Abstract
Background:
The aim of this study was to describe the epidemiology, physiopathology, and outcomes of elbow “unhappy triad” trauma in children, combining a posterior dislocation, a proximal radius fracture, and a third lesion (i.e. bony or capsuloligamentous injury).
Methods:
A retrospective bicentric study was conducted between 1999 and 2020. All skeletally immature children who presented to the emergency department and underwent surgery for a proximal radius injury were selected. Among this selection, only patients with two associated ipsilateral elbow injuries (i.e. posterior elbow dislocation and a bony and/or capsuloligamentous injury) were included. Active elbow ranges of motion, Mayo Elbow Performance Score and Quick-Disabilities Of The Arm, Shoulder And Hand scores and standard radiographs were recorded at last follow-up.
Results:
Twenty-one patients met the inclusion criteria (mean age at surgery = 11.4 years) among 737 selected. The “unhappy triad” diagnosis was made preoperatively in nine cases (bone lesion only), intraoperatively in nine cases, and postoperatively in one case. The third lesions were surgically treated when the lesion was a bony fracture or if the elbow remains unstable between 60° and 90° of flexion (i.e. capsuloligamentous injury). Twenty patients were reviewed (mean follow-up = 5.8 years). The complications and re-operations rates were of 10%.
Conclusion:
The “unhappy” triad of the child’s elbow is a rare injury, where the preoperative diagnosis is frequently missed and lead to 10% of complications and re-operations.
Level of evidence:
level III.
Keywords: Trauma elbow, triad elbow, pediatrics
Introduction
Elbow fractures account for approximately 7%–9% of upper limb fractures in children,1,2 occurring mostly between 9 and 11 years of age. 3 Skeletal immaturity is accountable for weakened enthesis areas, especially at the insertion zones of the capsule and ligaments onto the cartilage matrix. Most pediatric classifications of elbow fractures focus on bone displacement, and to the best of our knowledge, there is no diagnostic classification reporting on the occurrence of complex injuries that combine bony and capsuloligamentous lesions.4,5 In adult traumatology, the terrible triad of the elbow is a well-described injury, widely reported in the literature.6,7 Combining several bony and capsuloligamentous lesions, this triad is defined as the association of a posterior dislocation of the elbow, a radial head fracture, and a fracture of the coronoid process of the ulna. Is there an equivalent triad in pediatrics? Unlike adults, children’s elbows are more flexible, with strong ligaments and weak immature bones. Consequently, the description of this triad adult injury cannot be applied as is in children. In the literature, a few case reports8,9 and only one recent series 10 described a radial neck case fracture with an elbow dislocation and an osteochondral flap of the coronoid process.
In this series, we focused on the pediatric equivalent of the terrible triad that had been described in the adult elbow. We describe a triad, which we will call the “unhappy triad” in the immature elbow, that combines a fracture of proximal radius (i.e. radial neck and/or head) with a posterior dislocation of the joint and bony and/or capsuloligamentous injury of the anterior, medial or lateral aspect of the elbow. Therefore, the aim of our study was to describe the epidemiology and pathophysiology of complex elbow traumas in children called “unhappy triad” and report the functional and radiographic mid-term outcomes of patients presenting such lesions.
Materials and methods
Study population
A retrospective bicentric study was conducted between 1999 and 2020. A first review of medical records was performed by two surgeons, using an open-source data warehouse. 11 This screening included all skeletally immature children or adolescents who presented to the emergency department and underwent surgery for a proximal radius injury. Skeletally immaturity was defined on standard radiographs of the elbow by open physis at the epitrochlea, capitellum, radial head, and olecranon. Among this selection of patients, only cases presenting a complex elbow injury were included in the analysis, defined as the association of the proximal radius fracture, a posterior elbow dislocation, and a third lesion, including an injury of the medial or lateral and/or anterior compartment of the elbow. A second review of all included cases was conducted by two independent operators. Investigations were conducted according to the 1964 Declaration of Helsinki ethical standards. The study was registered in the national data protection authority (no. 2223801 v0), and the legal guardians of the patients were informed and consented to the study before any data collection and/or analysis.
