Abstract
Bone nonunion and bone defects frequently occur following high‐energy open injuries or debridement surgeries, presenting complex challenges to treatment and significantly affecting patients' quality of life. At present, there are three primary treatment options available for addressing bone nonunion and bone defects: vascularized bone grafts, the Masquelet technique, and the Ilizarov technique. The Ilizarov technique, also known as distraction osteogenesis, is widely favored by orthopedic surgeons because of several advantages, including minimal soft tissue requirements, low infection risk, and short consolidation time. However, in recent years, the application of the Masquelet technique has resulted in novel treatment methods for managing post‐traumatic bone infections when bone defects are present. Although these new techniques do not constitute a panacea, they continue to be the most commonly employed options for treating complex large bone nonunion and bone defects. This review evaluates the currently available research on the Ilizarov and Masquelet bone transport techniques applied at various anatomical sites. Additionally, it explores treatment durations and associated complications to establish a theoretical foundation that can guide clinical treatment decisions and surgical procedures for the management of bone nonunion and bone defects.
Keywords: Bone defects, Bone nonunion, Bone transport, Ilizarov technique, Masquelet technique
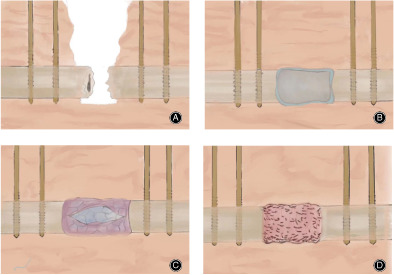
A: Thorough debridement and fixation. B: Filling with PMMA bone cement. C: 6–8 weeks after placement of PMMA bone cement, remove the bone cement and membrane induced endograft. D: Fusion of the grafted bone with the surrounding bone.
Introduction
As industrialization has accelerated, accidents involving traffic and engineering mishaps have become more frequent, resulting in increases in high‐impact injuries and limb fractures. Patients experiencing open fractures, osteomyelitis, and bone tumors are prone to severe wound infections, skin necrosis, and long‐term open wounds, increasing their susceptibility to bone defect infections and bone nonunion. 1 Both these conditions are difficult to treat due to the long treatment period required, potential complications, and often, severe episodes of infection in the bone following trauma. These events not only seriously impact patients' quality of life but also impose a heavy burden on families and society. 2 Consequently, clinicians are in urgent need of more effective methods for treating bone defects and bone nonunion in a range of scenarios.
To address these issues, the following approaches have emerged as the best options for treating infected bone and nonunion after open fractures: (i) lesion excision, gap filling, internal fixation, and bone grafting; (ii) antibiotic cement spacer and the induced membrane technique; 3 and (iii) the bone transport technique. These general approaches encompass the Ilizarov technique, the Masquelet technique, 4 , 5 the allogeneic bone grafting technique, 6 autologous bone grafting with blood vessels, 7 the application of bone morphogenetic proteins (BMPs), 8 and tissue engineering techniques. Among them, lesion excision, gap filling, internal fixation, and bone grafting constitute what has traditionally been the most widely used surgical approach for addressing infected bone defects with bone nonunion after open fractures, which improves the patient's condition by completely removing the inactivated bone and associated soft tissues. However, this set of procedures generally places more demands on the soft tissues preoperatively and is prone to postoperative infections and bone nonunion. Moreover, the efficiency of this approach is limited, and patients often require multiple procedures. As a result, the bones tend to heal slowly as medical costs continue to be incurred, and there is a greater risk of recurrent bone infections following trauma. 9
Following complete debridement of bone infections, the treatment of nonunion bone defects necessitates the application of bone transport techniques. Since their inception in the 1950s, these techniques have been refined and developed, emerging as one of the primary methods for treating post‐traumatic bone infections in conjunction with bone defects. The Ilizarov bone mobilization technique utilizes a device called the “Ilizarov external fixator,” an apparatus that employs wires and braces to gradually reposition fractured bone ends. By subjecting the bone to slow and continuous tensile stress, this method harnesses the principle of tensile stress to stimulate bone tissue regeneration. The Ilizarov technique is particularly effective in cases featuring complex deformities such as shortening and angulation, especially when accompanied by infection. 10
The Masquelet bone transport technique is a more conservative approach that utilizes an artificial membrane known as the “Masquelet membrane” to reconstruct segmental bone defects (Figure 1). This membrane stimulates the proliferation of stem cells and osteoblasts, facilitating the growth and integration of new bone. This bone transport technique is progressively gaining traction among orthopedic surgeons, as it eliminates the need for extensive soft tissue and autologous bone grafts. Furthermore, this technique can adequately control infections and concurrently repair bone and soft tissue defects. 11
FIGURE 1.
Masquelet technique diagram. (A) Thorough debridement and fixation. (B) Filling with PMMA bone cement. (C) 6–8 weeks after placement of PMMA bone cement, remove the bone cement and membrane induced endograft. (D) Fusion of the grafted bone with the surrounding bone.
To provide a reference for clinicians treating osteogenic bone defects stemming from different causes, this paper reviews the current state of domestic and international treatment strategies as well as research advancements pertaining to bone transport techniques that target osteogenic bone defects at various sites. The authors have conducted an evaluation of peer‐reviewed studies since 2018, benchmarking against clinical practice guidelines established by the American Institute for Healthcare Policy (Agency for Healthcare Research and Quality, AHRQ). The objective was to provide a treatment framework based on the most robust evidence available to inform clinical treatment decisions.
The search procedure is as follows. Source: the first author conducted a literature search in April 2023 using the keywords “bone transport; bone nonunion; bone defects; Ilizarov technique, Masquelet technique.” Literature search was conducted from 2000 to 2023 using PubMed, Web of Science, Google Scholar and FMRS, and the types of literature searched were original research articles, reviews, commentaries, case reports, meta‐analyses, etc. The amount of retrieved literature was1430 articles.
Inclusion criteria: (i) articles related to bone transport technology; (ii) articles that are important to the topic of this study but old; and (iii) similar articles were selected as close as possible to the time. Exclusion criteria: included: (i) articles with duplicated content; (ii) articles with the same type of research but without significant changes; (iii) articles with a long history.
