Abstract
Objectives
Parameniscal cysts can be removed without meniscectomy, but for large or multiloculated meniscal cysts, traditional arthroscopic excision may leave the meniscus unstable. This study aimed to describe a modified fat pad approach for parameniscal cyst arthroscopic excision that retains a stable structure of the synovial margin of the meniscus and to compare the clinical outcomes between the traditional cyst excision and modified excision techniques.
Methods
Fifty‐six patients with parameniscal cysts between 2014 and 2018 were retrospectively included in this study with 28 patients in each group. All patients underwent arthroscopic parameniscal cyst excisions with traditional and modified excision techniques respectively in each group. The International Knee Documentation Committee subjective (IKDC) score, Lysholm score, visual analogue scale (VAS) score, Tegner score, active range of motion (ROM) and time to recover full ROM were used to evaluate the clinical outcomes by using the t‐test.
Results
The patient population included 21 males and 35 females, with a mean follow‐up of 29 months. Of these, 28 patients underwent traditional arthroscopic cyst excisions and meniscal sutures, and 28 patients underwent arthroscopic excisions by the modified fat pad approach. There were no significant differences in the IKDC score, Lysholm score, Tegner score or VAS score between the traditional and modified excision groups at the final follow‐up time point. However, the postoperative time to recover full ROM in the modified excision group was significantly lower than those in the traditional excision group (p < 0.05).
Conclusion
Arthroscopic excision with the modified fat pad approach yielded a shorter pain phase and less time to recover full ROM during recovery compared with the traditional arthroscopic excision. The new method seemed to be effective, as evidenced by the positive clinical outcomes of patients.
Keywords: Arthroscopy, Excision, Knee, Parameniscal cysts
Arthroscopic excision with the modified fat pad approach yielded a shorter pain phase and less time to recover full range of movement during recovery compared with the traditional arthroscopic excision. The new method seemed to be effective, as evidenced by the positive clinical outcomes of patients.
Introduction
Parameniscal cysts were first described approximately one century ago and are small cystic lesions located along the peripheral margin of the meniscus. 1 Even so, the causes and pathogenesis of parameniscal cysts remains controversial. It is widely accepted that parameniscal cysts are associated with fibrocartilaginous myxoid degeneration or extrusion of synovial fluid through a meniscal tear. 2 , 3 , 4 Parameniscal cysts were considered relatively uncommon through the 1980s and 1990s 5 , 6 , 7 , 8 because most of them were small and asymptomatic and rarely present as a painful mass. 1 , 9 , 10 In fact, a typical meniscal cyst appears as a fluid mass on MRI, showing fluid signal intensity on both the T1‐ and T2‐weighted sequences. 11 As imaging research progresses, MRI has been the first choice in the diagnosis of these cysts. 12 , 13 MRI‐based evidence suggests that parameniscal cysts are not only more common than previously estimated but also more likely to occur on the lateral side of the knee. 5 , 12 , 14 It seems that the soft tissue around the lateral aspect of the knee is thinner than that in the medial compartment, so parameniscal cysts that form on the lateral side are more easily recognized than those that form on the medial side. 15 The lateral parameniscal cysts are involved more often than medial meniscus. 2 , 14
With the more widespread use of arthroscopy, the most commonly used treatments for parameniscal cysts have been arthroscopic excision and decompression. 16 , 17 , 18 It is well‐known that parameniscal cysts can be removed without meniscectomy, while for large or multiloculated meniscal cysts, arthroscopic decompression or excision may leave the meniscus unstable. According to several studies, 5 , 19 , 20 the incidence of parameniscal cyst recurrence in patients undergoing arthroscopic excision or arthroscopic decompression is estimated to be 9.4% to 15% and it has been widely recognized that factors such as cyst dimension, failure to disrupt the check‐valve mechanism, and multilobulated structure contribute to the recurrence rate of the cyst. Furthermore, the study of Chang et al. 17 found that the arthroscopic decompression group had a significantly higher recurrence risk (21%), compared to the arthroscopic excision group (4%). And the suture technique is performed to meniscocapsular opening or the synovial margin of the meniscus to lower the cyst recurrence rate. 17 , 21
From this, we developed an arthroscopic excision by a modified fat pad approach, which retains a stable structure of the synovial margin of the meniscus. It preserves the stable structure of the femoral and tibial sides of the meniscus well and eliminated the need for meniscal sutures. Our hypothesis is that the modified fat pad approach is an effective and repeatable technique. And we assume this less aggressive surgery with appropriate rehabilitation protocol can lead to better results. So we compared the clinical outcome of the new technique with the traditional excision. The purpose of this study were as follows: (i) to describe this new method; and (ii) to compare the clinical outcomes between the traditional excision and the modified excision technique.
