Abstract
Introduction:
Spinal cord injury (SCI) is characterized by serious both motor and sensory disability of the limbs below the injured segment. It is the most traumatic disorder among central nervous system (CNS) conditions which not only leads to psychological and physical harm to patients but also results in a dramatic loss in the life quality. Many efforts have been developed to find a therapeutic approach for SCI; however, an effective treatment has not yet been found. The lack of effective treatment approach and rehabilitation of SCI underscores the need to identify novel approaches. Tissue engineering associated with stem cells has been recently introduced as an effective treatment approaches for traumatic SCI. Although, low survival rates, immune rejection, cell dedifferentiation, and tumorigenicity have been addressed for tissue engineering. Regenerative medicine is an interdisciplinary field developing and applying tissue engineering, stem cell (SC) therapy, and SC-derived extracellular vesicle therapy that aims to provide reliable and safe ways to replace injured tissues and organs. The application of mesenchymal stem cells-derived extracellular vesicles (MSC-EVs) has recently attracted attention to improve central nervous system dysfunction such as SCI, mainly by promoting neurogenesis and angiogenesis.
Methods:
In this review article the latest information of SCI improvement using stem cell-derived extracellular vesicles published data in the Web of Science, Scopus, Science Direct and Pub Med databases were collected.
Results:
The data collected show that MSC-EVs, including exosomes, alone or in combination with scaffolds can can regenerate the injured nerve in SCI.
Conclusion:
This study summarizes the efficacy of MSC-EVs, including exosomes, alone or in combination with scaffolds in the treatment of SCI and then discusses the therapeutic outcomes observed in SCI experimental models following treatment with MSC-EVs alone or loaded on scaffolds in particular collagen-based scaffolds.
Highlights
The pathological process of SCI being very complex.
A complete effective strategy has yet to be found for treatment of SCI in human.
Exosomes derived-stem cells alone have great potential for the treatment of SCI.
Various biocompatible scaffolds are good drug carriers for SCI treatment.
Various biocompatible scaffolds are good carriers for exosomes.
Plain Language Summary
Human with spinal cord injury (SCI) show serious motor and sensory disability of the limbs. Since there is no an effective treatment for SCI, researchers are trying to develop and find a new therapeutic approach for SCI. CNS tissue engineering with various stem cells sources as well as their derived extracellular vesicle has been extensively attracted for providing reliable and safe approach for SCI treatment. Extracellular vesicles are lipid bilayer membrane-enclosed organelles containing various biomolecules involved in a variety of complex intercellular communication systems. They are released from all cell types into their surrounding environment and are important vehicles for paracrine The application of stem cells-derived extracellular vesicles (MSC-EVs) has recently attracted attention to improve central nervous system dysfunction such as SCI, mainly by promoting neurogenesis and angiogenesis.
Keywords: Spinal cord injury (SCI), Exosomes, Stem cells, Tissue engineering
1. Introduction
Central nervous system (CNS) disorders, especially spinal cord injury (SCI), remain among the most challenging pathologies with no or limited therapeutic strategies ( Ebrahimi-Barough et al., 2015). This traumatic disorder is characterized by serious motor and sensory disabilities of the limbs below the injured segment leading to physical and psychological harm to patients as well as a dramatic loss of life quality ( Liu et al., 2021). Despite the current treatments, such as hemodynamic therapy, surgical decompression, corticosteroids, and invasive spinal cord pressure monitoring, the function of the injured spinal cord has not been completely restored, and it is urgent to find a new method to treat SCI ( Hawryluk et al., 2015; Fehlings et al., 2012; Kwon et al., 2009; Ryken et al., 2013; Squair et al., 2017; Streijger et al., 2018; Wutte et al., 2019; Yang et al., 2019). Regenerative medicine is an interdisciplinary field developing and applying tissue engineering, SC therapy, and stem cells-derived extracellular vesicles therapy to provide reliable and safe ways to replace injured tissues and organs ( Shirian et al., 2016; Norouzi-Barough et al., 2020; Norouzi-Barough et al., 2021), it subsequently results in restoring the cellular function that is lost due to several conditions, such as SCI ( Liu et al., 2021; Wutte et al., 2019).
The sources of transplanted cells, including adult SCs, induced pluripotent SCs, and embryonic SCs, are considered the main factors involved in regenerative medicine. Mesenchymal stem cells (MSCs) are isolated easily from various tissues, including, amniotic fluid and membrane, Wharton’s jelly, adipose tissue, dental tissues, endometrium, limb bud, placenta, menstrual blood, peripheral blood, bone marrow, salivary gland, fetal membrane, synovial fluid foreskin, and sub-amniotic umbilical cord lining membrane ( Ullah et al., 2015; Najafi et al., 2020). MSCs have low immunogenicity and immunoregulatory properties; therefore they have been widely used as promising transplanted cells for a broad range of defects and diseases, approximately 1000 clinical trials, by regenerative medicine approaches (Ross et al., 2018, Five Decades Later, 2020), such as the regeneration of the damaged neuronal cells ( Guy & Offen, 2020).
Despite the advantages of differentiation of MSCs to the neuronal cells with neuron-like functions as well as immuno-modulating properties, some limitations were addressed for their implantation. The therapeutic effects of MSCs have not depended on the physical existence of the transplanted cells within the damaged sites of tissues ( Guy & Offen, 2020; Eleuteri et al., 2019). In addition, a few fractions of the transplanted MSCs are localized to the injured tissues and site ( Guy & Offen, 2020). To overcome these limitations, several extracellular vesicles and intercellular communication have been recently introduced ( Liu et al., 2019). Therefore in this review study, the current data regarding the efficacy of the existing MSC-derived EVs in targeting inflammatory and non-inflammatory processes to improve the therapeutic outcomes in experimental models of SCI are summarized.