Preoperative clinical and radiological assessments
Initial physical examination was performed in the emergency department to identify potential cutaneous, neurological, and/or vascular complications. All patients had preoperative and postoperative anterior–posterior (AP) and profile X-rays of the injured elbow. Patients who received an additional computed tomography (CT) scan were recorded. The proximal radius fracture was classified according to Chambers’ 12 classification. In cases of Salter–Harris types I and II lesions of the proximal radial physis (i.e. type I.A lesions according to Chambers), the radial head angulation was classified according to Judet’s classification. 13
Surgery and last follow-up outcomes
At last follow-up, patients were examined by one of the two observers, independent of the surgical procedure. Active elbow ranges of motion (ROM) in flexion/extension and pronosupination were recorded with goniometer. Mayo Elbow Performance Score (MEPS) 14 and Quick-Disabilities Of The Arm, Shoulder And Hand (DASH) 15 scores were reported. Standard antero-posterior and profile radiographs of the elbow and forearm were performed for all patients. Radiocapitellar dislocation was defined as a total loss of contact between both articular surfaces while subluxation was defined as a partial loss of contact of at least 50%. Cases of proximal radioulnar synostosis 16 and/or necrosis of the radial head were recorded.
Statistics
Results were presented as mean values ± standard deviation (range). Normality and heteroskedasticity of continuous data were assessed with Shapiro–Wilk and Levene’s tests, respectively. Continuous outcomes were compared with analysis of variance (ANOVA), Welch’s ANOVA, or Kruskal–Wallis tests, according to data distribution. Discrete outcomes were compared with chi-square or Fisher’s exact tests, accordingly. The alpha risk was set to 5%, and two-tailed tests were used. Statistical analysis was performed with EasyMedStat (version 3.19; www.easymedstat.com).
Results
Population
The medical records of 737 patients were initially selected. Among these files, only 21 patients (2.8%) met the inclusion criteria (Figure 1), including 13 girls and 8 boys, with a mean age at surgery of 11.4 ± 2.3 years (6.4–14.9). The initial trauma was a fall in 11 cases, from a height ranging from 1.5 to 7 m, a sports injury in 8 cases (i.e. in 6 cases while riding a horse and in 2 cases while playing basketball), and a motorbike accident in 2 cases. On initial examination, two patients presented with a sensory deficit, including one in the ulnar territory and one in the median and ulnar areas; no cutaneous and/or vascular complications were observed.
Figure 1.

Flow chart.
The patient lost to follow-up (Case 20) was described in the epidemiological results but withdrawn from the analysis at the last follow-up.
Assessment of triad injury
According to Chambers’ classification, 14 fractures of the radial proximal end were classified as type I.A lesions (i.e. Salter–Harris types I and II lesions), 4 fractures as type I.B lesions (i.e. Salter–Harris type IV lesions), and 3 fractures as a direct consequence of elbow dislocation (i.e. I.E lesions). Among the I.A group, 11 patients had an angulation of more than 60 degrees (i.e. grade-4 lesions according to Judet’s classification), while the remaining 3 patients had an angulation of 30–60 degrees (i.e. grade-3 lesions according to Judet’s classification). Regarding elbow dislocation, 12 patients presented with a posterolateral dislocation, 6 with a true posterior dislocation and 3 with a posteromedial dislocation.
Regarding the third lesion, 11 patients had a capsuloligamentous tear or equivalent (i.e. bony or cartilaginous enthesis avulsion), located on the elbow anterior compartment in six cases, the medial compartment in three cases, and the anteromedial compartment in two cases. Ten patients had fractures, including four medial epicondyle fractures and six coronoid fractures. Among those six coronoid fractures, three patients had an additional capsuloligamentous lesion of the elbow lateral compartment.
Diagnosis
The third lesion was diagnosed preoperatively in 10 cases (48%), intraoperatively in 10 cases (48%), and postoperatively in 1 case (4%). The children diagnosed preoperatively tended statistically (p = 0.07) to be older than the children diagnosed intra- and post-operatively (i.e. 12.2 ± 1.7 years old and 10.7 ± 2.6 years old).
Triad injuries characteristics were reported in Table 1, and patients’ characteristics were depicted in Table 2. All patients whose triad was diagnosed preoperatively (N = 10) had an anterior or medial fracture of the elbow apparent on preoperative radiographs, including a medial epicondyle fracture in four cases and a coronoid fracture in six cases. All patients whose triad was diagnosed during or after surgery (N = 11) had a capsuloligamentous lesion or a cartilaginous enthesis avulsion that was not apparent on preoperative radiographs. In 10 cases, the third lesion was identified during intraoperative testing, with elbow instability persisting after radial neck fracture stabilization. In a 13-year-old patient, the third lesion (i.e. capsuloligamentous tear of the anterior compartment) was identified postoperatively, with day 1 postoperative radiographs showing the recurrence of the initial posterior elbow dislocation.
Table 1.
