Abstract
Background
The novel pulsed thulium:yttrium–aluminum–garnet (p-Tm:YAG) laser was recently introduced. Current studies present promising p-Tm:YAG ablation efficiency, although all are based on non-human stone models or with unknown stone composition. The present study aimed to evaluate p-Tm:YAG ablation efficiency for stone dust from human urinary stones of known compositions.
Methods
Calcium oxalate monohydrate (COM) and uric acid (UA) stones were subjected to lithotripsy in vitro using a p-Tm:YAG laser generator (Thulio®, Dornier MedTech GmbH, Germany). 200 J was applied at 0.1 J × 100 Hz, 0.4 J × 25 Hz or 2.0 J × 5 Hz (average 10W). Ablated stone dust mass was calculated from weight difference between pre-lithotripsy stone and post-lithotripsy fragments > 250 µm. Estimated ablated volume was calculated using prior known stone densities (COM: 2.04 mg/mm3, UA: 1.55 mg/mm3).
Results
Mean ablation mass efficiency was 0.04, 0.06, 0.07 mg/J (COM) and 0.04, 0.05, 0.06 mg/J (UA) for each laser setting, respectively. This translated to 0.021, 0.029, 0.034 mm3/J (COM) and 0.026, 0.030, 0.039 mm3/J (UA). Mean energy consumption was 26, 18, 17 J/mg (COM) and 32, 23, 17 J/mg (UA). This translated to 53, 37, 34 J/mm3 (COM) and 50, 36, 26 J/mm3 (UA). There were no statistically significant differences for laser settings or stone types (all p > 0.05).
Conclusion
To our knowledge, this is the first study showing ablation efficiency of the p-Tm:YAG laser for stone dust from human urinary stones of known compositions. The p-Tm:YAG seems to ablate COM and UA equally well, with no statistically significant differences between differing laser settings.
Keywords: Laser, Pulsed Thulium:YAG, Kidney stones, Ablation, Endourology, Ureteroscopy, Dust
Introduction
The prevalence of urinary stone disease has been increasing over the past decade, and in tandem so has the volume of endourological surgeries to treat the disease burden [1]. Within the field of endourological surgery, the laser has been established as the main tool for lithotripsy over the last three decades [2]. For laser surgical techniques, stone dusting has become increasingly popular together with newest generation lasers [3–5].
Currently, the holmium:yttrium–aluminum–garnet (Ho:YAG) and the more recent thulium fiber laser (TFL) are widely used in endourological procedures [6–8], with their effectiveness against human urinary stones extensively evaluated [9–14].
Recently, novel pulsed thulium:yttrium–aluminum–garnet (p-Tm:YAG) lasers have been introduced to the market for clinical use. Studies on p-Tm:YAG ablation found in literature so far have shown promising data, although all these studies were based on artificial stone lithotripsy models (BegoStone, plaster of Paris, gypsum/glass) [15–17]. It was only until recently that the p-Tm:YAG was shown capable to ablate the most common human urinary stone types [18]. Two recent studies evaluated the clinical efficacy and safety of the p-Tm:YAG on case series of patients undergoing retrograde intrarenal surgery [19] and mini-percutaneous nephrolithotomy [20]. Both studies conclude that the p-Tm:YAG seems very promising, although no information relating to its applicability to differing stone compositions was provided.
With the above background, the aim of the present study was to evaluate the currently unexplored question of p-Tm:YAG ablation efficiency for stone dust from human urinary stones of two known compositions.
Materials and methods
Human urinary stones of two compositions were obtained from a stone biobank at Tenon Hospital, Paris: calcium oxalate monohydrate (COM) and uric acid (UA). Stones were chosen to match a diameter of about 5 mm, accepting that not all stones were perfectly spherical. This was in a comparable size range with other in vitro Ho:YAG and TFL ablation studies using human kidney stones [21–24] and stone phantoms [25, 26]. To simulate in vivo settings, all stones were immersed in saline for 24 h prior to experiments, due to kidney stones being of a crystalline structure primarily, but growing in a biological environment with complex intercrystalline spaces likely filled with urine [27].
Each stone separately underwent laser lithotripsy using the Dornier Thulio® p-Tm:YAG with its 270 µm core-diameter Dornier Thulio® Performance reusable laser fiber (Dornier MedTech GmbH, Wessling, Germany).