Underlying mechanisms involving in the pathophysiology of spinal cord injury (SCI)
Primary and secondary injuries are two consecutive processes involved in the pathology of SCI. Primary injury is an irreversible process, defined as a mechanical injury to the spinal cord ( Kumar et al., 2017). Mechanical injuries result in the rupture and destruction of the axonal membranes and the release of a variety of powerful axonal regeneration inhibitors decomposition products from the myelin sheath, such as myelin-associated glycoprotein, as neurite outgrowth inhibitor protein A, and chondroitin sulfate proteoglycan oligodendrocyte myelin glycoprotein ( Fournier et al., 2001; GrandPré et al., 2000; Beller & Snow, 2014). The secondary progressive injury has a delayed onset and is more complicated than the primary injury ( Ulndreaj et al., 2016, Javdani et al., 2019).
Scarring and inflammatory responses to spinal cord injury (SCI)
Inflammatory responses and scarring associated with SCI include a wide variety of cells and cellular activities, which vary based on timing, injury type, and spatial distribution ( Orr & Gensel, 2018). The destruction of the blood-spinal cord barrier leads to the release of inflammatory cytokines by inflammatory cells ( Ulndreaj et al., 2016). Secondary inflammation-induced injury after SCI includes electrolyte abnormalities and the release of excitatory amino acids and reactive oxygen species (ROS) that, in turn, lead to edema, ischemia, apoptosis, and cell necrosis at the injured site ( Liu et al., 2021). However, secondary injury responses by microglia, strocytes, endothelial cells, pericytes, Schwann cells, meningeal cells, fibroblasts, and other glial cells not only potentiate SCI damage but also facilitate endogenous repair ( Orr & Gensel, 2018).
Extracellular vesicles (EVs)
EVs are lipid bilayer membrane-enclosed organelles containing various biomolecules involved in a variety of complex intercellular communication systems. They are released from all cell types into their surrounding environment and are important vehicles for paracrine delivery of therapeutic agents ( Veziroglu & Mias, 2020).
They are classified into three main subtypes, including shedding microvesicles (MVs), exosomes (Exos), and apoptotic bodies (ABs) that are mainly differentiated and classified by their size, biogenesis pathway, cargo, and markers ( Norouzi-Barough et al., 2020; Norouzi-Barough et al., 2021).
Moreover, based on the latest guidelines (MISEV2018), the following criteria are recommended for the classification of EVs, biochemical makeup (CD63+/CD81/+-EVs, Annexin A5-stained EVs, etc.), physical properties of EVs, including density (low, middle, high, with each range defined) and size (“small EVs” (sEVs, 50 to 200 nm) and “medium/large EVs” (m/lEVs, more than 200 nm), definition of conditions or cell of origin (hypoxic EVs, podocyte EVs, and large oncosomes) ( Théry et al., 2018).
Among all EVs, only MVs and Exos (50–1000 nm) mimic the biological activity of parent cells and horizontally transfer the biomolecules, such as ribonucleic acid (RNA) fragments (ribosomal (r)RNA, long non-coding (lnc)RNAs, messenger (m)RNAs, transfer (t)RNA, piwi-interacting (pi)RNAs, micro (mi)RNAs, RNAs and Y-vault RNAs,) ( Sadovska et al., 2015), DNA (genomic DNA, mtDNA) (Williams et al., 2014), lipids, and proteins, to the local microenvironment and target cells, and subsequently mediate tissue regeneration through various mechanisms ( Roefs et al., 2020). Therefore, EVs have been explored to act as potential therapeutic agents in a wide range of neuronal diseases associated with inflammatory responses and neuronal apoptosis, such as SCI.
Neural stem cells (NSCs) and NSCs-derived small extracellular vesicles (NSC-sEV) in spinal cord injury (SCI)
NSCs have been reported to have the ability to self-renew and differentiate into astrocytes, oligodendrocytes, and neurons ( Tang et al., 2017). The unique neuroprotective function post-NSC transplantation has been widely studied to promote functional recovery after acute SCI ( Cheng et al., 2016; Kokaia & Lindvall, 2018). NSC transplantation mediates the promotion of regeneration, neurogenesis, plasticity and suppresses neuroinflammation ( Cheng et al., 2016; Kokaia & Lindvall, 2018). However, the low survival rate owing to ischemia and immune rejection has been addressed through the clinical application of direct NSC for the treatment of SCI ( Rong et al., 2019). Therefore, to overcome these limitations, NSC-sEVs have been recently reported to regenerate the SCI ( Rong et al., 2019).
NSC-sEV treatment has been reported to potentially inhibit neuroinflammation, attenuate neuronal apoptosis, reduce microglia activation, and experimentally promote functional recovery at an early stage of SCI by promoting autophagy ( Rong et al., 2019). Rong et al reported that NSC-sEV therapy of SCI rat model inhibits neuro-inflammation and reduces neuronal apoptosis depending on autophagy induction. sEVs produced by NSCs also showed therapeutic efficacy against inflammatory, ischemic, and neurodegenerative diseases ( Stevanato et al., 2016). The anti-inflammatory effect of NSC-sEVs also contributes to down-regulate the NO production by activated microglia involved in inflammation following traumatic SCI. The expression levels of pro-inflammatory cytokines are considerably suppressed in SCI pre-treated with NSC-sEVs ( Rong et al., 2019).
Mesenchymal stem cells (MSC)-derived exosomes
Exosomes are mostly secreted by MSCs ( Yu et al., 2014). The tetraspanins as the common exosomal surface markers (CD9, CD63, and CD81) are expressed by MSC-Derived Exosomes. MSC-derived exosomes also express ALG-2 interacting protein X, heat shock proteins (HSP)-60, HSP-70, and HSP-90, adhesion molecules (CD73, CD44, and CD29), and tumor susceptibility gene 101 ( Colombo et al., 2014). They also carry various biomolecules, such as lipids, nucleic acids (microRNAs [miRNAs]), and proteins (Zaharie et al., 2014). Several MSCs-derived exosomes have been reported to have potential promoters for functional recovery (FR) and their contents can serve as biomarkers in SCI ( Liu et al., 2021) that have been summarized in this study.