Characteristics of population.
| Population (N = 21) | Preoperative diagnoses (N = 10) | Surgical diagnoses (N = 10) | Postoperative diagnoses (N = 1) | |
|---|---|---|---|---|
| Mean age at surgery (years) ± SD (range) |
11.5 ± 2.3 (6.4–14.9) |
12.2 ± 1.7 (9.2–14.9) |
10.3 ± 2.6 (6.4–14.4) |
13 |
| Direction of elbow dislocation (n) | ||||
| Posterolateral | 12 | 7 | 5 | / |
| Isolated posterior | 6 | 1 | 4 | 1 |
| Posteromedial | 3 | 2 | 1 | / |
| Chambers classification for fracture of radius proximal end (n) | ||||
| I.A | 14 | 7 | 6 | 1 |
| I.B | 4 | 3 | 1 | / |
| I.E | 3 | / | 3 | / |
| Bony/capsular ligament lesion (n) | ||||
| Capsular ligament lesion | 11 | / | 10 | 1 |
| Bone fracture | 10 | 10 | / | / |
SD: standard deviation.
N represents the number of patients included.
Table 2.
Demographic characteristics for each patient.
| Patient (n) | Gender | Age (years) | Type of injury | Proximal radial fracture: chambers classification | Direction of elbow luxation | Description of the third lesion | Moment of the third’s lesion diagnostic |
|---|---|---|---|---|---|---|---|
| 1 | F | 12 | Fall | I.A | Postero-lateral | Medial epicondyle fracture | Preoperatively |
| 2 | M | 8 | Fall | I.A | Posterior | Anterior compartment tear | Peroperatively |
| 3 | F | 12 | Sport | I.B | Postero-lateral | Coronoid fracture | Preoperatively |
| 4 | M | 14 | Sport | I.A | Posteromedial | Coronoid fracture | Preoperatively |
| 5 | F | 9 | Sport | I.A | Posterolateral | Medial epicondyle fracture | Preoperatively |
| 6 | F | 6 | Fall | I.A | Posterolateral | Medial compartment tear | Peroperatively |
| 7 | M | 14 | Fall | I.B | Posterolateral | Coronoid fracture | Preoperatively |
| 8 | F | 8 | Motorbike | I.A | Posteromedial | Anteromedial compartment tear | Peroperatively |
| 9 | M | 13 | Fall | I.A | Posterior | Anterior compartment tear | Postoperatively |
| 10 | F | 9 | Sport | I.A | Posterior | Medial compartment tear | Peroperatively |
| 11 | F | 10 | Fall | I.A | Posterolateral | Medial epicondyle fracture | Preoperatively |
| 12 | F | 14 | Sport | I.B | Posterolateral | Medial compartment tear | Peroperatively |
| 13 | M | 13 | Fall | I.A | Posterolateral | Coronoid fracture | Preoperatively |
| 14 | M | 10 | Fall | I.B | Posteromedial | Coronoid fracture | Preoperatively |
| 15 | M | 10 | Fall | I.E | Posterolateral | Anterior compartment tear | Peroperatively |
| 16 | F | 12 | Sport | I.A | Posterolateral | Medial epicondyle fracture | Preoperatively |
| 17 | F | 10 | Fall | I.A | Posterolateral | Anterior compartment tear | Peroperatively |
| 18 | H | 14 | Motorbike | I.E | Posterior | Anterior compartment tear | Peroperatively |
| 19 | F | 10 | Sport | I.E | Posterior | Anteromedial compartment tear | Peroperatively |
| 20 a | F | 12 | Sport | I.A | Posterior | Coronoid fracture | Preoperatively |
| 21 | F | 11 | Fall | I.A | Posterolateral | Anterior compartment tear | Peroperatively |
Lost to follow-up.
Surgical procedures
Regarding proximal radius fractures, 9 closed reductions were performed (including 6 which required internal fixation with an intramedullary wire and 3 which were stable without osteosynthesis), and 12 open reductions and internal fixations (including 6 with an intramedullary wire, 5 with a bicortical wire, and 1 screw osteosynthesis) (Table 3). In cases where the third lesion was an epitrochlear fracture (i.e. 4 patients), the fixation was performed in the same operating time, using wires. In the other cases (i.e. 17 patients), elbow stability was tested after reduction and stabilization of the radius fracture. If elbow stability was maintained in full supination and in flexion ranging from 60° to 90° (i.e. 10 cases), it was decided not to perform surgical treatment of the capsuloligamentous lesion and immobilize the elbow in a cast in the stability position. If elbow stability was not maintained (i.e. 7 cases), a surgical repair of the injured compartment was performed, with reinsertion with anchors or direct suture (Table 3).
Table 3.