Methods
Patient Selection
The inclusion criteria were as follows: (i). inpatients undergoing parameniscal cyst excisions from 2014 to 2018; (ii) all patients were diagnosed with parameniscal cysts and the diagnoses were confirmed by MRI; and (iii) patients were treated with traditional arthroscopic excisions or arthroscopic excisions by the modified fat pad approach. Patients with various metabolic bone diseases, such as incomplete osteogenesis and osteomalacia were excluded.
As a result, 56 patients with a mean age of 38.24 years undergoing parameniscal cyst excisions from 2014 to 2018 were retrospectively evaluated. All patients had a III°lateral meniscus injury according to the three‐grade staging system, 22 and basically horizontal or radial meniscus tears and complained of pain, mechanical locking, or a palpable mass in the knee.
Both operation procedures will be fully explained to the patient before surgery, and the actual treatment modalities will be decided by patients with full respect for the wishes of themselves. Patients who only received conservative medical treatment, patients who failed to sign the informed consent form, and patients with concomitant ligament injuries, chronic intraarticular fractures, rheumatoid arthritis, osteoarthritis, gouty arthritis, or lost to follow‐up were excluded. Our research was approved by the Institutional Ethics Committee (2017‐358). All procedures were achieved by one surgeon. All patients were informed and signed a written informed consent upon participation in this study. A flow diagram in the selection of eligible patients is shown in Figure 1.
FIG. 1.

The flow diagram in the selection of eligible patients.
Clinical Assessment
All patients were followed up at the 2nd week, 4th week, 6th week, 8th week, 10th week, 3rd month, 6th month, 12th month, and the final point after the surgical procedure. The clinical outcomes were evaluated by the International Knee Documentation Committee (IKDC) score, Lysholm score, visual analogue scale (VAS) score, Tegner score, and active range of motion (ROM) at preoperative and each time point. In addition, we also included the time to recover full ROM compared to the opposite side in the clinical outcomes. The follow‐up with evaluation scales were in accordance with the standard procedures of the hospital.
Radiological Assessment
The patients underwent radiological assessment using MRI preoperatively at the radiological center of our hospital. Postoperative radiological assessments were performed on either MRI or ultrasound depending on patient preference at the same radiological center as before. A sports medicine surgeon and a musculoskeletal radiologist evaluated the preoperative and postoperative radiological imaging. If a discrepancy was noted between the two readers, another two musculoskeletal radiologists and one sports medicine surgeon reached a consensus. The postoperative radiological assessment aimed to verify the removal of a cyst or no recurrence.
Surgical Techniques
For the traditional arthroscopic excision, patients were placed in the supine position, and an arthroscopic diagnosis was conducted with the standard anterolateral and anteromedial portals of the injured knee. After the arthroscopic diagnosis, the cysts with the wall were completely removed through the existing portals and the torn meniscus was debrided down to a stable rim, preserving as much meniscal tissue as possible. Then, the suture technique was performed to stabilize the synovial margin of the meniscus. After that, the stability was assessed.
For arthroscopic excisions by a modified fat pad approach, we first established the anterolateral portal to perform the arthroscopic diagnosis and then established the anteromedial portal to probe, debride and reshape the torn meniscus. Finally, the arthroscope and shaver were inserted from the appropriate anteromedial and anterolateral portals, respectively. Then a passageway to the cyst was made by shaver through the anterolateral fat pad at the level of the lateral meniscus with the stable structure of the femoral and tibial sides of the meniscus intact. An extra lateral portal beside the cysts was made under arthroscopic view. Then the arthroscope was switched to an anterolateral portal and instruments were inserted from the lateral portal. The cysts were exposed under direct arthroscopic view and removed horizontally along with the meniscus tissue. Even very small cysts can be found and removed by this technique.