Exosomes derived from pericytes (P-sEVs)
Pericytes are contractile cells that encircle endothelial cells ( Simonavicius et al., 2012). Pericytes are crucial compounds of the astrocytes, endothelial cells (ECs) in the neurovascular unit, and neurons ( Dore-Duffy & Cleary, 2011). They take part in the control of integrity and permeability of microvascular, pressure of microcirculation, participation in angiogenesis, and regulation of ECs differentiation by paracrine signaling and direct physical contact ( Orekhov et al., 2014). ECs can take up exosomes of pericytes due to the special relationship between endothelial cells and pericytes that play a role in the mediation of ECs function. P-sEVs reduce pathological changes and improve blood flow, motor function, and oxygen deficiency after SCI. P-sEVs improve the endothelial ability to protect the blood-spinal cord barrier, regulate blood flow, and decrease edema. The down-regulated expression of Bax, matrix metalloproteinase 2 (MMP2), hypoxia-inducible factor 1 alpha (HIF-1α), and, aquaporin-4, as well as the up-regulated expression of bcl-2 claudin-5 by P-sEVs led to inhibit apoptosis ( Yuan et al., 2019). Therefore, they have been suggested to have therapeutic prospects for apoptosis and regulating microcirculation after SCI ( Yuan et al., 2019).
Exosomes derived from human placenta (hP-sEVs)
MSCs derived from the human placenta have low immunogenicity and their effectiveness is attributed to the secretion of factors. hP-sEVs have been shown to improve neurologic function in mice SCI models. hP-sEVs have proangiogenic effects on endothelial cells leading to promote angiogenesis in mice SCI model after injury ( Zhang et al., 2020).
Exosomes derived from bone marrow (BM-sEVs)
Mesenchymal stem cells (MSCs)
Astrocytes play a crucial role in the process of SCI, since they can inhibit or promote central nervous system (CNS) recovery. A1 astrocytes, rapidly induced by neuroinflammation, are formed after SCI. The inhabitation of their neurotoxic effects on synapses, myelin, and neurons may be a promising strategy for the treatment of SCI ( Liddelow et al., 2017). Following SCI, BM-MSC, and BM-sEVs reduce SCI-induced A1 astrocytes via down-regulation of phosphorylated nuclear factor kappa-light-chain-enhancer of activated B cells (NFκB) p65. They exert anti-inflammatory and neuroprotective effects with therapeutic effects when injected intravenously ( Wang et al., 2018). Not only is the secondary injury induced by inflammation in SCI regulated by the NF-κB pathway ( Conti et al., 2003), but it is also extensively activated by a variety of pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α) and interleukin-1 (IL-1) as well as reactive oxygen species (ROS) ( Kaltschmidt & Kaltschmidt, 2009). So inhibition of the NF-κB signaling pathway can promote FR after SCI ( Wang et al., 2018).
Autophagy is critical for the protection against SCI and BM-sEVs have been shown to attenuate neuronal apoptosis by promoting autophagy in vitro and after SCI and improve functional behavior and recovery of motor function in SCI rat model ( Guo et al., 2019).
Human umbilical cord-derived exosomes (hUC-sEVs)
The modulation of inflammation is obtained after the injection of hUC-MSCs and hUC-EVs in rat SCI model, which may be contributed to their potential to reach the injured spinal cord tissue and directly interact with microglia.
The capability of hUC-EVs to interact with rat microglia has been addressed in vitro using microglia cultures. Since hUC-EVs have been shown to reduce the induction of expression levels of IL-1β and IL-6 in rat microglia cultures in response to LPS, they may directly interact with the activated microglia at their early activation and modify the cytokine expression profile toward a milder pro-inflammatory response and inhibit the mRNA expression level of pro-inflammatory cytokines during secondary injury in a SCI ( Romanelli et al., 2019). The hUC-EVs also contribute to the recovery of motor function by inhibiting scar formation ( Romanelli et al., 2019). It has been suggested that hUC-sEVs can improve the activity of aged MSCs and enhance their function by down-regulating apoptotic protease activating factor 1 (Apaf1) having a pro-apoptotic activity ( Zhang et al., 2020).
Human endometrial-derived exosomes (hE-sEVs)
The endometrium has been recently introduced as an available source of MSCs that can be isolated without anesthesia and adverse effects ( Ebrahimi-Barough et al., 2015). However, the therapeutic potential of human endometrial MSCs as well as the biological role of hEsEVs has been previously established; the effectiveness of hE-sEVs for treating SCI is still known. However, hE-sEVs have been shown to increase the proliferation, migration, and angiogenesis of HUVECs in in vitro ( Taghdiri Nooshabadi et al., 2019).
Epidural fat-mesenchymal stem cells derived exosomes (EF-sEVs)
Intravenous injection of EF-sEVs has been shown to inhibit NLRP3 inflammasome activation and reduced the expression of inflammatory cytokines ( Huang et al., 2020). In addition, systemic administration of EF-sEVs in SCI rat model results in up and down-regulated expression levels of antiapoptotic B-cell lymphoma 2 (Bcl-2) and proapoptotic protein Bax, respectively ( Huang et al., 2020).
Exsosme loaded on scaffolds
In contrast to the local implantation of MSC-sEVs, which is a promising therapeutic strategy, the efficacy of exosomes has been reported to be limited by the poor presence at the lesion site of the spinal cord when injected systematically ( Li et al., 2020). Therefore an effective delivery strategy using a three-dimensional biocompatible scaffold has been demonstrated to achieve the efficient retention, effective delivery, release, and integration of exosomes in the injured spinal cord ( Li et al., 2020). A variety of materials are capable to carry the transplanted cells for treating SCI. However, based on our knowledge, biocompatible 3D scaffolds for adhesive sEVs delivery remains poorly investigated. Li et al. (2020) have recently shown the local delivery of hP-sEVs by using an adhesive hyaluronic acid (HA) hydrogel.
2. Discussion
Individuals with SCI usually suffer from permanent neurological and non-neurological disorders and deficits, while therapeutic efficacies are limited ( Bourassa-Moreau et al., 2013). At present, no clinical trials of MSC-sEVs have been conducted to regenerate the SCI. However, stem cell therapy as well as exosome-derived stem cells isolated from different sources seems to be an attractive option for treating SCI. An injured spinal cord is poorly regenerated due to insufficient repair of endogenous cells, the weakened ability of axonal growth, and the presence of inhibitory molecules at the injured site ( Wu et al., 2015; He & Jin, 2016; Jure et al., 2017). Overcoming these obstacles leads to finding an ideal strategy for the treatment of SCI.