Since optimal settings for the production of stone dust using the p-Tm:YAG were not known at the time of this study, we explored several different laser settings. For each sample submitted to lithotripsy, a cumulative energy of 200 J was applied, with the use of one of three laser settings: 0.1 J × 100 Hz, 0.4 J × 25 Hz, and 2.0 J × 5 Hz. All chosen settings resulted in an average power of 10W. For each stone sample, as the average power used (10W) was the same to reach a common cumulative energy (200J), the lasing time was the same throughout all experiments. As suggested by the graphical user interface (GUI), the “Dusting” mode was used for the lower pulse range (the GUI proposes a pulse energy ranging from 0.1 J to 0.5 J in this mode), whereas the “Standard Fragmenting” mode was used for the higher pulse range (the GUI proposes a pulse energy ranging from 0.6 J to 2.0 J in this mode). For the 0.1 J × 100 Hz setting, we chose the lowest pulse energy possible (0.1 J) on the GUI in “Dusting” mode with a corresponding frequency (100 Hz) to reach a power of 10W. For the 0.4 J × 25 Hz setting, the pulse energy was matched to a generally accepted dusting setting (0.4 J × 25 Hz) for lithotripsy with Ho:YAG and TFL (GUI “Dusting” mode) [4, 28]. The third 2.0 J × 5 Hz setting was chosen to evaluate high pulse energy lithotripsy, meeting the previously set 10W average power (GUI “Standard Fragmenting” mode). As pulse duration was not displayed on the GUI and could not be changed within the operating modes themselves, this laser setting was not further explored. For each of the three laser settings and for each two stone types, lithotripsy was repeated separately with 5 urinary stones resulting in 5 measurements per laser setting and stone type (total of 30 samples).
Laser lithotripsy was performed under direct endoscopic vision in a 10 ml glass cuvette using the OTU WiScope (OTU Medical Inc, CA, USA) flexible ureteroscope, with sterile 0.9% sodium chloride saline irrigation at room temperature (21 °C) and constant irrigation pressure (40 cmH2O). Before lithotripsy of each stone sample, the laser fiber tip was cut with regular metal surgical scissors through the protective blue jacket. We used the same reusable fiber for all experiments performed. During lithotripsy, the laser fiber tip was continuously maintained as close as possible to the surface of the stones (i.e., working distance as short as possible).
Primary outcome was ablation mass efficiency defined as ablated stone dust mass per unit of laser energy (mg/J). Ablated stone dust mass was calculated from the difference in weight between the pre-lithotripsy stone and post-lithotripsy remnant fragments, in reminiscence of prior studies using this method to evaluate ablation parameters [17, 29–32]. Post-lithotripsy fragments were defined as particles > 250 µm, considering a prior study defining stone dust as stone particle ≤ 250 µm [33]. For that purpose, each post-lithotripsy sample was separately passed through a 250 µm mesh size laboratory sieve (Eisco sorting sieve, Eisco Scientific LLC, NY, USA), and poured with a total of 500 ml saline to isolate remnants fragments from filtered-off stone dust. For weighing of stones and remnant fragments, samples were dried with dabbing of filter paper to remove excess saline, then weighed with a laboratory balance AX105DR Analytical Balance (Mettler-Toledo GmbH, Greifensee, Switzerland).
Secondary outcome was estimated ablation volume efficiency in terms of ablated volume per unit of energy (mm3/J), to relate with prior studies that evaluated ablated volume rather than weight in vitro [9, 34, 35]. For calculation of estimated ablated stone volume, stone density values of 2.038 mg/mm3 for COM and 1.546 mg/mm3 for UA were used, respectively, based on measurements from a prior study using a pycnometer for evaluation of human urinary stone density [36]. The estimated ablated volume was then calculated by ablated stone dust mass divided by stone density (volume = mass / density).
Finally, ablation mass efficiency (mg/J) and ablation volume efficiency (mm3/J) were converted to energy consumption (J/mg and J/mm3, respectively). This allowed evaluation of the secondary outcome from the perspective of “How much energy do we need to ablate 1 mm3 of stone”, to relate with prior studies that evaluated laser energy consumption rather than laser efficiency [9, 10, 14, 37–44].
Statistical analysis
Analyses comparing the three laser settings for each stone composition type were performed using one-way ANOVA with Tukey post hoc comparisons. Unpaired t test analyses were performed to evaluate pre-lithotripsy weight, ablation efficiency, and energy consumption between COM and UA stones. A two-sided p value < 0.05 was considered statistically significant. All descriptive and statistical analyses were performed with GraphPad Prism 9.5.1 (GraphPad Software, La Jolla CA, USA).
Results
Ablated stone dust mass
Mean stone weight before lithotripsy for COM was 22 mg (95% CI 20–25) vs. UA 27 mg (95% CI 23–31) (p = 0.07). Mean ablated stone dust mass with 200 J of laser energy was 8.4, 11.8, 13.9 mg for COM (ANOVA p = 0.08) and 8.1, 9.3, 12.1 mg for UA (ANOVA p = 0.11) for the laser settings 0.1 J × 100 Hz, 0.4 J × 25 Hz, 2.0 J × 5 Hz, respectively (Table 1).
