patient reports increased pain.
Muscle Stretching Principles
Consensus Point: Muscular stretching should not be a focus of physiotherapy as AD is a diagnosis of instability. The focus of physiotherapy for patients with AD should be optimizing joint stability, not increasing mobility.
As previously mentioned, the iliopsoas complex acts as a secondary stabilizer to the hip joint and may be hypertonic secondary to the lack of osseous coverage associated with AD.67,68 Other muscles, such as the hip adductors, which act to stabilize the pelvis and lower extremity during the stance phase of gait, may also exhibit hypertonicity. Evaluation of the flexibility of these muscles may indicate they muscle tightness, the authors caution against restoring flexibility to these muscles in the early stages of the rehabilitation process as these muscles are providing anterior joint stability in the setting of osseous instability. Once adequate posterolateral hip strength has been established, providing increased dynamic hip joint stability, stretching can be initiated as tolerated. It should be noted, however, that the expert panel recommends a larger focus be placed on strength and neuromuscular control training to improve joint stability.
Cardiovascular Exercise
Consensus Point: Low impact activities such as cycling, the elliptical, and swimming (with a pool buoy if necessary) should be encouraged if pain-free. High impact cardiovascular activities such as running and plyometrics may be initiated as tolerated when strength and neuromuscular control improves and hip joint irritability and decreased.
The importance of cardiovascular exercise is well established.71,72 Maintenance of cardiovascular fitness during a trial of non-operative physiotherapy for the treatment of AD is crucial to allow for re-initiation of recreational activities as pain allows. Given individuals with AD often complain of pain with upright and high impact activities, low impact activities including cycling, the elliptical trainer, and swimming should be encouraged. Modifications may need to be made, such as adjusting seat position, stride length, and swim stroke, to allow these activities to be performed without increasing symptoms. These activities should be adjunct to strength and neuromuscular control exercises. As strength and functional control improves, individuals may report improved tolerance to higher impact activities. These high impact cardiovascular activities, including running and plyometrics, should be encouraged as pain allows.
Return to Recreational Activities/Sports
Return to Straight Line Running
Consensus Point: Individuals may begin running when they demonstrate normalized strength, minimal hip joint irritability, appropriate pelvic and lower extremity neuromuscular control during SL activities, and a normal gait pattern during ambulation at faster paces (Table I).
Table I. Panelist recommendations for return to recreational activities/sports.
| Return to Straight Line Running | Initiation of Plyometric Activities | Full Return to Sports |
|---|---|---|
|
|
|
Straight line running should be utilized as the first step in the return to sport progression as it introduces a dynamic, low load through the lower extremity and helps improve cardiovascular endurance. Utilizing objective criteria, including pain, ROM, and functional control, is crucial as running is the first sport-specific activity in the rehabilitation process. Despite the increased recognition of non-arthritic hip joint pathologies, there is a dearth of literature supporting return to run criteria for these individuals. The panelists recommend utilizing a combination of measures, including hip joint pain, lumbopelvic and lower extremity neuromuscular control during SL activities, and gait, to assess for readiness to return to straight line running. Running should be progressed in a gradual manner utilizing walk/jog intervals to allow for monitoring of hip joint irritability. If the patient demonstrates appropriate tolerance to a running progression, low-level agility drills, including ladder drills, should be initiated.
Initiation of Plyometric Activities
Consensus Point: Plyometric activities should be initiated when an individual demonstrates normalized strength, minimal to no pain, and appropriate pelvic and lower extremity neuromuscular control during all running and low-level agility tasks (Table I).
Plyometrics exercises are crucial for return to sport progression as such activities improve power development during functional movement patterns, allowing the individual to prepare for their sporting demands.73 Along with increased power production, plyometrics increase peak force and velocity of acceleration movements and increase muscle activation.74 The panelists recommend progressing to plyometric activities when an individual is demonstrating minimal to no pain and appropriate pelvic and lower extremity neuromuscular control during straight line running and low-level agility tasks. Plyometric exercise should begin with double leg activities, progressing to SL activities when the patient demonstrates appropriate functional control with double leg tasks. Careful attention should be pain to dosing of plyometric activities, specifically contacts per session, and should be based on athletic ability or exercise volume.75
Full Return to Sport
Consensus Point: An individual should be cleared for full participation in sporting activities when they demonstrate normalized strength, adequate pelvic and lower extremity neuromuscular control during SL tasks, and tolerance to all sport specific activities including running and plyometrics (Table I).
Full return to activity is a common goal of individuals with symptomatic AD as these individuals tend to be young and athletic. Currently, there is no literature indicating return to sport rates or objective criteria that should be utilized to determine readiness to return to full participation in individuals with AD. The panelists recommend utilizing a combination of strength, lower extremity neuromuscular control, and tolerance to sport specific activities as criteria to determine readiness for full return to sport. Along with this objective criteria, psychological readiness should be taken into account as decreased psychological readiness may result in reinjury and/or decreased sport performance.76–79 In individuals with femoroacatebaular impingement syndrome (FAIS), Jochimsen et al.80 reported low self-efficacy and high kinesiophobia resulted in worse function and increased pain. Given the long-standing nature of AD and similar activity limitations seen with FAIS, an assumption can be made that these individuals will exhibit signs consistent with low confidence and fear and clinicians should recognize the importance of these factors when considering full return to sport clearance.