To date, the therapeutic efficacy of the exosomes derived from stem cells for treating an injured spinal cord tissue has been mainly demonstrated by several mechanisms, including anti-inflammatory effects, regulation of inflammation, angiogenesis promotion, and axon formation, maintenance of the integrity of the blood–spinal cord barrier, and inhibition of apoptosis ( Kumar et al., 2017; Ren et al., 2020; Rong et al., 2019; Zhang et al., 2020). The exosomes increase A2 astrocytes playing a neuroprotective role by up-regulating the expression of neurotrophic factors. In contrast, they decrease the A1 astrocytes that are rapidly formed post-SCI and have neurotoxic effects. The exsosome reduces the A1 astrocytes by inhibiting the nuclear translocation of NF-κB p65 ( Wang et al., 2018).
It has been shown that the exosomes can be used as valuable carriers for targeting miRNAs (miRNA-21, miRNA, 29, miRNA-133b, miRNA-126, miRNA-216) at the SCI site. The miRNA-29, miRNA133b, and miRNA126 promote axonal regeneration. The miRNA-216 and miRNA-21 promote microgelia polarization and reduce neuronal apoptosis, respectively ( Ren et al., 2020, Huang et al., 2020). miRNAs play a crucial role in the recovery of motor function, reducing neuronal axonal regeneration, mediating inflammation, neuronal differentiation, growth, and apoptosis ( Huang et al., 2020).
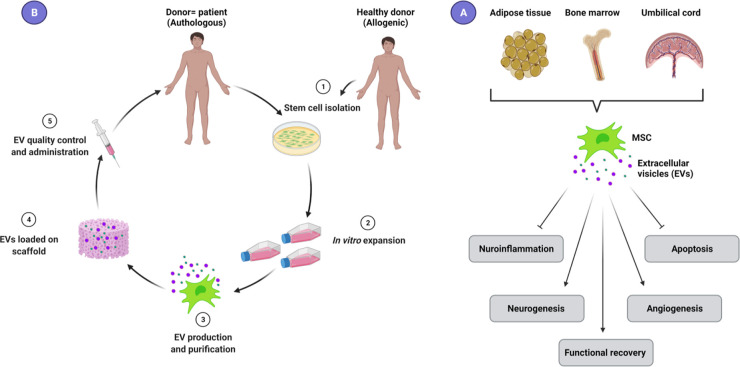
The anti-inflammatory effects of exosomes are attributed to multiple effects of the exosomes. They directly interact with the activated and polarized microglia and down-regulate the mRNA expression level of pro-inflammatory cytokines, such as IL-1β and IL-6 during secondary injury ( Romanelli et al., 2019). The nucleotide-binding domain-like receptor protein 3 (NLRP3) inflammasome is a crucial protein complex-inflammasome that activates the resident immune cells leading to neuro-inflammation and secondary injury of SCI ( Zhou et al., 2016). It has been shown that the activity of the NLRP3 inflammasome is increased in SCI models ( Zhou et al., 2016). Functional recovery occurred by inhibiting the activation of the NLRP3 inflammasome in a rat model of SCI ( Jiang et al., 2017). Intravenous injection of EF-sEVs inhibits the activation of NLRP3 inflammasomes and reduces inflammation. Sun et al. (2018) found that hU-sEVs increase the levels of the anti-inflammatory cytokines IL-4 and IL-10 and reduce the levels of the pro-inflammatory cytokines IL-6, TNF-α, interferon-γ, and granulocyte colony-stimulating factor. Figure 1 shows the EVs sources and their action mechanisms.
Figure 1.
Most common sources of mesenchymal stem cells (MSCs), bone marrow, adipose tissue, and umbilical cord
A) Extracellular vesicles (EVs), including exosomes and microvesicles are released from different cell types, including MSCs, and mediate the beneficial effects of MSCs on target cells. MSC-EVs reduce neuroinflammation by inhibiting the activation of astrocytes and microglia and switching to an anti-inflammatory phase. They also attenuate neuronal apoptosis, and promote angiogenesis, neurogenesis, and functional recovery in SCI patients.
B) EVs can be derived from the patient’s MSCs (authologous) or from healthy donors (allogenic) and then expand in vitro. In the next step, EVs are extracted and purified by various protocols based on different protein markers, sizes, and density of EVs. Isolated EVs following quality control can be administrated directly, or with biocompatible 3D scaffolds.
3. Conclusion
Although treating SCI has been extensively studied, no effective strategy has yet been found to restore lost function. The treatment of SCI remains a great challenge and hinders the development of treatments leading to a full recovery due to the pathological process of SCI being very complex. Exosomes derived from stem cells alone or loaded on various biocompatible scaffolds, such as collagen hydrogel or other ECM-based scaffolds can be considered good drug carriers that have great potential for the treatment of SCI.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
All authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Tehran University of Medical Sciences.