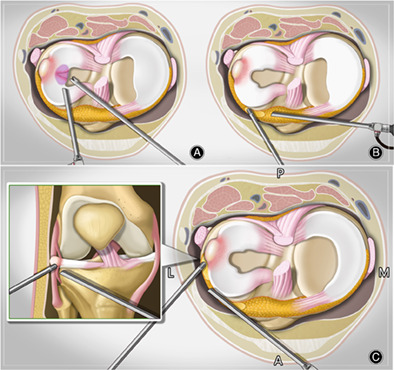
Compared with the traditional arthroscopic cyst excision, the modified arthroscopic cyst excision can preserve the stable structures of the meniscus synovial rim and can clearly show the inner and surrounding tissues of the parameniscal cyst. The modified procedure is shown in Figure 2. Arthroscopic photographs show the whole process in Figure 3.
FIG. 2.

The operation procedure by a modified fat pad approach. (A) An anterolateral portal was established to perform the arthroscopic diagnosis. The anteromedial portal was established to probe, debride and reshape the torn meniscus. (B) A passageway to the cyst was made by shaver through the anterolateral fat pad at the level of the lateral meniscus with the stable structure of the femoral and tibial sides of the meniscus intact. (C) An extra lateral portal beside the cysts was made under arthroscopic view. The arthroscopy and shaver were inserted in the anteromedial and anterolateral portals, respectively, to expose the cysts laterally and remove them horizontally along with the meniscus from the planned level of the fat pad.
FIG. 3.
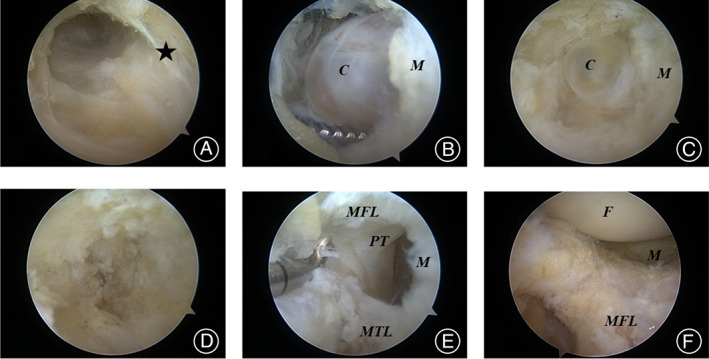
Images under arthroscopy during surgery. (A) Passageway to the cyst was made by shaver through the anterolateral fat pad at the level of the meniscus. (B) Blunt dissection exposes the cyst. (C) Exposure of small deep cysts after excision of large cysts. (D) Exposure of the popliteal tendon after complete excision of the cyst. (E, F) Situation after cyst removed. Asterisk: level of meniscus; MFL: meniscofemoral ligament; M: meniscus; MTL: meniscotibial ligament; C: cyst; F: femur; PT: popliteal tendon.
Rehabilitation
There were different rehabilitation protocols for patients in different groups. All patients in the modified group were not allowed to use the orthosis and were required to start partial weight‐bearing on the day of surgery. Full weight‐bearing was suggested 4 weeks after surgery. Knee ROM with permission to attempt 90° 2 weeks after surgery and 120° 4 weeks after surgery. While patients in the traditional group were requested to use the orthosis for the first 4 weeks and start partial weight‐bearing and functional exercises for knee flexion (90°) after 4 weeks. Knee ROM was suggested to be 120° and full weight‐bearing could be achieved 6 weeks after surgery.
Statistical Analysis
Data were analyzed using the Statistical Package for Social Sciences 15.0 for Windows (SPSS Inc., Chicago, IL, USA). The t‐test was used to assess the clinical outcomes, including the IKDC score, Lysholm score, VAS score, Tegner score, active ROM, and time to recover full ROM. p < 0.05 were considered statistically significant.