Referral to a Physician Hip Specialist
Consensus Point: An individual should be referred for initial or return consultation to a physician specializing in hip preservation if they are exhibiting no decrease in symptoms despite improved strength and neuromuscular control with completion of 4-8 weeks of physiotherapy.
After the initial diagnosis of AD, an individual may be referred for physiotherapy. If after 4-8 weeks of hip specific physiotherapy, the individual reports no decrease in symptoms despite improved strength and neuromuscular control, a referral to a physician specializing in hip preservation is indicated. It should also be noted that individuals with more severe disease may not be candidates for a trial of non-operative management due to the increased possibility of early onset arthritis.81 Severity of disease is often classified utilizing the lateral center edge angle (LCEA) on an anteroposterior radiograph, with an LCEA < 20 degrees considered pathologic and an LCEA between 20-25 degrees considered borderline dysplastic.82 While the LCEA is an oversimplification of the diagnosis, it may be a useful finding for physiotherapists to consider when determining timing of physician referral.83
CONCLUSION
A trial of non-operative rehabilitation is often recommended in the setting of AD. However, no physiotherapy guidelines or description of therapeutic activity progression currently exist in the literature. This Delphi study established expert based recommendations regarding initial evaluation principles, activity modifications, therapeutic exercise progression, return to activity criteria, and indications for physician referral. This study will help reduce practice variation and is the first step in determining who is appropriate for a trial of non-operative rehabilitation. Future studies need to assess patient outcomes with utilization of this protocol and determine how many patients convert to surgery despite targeted rehabilitation.
Corresponding Author
Ashley Disantis, DPT, OCS
Rangos School of Health Sciences, Department of Physical Therapy
Duquesne University
Pittsburgh, PA USA
disantisae@chp.edu
412-979-4733
CONFLICTS OF INTEREST
The authors report no conflicts of interest
Acknowledgments
ACKNOWLEDGEMENTS
We want to acknowledge all physiotherapists who put their time and effort into completion of the three survey rounds of this Delphi study. Their work was essential in creating this consensus statement.
References
- Hip dysplasia in the young adult. Gala Luca, Clohisy John C., Beaulé Paul E. Jan;2016 The Journal of Bone and Joint Surgery. 98(1):63–73. doi: 10.2106/jbjs.o.00109. doi: 10.2106/jbjs.o.00109. [DOI] [PubMed] [Google Scholar]
- How are dysplastic hips different? A three-dimensional CT study. van Bosse Harold, Wedge John H., Babyn Paul. May;2015 Clin Orthop Relat Res. 473(5):1712–1723. doi: 10.1007/s11999-014-4103-y. doi: 10.1007/s11999-014-4103-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Incidence and characteristics of femoral deformities in the dysplastic hip. Clohisy John C., Nunley Ryan M., Carlisle Jack C., Schoenecker Perry L. Jan;2009 Clin Orthop Relat Res. 467(1):128–134. doi: 10.1007/s11999-008-0481-3. doi: 10.1007/s11999-008-0481-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. Klaue K, Durnin CW, Ganz R. May;1991 The Journal of Bone and Joint Surgery. British volume. 73-B(3):423–429. doi: 10.1302/0301-620x.73b3.1670443. doi: 10.1302/0301-620x.73b3.1670443. [DOI] [PubMed] [Google Scholar]
- Patient-specific analysis of cartilage and labrum mechanics in human hips with acetabular dysplasia. Henak C.R., Abraham C.L., Anderson A.E., Maas S.A., Ellis B.J., Peters C.L., Weiss J.A. Feb;2014 Osteoarthritis and Cartilage. 22(2):210–217. doi: 10.1016/j.joca.2013.11.003. doi: 10.1016/j.joca.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Articular cartilage abnormalities in dysplastic hips without joint space narrowing. Nishii Takashi, Sugano Nobuhiko, Tanaka Hisashi, Nakanishi Katsuyuki, Ohzono Kenji, Yoshikawa Hideki. Feb;2001 Clinical Orthopaedics and Related Research. 383(383):183–190. doi: 10.1097/00003086-200102000-00020. doi: 10.1097/00003086-200102000-00020. [DOI] [PubMed] [Google Scholar]