Surgical procedure for each patient.
| Patient (n) | Surgery procedure for the radial fracture | Surgery procedure for the third lesion | Elbow stability at the end of procedure | Duration of the plaster cast (weeks) | Physiotherapy |
|---|---|---|---|---|---|
| 1 | Closed reduction | Osteosynthesis (wires) | Stable | 6 | No |
| 2 | Open reduction CM wires | No | Stable above 60° flexion | 5 | No |
| 3 | Open reduction and wires | Lateral ligament repair | Stable | 6 | Yes |
| 4 | Open reduction and CM wires | Ligament repair | Stable | 3 | Yes |
| 5 | Closed reduction and CM wires | Osteosynthesis (wires) | Stable | 6 | No |
| 6 | Closed reduction and CM wires | No | Stable above 60° flexion | 3 | No |
| 7 | Open reduction and screws | Ligament repair | Stable | 6 | Yes |
| 8 | Closed reduction and CM wires | Ligament repair | Stable | 6 | Yes |
| 9 | Closed reduction and CM wires | No | Stable above 60° flexion | 6 | No |
| 10 | Open reduction and wires | No | Stable above 60° flexion | 4 | Yes |
| 11 | Open reduction and wires | Osteosynthesis (wires) | Stable | 6 | Yes |
| 12 | Closed reduction | No | Stable above 60° flexion | 6 | Yes |
| 13 | Closed reduction | Coronoid ablation and ligament repair | Stable | 6 | Yes |
| 14 | Open reduction and wires | Ligament repair | Stable | 3 | No |
| 15 | Open reduction and CM wires | No | Stable above 60° flexion | 8 | No |
| 16 | Closed reduction and CM wires | Osteosynthesis (wires) | Stable | 8 | No |
| 17 | Open reduction and CM wires | No | Stable above 60° flexion | 6 | No |
| 18 | Open reduction and wires | Ligament repair | Stable | 5 | No |
| 19 | Open reduction and CM wires | No | Stable above 60° flexion | 6 | No |
| 20 a | Open reduction and CM wires | No | Stable above 60° flexion | 5 | No |
| 21 | Closed reduction and CM wires | No | Stable above 60° flexion | 4 | No |
CM: centro-medullary.
Lost to follow-up.
Complications and additional surgeries
Complications were observed in 2 patients (10%), including a persistent posteromedial elbow instability on day 15 due to secondary displacement of the radial head fracture (Case 3) and a non-union of the radius fracture (Case 19) (Table 4). In Case 3, only the ligament lateral tear had been repaired by the approach of the radial head fracture’s osteosynthesis. The cartilage avulsion fracture of the coronoid had been neglected. Two patients required an additional surgery (10%), with Case 3 who required a new procedure on day 16 that included a radial head arthroplasty, a coronoid osteosynthesis by screws and a medial collateral ligament repair, and Case 11 who underwent elbow arthrolysis 3 years after the initial procedure due to severe pronosupination limitation with preoperative ROM of 30°/30°, respectively (Table 4).
Table 4.
Outcomes for each patient.
| Patient (n) | Follow-up (years) | ROM Extension/flexion (°) |
ROM Pronation/supination (°) |
MEPS (/100) | Quick-DASH (/100) | Abnormalities radiographic | Complications | Re-operations |
|---|---|---|---|---|---|---|---|---|
| 1 | 14 | 0/150 | 90/90 | 100 | 0 | No | No | No |
| 2 | 2 | 0/140 | 60/60 | 100 | 4 | Synostosis | No | No |
| 3 | 6 | 20/140 | 40/40 | 77.5 | 34 | No | Day 15: instability and radial head displacement/stiffness | Day 16: radial head arthroplasty, coronoid osteosynthesis, and medial compartment repair |
| 4 | 6 | 20/150 | 90/-10 | 90 | 6.8 | Radiocapitellar subluxation | No | No |
| 5 | 7 | 0/150 | 90/90 | 86.5 | 2.3 | No | No | No |
| 6 | 19 | 0/150 | 90/90 | 100 | 0 | Radiocapitellar subluxation | No | No |
| 7 | 2 | 20/150 | 90/90 | 100 | 0 | No | No | No |
| 8 | 2 | 0/150 | 90/20 | 95 | 6.25 | Radial head necrosis | No | No |
| 9 | 3 | 0/150 | 90/90 | 100 | 0 | No | No | No |
| 10 | 2 | 10/110 | 60/20 | 90 | 31.2 | No | No | No |
| 11 | 9 | 10/150 | 30/30 | 72.5 | 36.3 | No | No | Years 3: arthrolysis |
| 12 | 6 | 20/150 | 90/90 | 100 | 31.8 | No | No | No |
| 13 | 18 | 0/150 | 90/90 | 100 | 0 | No | No | No |
| 14 | 2 | 0/140 | 45/60 | 100 | 0 | No | No | No |
| 15 | 11.5 | 0/150 | 10/0 | 100 | 13.6 | Synostosis | No | No |
| 16 | 3.5 | 0/150 | 90/90 | 100 | 2.3 | No | No | No |
| 17 | 14.5 | 0/120 | 0/30 | 81 | 43.1 | No | No | No |
| 18 | 1.5 | 20/120 | 90/30 | 81 | 22.7 | No | No | |
| 19 | 10.5 | 0/140 | 10/50 | 100 | 9 | Radial head necrosis | Pseudarthrosis of the radial head | No |
| 20 a | / | / | / | / | / | / | / | / |
| 21 | 2.5 | 0/140 | 80/80 | 91 | 11.3 | No | No | No |
ROM: range of motion; MEPS: Mayo Elbow Performance Score.