Results
The patient population included 21 males and 35 females, with a mean follow‐up of 29 months. Of these, 28 patients underwent traditional arthroscopic excisions, and 28 patients underwent arthroscopic excisions by the modified fat pad approach and an extra lateral portal. The patient population in the traditional excision group included 11 males and 17 females, with a mean age of 37.78 ± 11.46 years, while that in the modified excision group included 10 males and 18 females, with a mean age of 38.69 ± 11.04 years. There were no significant differences in terms of gender, age, or injury side between the two groups (p > 0.05). Additionally, the preoperative IKDC, Lysholm, VAS, and Tegner scores were similar in the two groups. Characteristics of the traditional excision and modified excision groups are shown in detail in Table 1.
TABLE 1.
Characteristics of the traditional and modified excision groups.
| Characteristics | Traditional excision | Modified excision | P value | |
|---|---|---|---|---|
| Total number | 28 | 28 | n.s | |
| Age (years) | 37.78 ± 11.46 | 38.69 ± 11.04 | n.s | |
| Gender | Male | 11 (39%) | 10 (36%) | n.s |
| Female | 17 (61%) | 18 (64%) | n.s | |
| Injury side | Left | 14 (50%) | 13 (46%) | n.s |
| Right | 14 (50%) | 15 (54%) | n.s | |
| Size of parameniscal cyst | 2.64 ± 0.72 | 2.61 ± 0.56 | n.s | |
| Preoperative VAS score | 5.07 ± 1.6 | 5.43 ± 1.82 | n.s | |
| Preoperative Lysholm score | 58 ± 14.32 | 59.07 ± 18.03 | n.s | |
| Preoperative IKDC score | 46.61 ± 10.46 | 48.46 ± 13.04 | n.s | |
| Preoperative Tegner score | 2.54 ± 0.9 | 2.57 ± 0.91 | n.s |
Note: Data are presented as the means ± SD or numbers (%); p > 0.05: statistically non‐significant (n.s.).
Abbreviations: IKDC, International Knee Documentation Committee; VAS, visual analogue scale.
Clinical Assessment
Both groups showed great improvement in the clinical outcomes at the final follow‐up point. The clinical outcomes revealed no statistically significant differences using the Lysholm, IKDC, Tegner score, and VAS score at the final follow‐up point (p > 0.05). The time to recover full ROM was 11.12 ± 3.72 weeks and 8 ± 4.16 weeks in the traditional and modified excision groups, respectively. Statistical analysis revealed a decreased time to recover full ROM in the modified excision group compared to the traditional excision group. Postoperative clinical outcomes in the two groups are shown in Table 2, Figures 4 and 5.
TABLE 2.
Postoperative outcomes between the traditional and modified excision groups at final follow‐up.
| Characteristics | Traditional excision | Modified excision | P value |
|---|---|---|---|
| Postoperative Lysholm score | 86.29 ± 9.79 | 85.04 ± 11.32 | n.s |
| Postoperative IKDC score | 77.61 ± 7.53 | 78.57 ± 9.61 | n.s |
| Postoperative Tegner score | 5.75 ± 1.87 | 5.93 ± 1.73 | n.s |
| Time to recover full ROM (weeks) | 11.12 ± 3.72 | 8 ± 4.16 | p = 0.004 |
Note: Data are presented as means ± SD; p > 0.05: statistically nonsignificant (n.s).
Abbreviations: IKDC, International Knee Documentation Committee; ROM, range of motion.
FIG. 4.

Postoperative VAS score between the traditional and modified excision groups.
FIG. 5.

Postoperative active ROM between the traditional and modified excision groups.
Radiological Assessment
There were parameniscal cysts that occurred with a meniscal tear in all patients preoperatively. Radiological imaging was consistent with the patients' symptoms and all patients were eligible for the operation. As for the postoperative imaging in the modified excision group, they showed this new method removed the cysts, retained the synovial margin of the meniscus without making destruction of the internal structure of meniscus, and enabled the stability of the structure. The case is shown in Figure 6.
FIG. 6.