- The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Crawford Matthew J, Dy Christopher J, Alexander Jerry W, Thompson Matthew, Schroder Steven J, Vega Charles E, Patel Rikin V, Miller Andrew R, McCarthy Joseph C, Lowe Walter R, Noble Philip C. Dec;2007 Clin Orthop Relat Res. 465:16–22. doi: 10.1097/blo.0b013e31815b181f. doi: 10.1097/blo.0b013e31815b181f. [DOI] [PubMed] [Google Scholar]
- Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Domb Benjamin G., Stake Christine E., Lindner Dror, El-Bitar Youssef, Jackson Timothy J. Aug 16;2013 The American Journal of Sports Medicine. 41(11):2591–2598. doi: 10.1177/0363546513499154. doi: 10.1177/0363546513499154. [DOI] [PubMed] [Google Scholar]
- The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. Murphy S B, Ganz R, Müller M E. Jul;1995 The Journal of Bone & Joint Surgery. 77(7):985–989. doi: 10.2106/00004623-199507000-00002. doi: 10.2106/00004623-199507000-00002. [DOI] [PubMed] [Google Scholar]
- The John Charnley Award: Redefining the natural history of osteoarthritis in patients with hip dysplasia and impingement. Wyles Cody C., Heidenreich Mark J., Jeng Jack, Larson Dirk R., Trousdale Robert T., Sierra Rafael J. Feb;2017 Clin Orthop Relat Res. 475(2):336–350. doi: 10.1007/s11999-016-4815-2. doi: 10.1007/s11999-016-4815-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osteoarthritis as a disease of mechanics. Felson D.T. Jan;2013 Osteoarthritis and Cartilage. 21(1):10–15. doi: 10.1016/j.joca.2012.09.012. doi: 10.1016/j.joca.2012.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Is hip morphology a risk factor for developing hip osteoarthritis? A systematic review with meta-analysis. Casartelli N.C., Maffiuletti N.A., Valenzuela P.L., Grassi A., Ferrari E., van Buuren M.M.A., Nevitt M.C., Leunig M., Agricola R. Sep;2021 Osteoarthritis and Cartilage. 29(9):1252–1264. doi: 10.1016/j.joca.2021.06.007. doi: 10.1016/j.joca.2021.06.007. [DOI] [PubMed] [Google Scholar]
- Acetabular edge loading during gait is elevated by the anatomical deformities of hip dysplasia. Song Ke, Pascual-Garrido Cecilia, Clohisy John C., Harris Michael D. Jul 1;2021 Frontiers in Sports and Active Living. 3:687419. doi: 10.3389/fspor.2021.687419. doi: 10.3389/fspor.2021.687419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Role of the acetabular labrum in load support across the hip joint. Henak Corinne R., Ellis Benjamin J., Harris Michael D., Anderson Andrew E., Peters Christopher L., Weiss Jeffrey A. Aug;2011 Journal of Biomechanics. 44(12):2201–2206. doi: 10.1016/j.jbiomech.2011.06.011. doi: 10.1016/j.jbiomech.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscle-tendon-related pain in 100 patients with hip dysplasia: prevalence and associations with self-reported hip disability and muscle strength. Jacobsen Julie Sandell, Hölmich Per, Thorborg Kristian, Bolvig Lars, Jakobsen Stig Storgaard, Søballe Kjeld, Mechlenburg Inger. 2018J Hip Preserv Surg. 5(1):39–46. doi: 10.1093/jhps/hnx041. doi: 10.1093/jhps/hnx041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natural history of the dysplastic hip following modern periacetabular osteotomy. Wyles Cody C., Vargas Juan S., Heidenreich Mark J., Mara Kristin C., Peters Christopher L., Clohisy John C., Trousdale Robert T., Sierra Rafael J. May 15;2019 Journal of Bone and Joint Surgery. 101(10):932–938. doi: 10.2106/jbjs.18.00983. doi: 10.2106/jbjs.18.00983. [DOI] [PubMed] [Google Scholar]
- 14-year hip survivorship after periacetabular osteotomy: a follow-up study on 1,385 hips. Larsen Josefine Beck, Mechlenburg Inger, Jakobsen Stig Storgaard, Thilleman Theis Munchholm, Søballe Kjeld. Feb 28;2020 Acta Orthopaedica. 91(3):299–305. doi: 10.1080/17453674.2020.1731159. doi: 10.1080/17453674.2020.1731159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Periacetabular osteotomy to treat residual dysplasia in adolescents and young adults: indications, complications, results. Millis M. B., McClincy M. Aug;2018 Journal of Children's Orthopaedics. 