Lost to follow-up.
Last follow-up
The patient lost to follow-up (Case 20) was removed from the analysis. The mean follow-up was 5.8 ± 5 years (2–18). At last follow-up (Table 4), mean elbow ROM in flexion, extension, pronation, and supination were of 142° ± 12° (110°–150°), 5° ± 8° (0°–20°), 66° ± 31° (0°–90°) and 56° ± 33° (−10° to 90°), respectively. Mean MEPS and Quick-DASH scores were of 93 ± 9 points (72.5–100) and 13 ± 17 points (0–43), respectively.
At last follow-up, mean active ROM in flexion, pronation, and supination was significantly lower in patients with an open approach for radial fracture reduction (i.e. 137°, 48°, and 30°, respectively) than in patients with a closed reduction (i.e. 150°, 90°, and 90° with p = 0.02, p = 0.005, and p = 0.0001, respectively). There was a statistical trend for the MEPS score (90 vs 97 points; p = 0.06) and the Quick-DASH (18 vs 6 points; p = 0.06). At the last follow-up, we found four radiological abnormalities (two radioulnar synostosis, one radial head osteonecrosis, and one radiocapitellar subluxation) in the open approach radial osteosynthesis group, whereas we reported one case of radioulnar synostosis and one case of radiocapitellar subluxation in the closed reduction radial head fracture group. We reported radiographic abnormalities in six cases, including two radiocapitellar subluxation (10%), two proximal radioulnar synostosis (10%), and two osteonecrosis of the radial head (10%).
Discussion
Radial neck fractures represent slightly more than 1% of childhood fractures 17 and approximately 5% of childhood elbow fractures.18,19 According to our study, the “unhappy triad” of the children elbow is a rather rare lesion that can be observed in less than 3% of proximal radius fractures that required surgical treatment. Its sex ratio was 1.5 in favor of girls, and the mean age at the time of injury was 11.4 ± 2.3 years old. These findings are consistent with the female predominance and mean age of occurrence between 9 and 11 years that are observed for other elbow fractures. 3 As previously described, complex elbow injuries are commonly the consequence of high-energy mechanisms. 20
The retrospective analysis of this case series demonstrated that, depending on the nature of the third lesion (i.e. evident fractures vs capsuloligamentous lesions), the diagnosis was made at three different times. In patients with fractures, the diagnosis could be made in the emergency department, since all three lesions were visible on initial X-rays. In patients whose triad was not diagnosed preoperatively, the diagnosis was made intra- or post-operatively due to the subsequent instability. Intra-operatively, the operating surgeon noted a persistent instability of the elbow despite stable reduction and fixation of the radial fracture. Postoperatively, the diagnosis was made on the day 1 radiographs that also demonstrated a persistent elbow instability. Such delayed diagnosis was made in 11 cases; these children tended to be younger than the ones with evident fractures (10.7 ± 2.6 years vs 12.4 ± 1.7 years), but no significant difference could be outlined (p = 0.07).
An example is the case (Figure 2) of an 8-year-old girl whose diagnosis was made intraoperatively because of persistent elbow instability despite stable osteosynthesis of the proximal radius fracture. Significant soft tissues swelling of the medial aspect of the elbow was visible on the standard AP radiograph and was attributed to an anteromedial capsuloligamentous third lesion. Fixation of the medial ligament and anterior capsule allowed us to obtain satisfactory elbow stability. We can also address whether an ultrasound or magnetic resonance imaging (MRI) examination would have helped diagnose ligament tears. 21 The advantage of MRI is that it is free of radiation, is operator independent, and allows the diagnosis of traumatic cartilaginous and ligament injuries of the elbow in children. 22 Nevertheless, it depends on the surgeons’ practices because in our analysis centers, the reduction of the dislocation is performed in the operating room for better analgesia and to test the stability under general anesthesia.
