Abstract
Antibiotics are known to be able to cause hypersensitivity reactions through various mechanisms. We present a case of drug-induced immune thrombocytopenia (DITP) and anaphylactic shock occurring simultaneously in a dog after the administration of two classes of antibiotics, namely trimethoprim-sulfamethoxazole (TMP-SMX) and amoxicillin-clavulanate (AMC). The patient recovered completely from DITP on discontinuation of TMP-SMX and the anaphylactic shock caused by AMC was treated with intensive care. DITP is a rare adverse drug reaction (ADR), and anaphylactic shock is a life-threatening ADR. This is the first case report of a dog manifesting two types of hypersensitivity reactions caused by two antibiotics.
Keywords: Case reports, immune thrombocytopenia, adverse drug reaction, anaphylactic shock, antibiotics
INTRODUCTION
A hypersensitivity reaction is an inappropriate and excessive immune response to an antigen or allergen resulting in undesirable effects [1,2]. There are four types of hypersensitivity reactions. Briefly, type I hypersensitivity is an immediate hypersensitivity and mediated by immunoglobulin E (IgE) and mast cells; type II hypersensitivity is called antibody-mediated cytotoxic hypersensitivity involving the formation of autoantibodies; type III hypersensitivity is accompanied by the immune complex; type IV hypersensitivity involves cellular immunity, which is caused by T lymphocytes [1,2].
Atopic diseases such as utricaria, allergic rhinitis, and atopic dermatitis, and anaphylaxis are well-known type I hypersensitivity reactions, typically mediated by IgE [1]. The fragment crystallizable region of the IgEs binds to mast cells [1]. When an allergen binds to the IgE on the surface of the mast cell, it causes the release of potent inflammatory mediators from the cytoplasmic granules present in the mast cells [1]. Thus, a type I hypersensitivity reaction occurs because of exposure to an antigen and the exaggerated response of the IgE to the antigen.
Type II hypersensitivity reaction is characterized by the formation of antibodies reacting against cellular and extracellular components [1]. There are several mechanisms for this type of hypersensitivity: anomalies of normal immunoregulation, alloimmunization, cross-reacting antibodies, and the production of autoantibodies by cancerous cells [1]. Specific type II hypersensitivity immune diseases are immune-mediated hemolytic anemia, immune-mediated thrombocytopenia (IMT), and drug-induced immune thrombocytopenia (DITP) [1,2,3].
These hypersensitivity reactions could occur with various medications [1,3], and among them, it is well-known that antibiotics cause such reactions. Amoxicillin-clavulanate (AMC) is a combination of a bactericidal aminopenicillin with a beta-lactamase inhibitor, thereby expanding the spectrum of these beta-lactam antibiotics against beta-lactamase-producing bacteria [4]. Trimethoprim-sulfamethoxazole (TMP-SMX) is a potentiated sulfonamide antimicrobial agent and owes its bactericidal properties to the inhibition of enzymes in the folic acid pathway [5].
Here, we present a case of two types of hypersensitivity reactions that occurred simultaneously in a dog, which are presumed DITP caused by the TMP-SMX and anaphylactic shock induced by the AMC.
CASE DESCRIPTION
A 9-year-old castrated male Shih-Tzu dog presented to the Veterinary Medicine Teaching Hospital with multifocal bruises and melena. The dog was treated with TMP-SMX (15 mg/kg PO twice a day for 7 days) for the soft stools at a local animal hospital. Earlier history indicated that this prescription had been made occasionally for the patient and there were complaints of lethargy, vomiting, skin flare, crusting and itching whenever the TMP-SMX was taken.