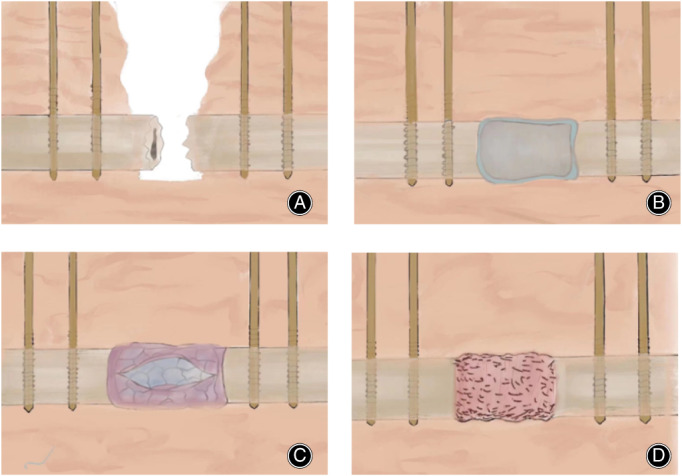
Quality assessment: a total of 1430 relevant articles were initially obtained, and the collectors assessed the validity and applicability of the included articles by reading the titles and abstracts of the articles for preliminary screening; repetitive studies and irrelevant articles were excluded, and a total of 62 articles in Chinese and English were finally included in the review, which were obtained from the databases of PubMed, Web of Science, and FMRS (Figure 2).
FIGURE 2.
Literature screening flowchart.
Bone Transport Technique in Upper Extremity Bones
Upper extremity bone discontinuities are complex and rare in clinical practice. Traditional reconstructive approaches present special challenges due to the potential for surgical infections and the formation of scar tissue, which can lead to neurovascular anatomical abnormalities, disruptions in normal skeletal anatomy, and soft tissue distortions. Though one alternative treatment adopts various microsurgical reconstruction techniques to address the bone defect with limited lengthening, 12 this procedure is plagued by a high incidence of complications and requires greater skill on the part of the performing microsurgeon.
Bone transport techniques offer an effective solution to these problems. Demir et al. 13 described an internal bone transport method for managing complex forearm bone discontinuities which allowed for axial and internal bone transport without damaging the intricate neurovascular anatomy or compromising the integrity of the soft tissue envelope. Their study encompassed five patients (mean age: 27 years) who presented with osseous nonunion of upper extremity bones (three ulna, two radius) and were successfully treated. In another study, Wu et al. 14 combined bone transport with locking plate grafting to treat ulnar osseous nonunion. Zhang et al. 1 conducted a retrospective analysis involving 16 patients with infected forearm osteochondral nonunion who were treated using bone grafting, resulting in satisfactory outcomes. Similarly, Liu et al. 11 conducted a retrospective analysis of 21 patients with infected forearm bone nonunion who underwent external fixator bone transfer post‐debridement. Liu et al. 15 also retrospectively analyzed 12 patients with infected forearm stem bone defects who underwent bone transfer surgery with a unilateral external fixator, and nearly all patients experienced favorable clinical outcomes. Zhu et al., 16 successfully healed a patient with an open high‐energy open injury using modified Masquet technology assisted personalized three‐dimensional (3D) printing of the elbow joint. The elbow joint had good motor function during follow‐up.
These examples demonstrate the efficacy of the Ilizarov segmental bone transfer technique in managing infected forearm stem bone defects. The effectiveness of this technique has also been demonstrated in the treatment of infected forearm diaphyseal defects (Table 1).
TABLE 1.
Application of Bone Transportin Upper Limb Bone
| Researchers (first author) | Numbers | Average age (years) | Bone transport site (number of cases) | Average follow‐up time (months) | Cure rate (%) |
|---|---|---|---|---|---|
| Level III Evidence | |||||
| Demir 13 | 5 | 27 | Ulna (3),radius (2) | 5.6 | 100.00 |
| Zhang 1 | 16 | 38.25 | Radius (9),ulna (7) | 39.63 | 100.00 |
| Liu 11 | 21 | 27.1 | Radius (7),ulna (12),both (2) | 77.5 | 100.00 |
| Liu 15 | 12 | 39 | Radius (10),ulna (2) | 28.2 | 100.00 |
| Zhu 16 | 1 | 31 | Elbow (1) | 15.0 | 100.00 |
Note: “–” Indicates not stated in the literature.
While the bone transport method has achieved satisfactory outcomes in treating upper extremity bone defects, additional factors such as the initial injury's severity, degree of infection, and length of the defect can all impact bone healing. Furthermore, current research relies on a limited number of studies, warranting careful consideration of its findings. The use of bone transport techniques for patients with upper extremity bone defects or nonunion remains relatively limited and necessitates further research and advancement. Future research should seek to develop more personalized and customized bone transport technology devices, particularly for patients with upper extremity bone defects and discontinuities. As biotechnology continues to advance, the development of more suitable biomaterials could enhance the application of bone transport techniques in cases involving upper extremity bone defects and osteochondral discontinuities. Despite the enormous challenges associated with treating these conditions, the application of bone transport technology in this domain holds significant promise.
Bone Transport Technique in Lower Extremity Bones
In the long, weight‐bearing bones of the lower extremities, soft tissue often fills gaps left by bone defects when the bone ends do not reach the appropriate docking site quickly enough, delaying bone healing. Bone transport techniques prove invaluable by helping to shorten the time it takes for the bone ends to connect with the defect area and enable the possibility of early bone grafting to effectively address bone nonunion issues. It should be further noted that bone defects and osteonecrosis in the lower extremities are among the most common and formidable orthopedic problems that occur at any site, with occurrences in the tibiofibular joints in particular requiring timely and effective treatment interventions.