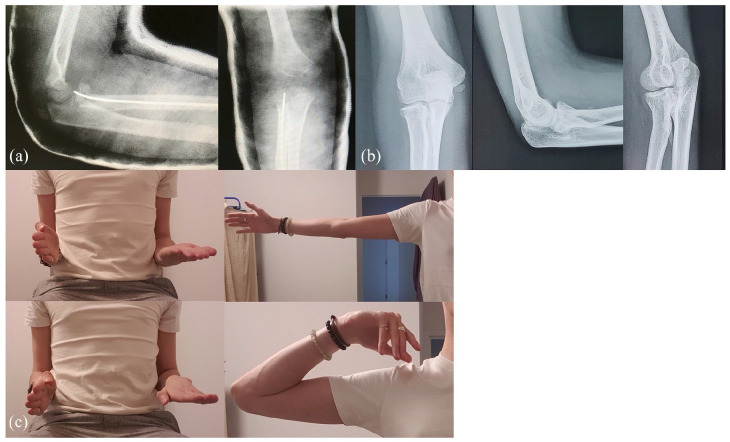
Figure 2.
Case 8. Frontal and sagittal preoperative radiographs (a) of an unhappy triad after reduction of elbow dislocation in an 8-year-old child. Soft tissue depth is increased in the medial compartment and may suggest a third capsule-ligament injury. Peroperative radiographs (b). Frontal and sagittal last follow-up radiographs (c) show good joint congruence after retention of the anteromedial plane but early epiphyseal necrosis of the radius.
Another important finding of this study lies in the classification of anatomical lesions. In fact, we did not observe any radial neck fracture called “reduction injuries,” as previously reported by Jeffery 18 (i.e. I.D lesions according to Chambers’ classification). Instead, we noted only anterior displacements of radial neck fractures, called “dislocation injuries” by Jeffery 18 (i.e. three patients presenting with a I.E lesion according to Chambers’ classification). Our hypothesis is that there is a ligament disruption in these elbow “unhappy triads”; subsequently, reduction lesions would be highly unlikely.
Based on those findings, we propose a classification of the “unhappy triad” of the child’s elbow (Figure 3). Type A describes the anatomical nature of the injury (i.e. bone or ligament). Type B describes the affected compartment, either medial, anterior, or a combination of the two compartments. Accordingly, in type A1 with a visible bony lesion visible, we propose the osteosynthesis of the fracture. In case of a patient presenting in the emergency department with a combination of elbow dislocation and proximal radius fracture, we propose a complementary examination by ultrasound or MRI, after reduction of the dislocation in emergency department, to detect a possible cartilage or ligament injury (type A2). In the absence of available imaging or a dislocation reduction in operating room, further surgical exploration of the capsuloligamentous insertion on the coronoid may be necessary if instability persists despite stabilization of the proximal radius fracture.
Figure 3.

Classification of unhappy traumatic triad of children’s elbow.
The outcomes at last follow-up provide two significant findings. First, active ROM (i.e. flexion, pronation, and supination) are significantly impaired (by 13°, 32°, and 60° on average) if the open approach for the reduction of the proximal radial fracture was performed compared to a closed reduction (Figure 4). This is an important consideration for the surgeon to consider before proceeding with an open approach, and an important message for parents regarding future functional results. Yang et al. 23 reported in a recent series of 101 reviewed cases of surgically treated radial neck fracture with a mean flexion of around 148°, extension of −3°, pronation of 78°, and supination of 94° at 3.8 years mean follow-up. These findings seem consistent with our study in which, after a mean follow-up of 5.8 years, active ROM were 137°, 5°, 48°, and 30° in cases with an open approach, and 150°, 5°, 90°, and 90° in cases with a closed reduction, respectively. In this article, 23 he reports also that the rate of unsatisfactory results in open reduction group (75%) was significantly higher than that in the closed reduction group (22%) (p ≤ 0.001). This is consistent with our secondary result. Second, we found no significant differences between patients who underwent capsuloligamentous surgical repair and those who were treated with orthopedic immobilization. In reviewing the records, patients treated with immobilization were those whose persistent instability (i.e. after stabilization of the radius fracture) remains below 60° of flexion (Table 3). In cases where instability persisted above 60° of flexion in neutral, varus, or forced valgus position, surgical repair was performed. The question that remains is whether to operate on those with persistent instability below 60° of flexion. For cases where only the anterior compartment was affected, the results were satisfactory (Table 4). However, in Case 6, where the initial injury was to the medial capsuloligamentous compartment, a radiographic anterior subluxation of the radial head persisted at last follow-up, without functional consequence at the last follow-up.