Table 1.
p-Tm:YAG ablation efficiency for stone dust from human urinary stones
| Stone composition | Laser setting (200 J@10W) | One-way ANOVA for laser settings within each stone composition | |||
|---|---|---|---|---|---|
| 0.1 J × 100 Hz | 0.4 J × 25 Hz | 2.0 J × 5 Hz | |||
|
Ablated stone dust mass (mg) (95% CI) |
COM |
8.4 (5.1–11.7) |
11.8 (7.9–15.8) |
13.9 (8.2–19.6) |
p = 0.08 |
| UA |
8.1 (3.9–12.3) |
9.3 (5.7–12.9) |
12.1 (9.5–14.8) |
p = 0.11 | |
| Student’s t test for each laser setting | p = 0.89 | p = 0.22 | p = 0.45 | – | |
|
Ablation mass efficiency (mg/J) (95% CI) |
COM |
0.042 (0.025–0.058) |
0.059 (0.039–0.079) |
0.070 (0.041–0.098) |
p = 0.08 |
| UA |
0.041 (0.019–0.062) |
0.046 (0.028–0.064) |
0.061 (0.047–0.074) |
p = 0.11 | |
| Student’s t test for each laser setting | p = 0.89 | p = 0.22 | p = 0.45 | – | |
|
Ablation volume efficiency* (mm3/J) (95% CI) |
COM |
0.021 (0.012–0.029) |
0.029 (0.019–0.039) |
0.034 (0.020–0.048) |
p = 0.08 |
| UA |
0.026 (0.013–0.040) |
0.030 (0.018–0.042) |
0.039 (0.031–0.048) |
p = 0.11 | |
| Student’s t test for each laser setting | p = 0.35 | p = 0.86 | p = 0.42 | - | |
*Volume estimated using prior reported stone density of natural human urinary stones[36]
Ablation efficiency
Overall ablation efficiency was 0.053 mg/J (95% CI 0.046–0.060), translating to 0.030 mm3/J (95% CI 0.026–0.034). When considering only COM samples, overall ablation efficiency was 0.057 mg/J (95% CI 0.046–0.068), translating to 0.028 mm3/J (95% CI 0.022–0.033). For UA samples, overall ablation efficiency was 0.049 mg/J (95% CI 0.040–0.058), translating to 0.032 mm3/J (95% CI 0.026–0.037).
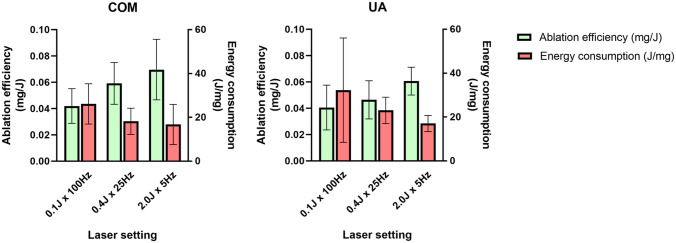
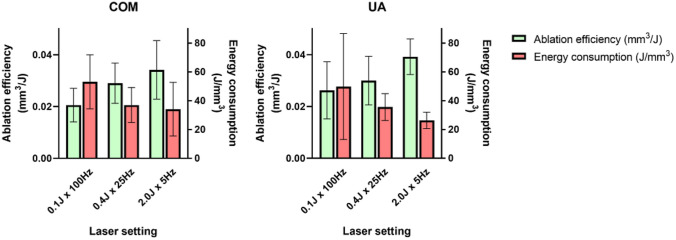
Comparisons of ablation efficiency for each laser setting and stone type are summarized in Table 1, as well as in Fig. 1 (mass) and Fig. 2. (volume). There were no significant differences of ablation efficiency between settings for both COM and UA (ANOVA p = 0.08 and p = 0.11 respectively). Likewise, when comparing stone compositions within each laser setting, there were no significant differences (all p > 0.05).
Fig. 1.
p-Tm:YAG laser ablation mass efficiency (mg/J) and energy consumption (J/mg) for stone dust
Fig. 2.
p-Tm:YAG laser ablation volume efficiency (mm3/J) and energy consumption (J/mm3) based on estimated ablated stone dust volume
Energy consumption
Overall energy consumption was 22 J/mg (95% CI 18–27), translating to 39 J/mm3 (95% CI 32–47). For COM, this was 20 J/mg (95% CI 15–25), translating to 41 J/mm3 (95% CI 32–51), and for UA 24 J/mg (95% CI 16–32), translating to 37 J/mm3 (95% CI 25–50). Comparisons of estimated energy consumption for each laser setting and stone type are summarized in Table 2, Fig. 1 (mass), and Fig. 2 (volume). In analogy to laser ablation efficiency comparisons, there were no significant differences of energy consumption between COM and UA for laser settings (ANOVA p = 0.20 and p = 0.27, respectively). Likewise, when comparing stone compositions within each laser setting, there were no significant differences (all p > 0.05).