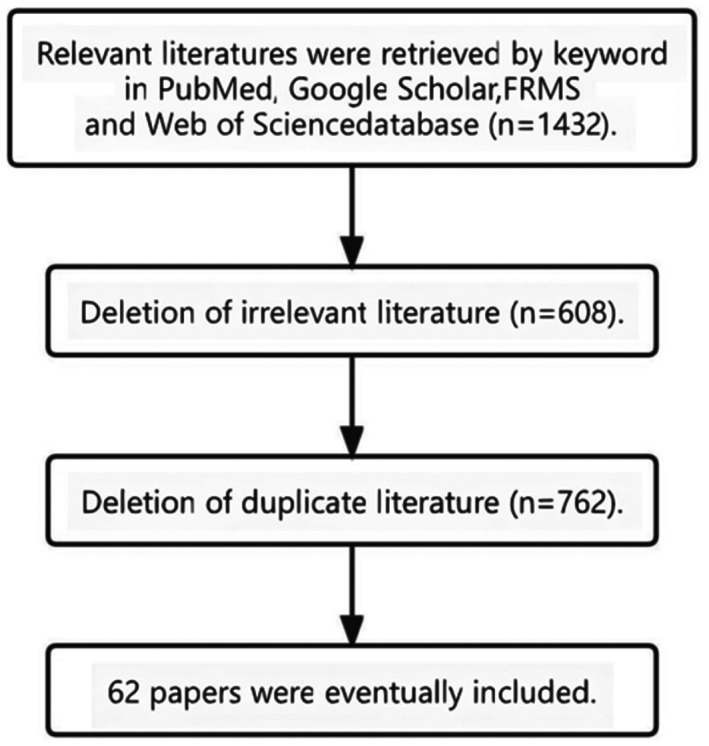
Research has demonstrated bone transport techniques' efficacy in treating lower extremity bone defects and discontinuities with favorable outcomes. As a result, these techniques have become the preferred treatment option for addressing bone defects and osteochondral nonunion in the lower extremity (Figure 3). Aktuglu et al. 17 conducted a study and functional analysis investigating cases of patients with infected or non‐infected critical‐size tibial bone defects who were treated using bone transport methods. Their analysis encompassed 27 articles exploring the treatment outcomes of 619 patients. They found a mean bone healing rate of 90.2% (range: 77%–100%), demonstrating a low rate of functional outcomes for patients with infected or non‐infected critical size tibial bone defects when treated with traditional bone transport techniques. Therefore, the Ilizarov bone transport technique offers promise as a viable alternative for addressing patients with this condition.
FIGURE 3.
Schematic diagram of Ilizarov technique for tibiofibular fracture. (A) Lower limb tibiofibular fracture with bone discontinuity. (B\C) Ilizarov external fixator stretches and positions the broken end of the bone to a predetermined position by means of wires and braces, stimulating the regenerative potential of the bone tissue by slow and continuous tensile stress. (D) New bone scab formation and tibiofibular fracture healing.
In another investigation, Sigmund et al. 18 conducted a prospective comparison between bifocal acute shortening and re‐lengthening (ASR) with bone transport technology (BT) for the reconstruction of segmental defects resulting from surgical infection resections. The study involved 47 patients, with 20 patients in the ASR group (mean bone defect size: 4.0 cm) and 27 patients in the BT group (mean bone defect size: 5.9 cm). The infection eradication rate was found to be 100% at the final follow‐ups for all patients in both groups, with similar final Association for the study and application of the method of Ilizarov (ASAMI) functional and skeletal scores. These findings confirm the effectiveness and safety of segmental resection using the Ilizarov technique for the reconstruction of infected tibial defects, which not only eliminates infection risk but also facilitates healing.
In a retrospective study by Lovisetti et al., 19 21 patients underwent BT with preservation of the ankle joint, resulting in complete fracture healing at the final follow‐up (mean follow‐up: 14.6 months). The authors concluded that the preserved ankle bone transport technique is an effective alternative to bone grafting and arthodesis for the treatment of periarticular bone nonunion at the distal tibia. Furthermore, it can be safely used in patients with infected bone nonunion near the ankle joint. Summers et al. 20 described the application of internal BT using magnetic nailing in five cases of traumatic segmental femoral bone defects (mean femoral defect size: 8.7 cm). The results showed complete consolidation in all five patients, with mean times to consolidation and index of 7.5 months and 0.8 months/cm, respectively.
In another study, Wen et al. 21 conducted a retrospective analysis involving 110 patients treated with bone transport techniques and another 110 patients treated with the antibiotic cement spacer and induced membrane technique. The results demonstrated superior clinical recovery rates and bone healing indices in the group that had undergone bone transport techniques, with significantly lower wound infection rates (7.3%) compared to the antibiotic cement spacer and induced membrane group. Their findings highlight the favorable clinical outcomes resulting from the use of bone transport techniques for treating bone defects, with clear advantages over bone grafting or the induced membrane technique alone. These advantages include shorter external fixator time, faster overall healing time, fewer complications, and improved limb function. Notably, the size of the bone defect varied among the patients included in the analysis. For example, in cases where lower extremity bone loss was between 5 and 8 cm, the required transport phase was relatively short. However, the replacement of bone transport internal fixation devices increased costs and the financial burden for patients (Table 2). Clearly, the bone transport technique is effective for reconstruction of bone at lower limb sites, addressing bone defects, promoting fracture healing, and restoring lower limb functionality.
TABLE 2.