References
- Ebrahimi-Barough S., Norouzi Javidan A., Saberi H., Joghataei M. T., Rahbarghazi R., Mirzaei E., et al. (2015). Evaluation of motor neuron-like cell differentiation of hEnSCs on biodegradable PLGA nanofiber scaffolds. Molecular Neurobiology, 52(3), 1704–1713. [DOI: 10.1007/s12035-014-8931-2] [PMID https://www.ncbi.nlm.nih.gov/pubmed/25377792] [DOI] [PubMed] [Google Scholar]
- Liu W. Z., Ma Z. J., Li J. R., Kang X. W. (2021). Mesenchymal stem cell-derived exosomes: Therapeutic opportunities and challenges for spinal cord injury. Stem cell Research & Therapy, 12(1), 102. [DOI: 10.1186/s13287-021-02153-8] [PMID https://www.ncbi.nlm.nih.gov/pubmed/33536064] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wutte C., Klein B., Becker J., Mach O., Panzer S., Strowitzki M., et al. (2019). Earlier decompression (< 8 hours) results in better neurological and functional outcome after traumatic thoracolumbar spinal cord injury. Journal of Neurotrauma, 36(12), 2020–2027. [DOI: 10.1089/neu.2018.6146] [PMID https://www.ncbi.nlm.nih.gov/pubmed/30489193] [DOI] [PubMed] [Google Scholar]
- Yang M., Yin X., Liu S., Hui H., Yan L., He B., et al. (2019). Letter: Ultra-early (<12 hours) surgery correlates with higher rate of american spinal injury association impairment scale conversion after cervical spinal cord injury. Neurosurgery, 85(2), E399–E400. [DOI: 10.1093/neuros/nyz154] [PMID https://www.ncbi.nlm.nih.gov/pubmed/31173146] [DOI] [PubMed] [Google Scholar]
- Ryken T. C., Hurlbert R. J., Hadley M. N., Aarabi B., Dhall S. S., Gelb D. E., et al. (2013). The acute cardiopulmonary management of patients with cervical spinal cord injuries. Neurosurgery, 72(Suppl 2), 84–92. [DOI: 10.1227/NEU.0b013e318276ee16] [PMID https://www.ncbi.nlm.nih.gov/pubmed/23417181] [DOI] [PubMed] [Google Scholar]
- Hawryluk G., Whetstone W., Saigal R., Ferguson A., Talbott J., Bresnahan J., et al. (2015). Mean arterial blood pressure correlates with neurological recovery after human spinal cord injury: Analysis of high frequency physiologic data. Journal of Neurotrauma, 32(24), 1958–1967. [DOI: 10.1089/neu.2014.3778] [PMID https://www.ncbi.nlm.nih.gov/pubmed/25669633] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4677564/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streijger F., So K., Manouchehri N., Gheorghe A., Okon E. B., Chan R. M., et al. (2018). A direct comparison between norepinephrine and phenylephrine for augmenting spinal cord perfusion in a porcine model of spinal cord injury. Journal of Neuro-trauma, 35(12), 1345–1357. [DOI: 10.1089/neu.2017.5285] [PMID https://www.ncbi.nlm.nih.gov/pubmed/29338544] [DOI] [PubMed] [Google Scholar]
- Squair J. W., Bélanger L. M., Tsang A., Ritchie L., Mac-Thiong J. M., Parent S., et al. (2017). Spinal cord perfusion pressure predicts neurologic recovery in acute spinal cord injury. Neurology, 89(16), 1660–1667. [DOI: 10.1212/WNL.0000000000004519] [PMID https://www.ncbi.nlm.nih.gov/pubmed/28916535] [DOI] [PubMed] [Google Scholar]
- Fehlings M. G., Vaccaro A., Wilson J. R., Singh A., W Cadotte D., Harrop J. S., et al. (2012). Early versus delayed decompression for traumatic cervical spinal cord injury: Results of the surgical timing in acute spinal cord injury study (STASCIS). Plos One, 7(2), e32037. [DOI: 10.1371/journal.pone.0032037] [PMID https://www.ncbi.nlm.nih.gov/pubmed/22384132] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3285644/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon B. K., Curt A., Belanger L. M., Bernardo A., Chan D., Markez J. A., et al. (2009). Intrathecal pressure monitoring and cerebrospinal fluid drainage in acute spinal cord injury: A prospective randomized trial. Journal of Neurosurgery, 10(3), 181–193. [DOI: 10.3171/2008.10.SPINE08217] [PMID https://www.ncbi.nlm.nih.gov/pubmed/19320576] [DOI] [PubMed] [Google Scholar]
- Norouzi-Barough L., Asgari Khosro Shahi A., Mohebzadeh F., Masoumi L., Haddadi M. R., Shirian S. (2020). Early diagnosis of breast and ovarian cancers by body fluids circulating tumor-derived exosomes. Cancer Cell International, 20, 187. [DOI: 10.1186/s12935-020-01276-x] [PMID https://www.ncbi.nlm.nih.gov/pubmed/32489323] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7247259/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norouzi-Barough L., Shirian S., Gorji A., Sadeghi M. (2022). Therapeutic potential of mesenchymal stem cell-derived exosomes as a cell-free therapy approach for the treatment of skin, bone, and cartilage defects. Connective Tissue Research, 63(2), 83–96. [DOI: 10.1080/03008207.2021.1887855] [PMID https://www.ncbi.nlm.nih.gov/pubmed/33563070] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7247259/] [DOI] [PubMed] [Google Scholar]
- Shirian S., Ebrahimi-Barough S., Saberi H., Norouzi-Javidan A., Mousavi S. M., Derakhshan M. A., et al. (2016). Comparison of capability of human bone marrow mesenchymal stem cells and endometrial stem cells to differentiate into motor neurons on electrospun poly(ε-caprolactone) scaffold. Molecular Neurobiology, 53(8), 5278–5287. [DOI: 10.1007/s12035-015-9442-5] [PMID https://www.ncbi.nlm.nih.gov/pubmed/26420037] [DOI] [PubMed] [Google Scholar]