12(4):349–357. doi: 10.1302/1863-2548.12.180068. doi: 10.1302/1863-2548.12.180068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehabilitation guidelines for use following a periacetabular osteotomy (PAO): A North American based delphi consensus. Disantis Ashley E., Ruh Ethan, Martin RobRoy, Enseki Keelan, McClincy Michael. Oct 2;2022 Int J Sports Phys Ther. 17(6):1002–1015. doi: 10.26603/001c.38043. doi: 10.26603/001c.38043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Descriptive epidemiology of acetabular dysplasia: The Academic Network of Conservational Hip Outcomes Research (ANCHOR) periacetabular osteotomy. Sankar Wudbhav N., Duncan Stephen T., Baca Geneva R., Beaulé Paul E., Millis Michael B., Kim Young-jo, Peters Christopher L., Podeszwa David A., Schoenecker Perry L., Sierra Rafael J., Sink Ernest L., Sucato Daniel J., Trousdale Robert T., Zaltz Ira, Clohisy John C. Feb;2017 Journal of the American Academy of Orthopaedic Surgeons. 25(2):150–159. doi: 10.5435/jaaos-d-16-00075. doi: 10.5435/jaaos-d-16-00075. [DOI] [PubMed] [Google Scholar]
- Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. Nunley Ryan M., Prather Heidi, Hunt Devyani, Schoenecker Perry L., Clohisy John C. May 4;2011 J Bone Joint Surg Am. 93(Supplement_2):17–21. doi: 10.2106/jbjs.j.01735. doi: 10.2106/jbjs.j.01735. [DOI] [PubMed] [Google Scholar]
- Femoral version abnormalities significantly outweigh effect of cam impingement on hip internal rotation. Kraeutler Matthew J., Chadayammuri Vivek, Garabekyan Tigran, Mei-Dan Omer. Feb 7;2018 Journal of Bone and Joint Surgery. 100(3):205–210. doi: 10.2106/jbjs.17.00376. doi: 10.2106/jbjs.17.00376. [DOI] [PubMed] [Google Scholar]
- Femoral anteversion in the hip: comparison of measurement by computed tomography, magnetic resonance imaging, and physical examination. Botser Itamar B., Ozoude George C., Martin Dorea E., Siddiqi Aheed J., Kuppuswami Sivaraja, Domb Benjamin G. May;2012 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 28(5):619–627. doi: 10.1016/j.arthro.2011.10.021. doi: 10.1016/j.arthro.2011.10.021. [DOI] [PubMed] [Google Scholar]
- Relationship between femoral anteversion and findings in hips with femoroacetabular impingement. Ejnisman Leandro, Philippon Marc J., Lertwanich Pisit, Pennock Andrew T., Herzog Mackenzie M., Briggs Karen K., Ho Charles P. Mar;2013 Orthopedics. 36(3):e293–300. doi: 10.3928/01477447-20130222-17. doi: 10.3928/01477447-20130222-17. [DOI] [PubMed] [Google Scholar]
- Reliability of goniometric measurements and visual estimates of hip ROM in patients with osteoarthrosis. Holm Inger, Bolstad Bjørg, Lütken Teresa, Ervik Anne, Røkkum Magne, Steen Harald. Nov;2000 Physiotherapy Research International. 5(4):241–248. doi: 10.1002/pri.204. doi: 10.1002/pri.204. [DOI] [PubMed] [Google Scholar]
- Clinical tests to determine femoral version category in people with chronic hip joint pain and asymptomatic controls. Uding Alexandria, Bloom Nancy J., Commean Paul K., Hillen Travis J., Patterson Jacqueline D., Clohisy John C., Harris-Hayes Marcie. Feb;2019 Musculoskeletal Science and Practice. 39:115–122. doi: 10.1016/j.msksp.2018.12.003. doi: 10.1016/j.msksp.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The role of femoral neck anteversion in the development of osteoarthritis in dysplastic hips. Li H., Wang Y., Oni J. K., Qu X., Li T., Zeng Y., Liu F., Zhu Z. Dec;2014 The Bone & Joint Journal. 96-B(12):1586–1593. doi: 10.1302/0301-620x.96b12.33983. doi: 10.1302/0301-620x.96b12.33983. [DOI] [PubMed] [Google Scholar]
- Muscular activity of patella and hip stabilizers of healthy subjects during squat exercises. Felicio L. R., Dias L. A., Silva A. P., Oliveira A. S., Bevilaqua-Grossi D. 2011Rev Bras Fisioter. 15(3):206–11. [PubMed] [Google Scholar]
- Electromyographic activity of selected trunk and hip muscles during a squat lift. Effect of varying the lumbar posture. Vakos J. P., Nitz A. J., Threlkeld A. J., Shapiro R., Horn T. Mar;1994 Spine. 19(Supplement):687–695. doi: 10.1097/00007632-199403001-00008. doi: 10.1097/00007632-199403001-00008. [DOI] [PubMed] [Google Scholar]
- Core stability and its relationship to lower extremity function and injury. Willson John D., Dougherty Christopher P., Ireland Mary Lloyd, Davis Irene McClay. Sep;2005 Journal of the American Academy of Orthopaedic Surgeons. 13(5):316–325. doi: 10.5435/00124635-200509000-00005. doi: 10.5435/00124635-200509000-00005. [DOI] [PubMed] [Google Scholar]
