Abstract
STUDY QUESTION
What are the knowledge, perceptions and attitudes towards fertility and elective oocyte cryopreservation (OC) for age-related fertility decline (ARFD) in women in the UK?
SUMMARY ANSWER
Awareness of OC for ARFD has reportedly improved compared to studies carried out almost a decade ago, but inconsistencies in knowledge remain regarding the rate of miscarriage amongst specific age groups, the financial costs and optimal age to undergo OC for ARFD.
WHAT IS KNOWN ALREADY
The age of first-time motherhood has increased amongst western societies, with many women of reproductive age underestimating the impact of age on fertility. Further understanding of women’s awareness of their fertility, the options available to preserve it and the barriers for seeking treatment earlier are required in order to prevent the risk of involuntary childlessness.
STUDY DESIGN, SIZE, DURATION
A hyperlink to a cross-sectional survey was posted on social media (Instagram) between 25 February 2021 and 11 March 2021.
PARTICIPANTS/MATERIALS, SETTING, METHODS
Women from the general population aged 18–50 years were invited to complete the survey.
MAIN RESULTS AND THE ROLE OF CHANCE
In total, 5482 women fulfilled the inclusion criteria and completed the survey. The mean age of participants was 35.0 years (SD 10.25; range 16–52). Three quarters (74.1%; n = 4055) disagreed or strongly disagreed they felt well informed regarding the options available to preserve their fertility, in case of a health-related problem or ARFD. The majority overestimated the risk of miscarriage in women aged ≥30 years old, with 14.5% correctly answering 20%, but underestimated the risks in women ≥40, as 20.1% correctly answered 40–50%. Three quarters (73.2%; n = 4007) reported an awareness of OC for ARFD and 65.8% (n = 3605) reported that they would consider undergoing the procedure. The number of women who considered OC for ARFD across age groups were as follows: 18–25 (8.3%; n = 300), 26–30 (35.8%; n = 1289), 31–35 (45.9%; n = 1654), 36–40 (9.6%; n = 347), 41–45 (0.3%; n = 13), and 46–50 (0.1%; n = 2). The majority of women (81.3%; n = 4443) underestimated the cost of a single cycle of OC for ARFD (<£5000). Furthermore, 10.4% (n = 566) believed a single cycle would be adequate enough to retrieve sufficient oocytes for cryopreservation. Approximately 11.0% (n = 599) believed OC for ARFD may pose significant health risks and affect future fertility. Less than half agreed or strongly agreed that the lack of awareness regarding OC for ARFD has impacted the likelihood of pursuing this method of fertility preservation further (41.4%; n = 2259).
LIMITATIONS, REASONS FOR CAUTION
Results from cross-sectional studies are limited as interpretations made are merely associations and not of causal relationships. The online nature of participant recruitment is subject to selection bias, considering women with access to social media are often from higher socioeconomic and education backgrounds, thus limiting generalizability of the findings.
WIDER IMPLICATIONS OF THE FINDINGS
Further education regarding the financial costs and optimal age to undergo elective OC to increase the chances of successful livebirth are required. Clinicians should encourage earlier fertility counselling to ensure that OC is deemed a preventative measure of ARFD, rather than an ultimate recourse to saving declining fertility.
STUDY FUNDING/COMPETING INTEREST(S)
No funding was required for this article. There are no conflicts of interests to declare.
TRIAL REGISTRATION NUMBER
N/A.
Keywords: age-related fertility decline, age-specific fertility rate, elective oocyte cryopreservation, fertility awareness, cross-sectional online survey, fertility preservation, knowledge of fertility, involuntary childlessness, reproductive aspirations, knowledge of miscarriage
Introduction
Societal evolution and advancements in gender equality have led to the transition of female gender roles worldwide. As such, amongst western societies, the trend for women to delay their childbearing years is commonly observed. This is exemplified by the age of first time motherhood increasing from 26.7 years in 1970 to 30.7 in 2019 in the UK (Statista, 2021). However, increasing age is associated with decline of ovarian reserve and atresia of oocytes, from ∼500 000 oogonia at the start of puberty to 25 000 oocytes by the age of 37 (Faddy et al., 1992). Furthermore, an exponential decrease in oocyte quality is also observed with advanced age, with associated declining pregnancy rates and reduced fecundity (Navot, 1991). Consequently, predictive models suggest should women delay conception until the age of 35 or 40 years, 14% and 34.8% would remain childless respectively (Leridon and Slama, 2008). This perhaps explains why involuntary childlessness has become more prevalent in particularly high-income countries (HICs), especially European, as more women and men delay parenthood (Nicoletti and Tanturri, 2008).