Application of bone transport in lower extremity bones
| Researchers (first author) | Numbers | Average age (years) | Bone transport site (number of cases) | Average follow‐up time (months) | Cure rate (%) |
|---|---|---|---|---|---|
| Level I Evidence | |||||
| Wen 22 | 199 | ≥16 | – | – | – |
| Aktuglu 17 | 619 | 36.1 | Tibia | – | 72.05 |
| Level IIa Evidence | |||||
| Barawi 23 | 20 | 31.75 | Tibia | 9.6 | 100.00 |
| Sigmund 18 | 27 | Tibia | 37.9 | 100.00 | |
| Meselhy 24 | 14 | 31.64 | Tibia | 40.5 ± 6.9 | 100.00 |
| Rohilla 25 | 13 | 31.77 | Tibia | 31.62 | 75.00 |
| Atef 26 | 44 | 35.61 ± 8.57 | Ankle Joint | 37.16 ± 5.31 | 97.93 |
| Xiayimaierdan 27 | 100 | 35–65 | Tibia | 10 | 100.00 |
| Level III Evidence | |||||
| Lovisetti 19 | 21 | 48.6 | Tibia | 14.6 | 100.00 |
| Huang 28 | 84 | 19–68 | Large Sections | 29.05 ± 2.95 | 80.20 |
| Li 29 | 68 | 35.6 | Tibia | 30.8 | 76.47 |
| Wang 30 | 10 | 11–15 | Femur (7), Tibia (3) | 68.6 ± 26.6 | 90.00 |
| Summers 20 | 5 | 46.8 | Femur | 21.3 | 100.00 |
| Wen 21 | 110 | 67 ± 1.3 | Tibia | 48 | 100.00 |
| Zhang 31 | 16 | 39.1 | Tibia | 29.5 ± 1.8 | 100.00 |
| Li 32 | 26 | 40.4 | Tibia | 28.5 ± 5.8 | 100.00 |
| Biz 33 | 72 | ‐ | Tibia | 259.2 | 100.00 |
| Napora 34 | 38 | 46.8 | Femur | 98.8 | 90 |
| Solomin 35 | 1 | 55 | Tibia | 67 | 100.00 |
| Rosteius 36 | 42 | 45.5 ± 15.1 | Knee Joint | 40.8 ± 24.4 | 76.2 |
| Alshahrani 37 | 1 | 40 | Patella | – | 100.00 |
| Zhou 38 | 102 | ≥16 | Tibia (76), Femur (26) | 15.92 | 100.00 |
| Abula 39 | 14 | 35.5 | Tibia | 29.49 ± 4.34 | 100.00 |
| Ren 40 | 66 | 16–65 | Fibula | – | – |
| Bari 41 | 46 | 38.2 | Tibia | 28.5 ± 1.5 | 86.96 |
| Dumlao III 42 | 43 | 25.27 | Tibia | 37.67 | 100.00 |
| Mahran 43 | 16 | 36.5 | Tibia (14) Femur (2) | – | 87.50 |
| Song 44 | 37 | 36 | Femur | 38.4 | 65.00 |
| Liu 45 | 282 | 40 | Femur | 24 | 82.62 |
| Yin 46 | 5 | 29.2 | Fibula, Tibia | 24.8 | 100.00 |
| Yin 47 | 110 | 38.9 | Tibia (72) Femur (18) | 23.12 | 87.27 |
| Solomin 48 | 29 | 38.4 | Knee Joint | 28.83 | ‐ |
| Aktuglu 49 | 24 | 35.04 ± 17.19 | Tibia | 74.08 ± 24.17 | 96.00 |
| Xu 50 | 31 | 33.4 | Tibia | 32 | 64.00 |
| Zhang 51 | 4 | 36 | Heel bone | 14 | 100.00 |
Note: “–” Indicates not stated in the literature.
Particularly in weight‐bearing lower limbs, this approach leverages surrounding healthy bones to repair defects without the need for autologous bone grafting. It has the additional benefit of avoiding the various potential complications that arise following bone grafting procedures. Moreover, bone transport techniques involve relatively easy operations, are less invasive, and boast faster recovery times, reducing patient pain and discomfort. This enhancement of patient quality of life post‐trauma demands further research to determine which treatment options can provide the greatest benefit in lower extremity bone defect cases.
Application of Bone Transport Technology (BT) at Atypical Sites
In recent years, bone transport techniques have been widely used in the treatment of large bone nonunion and bone defects, not only in the long bones of the upper or lower extremities, but also at atypical sites, such as the femoral neck, heel bone, and sacrum. Addressing bone defects and bone nonunion at these atypical sites creates additional complexities and surgical challenges which have traditionally limited the application of bone transport techniques. However, ongoing technological advancements have allowed some researchers to employ these methods at atypical sites to positive effect.
In an experimental animal study, Hikiji et al. 52 used an internal retractor in 42 rabbits after removing the condyle and intra‐articular disc and performing an L‐shaped osteotomy from the anterior edge of the coronoid process to the posterior edge of the mandible. Microscopic observations revealed new bone and substantial cartilage within the retraction gap, as well as new bone formation at the anterior margin of the transported segment. After 8 weeks of extension completion, the mature cortical bone had regenerated, demonstrating the potential application of bone transport techniques in temporo‐mandibular joint reconstruction. In another study, Elbanoby et al. 53 reported the successful reconstruction of large post‐traumatic cranial defects in two young children via BT distraction osteogenesis, yielding satisfactory results. Furthermore, Ruben et al. 54 described the bone transport DO technique (TDO) for the treatment of mandibular defects after tumor ablation in eight patients with benign tumors, which resulted in successful mandible reconstruction through intraoral BT in all cases.
Li et al. 55 Employed an Ilizarov external fixation device for joint fusion in 72 elderly patients with traumatic ankle arthritis. X‐rays taken pre‐ and post‐surgery were used to gauge tibial inclination and to assess foot inversion/eversion. American Orthopedic Foot and Ankle Society (AOFAS) scores and visual analogue scale (VAS) scores for ankle pain were compared via paired t‐tests. Remarkably, both ankles achieved fusion at approximately 12.7 weeks (range: 11–18 weeks). This outcome indicates the promising therapeutic potential of the Ilizarov device (Table 3).
TABLE 3.
Application of bone transport in other atypical sites bones
| Researchers (first author) | Numbers | Age (years) | Bone transport site (number of cases) | Average follow‐up time (months) | Cure rate |
|---|---|---|---|---|---|
| Level IV Evidence | |||||
| Elbanoby 53 | 2 | 1.8 | Skull | 3 | Partial healing |
| Ruben 54 | 8 | 32 | Mandible | 12 | 100.00 |
| Li 55 | 72 | 65.4 | Ankle | 31.5 | 86.10 |
Note: “–” Indicates not stated in the literature.
Based on a review of the available literature, it appears that bone transport techniques hold considerable promise in addressing large bone defects with bone nonunion, especially at atypical sites, where the complexity of the injuries is substantially greater. The reconstruction of atypical sites and soft tissue defects entails increased time commitments and additional effort on the part of both the patient and surgeon. Treatment complications can include pain, surgical access issues, joint stiffness, nonunion, recurrent infections, and even the possibility of amputation. Incisional infections are another common problem, but these can be successfully treated and—if detected early enough—prevented from spreading further into the bone, where they can cause secondary damage.