- Hip Strength deficits in patients with symptomatic femoroacetabular impingement and labral tears. Nepple Jeffrey J., Goljan Peter, Briggs Karen K., Garvey Sean E., Ryan Mark, Philippon Marc J. Nov;2015 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 31(11):2106–2111. doi: 10.1016/j.arthro.2015.04.095. doi: 10.1016/j.arthro.2015.04.095. [DOI] [PubMed] [Google Scholar]
- Impaired hip muscle strength in patients with femoroacetabular impingement syndrome. Kierkegaard Signe, Mechlenburg Inger, Lund Bent, Søballe Kjeld, Dalgas Ulrik. Dec;2017 Journal of Science and Medicine in Sport. 20(12):1062–1067. doi: 10.1016/j.jsams.2017.05.008. doi: 10.1016/j.jsams.2017.05.008. [DOI] [PubMed] [Google Scholar]
- Asymmetry in muscle strength, dynamic balance, and range of motion in adult symptomatic hip dysplasia. Wang Haifang, Yu Hailong, Kim Yonghwan, Chen Tingting. Apr 5;2022 Symmetry. 14(4):748. doi: 10.3390/sym14040748. doi: 10.3390/sym14040748. [DOI] [Google Scholar]
- Diagnostic accuracy of clinical tests for cam or pincer morphology in individuals with suspected FAI syndrome: a systematic review. Caliesch Rahel, Sattelmayer Martin, Reichenbach Stephan, Zwahlen Marcel, Hilfiker Roger. Apr;2020 BMJ Open Sport & Exercise Medicine. 6(1):e000772. doi: 10.1136/bmjsem-2020-000772. doi: 10.1136/bmjsem-2020-000772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diagnostic accuracy of 3 physical examination tests in the assessment of hip microinstability. Hoppe Daniel J., Truntzer Jeremy N., Shapiro Lauren M., Abrams Geoffrey D., Safran Marc R. Nov;2017 Orthopaedic Journal of Sports Medicine. 5(11):2325967117740121. doi: 10.1177/2325967117740121. doi: 10.1177/2325967117740121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hip microinstability diagnosis and management: a systematic review. Cohen Dan, Jean Pierre-Olivier, Patel Milin, Aravinthan Neveadan, Simunovic Nicole, Duong Andrew, Safran Marc R., Khanduja Vikas, Ayeni Olufemi R. 2023Knee Surgery, Sports Traumatology, Arthroscopy. 31(1):16–32. doi: 10.1007/s00167-022-06976-7. doi: 10.1007/s00167-022-06976-7. [DOI] [PubMed] [Google Scholar]
- Ankle inversion injury and hypermobility: effect on hip and ankle muscle electromyography onset latency. Beckman Scott M., Buchanan Thomas S. Dec;1995 Archives of Physical Medicine and Rehabilitation. 76(12):1138–1143. doi: 10.1016/s0003-9993(95)80123-5. doi: 10.1016/s0003-9993(95)80123-5. [DOI] [PubMed] [Google Scholar]
- Hip abductor weakness in distance runners with iliotibial band syndrome. Fredericson Michael, Cookingham Curtis L., Chaudhari Ajit M., Dowdell Brian C., Oestreicher Nina, Sahrmann Shirley A. Jul;2000 Clinical Journal of Sport Medicine. 10(3):169–175. doi: 10.1097/00042752-200007000-00004. doi: 10.1097/00042752-200007000-00004. [DOI] [PubMed] [Google Scholar]
- Hip muscle weakness and overuse injuries in recreational runners. Niemuth Paul E., Johnson Robert J., Myers Marcella J., Thieman Thomas J. Jan;2005 Clinical Journal of Sport Medicine. 15(1):14–21. doi: 10.1097/00042752-200501000-00004. doi: 10.1097/00042752-200501000-00004. [DOI] [PubMed] [Google Scholar]
- Core stability measures as risk factors for lower extremity injury in athletes. Leetun DARIN T., Ireland MARY LLOYD, Willson JOHN D., Ballantyne BRYON T., Davis IRENE MCCLAY. Jun;2004 Medicine & Science in Sports & Exercise. 36(6):926–934. doi: 10.1249/01.mss.0000128145.75199.c3. doi: 10.1249/01.mss.0000128145.75199.c3. [DOI] [PubMed] [Google Scholar]
- Hip strength in females with and without patellofemoral pain. Ireland Mary Lloyd, Willson John D., Ballantyne Bryon T., Davis Irene McClay. Nov;2003 Journal of Orthopaedic & Sports Physical Therapy. 33(11):671–676. doi: 10.2519/jospt.2003.33.11.671. doi: 10.2519/jospt.2003.33.11.671. [DOI] [PubMed] [Google Scholar]
- Core strength and lower extremity alignment during single leg squats. Willson JOHN D., Ireland MARY LLOYD, Davis IRENE. May;2006 Med Sci Sports Exerc. 38(5):945–952. doi: 10.1249/01.mss.0000218140.05074.fa. doi: 10.1249/01.mss.0000218140.05074.fa. [DOI] [PubMed] [Google Scholar]