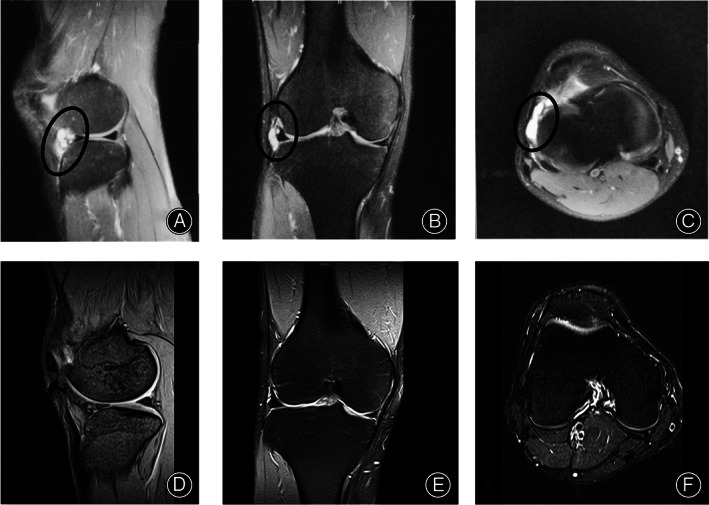
A 32‐year‐old male who felt pain over the lateral aspect of right knee with parameniscal cysts. (A–C) Sagittal, coronal and axial T2‐weighted fat‐saturated images demonstrated cysts. (D–F) Sagittal, coronal and axial T2‐weighted fat‐saturated images demonstrated the removal of cyst.
Discussion
The present study described the parameniscal cyst arthroscopic excision by the modified fat pad approach. It was observed that the 28 patients who had this new treatment obtained encouraging clinical outcomes. In addition, patients had a shorter pain phase and less time to recover to full ROM in the modified excision group.
Risk Factors of Recurrence
Several researchers 5 , 7 , 23 , 24 have identified risk factors of recurrence such as failure to abolish the check‐valve mechanism or open the meniscocapsular junction. In addition, for parameniscal cysts with large meniscal tears, the standard anteromedial and anterolateral portals in the traditional excision may limit the surgical field of vision and prevent surgeons from obtaining a complete debridement of the meniscal substance and its connecting tract, and completely opening the check‐valve mechanism. 10
Existed Surgical Technology
Parameniscal cysts, formed within or adjacent to the menisci, 10 are commonly treated by arthroscopy. Two common arthroscopic techniques are excision and decompression, and both aim to relieve symptoms. For large or huge cystic lesions, arthroscopic or open excision 17 , 25 , 26 is recommended to reduce the risk of recurrence. The conventional excision may destabilize the meniscus and need the insertion of the suture needle, which may require a longer time to rehabilitation and create microtrauma to cause degenerative change.
Furthermore, several arthroscopic techniques of intracapsular decompression while avoiding the torn meniscus have been previously reported. In a previous study, a 5‐mm channel that connected the cyst and capsule was built to equalize the pressure from the cyst and articular cavity. 27 This study reported good clinical outcomes, but only eight patients were included. Therefore, this study required more patients to be included to verify the effectiveness of the technique. Another study reported that creating a hole between the horizontal tear and cyst yielded “good” or “excellent” results in 89% of all cases. However, the inconsistent follow‐up limited the reliability of the results. MacMahon et al. performed the simple aspiration of the cysts and injection of methylprednisolone acetate (40 mg) and bupivacaine (1 mL). 28 Though this method avoided surgery, the failure rate was as high as 33%. Furthermore, arthroscopic decompression alone may not be sufficient to remove all of the cystic material from the septate meniscal cysts. 29 Additionally, the intra‐articular meniscal tear should be resected to abolish the possible check‐valve mechanism. 30
Modified Technology in this Study
To better circumvent the problems above, we developed parameniscal cyst arthroscopic excision by a modified fat pad approach. The modified fat pad approach can provide better visualization of the entire parameniscal cyst, clearly show the inner and surrounding tissues of the cyst, especially the synovial rim of the meniscus and even small cysts within the synovial rim of the meniscus, and help to remove the cysts as completely as possible. Owing to horizontal removal along with the meniscus from the planned level of the fat pad, the meniscal tissue and its peripheral rim attachment can be well preserved, and meniscal sutures are not required, which causes less damage to the surrounding important structures.