Figure 4.
Case 15. Sagittal and frontal postoperative radiographs (a). Frontal and sagittal last follow-up (11.5 years after surgery) radiographs (b) show a proximal radioulnar synostosis. Range of motions of elbow at the last follow-up (c) show a limitation of pronation and supination.
The findings of this study should be considered in the light of its inherent limitations. It is a retrospective study for a rare entity with only 21 patients. However, all children requiring surgical care due to an osteoarticular emergency in the urban area in which we work are transferred to three pediatric university centers. It is the largest series describing this elbow traumatic triad combination; Magee et al. 10 presented a series of 26 elbow trauma cases, of which only 7 cases corresponded with our “unhappy” triad. Our multicentric research collects the data from two of these three centers. Another limitation of this study is that we did not assess the results at the last follow-up according to the quality of bone reduction or ligament repair from the first surgery. It is difficult in a retrospective study to assess the quality of surgery, as this is usually a very subjective criterion, but this potential bias should be taken into consideration. In addition, to our knowledge, there have been no studies validating the Mayo Elbow Performance Score (MEPS) in adolescents. However, it is widely used in the literature as a tool for assessing results after the management of a traumatized elbow in children.14,24
Conclusion
The “unhappy” triad of the child’s elbow, i.e., combining a posterior dislocation, a proximal radius fracture, and a third lesion (bony or capsuloligamentous injury), is a rare injury resulting from a high-energy trauma and whose preoperative diagnosis is missed in 50% of cases. Further surgical exploration of the capsuloligamentous insertion on the coronoid or the medial compartment (i.e. the third lesion) may be necessary if elbow instability persists beyond 60° of flexion despite stabilization of the proximal radius fracture. It is essential to consider the “unhappy” triad as a severe injury leading to complications and re-operations in 10% of cases, as well as proximal radioulnar synostosis, radiocapitellar subluxation, and radial head necrosis in almost 30% of cases at mid-term follow-up.
Supplemental Material
Supplemental material, sj-pdf-1-cho-10.1177_18632521231211643 for “Unhappy triad” of the trauma elbow in children: Diagnosis, classification, and mid-term outcomes by Tristan Langlais, Emmanuelle Louis, Alina Badina, Raphael Vialle, Stéphanie Pannier, Malo Le Hanneur and Franck Fitoussi in Journal of Children’s Orthopaedics
Footnotes
Author’s note: Franck Fitoussi is also affiliated to CRMR STREAM (Limb Malformation Referral Center), Paris, France.
Author contributions: T.L. contributed to data analysis and interpretation, critical revisions, manuscript writing, manuscript review, and statistical analysis. E.L. contributed to data acquisition, data analysis and interpretation, and manuscript writing. A.B. contributed to data acquisition. R.V. and S.P. contributed to critical revisions and manuscript review. M.L.H. contributed to critical revisions, manuscript review, administration, and study supervision. F.F. contributed to critical revisions, manuscript review, and study supervision.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The study has been approved by a local ethics committee (IRB no. 19-01 v0). It was also registered in the National Committee of Computer science and Liberties register (no. 2223801 v0); once legal guardians of each patient were individually informed, charts review was conducted following the 1964 Declaration of Helsinki ethical standards and the Methodology of Reference MR-003.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Inform consent: Written informed consent was obtained in each case from both the patient and the parents.