Table 2.
p-Tm:YAG energy consumption for stone dust from human urinary stones
| Mean measurement | Stone composition | Laser setting (200 J@10W) | One-way ANOVA for laser settings within each stone composition | ||
|---|---|---|---|---|---|
| 0.1 J × 100 Hz | 0.4 J × 25 Hz | 2.0 J × 5 Hz | |||
| Energy per ablated mass (J/mg) (95% CI) | COM |
26.1 (14.7–37.5) |
18.2 (10.8–25.6) |
16.8 (5.4–28.1) |
p = 0.20 |
| UA |
32.2 (2.7–61.8) |
23.0 (15.5–30.5) |
17.0 (12.4–21.6) |
p = 0.27 | |
| Student’s t test for each laser setting | p = 0.61 | p = 0.24 | p = 0.95 | – | |
| Energy per estimated ablated volume* (J/mm3) (95% CI) | COM |
53.2 (29.9–76.5) |
37.0 (21.9–52.2) |
34.1 (11.0–57.3) |
p = 0.20 |
| UA |
49.8 (4.2–95.5) |
35.6 (24.0–47.2) |
26.3 (19.2–33.4) |
p = 0.27 | |
| Student’s t test for each laser setting | p = 0.86 | p = 0.84 | p = 0.40 | – | |
*Volume estimated using prior reported stone density of natural human urinary stones[36]
Discussion
To the best of our knowledge, this is the first study evaluating ablation efficiency of the p-Tm:YAG laser for stone dust from human urinary stones of different compositions. The p-Tm:YAG laser appears to ablate COM and UA stones equally well, with no significant differences between differing laser settings.
Additionally, this study provides a unique methodology accounting for the quality of ablated stone mass (i.e., particles ≤ 250 µm). Prior studies that used volumetric measurements in highly standardized in vitro settings (e.g., single-pulse craters, or fissures on perfectly flat artificial stones) [9, 17, 34, 35] completely omitted the quality assessment of pulverized stone material. Larger stone fragments may arguably have chipped-off the “main stone” during lithotripsy and falsely account for ablated stone volume [32]. Super-standardized study setups, with fixed standoff distance of the laser fiber tip not adjusted throughout the lithotripsy process, may not entirely reflect real-life laser application. Therefore, we deliberately chose a study setting simulating in vivo lithotripsy with free-hand application, where the targeting of stones’ surfaces will never be as standardized as it can be set in vitro.
Regarding choice of ablation efficiency measurement units, there is no current consensus on standardized terminology. Therefore, we chose mg/J and mm3/J units to reflect that a higher value would represent a more efficient process of laser lithotripsy. This is opposed to using energy consumption (J/mg and J/mm3) [34], where counterintuitively the higher the value, the worse the ablation efficiency. For the sake of readability and considering that several prior studies reporting their results as J/mm3 rather than mm3/J [9, 14, 37, 38], we provided our results considering both energy consumption and laser efficiency measurement units. The energy consumption was in the range 26.3–53.2 J/mm3 in the present study, translating to a laser efficiency of 0.021–0.039 mm3/J. These measurements compare with a wide range of different energy consumption outcomes reported for Ho:YAG and TFL lasers, ranging from 2.0–43.5 J/mm3 in vitro and 2.7–47.8 J/mm3 in vivo [45]. Direct comparison of results between these studies seems hazardous, unless standardized lasering conditions and outcome measurement methods are applied (including stone composition types, volume, density, laser settings, and total energy). Thus, further in vivo studies are warranted to compare ablation efficiency between these three lasers on human urinary stones head-to-head under the same conditions.
Worth mentioning, the methodology of our study required stone weight measurement as a primary outcome, while clinical decisions are mostly based on stone size metrics (ideally stone volume). Therefore, ablated stone mass was converted to estimated ablated stone volume. Considering ablated stone volume rather than mass, the general pattern of higher ablated stone weight favoring COM translated to a higher ablated stone volume favoring UA instead. Thus, evaluation of laser performance should always include analysis and discussion of several important metrics, including stone mass, density, and volume.
The optimal settings for ablation of human urinary stones with the p-Tm:YAG is currently unknown. It is interesting to note that there is a non-significant pattern for better ablation efficiency favoring a higher pulse energy (2.0 J × 5 Hz), followed by the next lower pulse energy (0.4 J × 25 Hz) and finally worst ablation efficiency for the lowest pulse energy setting (0.1 J × 100 Hz). Prior in vitro studies on evaluation versions of the p-Tm:YAG using BegoStone plates had similar findings of increased ablation efficiency when single-pulse energy was increased [16, 17]. Our study setup additionally accounts for some degree of retropulsion at higher pulse energies, and as aforementioned uses strict quality assessment of pulverized stone material for particle size meeting a known stone dust definition. This is not accounted for in the prior p-Tm:YAG study setups using fixed stone plates measuring effects of ablation craters [16, 17], or with omittance of chipped-off stone particle size assessment [17]. Furthermore, limitations of using BegoStone as compared to human stones are stated as limitations in one study [16]. No randomized clinical trial comparing laser settings and stone compositions for the p-Tm:YAG is currently available, and this should be further explored in vivo. When choosing laser settings, there are other considerations besides laser ablation efficiency. Based on clinical experience, the surgeon should be aware that a higher pulse energy may be associated with higher risk of stone retropulsion and mucosal bleeding. High frequency settings may impair visibility and cause poorer control on the target, which might be particularly harmful when lasering with high frequency in the ureter.