These surgical techniques are relatively simple techniques for surgeons. An extra lateral portal beside the cysts is made through the anterolateral fat pad and the meniscus can keep stable while the cysts are removed. Compared to the existed technologies mentioned above, the modified technique does not increase the difficulty of the surgery and could lower the rate of recurrence and shorten the time of rehabilitation. But there are still some points to be aware of during the operation. First, an external lateral portal is required. Second, it should be determined that the pathway to the fat pad is located at the level of meniscus so as to avoid injury to the meniscotibial ligament and the meniscocapsular ligament. Third, careful exploration is needed to avoid missing small cysts during operation.
Comparison of Outcomes
The most encouraging result of this study is a shorter recovery time to the full ROM and a shorter pain phase in the modified arthroscopic excision compared to the traditional arthroscopic excision. Due to the immobilization from orthosis, the VAS score in the traditional excision group was lower at the first 4 weeks after surgery. But once functional exercises started, the VAS score rose. Furthermore, traditional excision with meniscal sutures could change tension and cause pain, which is different from the modified excision without meniscal sutures. Patients in modified excision started immediate functional exercises with no orthosis postoperatively, so the recovery time to full ROM and muscle strength was superior to the traditional excision, which resulted in less impact on patients' work and life. Compared with previous studies, 5 , 17 , 19 , 20 patient functional outcomes are generally favorable when not considering recurrence. However, in previous studies, the overall recurrence rate was between 9.4% and 15%, and the recurrence rate for arthroscopic decompression surgery could reach up to 21%. 17 In a study 19 combining platelet‐rich plasma (PRP) treatment and suturing techniques, which included 15 patients, no recurrence was found in 2 years of follow‐up. And previous studies have not specifically reported the average time to fully recover ROM, which is a significant finding in this study.
The excellent clinical outcomes of patients have claimed that this new approach retains the steady meniscus synovial margin structure. The imaging also showed the partial defect of the fat pad produced by the approach could heal completely. And no cases of recurrence were found. Compared to traditional arthroscopic excision, the time to full ROM recovery and the duration of pain are shorter with the modified arthroscopic excision.
Limitations
There are still several limitations of our study. First, this is a retrospective study with nonrandomization, case grouping is chosen based on the patient's wishes, rather than random grouping, however, there was no statistical difference in the baseline data of patients, thus reducing the grouping bias of the study as much as possible. Second, this study is limited by the number of patients included. Third, the rehabilitation protocols were different. But it was brought about by the difference between two surgical methods. The modified excision allowed more aggressive rehabilitation in the early period.
Future Studies
In the future studies, prospective randomized controlled trial with increased sample size can be designed to compare the outcomes of arthroscopic excision using the modified fat pad approach and traditional arthroscopic excision. And a cost‐effectiveness analysis can be performed to comparing the modified fat pad approach and traditional excision. This analysis should consider factors such as surgical time, hospital stay, rehabilitation costs, and long‐term outcomes. Moreover, in the retrospective study of Screpis et al., 19 the use of autologous platelet‐rich fibrin matrix combined with meniscal repair in the treatment of parameniscal cyst demonstrated excellent subjective clinical outcomes. This suggested that the modified technique could potentially be integrated with the use of an autologous platelet‐rich fibrin matrix to achieve improved clinical outcomes.
Conclusion
In conclusion, arthroscopic excision by the modified fat pad approach resulted in a significantly shorter pain phase and less time to recover full ROM than a traditional arthroscopic excision. This method may be more widely applied to patients with parameniscal cysts who need arthroscopic surgery, especially those who need to recover quickly and return to daily activities and due to the positive clinical results of this method, it may stimulate more research to further optimize this method, in order to improve surgical outcomes and patient satisfaction.
Author Contributions
TL carried out all of the follow‐ups of the study and prepared the manuscript. RL and YS contributed to the follow‐ups of the study and analysis the data. YHL and MKY participated in designing the study. QL secured funding and was responsible for the study set‐up. All authors read and approved the final manuscript.
Conflict of Interest Statement
The authors declare that they have no competing interests. The authors also report that they have no conflicts of interest in authorship and publication of this article.
Ethics Approval
The present study was approved by the West China Hospital (No. 2017358).
Acknowledgments
We are grateful to all participating patients.