Recent developments within the field of oocyte vitrification have enabled the opportunity for women to preserve their reproductive potential, by electively cryopreserving their oocytes for future use. This is prior to the physiological decline in quality and quantity. The procedure is referred to herein, as oocyte cryopreservation (OC) for age-related fertility decline (ARFD). The process was deemed feasible, particularly when similar success rates in implantation, pregnancy, miscarriage and livebirth were observed between fresh and cryopreserved oocytes (Cobo et al., 2010; Crawford et al., 2017). Subsequently, when quantifying overall Likert responses, one study has reported that not finding a suitable partner (31%) and either the woman herself or her partner not being ready to start a family (17%), as the main indications for undergoing OC for ARFD (Jones et al., 2020).
The utilization rate of cryopreserved oocytes is between 3.1% and 12.1%, with subsequent rates of successful livebirth amongst these women between 17.5% and 30.5% (Gürtin et al., 2019; Kasaven et al., 2022). Evidently, given that live birth rates (LBRs) remain relatively low, OC for ARFD does not guarantee future successful livebirth. The process of OC for ARFD also remains limited by the loss of oocytes during thaw process, failed implantation and fertilization rates or miscarriage. This is exemplified by oocyte thaw survival rates between 80% and 90% and fertilization rates of 70–80% following intracytoplasmic sperm injection (ICSI) (Saumet et al., 2018).
Chances of successful livebirth are dependent on the age of cryopreservation and the number of oocytes retrieved. Data suggest success rates from both slow freezing and vitrification cycles decline significantly when the procedure is carried out at an age above 36 years (Cil et al., 2013). Furthermore, reproductive outcomes are far superior when OC for ARFD is performed when the patient is ≤35 years old compared to >35 (50% versus 22.9%, respectively) (Cobo et al., 2016). In women who are 35 years old, approximately 20–25 oocytes are required for an 80–85% chance of livebirth (Cobo et al., 2015). Moreover, in a woman of the same age, an average 1.2 cycles of stimulation are required to preserve at least 16 mature oocytes, for two future thaw cycles (Devine et al., 2015). Thus, considering the majority of women are currently undergoing OC for ARFD at the age of 37 (Cobo et al., 2016; Gürtin et al., 2019; Kasaven et al., 2022), the lower success rates of livebirth are unsurprising. It is imperative, therefore, that women are educated to make proactive decisions regarding their fertility. In particular, that they are encouraged to undergo OC for ARFD at an earlier age, whereby reproductive outcomes can be optimized. Although the main indication for undergoing OC is through circumstance in not finding a suitable partner, evidence also suggests that couples who have consciously delayed childbearing, on retrospect, did not feel well informed at the time of making decisions regarding their fertility (Loke et al., 2012). Furthermore, many experienced regret when prioritizing lifegoals over reproductive aspirations (Mac Dougall et al., 2013). This reflects the importance of tailoring the interventions or campaigns used to raise awareness of fertility to meet different individuals’ needs (Pedro et al., 2018).
An explanation of why women delay undergoing OC for ARFD may be related to their awareness or understanding of fertility. For example, a number of women of reproductive age underestimate the impact of age on fertility (Nouri et al., 2014), with many overestimating the success rate of livebirths through in vitro fertilisation (IVF) (Garcia et al., 2018). Women also remain unaware of the risks associated with childbearing at an advanced age (Cooke et al., 2010; Virtala et al., 2011). In a study of 257 women aged between 28 and 35 years, the majority (93%) felt moderately susceptible to the risk of infertility and 94% perceived the consequences of infertility as moderate (Ter Keurst et al., 2016). Additionally, in a study interviewing professional women, it was apparent that most had either never reflected on their own reproductive potential, or felt that by doing so it would cause unnecessary anxiety (Eriksson et al., 2013). As further evidence derived from the outcomes of OC for ARFD become available, it is important to comprehend women’s awareness of their fertility, the options available to them to preserve it, and the barriers for seeking treatment earlier. This will ensure that future reproductive outcomes can be optimized to prevent the risk of involuntary childlessness.