Of final note, COM is generally accepted as the “harder” stone to ablate compared to UA [9, 32, 46, 47]. Astonishingly no significant differences in ablation efficiency were found between these two stone types in the present study. This is analogous to a recent study where the high power Ho:YAG MOSES technology was found to ablate stones equally well, independent of stone density or composition type [14]. It is not known if the newest generation laser might ablate all stone types equally. This is a desirable property that needs to be further evaluated, with potential clinical implications affecting choice of laser and preoperative planning.
The study has several potential limitations. First, the present study is an in vitro attempt to assess p-Tm:YAG laser lithotripsy ablation efficiency that may impact in vivo use of the laser. The interpretation of data must be taken with care since environmental and surgical factors may impact clinical translation of the findings. Second, the sizes of the initial human urinary stones submitted to lithotripsy were rather small and not standardized, although this limitation is inherent to the use of human urinary stones, in reminiscence of prior in vitro Ho:YAG and TFL ablation studies using human kidney stones [21–24]. We balanced the necessity of repeated measurements using comparable human stones (5 repeated measurements × 3 laser settings × 2 stone types = total 30 samples) with the hypothetical ideal setup that was not possible to obtain (i.e., 30 stones samples of > 1 cm each). In addition, our study setup determined ablation performance measured by the stone weight difference pre-/post-lithotripsy. A recent randomized control trial comparing pulse-modulated Ho:YAG and TFL for renal and ureteral stones had small average stone sizes as well (largest stone diameter mean of 8.4/8.9 mm and median of 7.4/7.9 mm IQR [5.3–11.3]/[6.0–11.1] for each arm), reflecting that stones in real life, at least in the American setting and arguably the European setting, are not very large [48]. It would be interesting to repeat a similar study setup on several other stone compositions and if possible, larger stones in vivo to evaluate for differences. Third, rather than oven or freeze drying, the stones were dried with filter paper. However, the methodology was consistent for both pre- and post-lithotripsy samples, thus arguably mitigating the risks of a systematic bias. Finally, a limit of 200 J of energy was applied. As the mechanisms of relevance for lithotripsy with the p-Tm:YAG are not yet perfectly understood, further studies may be warranted looking at higher total energy applied. This may be closer to real world conditions.
Conclusion
Based on our results, the p-Tm:YAG seems to ablate COM and UA stones equally well with no statistically significant differences, demonstrating good ablation regardless of composition or differing laser settings. Future perspectives to explore for the p-Tm:YAG include determining the best laser settings for dusting and fragmenting. Also, it will be important to compare the p-Tm:YAG with other laser technologies and further urinary stone types.
Author’s contributions
J-LK: protocol/project development, data collection or management, data analysis, manuscript writing/editing. EV: data analysis, manuscript writing/editing. VDC: data analysis, manuscript writing/editing. FP: data analysis, manuscript writing/editing. YB: data analysis, manuscript writing/editing. AD: data analysis, manuscript writing/editing. AS: data analysis, manuscript writing/editing. NS: data analysis, manuscript writing/editing. FAS: data analysis, manuscript writing/editing. MH: data analysis, manuscript writing/editing. CP: data analysis, manuscript writing/editing. MD: data collection or management, data analysis, manuscript writing/editing. OT: research concept, data analysis, manuscript writing/editing. DE: data analysis, manuscript writing/editing. EXK: research concept, protocol/project development, data collection or management, data analysis, manuscript writing/editing.
Funding
Open access funding provided by University of Zurich. No funding was received for conducting this study.
Data availability
On request to corresponding author for raw data on the experimental setup.
Declarations
Conflict of interest
Vincent De Coninck is a speaker and/or consultant for BD Bard and Coloplast, and has no specific conflicts of interest relevant to this work. Olivier Traxer is a consultant for Coloplast, Karl Storz, Rocamed, Quanta Systems, Ambu, Boston Scientific and IPG Medical, and has no specific conflicts relevant to this work. Etienne Xavier Keller is a speaker and/or consultant for Coloplast, Olympus, Boston Scientific, Recordati, Debiopharm and Alnylam, and has no specific conflicts of interest relevant to this work. All other authors have no relevant financial or non-financial interests to disclose.