In the future, the development of more personalized and customized BT devices for patients with bone defects and nonunion in atypical areas should be better for meeting the specific surgical requirements and treatment needs. Through the implementation of 3D printing technology, BT devices and orthopedic implants tailored for use at atypical sites could be designed, enhancing the application and effectiveness of BT in cases involving bone defects and discontinuities.
Furthermore, it may be possible to combine bone transport technology with other emerging technologies, such as stem cell therapy and gene editing, further improving the treatment outcomes and recovery rates of patients with bone defects at atypical sites. Rollo et al. explored the combination of teriparatide with the Ilizarov technique to treat 40 cases of bone nonunion with infections. They concluded that three to 8 months of teriparatide treatment (20 μg/day) contributed to the consolidation of long bone nonunion in these cases as well as nonunion in animal models. 56 , 57 , 58 Additionally, the researchers observed that the effectiveness of teriparatide treatment in conjunction with the Ilizarov technique in addressing septic tibial nonunion appeared to be more closely correlated with patient comorbidities than with the Ilizarov technique itself. Their analysis of clinical and radiological results further confirmed the efficacy of teriparatide as an adjunctive treatment for septic bone nonunion.
Despite the challenges inherent in treating patients with bone defects and bone nonunion at atypical sites, continuing advancements in medical technology suggest a promising future for the application of BT in this sphere. Further research and clinical practice are essential for the refinement of this technique, especially at atypical sites.
Discussion
Characteristics and Treatment of Bone Nonunion and Bone Defects
Treating bone nonunion and bone defects is recognized as the most formidable challenge facing orthopedic practitioners. Serious complications such as soft tissue sinus tract infections, limb shortening and deformities, joint stiffness, and the development of multiple drug‐resistant bacteria frequently result in amputation. While autologous free bone grafting remains the gold standard for managing small bone defects, its efficacy diminishes when confronting larger defects. Problems such as extended graft‐recipient bone healing times or the inability to heal further hinder complete bone reconstruction. Research by Jain and Sinha 59 concluded that the autologous bone grafting method alone is only suitable for bone defects smaller than 4 cm.
Allogeneic bone grafting offers an alternative for addressing bone source shortages, yet its utilization for long bone segmental bone defects is less common due to heightened risks, including postoperative immune rejection, infection, bone nonunion, and re‐fracture. These complications are further compounded when bone defects occur in the context of an acute infection or a previous history of recurrent infections. Both autologous and allogeneic bone grafts, which rely on non‐viable tissues, are susceptible to bacterial colonization that exacerbates infections in environments with inadequate blood supply. Even when an infection is largely controlled, additional difficulties arise when the wound is closed after a large bone graft. These reasons, along with recurrence of post‐operative bone resorption and infections, have led to the abandonment of free bone grafting.
Similarly, free fibula grafting with vascularisation has been proven to be effective for treating large segmental bone defects (>6 cm), but it is not only technically demanding and traumatic, it also introduces necrosis risks if vascularisation of the grafted fibula fails. Moreover, the use of vascularized free fibula grafts for lower extremity bone defects often results in stress fractures or pseudarthrosis formation due to insufficient strength, 44 necessitating prolonged brace protection to facilitate complete bone reconstruction.
In contrast, bone transport techniques have been widely adopted because of the relatively simple operation, ability to mitigate damage to soft tissues, fewer soft tissue coverage requirements, and the capacity to fill bone defects with bone blocks of matching diameters. This has led some researchers to advocate for the establishment of the technique as the standard treatment of bone defects of the tibia larger than 6 cm when an infection is present.
Advantages of Bone Transport Techniques for Treating Infected Bone Defects
During bone transport, blood supply to the bone and soft tissues increases, helping to prevent infection recurrence. Additionally, external forces can be applied during treatment, or bone formation itself can be relied upon to automatically correct angular and rotational deformities. Therefore, bone transport techniques are particularly well‐suited to patients with infected bone defects when there is deep soft tissue scarring, inadequate local blood supply, or limb deformity.
However, Khaleel and Pool 60 identified certain shortcomings associated with bone transport techniques, including extended treatment periods, persistent chronic pain, various psychological problems, nail tract infections, mobility problems (due to the bulkiness of the external fixation brace), and delayed bone healing requiring additional bone grafting procedures. Despite these drawbacks, bone transport techniques, as a limb‐saving intervention, nonetheless possess significant advantages over other methods for treating bone defects with infections.
Indications for Bone Transport Techniques
For simple traumatic bone defects less than 3 cm, bone grafting methods can be effective and are also generally used for reconstructing bone defects larger than 3 cm when they result from acute trauma. However, when bone defects are caused by infected bone nonunion, chronic osteomyelitis, or the resection of malignant tumor segments, and the presence of an infection or tumor renders the free bone grafting approach unsuitable, bone transport techniques warrant consideration as a limb‐saving intervention. Pediatric patients can also benefit from bone transport techniques, particularly for lengthening lower limbs, correcting bone deformities, and addressing skeletal dysplasia. 61
Comparison between the Ilizarov Bone Transport Technique and the Masquelet Bone Transport Technique
Prior studies have suggested that the Masquelet technique outperforms the Ilizarov technique in terms of treatment duration, complication incidence rates, operability, treatment complexity, and patient comfort. However, compared to the Ilizarov technique, the Masquelet technique also requires more soft tissue as well as additional bone grafts when there are extensive bone defects. In addition, the use of the Ilizarov external fixation frame allows patients to bear weight earlier in the recovery process, which can enhance knee and ankle functionality.