Tao Li, Ran Li and Yi Shu are contributed equally to this manuscript.
Data Availability Statement
The data and materials are available from the medical records department of West China Hospital. The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1. Kose O, Erol B, Ozyurek S, Ege T. A giant medial parameniscal cyst of the knee joint. BMJ Case Rep. 2013;2013:bcr2013009440. 10.1136/bcr-2013-009440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barrie HJ. The pathogenesis and significance of menisceal cysts. J Bone Jt Surg, Br Vol. 1979;61:184–189. 10.1302/0301-620x.61b2.582035 [DOI] [PubMed] [Google Scholar]
- 3. Lantz B, Singer KM. Meniscal cysts. Clin Sports Med. 1990;9:707–725. [PubMed] [Google Scholar]
- 4. Stensby JD, Pringle LC, Crim J. MRI of the meniscus. Clin Sports Med. 2021;40:641–655. 10.1016/j.csm.2021.05.004 [DOI] [PubMed] [Google Scholar]
- 5. Hulet C, Souquet D, Alexandre P, Locker B, Beguin J, Vielpeau C. Arthroscopic treatment of 105 lateral meniscal cysts with 5‐year average follow‐up. Arthroscopy. 2004;20:831–836. 10.1016/j.arthro.2004.06.014 [DOI] [PubMed] [Google Scholar]
- 6. Mills CA, Henderson IJ. Cysts of the medial meniscus. Arthroscopic diagnosis and management. J Bone Jt Surg, Br Vol. 1993;75:293–298. [DOI] [PubMed] [Google Scholar]
- 7. Ryu RK, Ting AJ. Arthroscopic treatment of meniscal cysts. Arthroscopy. 1993;9:591–595. 10.1016/s0749-8063(05)80411-6 [DOI] [PubMed] [Google Scholar]
- 8. Seger BM, Woods GW. Arthroscopic management of lateral meniscal cysts. Am J Sports Med. 1986;14:105–108. 10.1177/036354658601400201 [DOI] [PubMed] [Google Scholar]
- 9. Asopa V, Douglas RJ, Heysen J, Martin D. Diagnosing snapping sartorius tendon secondary to a meniscal cyst using dynamic ultrasound avoids incorrect surgical procedure. Case Rep Radiol. 2013;2013:813232. 10.1155/2013/813232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ohishi T, Suzuki D, Matsuyama Y. Arthroscopic decompression for a Giant meniscal cyst. Orthopedics. 2016;39:e166–e168. 10.3928/01477447-20151222-15 [DOI] [PubMed] [Google Scholar]
- 11. Nguyen JC, De Smet AA, Graf BK, Rosas HG. MR imaging‐based diagnosis and classification of meniscal tears. Radiographics. 2014;34:981–999. 10.1148/rg.344125202 [DOI] [PubMed] [Google Scholar]
- 12. De Smet AA, Graf BK, del Rio AM. Association of parameniscal cysts with underlying meniscal tears as identified on MRI and arthroscopy. Am J Roentgenol. 2011;196:W180–W186. 10.2214/ajr.10.4754 [DOI] [PubMed] [Google Scholar]
- 13. Saraiva L, Saraiva AP, Coutinho M, Pereira da Silva JA. Parameniscal cyst: an important differential diagnosis in slow growing masses of the knee. ARP Rheumatol. 2023;2:83–84. [PubMed] [Google Scholar]
- 14. Campbell SE, Sanders TG, Morrison WB. MR imaging of meniscal cysts: incidence, location, and clinical significance. Am J Roentgenol. 2001;177:409–413. 10.2214/ajr.177.2.1770409 [DOI] [PubMed] [Google Scholar]
- 15. Lui TH. Endoscopic resection of medial extra‐articular cysts of the knee. Arthrosc Tech. 2017;6:e461–e466. 10.1016/j.eats.2016.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bombaci H, Kuyumcu M, Coskun T, Kaya E. When should the external approach be resorted to in the arthroscopic treatment of perimeniscal cyst? Sicot‐J. 2016;2:19. 10.1051/sicotj/2015046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chang JJ, Li YH, Lin GM, Wu CC, Shen HC, Pan RY. Comparison of the recurrence risk of parameniscal cysts between patients treated with arthroscopic excision and arthroscopic decompression techniques. Knee Surg, Sports Traumatol, Arthrosc. 2016;24:1547–1554. 10.1007/s00167-016-3998-0 [DOI] [PubMed] [Google Scholar]