Competing interest
The Thulio® p-Tm:YAG laser generator was provided by Dornier MedTech Gmbh for a short time period specifically dedicated to the present study.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Geraghty RM, Jones P, Somani BK. Worldwide trends of urinary stone disease treatment over the last two decades: a systematic review. J Endourol. 2017;31(6):547–556. doi: 10.1089/end.2016.0895. [DOI] [PubMed] [Google Scholar]
- 2.Kronenberg P, Traxer O. Update on lasers in urology 2014: current assessment on holmium:yttrium–aluminum–garnet (Ho:YAG) laser lithotripter settings and laser fibers. World J Urol. 2015;33(4):463–469. doi: 10.1007/s00345-014-1395-1. [DOI] [PubMed] [Google Scholar]
- 3.Matlaga BR, Chew B, Eisner B, Humphreys M, Knudsen B, Krambeck A, et al. Ureteroscopic laser lithotripsy: a review of dusting vs fragmentation with extraction. J Endourol. 2018;32(1):1–6. doi: 10.1089/end.2017.0641. [DOI] [PubMed] [Google Scholar]
- 4.Doizi S, Keller EX, De Coninck V, Traxer O. Dusting technique for lithotripsy: what does it mean? Nat Rev Urol. 2018;15(11):653–654. doi: 10.1038/s41585-018-0042-9. [DOI] [PubMed] [Google Scholar]
- 5.Keller EX, De Coninck V, Doizi S, Daudon M, Traxer O. Thulium fiber laser: ready to dust all urinary stone composition types? World J Urol. 2020 doi: 10.1007/s00345-020-03217-9. [DOI] [PubMed] [Google Scholar]
- 6.Giusti G, Pupulin M, Proietti S. Which is the best laser for lithotripsy? The referee point of view. Eur Urol Open Sci. 2022;44:20–22. doi: 10.1016/j.euros.2022.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Traxer O, Sierra A, Corrales M. Which is the best laser for lithotripsy? Thulium fiber laser. Eur Urol Open Sci. 2022;44:15–17. doi: 10.1016/j.euros.2022.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim HJ, Ghani KR. Which is the best laser for lithotripsy? Holmium laser. Eur Urol Open Sci. 2022;44:27–29. doi: 10.1016/j.euros.2022.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panthier F, Ventimiglia E, Berthe L, Chaussain C, Daudon M, Doizi S, et al. How much energy do we need to ablate 1 mm3 of stone during Ho:YAG laser lithotripsy? An in vitro study. World J Urol. 2020;38(11):2945–2953. doi: 10.1007/s00345-020-03091-5. [DOI] [PubMed] [Google Scholar]
- 10.Sierra A, Corrales M, Kolvatzis M, Traxer O. Initial clinical experience with the thulium fiber laser from Quanta System: First 50 reported cases. World J Urol. 2022;40(10):2549–2553. doi: 10.1007/s00345-022-04096-y. [DOI] [PubMed] [Google Scholar]
- 11.Traxer O, Corrales M. Managing urolithiasis with thulium fiber laser: Updated real-life results—a systematic review. J Clin Med. 2021 doi: 10.3390/jcm10153390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Traxer O, Keller EX. Thulium fiber laser: the new player for kidney stone treatment? A comparison with Holmium:YAG laser. World J Urol. 2020;38(8):1883–1894. doi: 10.1007/s00345-019-02654-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Castellani D, Fong KY, Lim EJ, Chew BH, Tailly T, Emiliani E, et al. Comparison between Holmium:YAG laser with MOSES technology versus thulium fiber laser lithotripsy in retrograde intrarenal surgery for kidney stones in adults: a propensity score-matched analysis from the FLEXible ureteroscopy outcomes registry (FLEXOR) J Urol. 2023 doi: 10.1097/JU.0000000000003504. [DOI] [PubMed] [Google Scholar]
- 14.Majdalany SE, Levin BA, Ghani KR. The efficiency of moses technology holmium laser for treating renal stones during flexible ureteroscopy: relationship between stone volume, time, and energy. J Endourol. 2021;35(S3):S14–S21. doi: 10.1089/end.2021.0592. [DOI] [PubMed] [Google Scholar]
- 15.Kraft L, Petzold R, Suarez-Ibarrola R, Miernik A. In vitro fragmentation performance of a novel, pulsed Thulium solid-state laser compared to a Thulium fibre laser and standard Ho:YAG laser. Lasers Med Sci. 2022;37(3):2071–2078. doi: 10.1007/s10103-021-03495-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petzold R, Miernik A, Suarez-Ibarrola R. In vitro dusting performance of a new solid state thulium laser compared to holmium laser lithotripsy. J Endourol. 2021;35(2):221–225. doi: 10.1089/end.2020.0525. [DOI] [PubMed] [Google Scholar]
- 17.Kraft L, Yilmaz M, Petzold R, Gratzke C, Suarez-Ibarrola R, Miernik A. Dusting efficiency of a novel pulsed thulium: yttrium aluminum garnet laser vs a thulium fiber laser. J Endourol. 2022;36(2):259–265. doi: 10.1089/end.2021.0441. [DOI] [PubMed] [Google Scholar]