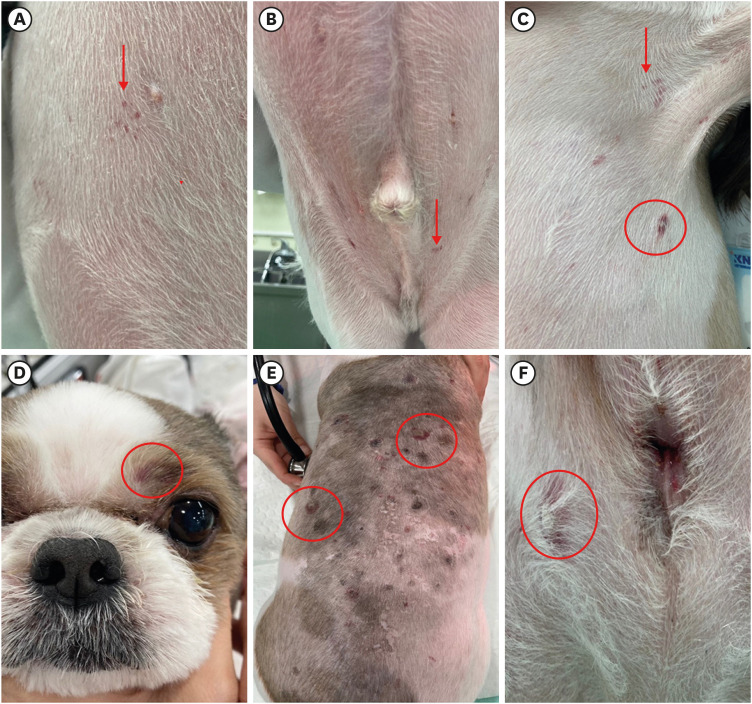
On physical examination, lethargy, multifocal petechia and ecchymosis were confirmed (Fig. 1). There were no remarkable findings in the vital signs. Blood analysis revealed severe thrombocytopenia (0 × 109/L [reference interval, 148–484] × 109/L), high C-reactive protein level (67.9 mg/L [reference interval, 0–20 mg/L]) and slightly elevated liver panels (alkaline phosphatase, 249 U/L [reference interval, 15–127 U/L]; gamma-glutamyl transferase, 11 U/L [reference interval, 0–6 U/L]) (Supplementary Table 1). Additional coagulation profile tests were performed including activated partial thromboplastin time (aPTT), prothrombin time, D-dimer level and thromboelastography (TEG) (Fig. 2A). Prolonged aPTT (112 sec [reference interval, 72–102 sec]) and hypocoagulabe state with normal levels of D-dimer (< 0.1 mg/L [reference interval, 0–0.3 mg/L]) were found (Supplementary Table 2). Hematological infection was excluded by the tick-borne polymerase chain reaction (GREEN VET, GC Holdings, Korea) analysis. There were no significant findings in the diagnostic imaging examinations.
Fig. 1. Results of physical examination. Presence of multiple petechia (red arrows) and ecchymosis (red circles) on various sites of the body were noticed.
Fig. 2. Thromboelastographic results of the patient. On arrival, the patient was in a hypocagulable state (A). A 10 days after discontinuing the TMP-SMX, the MA value returned to the normal range (B).
R, reaction time; K, K value; MA, maximum amplitude; PMA, platelet mapping assay; G, measure of clot rigidity; EPL, estimated potential lysis; A, alpha angle; CI, coagulation index; LY30, lysis at 30 min; TMP-SMX, trimethoprim-sulfamethoxazole.
Based on the results, IMT was suspected. Since the multifocal bruises and melena were observed after the patient took the TMP-SMX and given that there are some reports of DITP caused by the TMP-SMX in humans and dogs [5,6], TMP-SMX was discontinued and the patient was treated only with conservative therapy including IV fluids, a broad-spectrum antibiotics (AMC; Amocra, KUNHIL, Korea) to deal with melena and infectious disease which was not excluded at that time, and vitamin K (Alpha-K1, Cheil Bio R&D, Korea) supplementation without using immunosuppressive drugs.
A short time after the administration of intravenous AMC (13.75 mg/kg), dyspnea, systemic hypotension, bradycardia, erythema with swelling on the feet and face and a pale mucous membrane color were identified (Fig. 3A-C). To overcome this emergent situation, aggressive IV fluid therapy using Lactated Ringer’s Solution (Hartmann’s sol, JW Pharmaceutical, Korea), IV epinephrine (Epinephrine Injection, Dai Han Pharm., Korea) (0.01 mg/kg), IV chlorpheniramine (Chlorpheniramine Maleate Injection Huons, Huons, Korea) (0.4 mg/kg), and IV atropine (Atropine Sulfate Injection, Dai Han Pharm.) (0.04 mg/kg) was administered. The patient gradually recovered from the anaphylactic signs such as erythema, swelling, and systemic hypotension. (Fig. 3D-F). Soon after the patient stabilized, the antibiotic was changed to metronidazole (Flasinyl Tab., inno.N, Korea).
Fig. 3. A short time after the administration of intravenous AMC (A-C). Swelling of the face and the feet were noticed (red circles). The patient returned to normal (red arrows) after administration of IV medications (epinephrine, chlorpheniramine, and atropine) and IV fluids (D-F).
AMC, amoxicillin-clavulanate; IV, intravenous.