- 18. Chernyad'ev SA, Chernookov AI, Grebenev EA, Sivkova NI, Zhilyakov AV, Babushkin DA, et al. Features of pathological changes of fibro‐cartilaginous tissue knee in patients with baker cyst. Vestn Rentgenol Radiol. 2016;97:274–282. [PubMed] [Google Scholar]
- 19. Screpis D, Piovan G, Natali S, Pasqualotto S, Magnanelli S, Iacono V, et al. The use of autologous platelet‐rich fibrin matrix combined with meniscal repair in the treatment of parameniscal cyst: clinical results and cyst recurrence after 2‐year of follow up. J Exp Orthop. 2021;8:110. 10.1186/s40634-021-00423-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. El‐Assal M, Mostafa M, Abdel‐Aal A, El‐Shafee M. Arthroscopy alone or in association with open cystectomy: in treatment of lateral meniscal cysts. Knee Surg, Sports Traumatol, Arthrosc. 2003;11:30–32. 10.1007/s00167-002-0321-z [DOI] [PubMed] [Google Scholar]
- 21. Ahn JH, Wang JH, Yoo JC, Kim SK, Park JH, Park JW. The modified outside‐in suture: vertical repair of the anterior horn of the meniscus after decompression of a large meniscal cyst. Knee Surg, Sports Traumatol, Arthrosc. 2006;14:1288–1291. 10.1007/s00167-006-0109-7 [DOI] [PubMed] [Google Scholar]
- 22. Wang P, Gao F, Sun W, Li Z, Wu X, Shi L, et al. Morphometric characteristics of the knee are associated with the injury of the meniscus. J Orthop Surg Res. 2022;17:498. 10.1186/s13018-022-03380-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pedowitz RA, Feagin JA, Rajagopalan S. A surgical algorithm for treatment of cystic degeneration of the meniscus. Arthroscopy. 1996;12:209–212. 10.1016/s0749-8063(96)90012-2 [DOI] [PubMed] [Google Scholar]
- 24. Sarimo J, Rainio P, Rantanen J, Orava S. Comparison of two procedures for meniscal cysts. A report of 35 patients with a mean follow‐up of 33 months. Am J Sports Med. 2002;30:704–707. 10.1177/03635465020300051301 [DOI] [PubMed] [Google Scholar]
- 25. Kim YM, D'Lima DD, Joo YB, Park IY. Huge intrameniscal cyst successfully treated by open debridement and combined arthroscopic and open repair: a case report. BMC Musculoskelet Disord. 2020;21:190. 10.1186/s12891-020-03218-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rocha de Faria JL et al. How to perform a Giant parameniscal cyst Exeresis: step by step technique. Arthrosc Tech. 2020;9:e669–e674. 10.1016/j.eats.2020.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Howell R, Kumar NS, Patel N, Tom J. Degenerative meniscus: pathogenesis, diagnosis, and treatment options. World J Orthop. 2014;5:597–602. 10.5312/wjo.v5.i5.597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Macmahon PJ, Brennan DD, Duke D, Forde S, Eustace SJ. Ultrasound‐guided percutaneous drainage of meniscal cysts: preliminary clinical experience. Clin Radiol. 2007;62:683–687. 10.1016/j.crad.2007.02.007 [DOI] [PubMed] [Google Scholar]
- 29. Haklar U, Ayhan E, Ustundag S, Canbora K. A new arthroscopic technique for lateral parameniscal cyst decompression. Knee. 2014;21:126–128. 10.1016/j.knee.2013.04.019 [DOI] [PubMed] [Google Scholar]
- 30. Tudisco C, Meo A, Blasucci C, Ippolito E. Arthroscopic treatment of lateral meniscal cysts using an outside‐in technique. Am J Sports Med. 2000;28:683–686. 10.1177/03635465000280051101 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data and materials are available from the medical records department of West China Hospital. The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.