References
- 1. Beekman F, Sullivan JE. Some observations on fractures of long bones in children. Am J Surg 1941; 51: 722–738. [Google Scholar]
- 2. Landin LA, Danielsson LG. Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop Scand 1986; 57(4): 309–312. [DOI] [PubMed] [Google Scholar]
- 3. D’souza S, Vaishya R, Klenerman L. Management of radial neck fractures in children: a retrospective analysis of one hundred patients. J Pediatr Orthop 1993; 13(2): 232–238. [PubMed] [Google Scholar]
- 4. Finnbogason T, Karlsson G, Lindberg L, et al. Nondisplaced and minimally displaced fractures of the lateral humeral condyle in children: a prospective radiographic investigation of fracture stability. J Pediatr Orthop 1995; 15(4): 422–425. [DOI] [PubMed] [Google Scholar]
- 5. Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet 1959; 109(2): 145–154. [PubMed] [Google Scholar]
- 6. Klug A, Nagy A, Gramlich Y, et al. Infographic: surgical treatment of the radial head in terrible triad injuries of the elbow. Bone Joint J 2020; 102-B(12): 1618–1619. [DOI] [PubMed] [Google Scholar]
- 7. Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am 2002; 84(4): 547–551. [DOI] [PubMed] [Google Scholar]
- 8. Rooke GMJ, Maarschalk JA, Navarre P. Pediatric terrible triad injury of the elbow: a rare and easily missed injury: a case report. JBJS Case Connect 2018; 8(4): e106. [DOI] [PubMed] [Google Scholar]
- 9. Valisena S, Hamitaga F, Gonzalez JG, et al. Osteochondral flap fracture of the coronoid in pediatric elbow dislocation: a case report and literature review. Eur J Orthop Surg Traumatol 2019; 29(1): 213–220. [DOI] [PubMed] [Google Scholar]
- 10. Magee LC, Baghdadi S, Gohel S, et al. Complex fracture-dislocations of the elbow in the pediatric population. J Pediatr Orthop 2021; 41(6): e470–e474. [DOI] [PubMed] [Google Scholar]
- 11. Garcelon N, Neuraz A, Benoit V, et al. Improving a full-text search engine: the importance of negation detection and family history context to identify cases in a biomedical data warehouse. J Am Med Inform Assoc 2017; 24: 607–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chambers HG. Fracture of the proximal radius and ulna. In: Kasser JR, Beaty JH. (eds) Rockwood and Wilkins’ fractures in children. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2001, pp. 483–528. [Google Scholar]
- 13. Metaizeau JP, Lascombes P, Lemelle JL, et al. Reduction and fixation of displaced radial neck fractures by closed intramedullary pinning. J Pediatr Orthop 1993; 13(3): 355–360. [DOI] [PubMed] [Google Scholar]
- 14. Nussberger G, Schädelin S, Mayr J, et al. Treatment strategy and long-term functional outcome of traumatic elbow dislocation in childhood: a single centre study. J Child Orthop 2018; 12(2): 129–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Beaton DE, Wright JG, Katz JN, et al. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am 2005; 87(5): 1038–1046. [DOI] [PubMed] [Google Scholar]
- 16. Failla JM, Amadio PC, Morrey BF. Post-traumatic proximal radio-ulnar synostosis: results of surgical treatment. J Bone Joint Surg Am 1989; 71(8): 1208–1213. [PubMed] [Google Scholar]
- 17. Landin LA. Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950–1979. Acta Orthop Scand Suppl 1983; 202: 1–109. [PubMed] [Google Scholar]
- 18. Jeffery CC. Fractures of the head of the radius in children. J Bone Joint Surg Br 1950; 32-B(3): 314–324. [DOI] [PubMed] [Google Scholar]
- 19. Fowles JV, Kassab MT. Observations concerning radial neck fractures in children. J Pediatr Orthop 1986; 6(1): 51–57. [PubMed] [Google Scholar]
- 20. Bastard C, Le Hanneur M, Pannier S, et al. Radial neck fractures in children secondary to horse-riding accidents: a comparative study. Orthop Traumatol Surg Res 2020; 106(7): 1293–1297. [DOI] [PubMed] [Google Scholar]
- 21. Barret H, Gastaud O, Laumonerie P, et al. Feasibility and technique of ultrasound traumatic elbow lesion assessment. Orthop Traumatol Surg Res 2021; 107(2): 102836. [DOI] [PubMed] [Google Scholar]
- 22. Chauvin NA, Gustas-French CN. Magnetic resonance imaging of elbow injuries in children. Pediatr Radiol 2019; 49(12): 1629–1642. [DOI] [PubMed] [Google Scholar]
- 23. Yang L, Yang X, Zuo J, et al. A retrospective review of 101 operatively treated radial neck fractures in children and analysis of risk factors for functional outcomes. Injury 2022; 53(10): 3310–3316. [DOI] [PubMed] [Google Scholar]
- 24. Guzikiewicz N, Małecki K, Sibiński M, et al. Clinical and radiological evaluation of radial neck factures in children and adolescents treated by percutaneous leverage reduction with Kirschner wire stabilization. Int Orthop. Epub ahead of print 9 September 2023. DOI: 10.1007/s00264-023-05965-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-cho-10.1177_18632521231211643 for “Unhappy triad” of the trauma elbow in children: Diagnosis, classification, and mid-term outcomes by Tristan Langlais, Emmanuelle Louis, Alina Badina, Raphael Vialle, Stéphanie Pannier, Malo Le Hanneur and Franck Fitoussi in Journal of Children’s Orthopaedics