Ten days after discontinuing the TMP-SMX treatment, the platelet counts returned to the normal range (422 × 109/L [reference interval, 148–484] × 109/L) and normalization of the coagulation profile was confirmed by TEG (Fig. 2B). The patient recovered from the severe thrombocytopenia after discontinuation of the drug (TMP-SMX), suspected to have caused DITP, and through this, a provisional diagnosis of DITP was made and anaphylactic shock caused by AMC. Furthermore, as two types of hypersensitivity (type I and type II) occurred simultaneously, it was advised that the patient avoid sulfonamide and beta-lactam antimicrobials. The study was conducted with the consent of the caregiver.
DISCUSSION
Thrombocytopenia, a condition wherein the platelet count is lower than the reference range [7], occurs due to the decreased production, and increased destruction [7]. In IMT, there is an increase in platelet clearance due to antibody-mediated platelet destruction [7,8]. IMT can be classified as primary or secondary [7,8].
DITP is a rare adverse drug reaction, and it is considered as secondary IMT [6]. The reported incidence in human is around 10 cases per 1,000,000 persons per year [6]. However, there is very little information about DITP in dogs. The proposed mechanisms associated with this phenomenon [6,10,11] are following: hapten-dependent antibody, drug-dependent antibody (DDabs), fiban-induced thrombocytopenia, autoantibody induction, and immune complex [6,8,9]. Among these, thrombocytopenia caused by sulfonamides is known to be mediated by DDabs [6,9]. DDabs have a low affinity for platelet glycoproteins [11]. The drugs which induce DDabs production make conformational changes in the platelet glycoprotein, which is recognized by the DDabs [6] resulting in higher affinity and specificity for the target glycoprotein [11].
Diagnosing the DITP is a challenge since there could be multiple etiologies for thrombocytopenia. Newly developed severe thrombocytopenia (below 20 k/µL) inducing bleeding after 5 to 10 days of new drug administration makes DITP likely [10]. Also, if the drug is the suspected cause of DITP, then the withdrawal of the suspected drug should be considered [10]. Normalization of the platelet count after discontinuation of the drug makes the diagnosis of DITP probable. Ideally, antibodies bound to platelets in the presence of the drug should be detected by laboratory tests to make a definite diagnosis of DITP [10]. However, in veterinary medicine, these laboratory tests are limited in the practical settings. Therefore, in this case, the diagnosis of presumed DITP was made since the drug was administered just prior to the onset of severe thrombocytopenia (0 × 109/L). Also, the normalization of the coagulation profile, platelet counts, and clinical signs after discontinuation of TMP-SMX confirmed the diagnosis.
In anaphylaxis, massive and rapid release of histamine leads to vasodilation and increased vascular permeability resulting in pruritis, bronchoconstriction and cardiac depression [12]. In dogs, hypotension, bronchospasm, pruritis, erythema and, hepatic insults could occur [12]. Epinephrine is considered the most crucial drug of choice for treating anaphylaxis [12]. It acts as a vasopressor to reverse hemodynamic instability [12]. Also, fluids, antihistamines, and corticosteroids can be used as adjunctive treatment options.
Antibiotics are commonly prescribed medication in veterinary medicine. However, there is a risk of a drug hypersensitivity reaction [3]. DITP can be classified as type II hypersensitivity [1,3]. Anaphylaxis is a severe type I hypersensitivity reaction and can be life-threatening [3]. In humans, beta-lactam antibiotics are common cause of drug-induced anaphylaxis [3]. Previously reported studies found that cross-reactivity between beta-lactams antibiotics (penicillins, cephalosporins, carbapenems, and beta-lactamase inhibitors) was 40 percent, however in a recent study found that the actual cross-reactivity is less than 5 percent [13]. In this case, two types of hypersensitivity have occurred simultaneously. It is known that cross-reactivity is unlikely between sulfonamide antimicrobials and sulfonamide non-antimicrobials since there is a structural difference [14]. There are no reports of cross-reactivity between sulfonamides and beta-lactam antibiotics. However, there is a report of an increased risk of allergic reaction to penicillins in humans when there was an allergic reaction to sulfonamides [15]. In this case, two different classes of antibiotics caused type I hypersensitivity (anaphylaxis by AMC) and presumed type II hypersensitivity (DITP by TMP-SMX). Therefore, hypersensitivity reaction to certain could mean the possibility of hypersensitivity reactions to other drugs. Hence, it is necessary to be alert through cautions monitoring for hypersensitivity reactions when more than one drug is administered.
In conclusion, careful monitoring should be performed when prescribing medication known to cause hypersensitivity reactions. This is the first case report of a dog manifesting two types of hypersensitivity reaction caused by two distinct classes of antibiotics.