- The architectural design of the gluteal muscle group: implications for movement and rehabilitation. Ward Samuel R., Winters Taylor M., Blemker Silvia S. Feb;2010 Journal of Orthopaedic & Sports Physical Therapy. 40(2):95–102. doi: 10.2519/jospt.2010.3302. doi: 10.2519/jospt.2010.3302. [DOI] [PubMed] [Google Scholar]
- Anatomy of the abductor muscles of the hip as studied by computed tomography. Clark J M, Haynor D R. Sep;1987 The Journal of Bone & Joint Surgery. 69(7):1021–1031. doi: 10.2106/00004623-198769070-00010. doi: 10.2106/00004623-198769070-00010. [DOI] [PubMed] [Google Scholar]
- Effects of lumbar extensor fatigue and fatigue rate on postural sway. Davidson B. S., Madigan M. L., Nussbaum M. A. Jul 28;2004 European Journal of Applied Physiology. 93(1-2):183–189. doi: 10.1007/s00421-004-1195-1. doi: 10.1007/s00421-004-1195-1. [DOI] [PubMed] [Google Scholar]
- Trendelenburg's test: 1895. Trendelenburg F. Oct;1998 Clinical Orthopaedics and Related Research. (355):3–7. doi: 10.1097/00003086-199810000-00002. doi: 10.1097/00003086-199810000-00002. [DOI] [PubMed]
- The significance of the Trendelenburg test. Hardcastle P, Nade S. Nov;1985 The Journal of Bone and Joint Surgery. British volume. 67-B(5):741–746. doi: 10.1302/0301-620x.67b5.4055873. doi: 10.1302/0301-620x.67b5.4055873. [DOI] [PubMed] [Google Scholar]
- Evidence-based procedures for performing the single leg squat and step-down tests in evaluation of non-arthritic hip pain: A literature review. McGovern Ryan P., Martin RobRoy L., Christoforetti John J., Kivlan Benjamin R. Jun;2018 International Journal of Sports Physical Therapy. 13(3):526–536. doi: 10.26603/ijspt20180526. doi: 10.26603/ijspt20180526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson C., Jull G., Hodges P., Hides J. Theraputic exercise for spinal segmental stabilization in low back pain: scientific basis and clinical approach. Churchill Livingstone; Edinburgh: [Google Scholar]
- Effects of isokinetic passive exercise and isometric muscle contraction on passive stiffness. Terada Shigeru, Miaki Hiroichi, Uchiyama Keita, Hayakawa Shozo, Yamazaki Toshiaki. 2013Journal of Physical Therapy Science. 25(10):1347–1352. doi: 10.1589/jpts.25.1347. doi: 10.1589/jpts.25.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The effects of isometric exercise types on pain and muscle activity in patients with low back pain. Rhyu Hyun-Seung, Park Hun-Kyung, Park Jung-Sub, Park Hye-Sang. Aug 24;2015 Journal of Exercise Rehabilitation. 11(4):211–214. doi: 10.12965/jer.150224. doi: 10.12965/jer.150224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do isometric and isotonic exercise programs reduce pain in athletes with patellar tendinopathy in-season? A randomised clinical trial. van Ark Mathijs, Cook Jill L., Docking Sean I., Zwerver Johannes, Gaida James E., van den Akker-Scheek Inge, Rio Ebonie. Sep;2016 Journal of Science and Medicine in Sport. 19(9):702–706. doi: 10.1016/j.jsams.2015.11.006. doi: 10.1016/j.jsams.2015.11.006. [DOI] [PubMed] [Google Scholar]
- Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Rio Ebonie, Kidgell Dawson, Purdam Craig, Gaida Jamie, Moseley G Lorimer, Pearce Alan J, Cook Jill. May 15;2015 British Journal of Sports Medicine. 49(19):1277–1283. doi: 10.1136/bjsports-2014-094386. doi: 10.1136/bjsports-2014-094386. [DOI] [PubMed] [Google Scholar]
- Efficacy of an inertial resistance training paradigm in the treatment of patellar tendinopathy in athletes: a case-series study. Romero-Rodriguez D., Gual G., Tesch P.A. Feb;2011 Physical Therapy in Sport. 12(1):43–48. doi: 10.1016/j.ptsp.2010.10.003. doi: 10.1016/j.ptsp.2010.10.003. [DOI] [PubMed] [Google Scholar]
- National Athletic Trainers' Association Position Statement: Prevention of Anterior Cruciate Ligament Injury. Padua Darin A., DiStefano Lindsay J., Hewett Timothy E., Garrett William E., Marshall Stephen W., Golden Grace M., Shultz Sandra J., Sigward Susan M. Jan 1;2018 J Athl Train. 53(1):5–19. doi: 10.4085/1062-6050-99-16. doi: 10.4085/1062-6050-99-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Hewett Timothy E., Myer Gregory D., Ford Kevin R., Heidt Robert S. Jr., Colosimo Angelo J., McLean Scott G., van den Bogert Antonie J., Paterno Mark V., Succop Paul. Apr;2005 The American Journal of Sports Medicine. 33(4):492–501. doi: 10.1177/0363546504269591. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- A review of electromyographic activation levels, timing differences, and increased anterior cruciate ligament injury incidence in female athletes. Hewett T E, Zazulak B T, Myer G D, Ford K R. Jun 1;2005 British Journal of Sports Medicine. 39(6):347–350. doi: 10.1136/bjsm.2005.018572. doi: 10.1136/bjsm.2005.018572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluteus medius muscle activation patterns as a predictor of low back pain during standing. Nelson-Wong Erika, Gregory Diane E., Winter David A., Callaghan Jack P. Jun;2008 Clinical Biomechanics. 23(5):545–553. doi: 10.1016/j.clinbiomech.2008.01.002. doi: 10.1016/j.clinbiomech.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Timing and relative intensity of hip extensor and abductor muscle action during level and stair ambulation. An EMG study. Lyons Kathryn, Perry Jacquelin, Gronley Joanne K., Barnes Lee, Antonelli Dan. Oct 1;1983 Phys Ther. 63(10):1597–1605. doi: 10.1093/ptj/63.10.1597. doi: 10.1093/ptj/63.10.1597. [DOI] [PubMed] [Google Scholar]
- The role of core stability in athletic function. Kibler W Ben, Press Joel, Sciascia Aaron. 2006Sports Medicine. 36(3):189–198. doi: 10.2165/00007256-200636030-00001. doi: 10.2165/00007256-200636030-00001. [DOI] [PubMed] [Google Scholar]
- Hip muscle activation and knee frontal plane motion during weight bearing therapeutic exercises. Lubahn A. J., Kernozek T. W., Tyson T. L., Merkitch K. W., Reutemann P., Chestnut J. M. 2011Int J Sports Phys Ther. 6(2):92–103. [PMC free article] [PubMed] [Google Scholar]
- Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. Boren K., Conrey C., Le Coguic J., Paprocki L., Voight M., Robinson T. K. 2011Int J Sports Phys Ther. 6(3):206–23. [PMC free article] [PubMed] [Google Scholar]
- The relationship of anticipatory gluteus medius activity to pelvic and knee stability in the transition to single-leg stance. Kim Daehan, Unger Janelle, Lanovaz Joel L., Oates Alison R. 2016PM&R. 8(2):138–144. doi: 10.1016/j.pmrj.2015.06.005. doi: 10.1016/j.pmrj.2015.06.005. [DOI] [PubMed] [Google Scholar]
- Does compensatory anterior pelvic tilt decrease after bilateral periacetabular osteotomy? Daley Erika, Nahm Nickolas, Koueiter Denise, Zaltz Ira. Apr 17;2019 Clinical Orthopaedics & Related Research. 477(5):1168–1175. doi: 10.1097/corr.0000000000000560. doi: 10.1097/corr.0000000000000560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Relationship between spinal sagittal alignment and acetabular coverage: a patient-matched control study. Fukushima Kensuke, Miyagi Masayuki, Inoue Gen, Shirasawa Eiki, Uchiyama Katsufumi, Takahira Naonobu, Takaso Masashi. Jul 3;2018 Archives of Orthopaedic and Trauma Surgery. 138(11):1495–1499. doi: 10.1007/s00402-018-2992-z. doi: 10.1007/s00402-018-2992-z. [DOI] [PubMed] [Google Scholar]
- Hip instability: a review of hip dysplasia and other contributing factors. Kraeutler M.J., Garabekyan T., Pascual-Garrido C., Mei-Dan O. 2016Muscle Ligaments and Tendons Journal. 6(3):343–353. doi: 10.32098/mltj.03.2016.10. doi: 10.32098/mltj.03.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walking patterns and hip contact forces in patients with hip dysplasia. Skalshøi Ole, Iversen Christian Hauskov, Nielsen Dennis Brandborg, Jacobsen Julie, Mechlenburg Inger, Søballe Kjeld, Sørensen Henrik. Oct;2015 Gait & Posture. 42(4):529–533. doi: 10.1016/j.gaitpost.2015.08.008. doi: 10.1016/j.gaitpost.2015.08.008. [DOI] [PubMed] [Google Scholar]
- Clinical outcomes after arthroscopic psoas lengthening: the effect of femoral version. Fabricant Peter D., Bedi Asheesh, De La Torre Katrina, Kelly Bryan T. Jul;2012 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 28(7):965–971. doi: 10.1016/j.arthro.2011.11.028. doi: 10.1016/j.arthro.2011.11.028. [DOI] [PubMed] [Google Scholar]
- Rehabilitation exercise progression for the gluteus medius muscle with consideration for iliopsoas tendinitis: an in vivo electromyography study. Philippon Marc J., Decker Michael J., Giphart J. Erik, Torry Michael R., Wahoff Michael S., LaPrade Robert F. May 12;2011 The American Journal of Sports Medicine. 39(8):1777–1786. doi: 10.1177/0363546511406848. doi: 10.1177/0363546511406848. [DOI] [PubMed] [Google Scholar]