Analyzing the effect of bone grafting at different sites for the treatment of bone nonunion and bone defects revealed that the Ilizarov bone grafting technique is preferable for addressing long bone defects such as chronic bone infections, epiphyseal separation, limb lengthening, fracture healing disorders, and limb deformities in the femur, tibia, and ulna. Conversely, the Masquelet technique may be more suitable for short bone defects such as those occurring in the fingers and toes, along with bone infections and tumors. For patients with more extensive bone defects who cannot tolerate prolonged treatment and have poor compliance, the Masquelet technique should be considered; on the other hand, the Ilizarov technique may be preferred by patients seeking to bear weight earlier or who have compromised skin and soft tissue conditions, more serious infections, and fewer bone defects. In cases where a post‐traumatic bone infection emerges in conjunction with bone defects, the Masquelet technique can more reliably achieve functional recovery than the Ilizarov technique. In conclusion, personalized treatment plans based on patient‐specific conditions and defect sites should guide the adoption of one approach or the other.
In the treatment of bone nonunion and bone defects, both the Ilizarov bone transport technique and the Masquelet induced membrane technique have been shown to achieve satisfactory bone healing outcomes. However, further research is required to explore how the latter approach can be converted into a one‐stage surgery more effectively, as well as how to encourage the development of different types of induction membranes and the integration of stem cells and cytokines to enhance bone healing in bone defect and nonunion scenarios. The combination of genetic engineering and BT may one day be used to modify bone cell genes, further augmenting therapeutic efficacy. Additionally, gene therapy methods could directly regulate the treatment of bone defects and nonunion.
Automation and intelligence in the context of the Ilizarov technique are important directions for future research. The combination of the Ilizarov technique with 3D printing technologies could yield prosthetics infused with antibiotic bone cement that control infections while maintaining limb length. This approach could offer additional therapeutic benefits such as reducing complications, lowering infection recurrence rates, and minimizing external fixation device usage duration. 2 Thus, the combination of the time‐honored Ilizarov methodology and the advancing domain of digital bone science has emerged as a crucial subject guiding the evolution of Ilizarov techniques in the future.
In conclusion, despite advancing insights into the various causes of bone nonunion and bone defects, effective treatment remains challenging. Both the Masquelet and Ilizarov techniques are effective tools for achieving healing in patients with this condition. However, surgeons and patients alike must be fully aware of the extended treatment time and potential complications inherent in using these complex procedures before deciding to undertake them. If healing is not apparent after four to 6 weeks following bone transport, additional grafting at the docking site should be performed. Nevertheless, bone transport techniques hold great promise for favorable skeletal integrity and mobility outcomes in the treatment of osteogenesis imperfecta bone defects.
Conflict of Interest Statement
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author Contributions
Zhenhao Li: Conceptualization, methodology, data curation, writing—original draft, funding acquisition. Jiahe Liu: conceptualization, methodology, data curation. Chenzhi Li: investigation, formal analysis. Mingjian Wu: software, data curation. Yancheng Li: software, data curation. Yan Cui: investigation. Wanqi Xiong: investigation. Zewen Wang: investigation. Baoyi Liu: supervision, project administration, writing—review and editing. Fan Yang: supervision, project administration, writing—review and editing.
Funding Information
This work was supported by Liaoning Province “Thousand and Ten Thousand Talents Project” training Fund support (Liao People's Society Letter [2020] No.78), Postdoctoral Science Foundation of Dalian (NO. 285395), Dalian Medical Science Research Project (NO. 2111038), Dalian Dengfeng Plan Medical Key Specialty Construction Project No. 243 (2021).
Contributor Information
Fan Yang, Email: surgeon_yangfan@163.com.
Baoyi Liu, Email: liubaoyi-513@163.com.
References
- 1. Zhang Q, Yin P, Hao M, Li J, Lv H, Li T, et al. Bone transport for the treatment of infected forearm nonunion. Injury. 2014;45:1880–1884. [DOI] [PubMed] [Google Scholar]
- 2. Li J, Li M, Wang W, Li B, Liu L. Evolution and development of Ilizarov technique in the treatment of infected long bone nonunion with or without bone defects. Orthop Surg. 2022;14:824–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yang HQ, Qu L. Ilizarov bone transport technique. Zhongguo Gu Shang. 2022;10:903–907. [DOI] [PubMed] [Google Scholar]
- 4. Swiontkowski MF. Outcome in patients with an infected nonunion of the long bones treated with a reinforced antibiotic bone cement rod. J Orthop Trauma. 2012;2012:43–45. [DOI] [PubMed] [Google Scholar]
- 5. Chen P, Yang DS, Guo QJ, Zhen XZ. Clinical observation of Masquelet technique for treatment of posttraumatic osteomyelitis LING Jian‐sheng. Journal of. Clin Orthop. 2019;22(5):610–612. [Google Scholar]
- 6. Keating JF, Simpson AHRW, Robinson CM. The management of fractures with bone loss. J Bone Joint Surg Br. 2005;87‐B:142–150. [DOI] [PubMed] [Google Scholar]
- 7. Du H, Fu Q. Allogenic bone transplantation versus autologous bone grafting for repair of limb comminuted fractures: bony union and bone activity. Chinese journal of tissue engineering. Research. 2015;19(8):1206–1210. [Google Scholar]
- 8. Deng ZH, Huang Y, Xiao LL, et al. Role and application of bone morphogenetic proteins in articular cartilage regeneration. Chinese journal of tissue engineering. Research. 2021;25(5):798–806. [Google Scholar]