- Ullah I., Subbarao R. B., Rho G. J. (2015). Human mesenchymal stem cells - current trends and future prospective. Bioscience Reports, 35(2), e00191. [DOI: 10.1042/BSR20150025] [PMID https://www.ncbi.nlm.nih.gov/pubmed/25797907] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4413017/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najafi S., Nosrati H., Faraji Z., Mohamadnia A., Shirian S., Mortazavi S. M., et al. (2020). Reconstruction of necrotic submandibular salivary gland using mesenchymal stem cells. Heliyon, 6(10), e05162. [DOI: 10.1016/j.heliyon.2020.e05162] [PMID https://www.ncbi.nlm.nih.gov/pubmed/33083616] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7551326/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimmons R. E. B., Mazurek M. S., Soos A., Simmons C. A. (2018). Mesenchymal stromal/stem cells in regenerative medicine and tissue engineering. Stem Cells International, 2018, 8031718. [DOI: 10.1155/2018/8031718] [PMID https://www.ncbi.nlm.nih.gov/pubmed/30210552] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6120267/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez-Salazar M., Gonzalez-Galofre Z. N., Casamitjana J., Crisan M., James A. W., Péault B. (2020). Five decades later, are mesenchymal stem cells still relevant? Frontiers in Bioengineering and Biotechnology, 8, 148. [DOI: 10.3389/fbioe.2020.00148] [PMID https://www.ncbi.nlm.nih.gov/pubmed/32185170] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7058632/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy R., Offen D. (2020). Promising opportunities for treating neurodegenerative diseases with mesenchymal stem cell-derived exosomes. Biomolecules, 10(9), 1320. [DOI: 10.3390/biom10091320] [PMID https://www.ncbi.nlm.nih.gov/pubmed/32942544] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7564210/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eleuteri S., Fierabracci A. (2019). Insights into the secretome of mesenchymal stem cells and its potential applications. International Journal of Molecular Sciences, 20(18), 4597. [DOI: 10.3390/ijms20184597] [PMID https://www.ncbi.nlm.nih.gov/pubmed/31533317] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6770239/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Bai X., Zhang A., Huang J., Xu S., Zhang J. (2019). Role of exosomes in central nervous system diseases. Frontiers in Molecular Neuroscience, 12, 240. [DOI: 10.3389/fnmol.2019.00240] [PMID https://www.ncbi.nlm.nih.gov/pubmed/31636538] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6787718/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar H., Ropper A. E., Lee S. H., Han I. (2017). Propitious therapeutic modulators to prevent blood-spinal cord barrier disruption in spinal cord injury. Molecular Neurobiology, 54(5), 3578–3590. [DOI: 10.1007/s12035-016-9910-6] [PMID https://www.ncbi.nlm.nih.gov/pubmed/27194298] [DOI] [PubMed] [Google Scholar]
- Fournier A. E., GrandPre T., Strittmatter S. M. (2001). Identification of a receptor mediating Nogo-66 inhibition of axonal regeneration. Nature, 409(6818), 341–346. [DOI: 10.1038/35053072] [PMID https://www.ncbi.nlm.nih.gov/pubmed/11201742] [DOI] [PubMed] [Google Scholar]
- GrandPré T., Nakamura F., Vartanian T., Strittmatter S. M. (2000). Identification of the nogo inhibitor of axon regeneration as a reticulon protein. Nature, 403(6768), 439–444. [DOI: 10.1038/35000226] [PMID https://www.ncbi.nlm.nih.gov/pubmed/10667797] [DOI] [PubMed] [Google Scholar]
- Beller J. A., Snow D. M. (2014). Proteoglycans: Road signs for neurite outgrowth. Neural Regeneration Research, 9(4), 343–355. [DOI: 10.4103/1673-5374.128235] [PMID https://www.ncbi.nlm.nih.gov/pubmed/25206822] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4146197/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulndreaj A., Chio J. C., Ahuja C. S., Fehlings M. G. (2016). Modulating the immune response in spinal cord injury. Expert Review of Neurotherapeutics, 16(10), 1127–1129. [DOI: 10.1080/14737175.2016.1207532] [PMID https://www.ncbi.nlm.nih.gov/pubmed/27352883] [DOI] [PubMed] [Google Scholar]
- Javdani M., Habibi A., Shirian S., Kojouri G. A., Hosseini F. (2019). Effect of selenium nanoparticle supplementation on tissue inflammation, blood cell count, and IGF-1 levels in spinal cord injury-induced rats. Biological Trace Element Research, 187(1), 202–211. [DOI: 10.1007/s12011-018-1371-5] [PMID https://www.ncbi.nlm.nih.gov/pubmed/29730750] [DOI] [PubMed] [Google Scholar]
- Orr M. B., Gensel J. C. (2018). Spinal cord injury scarring and inflammation: Therapies targeting glial and inflammatory responses. Neurotherapeutics, 15(3), 541–553. [DOI: 10.1007/s13311-018-0631-6] [PMID https://www.ncbi.nlm.nih.gov/pubmed/29717413] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6095779/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veziroglu E. M., Mias G. I. (2020). Characterizing extracellular vesicles and their diverse RNA contents. Frontiers in Genetics, 11, 700. [DOI: 10.3389/fgene.2020.00700] [PMID https://www.ncbi.nlm.nih.gov/pubmed/32765582] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7379748/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Théry C., Witwer K. W., Aikawa E., Alcaraz M. J., Anderson J. D., Andriantsitohaina R., et al. (2018). Minimal information for studies of extracellular vesicles 2018 (MISEV2018): A position statement of the international society for extracellular vesicles and update of the MISEV2014 guidelines. Journal of Extracellular Vesicles, 7(1), 1535750. [DOI: 10.1080/20013078.2018.1461450] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadovska L., Eglitis J., Line A. (2015). Extracellular vesicles as biomarkers and therapeutic targets in breast cancer. Anticancer Research, 35(12), 6379–6390. [Link https://ar.iiarjournals.org/content/35/12/6379.short] [PubMed] [Google Scholar]
- Thakur B. K., Zhang H., Becker A., Matei I., Huang Y., Costa-Silva B., et al. (2014). Double-stranded DNA in exosomes: A novel biomarker in cancer detection. Cell Research, 24(6), 766–769. [DOI: 10.1038/cr.2014.44] [PMID https://www.ncbi.nlm.nih.gov/pubmed/24710597] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4042169/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roefs M. T., Sluijter J. P. G., Vader P. (2020). Extracellular vesicle-associated proteins in tissue repair. Trends in Cell Biology, 30(12), 990–1013. [DOI: 10.1016/j.tcb.2020.09.009] [PMID https://www.ncbi.nlm.nih.gov/pubmed/33069512] [DOI] [PubMed] [Google Scholar]