- Muscle–tendon-related abnormalities detected by ultrasonography are common in symptomatic hip dysplasia. Jacobsen Julie Sandell, Bolvig Lars, Hölmich Per, Thorborg Kristian, Jakobsen Stig Storgaard, Søballe Kjeld, Mechlenburg Inger. May 4;2018 Archives of Orthopaedic and Trauma Surgery. 138(8):1059–1067. doi: 10.1007/s00402-018-2947-4. doi: 10.1007/s00402-018-2947-4. [DOI] [PubMed] [Google Scholar]
- Benefits of physical activity. Center for Disease Control and Prevention; [Google Scholar]
- American Heart Association Endurance exercise (aerobic)
- Current Concepts of Plyometric Exercise. Davies G., Riemann B. L., Manske R. 2015Int J Sports Phys Ther. 10(6):760–86. [PMC free article] [PubMed] [Google Scholar]
- Does plyometric training improve strength performance? A meta-analysis. Sáez-Sáez de Villarreal Eduardo, Requena Bernardo, Newton Robert U. Sep;2010 Journal of Science and Medicine in Sport. 13(5):513–522. doi: 10.1016/j.jsams.2009.08.005. doi: 10.1016/j.jsams.2009.08.005. [DOI] [PubMed] [Google Scholar]
- Plyometric exercise in the rehabilitation of athletes: physiological responses and clinical application. Chmielewski Terese L., Myer Gregory D., Kauffman Douglas, Tillman Susan M. May;2006 Journal of Orthopaedic & Sports Physical Therapy. 36(5):308–319. doi: 10.2519/jospt.2006.2013. doi: 10.2519/jospt.2006.2013. [DOI] [PubMed] [Google Scholar]
- The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Ardern Clare L, Österberg Annika, Tagesson Sofi, Gauffin Håkan, Webster Kate E, Kvist Joanna. Oct 7;2014 British Journal of Sports Medicine. 48(22):1613–1619. doi: 10.1136/bjsports-2014-093842. doi: 10.1136/bjsports-2014-093842. [DOI] [PubMed] [Google Scholar]
- Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Ardern Clare L., Taylor Nicholas F., Feller Julian A., Whitehead Timothy S., Webster Kate E. Jun 3;2013 The American Journal of Sports Medicine. 41(7):1549–1558. doi: 10.1177/0363546513489284. doi: 10.1177/0363546513489284. [DOI] [PubMed] [Google Scholar]
- A systematic review of the psychological factors associated with returning to sport following injury. Ardern Clare L, Taylor Nicholas F, Feller Julian A, Webster Kate E. 2013British Journal of Sports Medicine. 47(17):1120–1126. doi: 10.1136/bjsports-2012-091203. doi: 10.1136/bjsports-2012-091203. [DOI] [PubMed] [Google Scholar]
- Psychological factors are associated with return to pre-injury levels of sport and physical activity after ACL reconstruction. Baez Shelby E., Hoch Matthew C., Hoch Johanna M. 2020Knee Surgery, Sports Traumatology, Arthroscopy. 28(2):495–501. doi: 10.1007/s00167-019-05696-9. doi: 10.1007/s00167-019-05696-9. [DOI] [PubMed] [Google Scholar]
- Low self-efficacy and high kinesiophobia are associated with worse function in patients with femoroacetabular impingement syndrome. Jochimsen Kate N., Mattacola Carl G., Noehren Brian, Picha Kelsey J., Duncan Stephen T., Jacobs Cale A. 2020 J Sport Rehabil. 30(3):445–451. doi: 10.1123/jsr.2019-0498. doi: 10.1123/jsr.2019-0498. [DOI] [PubMed] [Google Scholar]
- Subclinical deformities of the hip are significant predictors of radiographic osteoarthritis and joint replacement in women. A 20 year longitudinal cohort study. Thomas G.E.R., Palmer A.J.R., Batra R.N., Kiran A., Hart D., Spector T., Javaid M.K., Judge A., Murray D.W., Carr A.J., Arden N.K., Glyn-Jones S. Oct;2014 Osteoarthritis and Cartilage. 22(10):1504–1510. doi: 10.1016/j.joca.2014.06.038. doi: 10.1016/j.joca.2014.06.038. [DOI] [PubMed] [Google Scholar]
- Evaluation and treatment of borderline dysplasia: Moving beyond the lateral center edge angle. Vaudreuil Nicholas J., McClincy Michael P. Feb;2020 Current Reviews in Musculoskeletal Medicine. 13(1):28–37. doi: 10.1007/s12178-020-09599-y. doi: 10.1007/s12178-020-09599-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mild or borderline hip dysplasia: Are we characterizing hips with a lateral center-edge angle between 18 degrees and 25 degrees appropriately? McClincy Michael P., Wylie James D., Yen Yi-Meng, Novais Eduardo N. 2019The American Journal of Sports Medicine. 47(1):112–122. doi: 10.1177/0363546518810731. doi: 10.1177/0363546518810731. [DOI] [PubMed] [Google Scholar]