- 18.Kwok JL, Ventimiglia E, De Coninck V, Corrales M, Sierra A, Panthier F, et al. Pulsed thulium:YAG laser—ready to dust all urinary stone composition types? Results from a PEARLS analysis. World J Urol. 2023 doi: 10.1007/s00345-023-04549-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Panthier F, Solano C, Chicaud M, Kutchukian S, Candela L, Doizi S, et al. Initial clinical experience with the pulsed solid-state thulium YAG laser from Dornier during RIRS: first 25 cases. World J Urol. 2023 doi: 10.1007/s00345-023-04501-0. [DOI] [PubMed] [Google Scholar]
- 20.Bergmann J, Rosenbaum CM, Netsch C, Gross AJ, Becker B. First clinical experience of a novel pulsed solid-state Thulium:YAG laser during percutaneous nephrolithotomy. J Clin Med. 2023 doi: 10.3390/jcm12072588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilson CR, Hardy LA, Kennedy JD, Irby PB, Fried NM. Miniature ball-tip optical fibers for use in thulium fiber laser ablation of kidney stones. J Biomed Opt. 2016 doi: 10.1117/1.JBO.21.1.018003. [DOI] [PubMed] [Google Scholar]
- 22.Hardy LA, Wilson CR, Irby PB, Fried NM. Rapid thulium fiber laser lithotripsy at pulse rates up to 500 Hz using a stone basket. IEEE J Select Top Quant Electron. 2014 doi: 10.1109/JSTQE.2014.2305715. [DOI] [Google Scholar]
- 23.Hutchens TC, Gonzalez DA, Irby PB, Fried NM. Fiber optic muzzle brake tip for reducing fiber burnback and stone retropulsion during thulium fiber laser lithotripsy. J Biomed Opt. 2017 doi: 10.1117/1.JBO.22.1.018001. [DOI] [PubMed] [Google Scholar]
- 24.Hardy LA, Wilson CR, Irby PB, Fried NM. Thulium fiber laser lithotripsy in an in vitro ureter model. J Biomed Opt. 2014 doi: 10.1117/1.JBO.19.12.128001. [DOI] [PubMed] [Google Scholar]
- 25.Taratkin M, Azilgareeva C, Corrales M, Teoh JYC, Allenov S, Inoyatov J, et al. Superpulse thulium fiber laser lithotripsy: an in vitro comparison of 200 μm and 150 μm laser fibers. World J Urol. 2021;39(12):4459–4464. doi: 10.1007/s00345-021-03800-8. [DOI] [PubMed] [Google Scholar]
- 26.Ventimiglia E, Doizi S, Kovalenko A, Andreeva V, Traxer O. Effect of temporal pulse shape on urinary stone phantom retropulsion rate and ablation efficiency using holmium:YAG and super-pulse thulium fibre lasers. BJU Int. 2020;126(1):159–167. doi: 10.1111/bju.15079. [DOI] [PubMed] [Google Scholar]
- 27.Khan SR, Hackett RL. Role of organic matrix in urinary stone formation: an ultrastructural study of crystal matrix interface of calcium oxalate monohydrate stones. J Urol. 1993;150(1):239–245. doi: 10.1016/S0022-5347(17)35454-X. [DOI] [PubMed] [Google Scholar]
- 28.Sierra A, Corrales M, Piñero A, Traxer O. Thulium fiber laser pre-settings during ureterorenoscopy: Twitter’s experts’ recommendations. World J Urol. 2022;40(6):1529–1535. doi: 10.1007/s00345-022-03966-9. [DOI] [PubMed] [Google Scholar]
- 29.Wollin DA, Ackerman A, Yang C, Chen T, Simmons WN, Preminger GM, et al. Variable pulse duration from a new Holmium:YAG laser: the effect on stone comminution, fiber tip degradation, and retropulsion in a dusting model. Urology. 2017;103:47–51. doi: 10.1016/j.urology.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 30.Wollin DA, Tom WR, Jiang R, Simmons WN, Preminger GM, Lipkin ME. An in vitro evaluation of laser settings and location in the efficiency of the popcorn effect. Urolithiasis. 2019;47(4):377–382. doi: 10.1007/s00240-018-1066-6. [DOI] [PubMed] [Google Scholar]
- 31.Emiliani E, Talso M, Cho SY, Baghdadi M, Mahmoud S, Pinheiro H, et al. Optimal settings for the noncontact Holmium:YAG stone fragmentation popcorn technique. J Urol. 2017;198(3):702–706. doi: 10.1016/j.juro.2017.02.3371. [DOI] [PubMed] [Google Scholar]
- 32.Teichman JMH, Vassar GJ, Bishoff JT, Bellman GC. Holmium:YAG lithotripsy yields smaller fragments than lithoclast, pulsed dye laser or electrohydraulic lithotripsy. J Urol. 1998;159(1):17–23. doi: 10.1016/S0022-5347(01)63998-3. [DOI] [PubMed] [Google Scholar]
- 33.Keller EX, De Coninck V, Doizi S, Daudon M, Traxer O. What is the exact definition of stone dust? An in vitro evaluation. World J Urol. 2021;39(1):187–194. doi: 10.1007/s00345-020-03178-z. [DOI] [PubMed] [Google Scholar]
- 34.King JB, Katta N, Teichman JMH, Tunnell JW, Milner TE. Increased ablation efficiency in hard and soft tissues using an annular beam. Progress in Biomedical Optics and Imaging - Proceedings of SPIE2022.