- Tang Y., Yu P., Cheng L. (2017). Current progress in the derivation and therapeutic application of neural stem cells. Cell death & Disease, 8(10), e3108. [DOI: 10.1038/cddis.2017.504] [PMID https://www.ncbi.nlm.nih.gov/pubmed/33069512] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5682670/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Z., Zhu W., Cao K., Wu F., Li J., Wang G., et al. (2016). Anti-inflammatory mechanism of neural stem cell transplantation in spinal cord injury. International Journal of Molecular Sciences, 17(9), 1380. [DOI: 10.3390/ijms17091380] [PMID https://www.ncbi.nlm.nih.gov/pubmed/27563878] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5037660/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokaia Z., Lindvall O. (2018). Sensors of succinate: Neural stem cell grafts fight neuroinflammation. Cell Stem Cell, 22(3), 283–285. [DOI: 10.1016/j.stem.2018.01.019] [PMID https://www.ncbi.nlm.nih.gov/pubmed/29499143] [DOI] [PubMed] [Google Scholar]
- Rong Y., Liu W., Wang J., Fan J., Luo Y., Li L., et al. (2019). Neural stem cell-derived small extracellular vesicles attenuate apoptosis and neuroinflammation after traumatic spinal cord injury by activating autophagy. Cell Death & Disease, 10(5), 340. [DOI: 10.1038/s41419-019-1571-8] [PMID https://www.ncbi.nlm.nih.gov/pubmed/31000697] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6472377/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevanato L., Thanabalasundaram L., Vysokov N., Sinden J. D. (2016). Investigation of content, stoichiometry and transfer of miRNA from human neural stem cell line derived exosomes. Plos One, 11(1), e0146353. [DOI: 10.1371/journal.pone.0146353] [PMID https://www.ncbi.nlm.nih.gov/pubmed/26752061] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4713432/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu B., Zhang X., Li X. (2014). Exosomes derived from mesenchymal stem cells. International Journal of Molecular Sciences, 15(3), 4142–4157. [DOI: 10.3390/ijms15034142] [PMID https://www.ncbi.nlm.nih.gov/pubmed/24608926] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3975389/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo M., Raposo G., Théry C. (2014). Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annual Review of Cell and Developmental Biology, 30, 255–289. [DOI: 10.1146/annurev-cell-bio-101512-122326] [PMID https://www.ncbi.nlm.nih.gov/pubmed/25288114] [DOI] [PubMed] [Google Scholar]
- Zaharie F., Muresan M. S., Petrushev B., Berce C., Gafencu G. A., Selicean S., et al. (2015). Exosome-carried microRNA-375 Inhibits cell progression and dissemination via Bcl-2 blocking in colon cancer. Journal of Gastrointestinal and Liver Diseases, 24(4), 435–443. [DOI: 10.15403/jgld.2014.1121.244.375] [PMID https://www.ncbi.nlm.nih.gov/pubmed/26697569] [DOI] [PubMed] [Google Scholar]
- Simonavicius N., Ashenden M., van Weverwijk A., Lax S., Huso D. L., Buckley C. D., et al. (2012). Pericytes promote selective vessel regression to regulate vascular patterning. Blood, 120(7), 1516–1527. [DOI: 10.1182/blood-2011-01-332338] [PMID https://www.ncbi.nlm.nih.gov/pubmed/22740442] [DOI] [PubMed] [Google Scholar]
- Dore-Duffy P., Cleary K. (2011). Morphology and properties of pericytes. Methods in Molecular Biology, 686, 49–68. [DOI: 10.1007/978-1-60761-938-3_2] [PMID https://www.ncbi.nlm.nih.gov/pubmed/21082366] [DOI] [PubMed] [Google Scholar]
- Orekhov A. N., Bobryshev Y. V., Chistiakov D. A. (2014). The complexity of cell composition of the intima of large arteries: Focus on pericyte-like cells. Cardiovascular Research, 103(4), 438–451. [DOI: 10.1093/cvr/cvu168] [PMID https://www.ncbi.nlm.nih.gov/pubmed/25016615] [DOI] [PubMed] [Google Scholar]
- Yuan X., Wu Q., Wang P., Jing Y., Yao H., Tang Y., et al. (2019). Exosomes derived from pericytes improve microcirculation and protect blood-spinal cord barrier after spinal cord injury in mice. Frontiers in Neuroscience, 13, 319. [DOI: 10.3389/fnins.2019.00319] [PMID https://www.ncbi.nlm.nih.gov/pubmed/31040762] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6476953/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Zhang C., Xu Y., Li C., Cao Y., Li P. (2020). Exosomes derived from human placenta-derived mesenchymal stem cells improve neurologic function by promoting angiogenesis after spinal cord injury. Neuroscience Letters, 739, 135399. [DOI: 10.1016/j.neulet.2020.135399] [PMID https://www.ncbi.nlm.nih.gov/pubmed/32979457] [DOI] [PubMed] [Google Scholar]
- Liddelow S. A., Guttenplan K. A., Clarke L. E., Bennett F. C., Bohlen C. J., Schirmer L., et al. (2017). Neurotoxic reactive astrocytes are induced by activated microglia. Nature, 541(7638), 481–487. [DOI: 10.1038/nature21029] [PMID https://www.ncbi.nlm.nih.gov/pubmed/28099414] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Pei S., Han L., Guo B., Li Y., Duan R., et al. (2018). Mesenchymal stem cell-derived exosomes reduce A1 astrocytes via downregulation of phosphorylated NFκB P65 subunit in spinal cord injury. Cellular Physiology and Biochemistry, 50(4), 1535–1559. [DOI: 10.1159/000494652] [PMID https://www.ncbi.nlm.nih.gov/pubmed/30376671] [DOI] [PubMed] [Google Scholar]
- Conti A., Cardali S., Genovese T., Di Paola R., La Rosa G. (2003). Role of inflammation in the secondary injury following experimental spinal cord trauma. Journal of Neurosurgical Science, 47(2), 89–94. [Link https://www.proquest.com/openview/a7400b5ef5ca70b8dff20150a8cac598/1?pq-origsite=gscholar&cbl=49236] [PubMed] [Google Scholar]