- 9. Müller MC, Kramer FJ, Swennen GRJ, Rahmsdorf M, Haupt C, van Griensven M, et al. A comparison of two types of free bone grafts as transport discs in segmental distraction for reconstruction of calvarial bone defects: an experimental study. Arch Orthop Trauma Surg. 2004;124:665–674. [DOI] [PubMed] [Google Scholar]
- 10. Shi J, Yang X, Song M, Zhang X, Xu Y. Clinical effects of early debridement, internal fixation, and Masquelet technique for childhood chronic haematogenous osteomyelitis of long bones. J Orthop Surg Res. 2023;18:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu T, Liu Z, Ling L, Zhang X. Infected forearm nonunion treated by bone transport after debridement. BMC Musculoskelet Disord. 2013;14:273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Thomas K, Berthold B, Günter G, Christoph H, Michael S. Outcome assessment after reconstruction of complex defects of the forearm and hand with osteocutaneous free flaps. Handchir Mikrochir P. 2007;39:388–395. [DOI] [PubMed] [Google Scholar]
- 13. Demir B, Ozkul B, Lapcin O, Beng K, Arikan Y, Yalcinkaya M. A modification of internal bone transport method for reconstruction of nonunion of forearm. Indian J Orthop. 2019;53:196–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wu C, Yuan C, Cao C, Yang H, Zou J. Bone transport combined with locking plate and bone grafting for treatment of nonunion of the ulna: a case report. Int J Clin Exp Med. 2013;6:996–1000. [PMC free article] [PubMed] [Google Scholar]
- 15. Liu Y, Yushan M, Liu Z, Liu J, Ma C, Yusufu A. Treatment of diaphyseal forearm defects caused by infection using Ilizarov segmental bone transport technique. BMC Musculoskelet Disord. 2021;22:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhu C, Zhang C, Zhao Y, Yu G, Yu L. Modified Masquelet technique assisting 3D printed elbow prosthesis for open elbow fracture with severe bone defect: a case report and technique note. Orthop Surg. 2022;14:3423–3430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Aktuglu K, Erol K, Vahabi A. Ilizarov bone transport and treatment of critical‐sized tibial bone defects: a narrative review. J Orthop Traumatol. 2019;20:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sigmund IK, Ferguson J, Govaert GAM, Stubbs D, McNally MA. Comparison of Ilizarov bifocal, acute shortening and Relengthening with bone transport in the treatment of infected, segmental defects of the tibia. J Clin Med. 2020;9:279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lovisetti G, Kirienko A, Myerson C, Vulcano E. Ankle salvage following nonunion of distal tibia fractures. Foot Ankle Int. 2018;39:1210–1218. [DOI] [PubMed] [Google Scholar]
- 20. Summers S, Krkovic M. Bone transport with magnetic intramedullary nails in long bone defects. Eur J Orthop Surg Traumatol. 2021;31:1243–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wen Y, Liu P, Wang Z, Li N. Clinical efficacy of bone transport technology in Chinese older patients with infectious bone nonunion after open tibial fracture. BMC Geriatr. 2021;21:488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wen H, Zhu S, Li C, Xu Y. Bone transport versus acute shortening for the management of infected tibial bone defects: a meta‐analysis. BMC Musculoskelet Disord. 2020;21:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Barawi O, Amen Z. Bone Transport of Tibia. Eur Sci J. 2018;14:12. [Google Scholar]
- 24. Meselhy MA, Singer MS, Halawa AM, Hosny GA, Adawy AH, Essawy OM. Gradual fibular transfer by ilizarov external fixator in post‐traumatic and post‐infection large tibial bone defects. Arch Orthop Trauma Surg. 2018;138:653–660. [DOI] [PubMed] [Google Scholar]
- 25. Rohilla R, Sharma PK, Wadhwani J, das J, Singh R, Beniwal D. Prospective randomized comparison of bone transport versus Masquelet technique in infected gap nonunion of tibia. Arch Orthop Trauma Surg. 2021;142:1923–1932. [DOI] [PubMed] [Google Scholar]
- 26. Atef A, El‐Rosasy M, El‐Tantawy A. Salvage arthrodesis for infected ankle fractures with segmental bone‐loss using Ilizarov concepts: a prospective study. Int Orthop. 2020;45:233–240. [DOI] [PubMed] [Google Scholar]
- 27. Xiayimaierdan M, Huang J, Fan C, Cai F, Aihemaitijiang Y, Xie Z. The efficiency of internal fixation with bone grafting at docking sites after bone transport for treatment of large segmental tibial bone defects. Am J Transl Res. 2021;13:5738–5745. [PMC free article] [PubMed] [Google Scholar]
- 28. Huang Q, Xu YB, Ren C, Li M, Zhang CC, Liu L, et al. Bone transport combined with bone graft and internal fixation versus simple bone transport in the treatment of large bone defects of lower limbs after trauma. BMC Musculoskelet Disord. 2022;23:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Li R, Zhu G, Chen C, Chen Y, Ren G. Bone transport for treatment of traumatic composite Tibial bone and soft tissue defects: any specific needs besides the Ilizarov technique? Biomed Res Int. 2020;2020:2716547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wang W, Yang J, Wang Y, Han G, Jia JP, Xu M, et al. Bone transport using the Ilizarov method for osteosarcoma patients with tumor resection and neoadjuvant chemotherapy. J Bone Oncol. 2019;16:100224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhang Y, Wang Y, Di J, Peng A. Double‐level bone transport for large post‐traumatic tibial bone defects: a single Centre experience of sixteen cases. Int Orthop. 2017;42:1157–1164. [DOI] [PubMed] [Google Scholar]
- 32. Li Y, Shen S, Xiao Q, Wang G, Yang H, Zhao H, et al. Efficacy comparison of double‐level and single‐level bone transport with Orthofix fixator for treatment of tibia fracture with massive bone defects. Int Orthop. 2020;44:957–963. [DOI] [PubMed] [Google Scholar]
- 33. Biz C, Crimì A, Fantoni I, Vigo M, Iacobellis C, Ruggieri P. Functional outcome and complications after treatment of comminuted tibial fractures or deformities using Ilizarov bone transport: a single‐center study at 15‐ to 30‐year follow‐up. Arch Orthop Trauma Surg. 2020;141:1825–1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Napora JK, Weinberg DS, Eagle BA, Kaufman BR, Sontich JK. Hexapod stacked transport for Tibial infected nonunions with bone loss: long‐term functional outcomes. J Orthop Trauma. 2018;32:7–e18. [DOI] [PubMed] [Google Scholar]