- 35.Aldoukhi AH, Black KM, Hall TL, Roberts WW, Ghani KR. Frequency threshold for ablation during holmium laser lithotripsy: How high can you go? J Endourol. 2020;34(10):1075–1081. doi: 10.1089/end.2020.0149. [DOI] [PubMed] [Google Scholar]
- 36.Zhong P, Chuong CJ, Preminger GM. Characterization of fracture toughness of renal calculi using a microindentation technique. J Mater Sci Lett. 1993;12(18):1460–1462. doi: 10.1007/BF00591608. [DOI] [Google Scholar]
- 37.Ventimiglia E, Pauchard F, Gorgen ARH, Panthier F, Doizi S, Traxer O. How do we assess the efficacy of Ho:YAG low-power laser lithotripsy for the treatment of upper tract urinary stones? Introducing the Joules/mm3 and laser activity concepts. World J Urol. 2021;39(3):891–896. doi: 10.1007/s00345-020-03241-9. [DOI] [PubMed] [Google Scholar]
- 38.Shrestha A, Corrales M, Adhikari B, Chapagain A, Traxer O. Comparison of low power and high power holmium YAG laser settings in flexible ureteroscopy. World J Urol. 2022;40(7):1839–1844. doi: 10.1007/s00345-022-04040-0. [DOI] [PubMed] [Google Scholar]
- 39.Mekayten M, Lorber A, Katafigiotis I, Sfoungaristos S, Leotsakos I, Heifetz EM, et al. Will stone density stop being a key factor in endourology? The impact of stone density on laser time using lumenis laser p120w and standard 20 W laser: a comparative study. J Endourol. 2019;33(7):585–589. doi: 10.1089/end.2019.0181. [DOI] [PubMed] [Google Scholar]
- 40.Corrales M, Traxer O. Initial clinical experience with the new thulium fiber laser: first 50 cases. World J Urol. 2021;39(10):3945–3950. doi: 10.1007/s00345-021-03616-6. [DOI] [PubMed] [Google Scholar]
- 41.Enikeev D, Taratkin M, Klimov R, Inoyatov J, Azilgareeva C, Ali S, et al. Superpulsed thulium fiber laser for stone dusting: in search of a perfect ablation regimen-a prospective single-center study. J Endourol. 2020;34(11):1175–1179. doi: 10.1089/end.2020.0519. [DOI] [PubMed] [Google Scholar]
- 42.Enikeev D, Grigoryan V, Fokin I, Morozov A, Taratkin M, Klimov R, et al. Endoscopic lithotripsy with a SuperPulsed thulium-fiber laser for ureteral stones: a single-center experience. Int J Urol. 2021;28(3):261–265. doi: 10.1111/iju.14443. [DOI] [PubMed] [Google Scholar]
- 43.Korolev D, Akopyan G, Tsarichenko D, Shpikina A, Ali S, Chinenov D, et al. Minimally invasive percutaneous nephrolithotomy with SuperPulsed Thulium-fiber laser. Urolithiasis. 2021;49(5):485–491. doi: 10.1007/s00240-021-01258-2. [DOI] [PubMed] [Google Scholar]
- 44.Taratkin M, Azilgareeva C, Korolev D, Barghouthy Y, Tsarichenko D, Akopyan G, et al. Prospective single-center study of superpulsed thulium fiber laser in retrograde intrarenal surgery: initial clinical data. Urol Int. 2022;106(4):404–410. doi: 10.1159/000516933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kwok J-L, De Coninck V, Ventimiglia E, Panthier F, Corrales M, Sierra A et al. Laser ablation efficiency, laser ablation speed and laser energy consumption during lithotripsy: what are they and how are they defined? A systematic review and proposal for a standardized terminology. Eur Urol Focus (Accepted) [DOI] [PubMed]
- 46.Chan KF, Choi B, Vargas G, Hammer DX, Sorg B, Pfefer TJ, et al. Free electron laser ablation of urinary calculi: an experimental study. IEEE J Select Top Quant Electron. 2001;7(6):1022–1033. doi: 10.1109/2944.983308. [DOI] [Google Scholar]
- 47.Razvi HA, Denstedt JD, Chun SS, Sales JL. Intracorporeal lithotripsy with the holmium:YAG laser. J Urol. 1996;156(3):912–914. doi: 10.1016/S0022-5347(01)65661-1. [DOI] [PubMed] [Google Scholar]
- 48.Haas CR, Knoedler MA, Li S, Gralnek DR, Best SL, Penniston KL, et al. Pulse-modulated Holmium:YAG laser vs the thulium fiber laser for renal and ureteral stones: a single-center prospective randomized clinical trial. J Urol. 2023;209(2):374–383. doi: 10.1097/JU.0000000000003050. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
On request to corresponding author for raw data on the experimental setup.