- Kaltschmidt B., Kaltschmidt C. (2009). NF-kappaB in the nervous system. Cold Spring Harbor Perspectives in Biology, 1(3), a001271. [DOI: 10.1101/cshperspect.a001271] [PMID https://www.ncbi.nlm.nih.gov/pubmed/20066105] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2773634/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo S., Perets N., Betzer O., Ben-Shaul S., Sheinin A., Michaelevski I., et al. (2019). Intranasal delivery of mesenchymal stem cell derived exosomes loaded with phosphatase and tensin homolog siRNA repairs complete spinal cord injury. ACS nano, 13(9), 10015–10028. [DOI: 10.1021/acsnano.9b01892] [PMID https://www.ncbi.nlm.nih.gov/pubmed/31454225] [DOI] [PubMed] [Google Scholar]
- Romanelli P., Bieler L., Scharler C., Pachler K., Kreutzer C., Zaunmair P., et al. (2019). Extracellular vesicles can deliver anti-inflammatory and anti-scarring activities of mesenchymal stromal cells after spinal cord injury. Frontiers in Neurology, 10, 1225. [DOI: 10.3389/fneur.2019.01225] [PMID https://www.ncbi.nlm.nih.gov/pubmed/31849808] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang N., Zhu J., Ma Q., Zhao Y., Wang Y., Hu X., et al. (2020). Exosomes derived from human umbilical cord MSCs rejuvenate aged MSCs and enhance their functions for myocardial repair. Stem Cell Research & Therapy, 11(1), 273. [DOI: 10.1186/s13287-020-01782-9] [PMID https://www.ncbi.nlm.nih.gov/pubmed/32641103] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taghdiri Nooshabadi V., Verdi J., Ebrahimi-Barough S., Mowla J., Atlasi M. A., Mazoochi T., et al. (2019). Endometrial mesenchymal stem cell-derived exosome promote endothelial cell angiogenesis in a dose dependent manner: A new perspective on regenerative medicine and cell-free therapy. Archives of Neuroscience, 6(4), e94041. [DOI: 10.5812/ans.94041] [DOI] [Google Scholar]
- Huang J. H., Fu C. H., Xu Y., Yin X. M., Cao Y., Lin F. Y. (2020). Extracellular vesicles derived from epidural fat-mesenchymal stem cells attenuate NLRP3 inflammasome activation and improve functional recovery after spinal cord injury. Neurochemical Research, 45(4), 760–771. [DOI: 10.1007/s11064-019-02950-x] [PMID https://www.ncbi.nlm.nih.gov/pubmed/31953741] [DOI] [PubMed] [Google Scholar]
- Li L., Zhang Y., Mu J., Chen J., Zhang C., Cao H., et al. (2020). Transplantation of human mesenchymal stem-cell-derived exosomes immobilized in an adhesive hydrogel for effective treatment of spinal cord injury. Nano Letters, 20(6), 4298–4305. [DOI: 10.1021/acs.nanolett.0c00929] [PMID https://www.ncbi.nlm.nih.gov/pubmed/32379461] [DOI] [PubMed] [Google Scholar]
- Bourassa-Moreau E., Mac-Thiong J. M., Feldman D. E., Thompson C., Parent S. (2013). Non-neurological outcomes after complete traumatic spinal cord injury: The impact of surgical timing. Journal of Neurotrauma, 30(18), 1596–1601. [DOI: 10.1089/neu.2013.2957] [PMID https://www.ncbi.nlm.nih.gov/pubmed/23829420] [DOI] [PubMed] [Google Scholar]
- Wu D., Klaw M. C., Connors T., Kholodilov N., Burke R. E., Tom V. J. (2015). Expressing constitutively active rheb in adult neurons after a complete spinal cord injury enhances axonal regeneration beyond a chondroitinase-treated glial scar. The Journal of Neuroscience, 35(31), 11068–11080. [DOI: 10.1523/JNEUROSCI.0719-15.2015] [PMID https://www.ncbi.nlm.nih.gov/pubmed/26245968] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4524976/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Z., Jin Y. (2016). Intrinsic control of axon regeneration. Neuron, 90(3), 437–451. [DOI: 10.1016/j.neuron.2016.04.022] [PMID https://www.ncbi.nlm.nih.gov/pubmed/27151637] [DOI] [PubMed] [Google Scholar]
- Jure I., Pietranera L., De Nicola A. F., Labombarda F. (2017). Spinal cord injury impairs neurogenesis and induces glial reactivity in the hippocampus. Neurochemical Research, 42(8), 2178–2190. [DOI: 10.1007/s11064-017-2225-9] [PMID https://www.ncbi.nlm.nih.gov/pubmed/28290135] [DOI] [PubMed] [Google Scholar]
- Ren Z., Qi Y., Sun S., Tao Y., Shi R. (2020). Mesenchymal stem cell-derived exosomes: Hope for spinal cord injury repair. Stem Cells and Development, 29(23), 1467–1478. [DOI: 10.1089/scd.2020.0133] [PMID https://www.ncbi.nlm.nih.gov/pubmed/33045910] [DOI] [PubMed] [Google Scholar]
- Huang J. H., Xu Y., Yin X. M., Lin F. Y. (2020). Exosomes derived from miR-126-modified MSCs promote angiogenesis and neurogenesis and attenuate apoptosis after spinal cord injury in rats. Neuroscience, 424, 133–145. [DOI: 10.1016/j.neuroscience.2019.10.043] [PMID https://www.ncbi.nlm.nih.gov/pubmed/31704348] [DOI] [PubMed] [Google Scholar]
- Ren Z. W., Zhou J. G., Xiong Z. K., Zhu F. Z., Guo X. D. (2019). Effect of exosomes derived from MiR-133b-modified ADSCs on the recovery of neurological function after SCI. European Review for Medical and Pharmacological Sciences, 23(1), 52–60. [Link https://www.europeanreview.org/wp/wp-content/uploads/52-60.pdf] [DOI] [PubMed] [Google Scholar]
- Zhou K., Shi L., Wang Y., Chen S., Zhang J. (2016). Recent advances of the NLRP3 inflammasome in central nervous system disorders. Journal of Immunology Research, 2016, 9238290. [DOI: 10.1155/2016/9238290] [PMID https://www.ncbi.nlm.nih.gov/pubmed/27652274] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5019917/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang W., Li M., He F., Zhou S., Zhu L. (2017). Targeting the NLRP3 inflammasome to attenuate spinal cord injury in mice. Journal of Neuroinflammation, 14(1), 207. [DOI: 10.1186/s12974-017-0980-9] [PMID https://www.ncbi.nlm.nih.gov/pubmed/29070054] [PMCID https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5657095/] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun G., Li G., Li D., Huang W., Zhang R., Zhang H., et al. (2018). hucMSC derived exosomes promote functional recovery in spinal cord injury mice via attenuating inflammation. Materials Science & Engineering, 89, 194–204. [DOI: 10.1016/j.msec.2018.04.006] [PMID https://www.ncbi.nlm.nih.gov/pubmed/29752089] [DOI] [PubMed] [Google Scholar]