- 35. Solomin L, Korchagin K, Tyulkin E, Shchepkina EA. Ilizarov bone transport in large knee joint defect (case report). Open Access J Trans Med Res. 2018;2:29. [Google Scholar]
- 36. Rosteius T, Pätzholz S, Rausch V, Lotzien S, Behr B, Lehnhardt M, et al. Ilizarov bone transport using an intramedullary cable transportation system in the treatment of tibial bone defects. Injury. 2021;52:1606–1613. [DOI] [PubMed] [Google Scholar]
- 37. Alshahrani AA. Management of Neglected Patellar Tendon Rupture via the Ilizarov apparatus and patellar transport following multistage reconstruction using contralateral patella tendon bone autograft: a case study. Indian J Orthop. 2022;56:933–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zhou CH, Ren Y, Song HJ, Ali AA, Meng XQ, Xu L, et al. One‐stage debridement and bone transport versus first‐stage debridement and second‐stage bone transport for the management of lower limb post‐traumatic osteomyelitis. J Orthop Transl. 2021;28:21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Abula A, Yushan M, Ren P, Abulaiti A, Ma C, Yusufu A. Reconstruction of soft tissue defects and bone loss in the tibia by flap transfer and bone transport by distraction Osteogenesis: a case series and our experience. Ann Plast Surg. 2020;84:6–S207. [DOI] [PubMed] [Google Scholar]
- 40. Ren GH, Li R, Hu Y, Chen Y, Chen C, Yu B. Treatment options for infected bone defects in the lower extremities: free vascularized fibular graft or Ilizarov bone transport? J Orthop Surg Res. 2020;15:439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bari M, Shahidul I. Trifocal bone transport by Ilizarov technique for large post‐traumatic tibial bone defects: a single Centre BARI‐ILIZAROV experience of 46 cases MOJ Orthop. Rheumatology. 2020;12:12–14. [Google Scholar]
- 42. Dumlao P III, Balce G. Utility of ipsilateral medial fibular transport using the Ilizarov frame in the treatment for non‐elderly patients sustaining massive Tibial bone defects as a sequela of trauma and infection: A systematic review. Acta Med Philipp. 2021;55:55. [Google Scholar]
- 43. Mahran MA, Thakeb MF, El‐Motassem EHM. Bone transport for the management of severely comminuted fractures without bone loss. Strategies Trauma Limb Reconstr. 2016;11:19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Song HR, Kale A, Park HB, Koo KH, Chae DJ, Oh CW, et al. Comparison of internal bone transport and vascularized fibular grafting for femoral bone defects. J Orthop Trauma. 2003;17:203–211. [DOI] [PubMed] [Google Scholar]
- 45. Liu Y, Yushan M, Liu Z, Liu J, Ma C, Yusufu A. Complications of bone transport technique using the Ilizarov method in the lower extremity: a retrospective analysis of 282 consecutive cases over 10 years. BMC Musculoskelet Disord. 2020;21:354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yin P, Zhang L, Zhang L, Li T, Li Z, Li J, et al. Ilizarov bone transport for the treatment of fibular osteomyelitis: a report of five cases. BMC Musculoskelet Disord. 2015;16:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Yin P, Zhang L, Li T, Zhang L, Wang G, Li J, et al. Infected nonunion of tibia and femur treated by bone transport. J Orthop Surg Res. 2015;10:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Solomin LN, Shchepkina EA, Korchagin KL, Buksbaum JR, Sheridan GA, Rozbruch SR. Knee joint bone defects: reconstruction with bone transport and arthrodesis. J Arthroplasty. 2021;36:2896–2906. [DOI] [PubMed] [Google Scholar]
- 49. Aktuglu K, Günay H, Alakbarov J. Monofocal bone transport technique for bone defects greater than 5 cm in tibia: our experience in a case series of 24 patients. Injury. 2016;47:S40–S46. [DOI] [PubMed] [Google Scholar]
- 50. Xu YQ, Fan XY, He XQ, Wen HJ. Reconstruction of massive tibial bone and soft tissue defects by trifocal bone transport combined with soft tissue distraction: experience from 31 cases. BMC Musculoskelet Disord. 2021;22:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Zhang L, Lu C, Lv Y, Wang X, Guo S, Zhang H. Three‐dimensional printing‐assisted Masquelet technique in the treatment of calcaneal defects. Orthop Surg. 2021;13:876–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hikiji H, Takato T, Matsumoto S, Mori Y. Experimental study of reconstruction of the temporomandibular joint using a bone transport technique. J Oral Maxillofac Surg. 2000;58:1270–1276. [DOI] [PubMed] [Google Scholar]
- 53. Elbanoby T, Aly GM, Abdelfattah U, Choi JW, Power HA, Abd El Fattah YA. Bone transport distraction Osteogenesis in the reconstruction of pediatric posttraumatic Calvarial defects. Plast Reconstr Surg Glob Open. 2019;7:e2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ruben M, Golaszewski J, Diaz A, et al. Tetrafocal intraoral bone transport for mandibular reconstruction combined with free fibula flap and mandibular zygomatic implants. Oral Surg Oral Med Oral Radiol. 2021;131:e39. [Google Scholar]
- 55. Li J, Wang W, Yang H, Li B, Liu L. Management of Elderly Traumatic Ankle Arthritis with Ilizarov external fixation. Orthop Surg. 2022;14:2447–2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Rollo G, Luceri F, Falzarano G, Salomone C, Bonura EM, Popkov D, et al. Effectiveness of teriparatide combined with the Ilizarov technique in septic tibial non‐union. Med Glas. 2021;18:287–292. [DOI] [PubMed] [Google Scholar]
- 57. Nishitani K, Mietus Z, Beck CA, Ito H, Matsuda S, Awad HA, et al. High dose teriparatide (rPTH1‐34) therapy increases callus volume and enhances radiographic healing at 8‐weeks in a massive canine femoral allograft model. PloS One. 2017;12:e0185446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ciurlia E, Leali PT, Doria C. Use of teriparatide off‐label: our experience and review of literature. Clin Cases Miner Bone Metab. 2017;14:28–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Jain AK, Sinha S. Infected nonunion of the long bones. Clin Orthop Relat Res. 2005;431:57–65. [DOI] [PubMed] [Google Scholar]
- 60. Khaleel A, Pool R. Bone Transport. Curr Orthopaed. 2001;15:229–237. [Google Scholar]
- 61. Lei T, Zhu GG, Mei H. Efficacy of one‐stage bone transport and two‐stage wrapped bone grafting in the treatment of large bone defect after congenital tibial pseudoarthroplasty in children. J Clin Ped Sur. 2022;04 vo 21:336–340. [Google Scholar]