Footnotes
Funding: This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2020R1F1A1073007).
Conflict of Interest: The authors declare no conflicts of interest.
- Conceptualization: Ahn JO.
- Data curation: Kim YH.
- Formal analysis: Jeong Y.
- Funding acquisition: Chung JY.
- Investigation: Jeong Y.
- Methodology: Kim YH.
- Project administration: Chung JY.
- Resources: Kim YH.
- Supervision: Chung JY.
- Validation: Ahn JO.
- Visualization: Ahn JO.
- Writing - original draft: Jeong Y.
- Writing - review & editing: Ahn JO.
SUPPLEMENTARY MATERIALS
Results of blood analysis
Coagulation profile of the patient
References
- 1.Pedersen NC. A review of immunologic diseases of the dog. Vet Immunol Immunopathol. 1999;69(2-4):251–342. doi: 10.1016/S0165-2427(99)00059-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Day MJ, Schultz RD. Chapter 12: Hypersensitivity Mechanisms. 2nd ed. Boca Raton: CRC Press; 2014. Veterinary immunology: principles and practice; pp. 139–152. [Google Scholar]
- 3.Maker JH, Stroup CM, Huang V, James SF. Antibiotic hypersensitivity mechanisms. Pharmacy (Basel) 2019;7(3):122. doi: 10.3390/pharmacy7030122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plumb DC. Amoxicillin/Clavulanic Acid. 9th ed. Hoboken: John Wiley & Sons; 2018. Plumb's veterinary drug handbook: desk; pp. 91–95. [Google Scholar]
- 5.Plumb DC. Sulfamethoxazole/Trimethoprim. 9th ed. Hoboken: John Wiley & Sons; 2018. Plumb's veterinary drug handbook: desk; pp. 1529–1535. [Google Scholar]
- 6.Vayne C, Guéry EA, Rollin J, Baglo T, Petermann R, Gruel Y. Pathophysiology and diagnosis of drug-induced immune thrombocytopenia. J Clin Med. 2020;9(7):2212. doi: 10.3390/jcm9072212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scott MA, Stockham SL. Chapter 4: Platelets. 2nd ed. Hoboken: John Wiley & Sons; 2013. Fundamentals of veterinary clinical pathology; pp. 223–257. [Google Scholar]
- 8.Schifferli A, Cavalli F, Godeau B, Liebman HA, Recher M, Imbach P, et al. Understanding immune thrombocytopenia: looking out of the box. Front Med (Lausanne) 2021;8:613192. doi: 10.3389/fmed.2021.613192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trepanier LA. Idiosyncratic toxicity associated with potentiated sulfonamides in the dog. J Vet Pharmacol Ther. 2004;27(3):129–138. doi: 10.1111/j.1365-2885.2004.00576.x. [DOI] [PubMed] [Google Scholar]
- 10.Arnold DM, Nazi I, Warkentin TE, Smith JW, Toltl LJ, George JN, et al. Approach to the diagnosis and management of drug-induced immune thrombocytopenia. Transfus Med Rev. 2013;27(3):137–145. doi: 10.1016/j.tmrv.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bougie DW, Peterson J, Rasmussen M, Aster RH. Mechanism of quinine-dependent monoclonal antibody binding to platelet glycoprotein IIb/IIIa. Blood. 2015;126(18):2146–2152. doi: 10.1182/blood-2015-04-643148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shmuel DL, Cortes Y. Anaphylaxis in dogs and cats. J Vet Emerg Crit Care (San Antonio) 2013;23(4):377–394. doi: 10.1111/vec.12066. [DOI] [PubMed] [Google Scholar]
- 13.Terico AT, Gallagher JC. Beta-lactam hypersensitivity and cross-reactivity. J Pharm Pract. 2014;27(6):530–544. doi: 10.1177/0897190014546109. [DOI] [PubMed] [Google Scholar]
- 14.Khan DA, Knowles SR, Shear NH. Sulfonamide hypersensitivity: fact and fiction. J Allergy Clin Immunol Pract. 2019;7(7):2116–2123. doi: 10.1016/j.jaip.2019.05.034. [DOI] [PubMed] [Google Scholar]
- 15.Strom BL, Schinnar R, Apter AJ, Margolis DJ, Lautenbach E, Hennessy S, et al. Absence of cross-reactivity between sulfonamide antibiotics and sulfonamide nonantibiotics. N Engl J Med. 2003;349(17):1628–1635. doi: 10.1056/NEJMoa022963. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Results of blood analysis
Coagulation profile of the patient