The objective of this study was to evaluate the general knowledge of fertility amongst women in the UK and assess their perceptions of OC for ARFD. This will identify the areas women require further knowledge and aid healthcare professionals in improving counselling, whilst encouraging informed reproductive decision-making.
Materials and methods
An online survey regarding the knowledge, attitudes, and perceptions towards fertility and OC for ARFD was advertised publicly on the social media platform Instagram, by a gynaecology U.K healthcare professional with over 70 000 followers, between 25 February 2021 and 11 March 2021. A hyperlink was shared directing participants to the survey using the platform Qualtrics (Qualtrics.com), with a brief summary and purpose of the study described in the invitation to participate. The summary reiterated that participation was exclusively voluntary with no offer of incentive to complete the survey. The inclusion criteria included women from the general population aged 18–50 years from the UK. Data from participants who did not fulfil the inclusion criteria were excluded from analysis. The survey consisted of 41 close ended questions and 2 open ended (see Supplementary Data File S1). The survey took approximately 10–12 minutes to complete and was designed for quantitative data interpretation.
The survey consisted of six categories. First, respondents answered questions regarding socio-demographic characteristics such as age, ethnicity, educational level, employment status, relationship status, and sexual orientation. This was followed by questions assessing current reproductive aspirations, including plans for future children. The third section assessed the respondent’s knowledge of fertility and the fourth the perceptions of fertility. The fifth section assessed attitudes and perceptions of OC for ARFD and the sixth, knowledge regarding the procedure. In order to prevent information bias, the process of OC for ARFD was explained after the participant completed sections of the survey pertaining to demographic information and knowledge of fertility, and prior to questions regarding knowledge, attitudes, and perceptions of OC for ARFD.
Statistical analyses
SPSS version 24 software (SPSS Inc., Armonk, NY, USA) was used for analysis of data. Descriptive statistics included mean ± SD or median ± range. Shapiro–Wilks test was performed to assess for normality.
Ethical approval
The study was reviewed and approved by the Institutional Review Board at Imperial Healthcare NHS Trust (21IC6577) on 21 January 2021. The survey was firstly peer reviewed by a team of reproductive healthcare specialists, not directly affiliated with the research and secondly trialled on healthcare professionals, with minor revisions made corresponding to the feedback provided.
Patient and public involvement
As the survey was trialled on healthcare professionals, respondents were not involved in the study design, its execution, or data analysis. Results will be communicated to respondents through the social media platform Instagram, and also via email, to those who requested the findings be shared with them.
Results
A total of 5500 women completed the survey. However, 18 were excluded from data analysis due to not fulfilling the inclusion criteria. Therefore 5482 complete surveys were analysed. The mean age of participants was 35.0 (SD 10.25, range 16–50) years old. Table 1 reports the demographic findings of participants. Table 2 summarizes the reproductive aspirations of the participants undertaking the survey. The majority (81.3%; n = 4456) of participants did not have children at the time of completing the survey. Of the women who did not already have children, 79.8% (n = 3555) wished to have a child in the future, whereas 20.2% (n = 901) did not want children and were therefore, voluntarily childless.
Table 1.
Participant demographics.
| Number (n) | % | |
|---|---|---|
| Age | ||
| <18 | 2 | 0.04 |
| 18–25 | 932 | 17.0 |
| 26–30 | 1936 | 35.3 |
| 31–35 | 1740 | 31.7 |
| 36–40 | 599 | 10.9 |
| 41–45 | 135 | 2.5 |
| 46–50 | 46 | 0.8 |
| Not answered | 92 | 1.7 |
| Ethnicity | ||
| White | 4760 | 86.9 |
| Asian | 382 | 7.0 |
| Black | 68 | 1.2 |
| Mixed | 193 | 3.5 |
| Would rather not say | 4 | 0.1 |
| Other | 73 | 1.3 |
| Not answered | 2 | 0.04 |
| Relationship status | ||
| Single | 1264 | 23.1 |
| In a relationship | 960 | 17.5 |
| Cohabiting with a partner | 1709 | 31.2 |
| Married | 1494 | 27.3 |
| Separated | 22 | 0.4 |
| Divorced | 28 | 0.5 |
| Widowed | 4 | 0.07 |
| Not answered | 1 | 0.02 |
| Sexual orientation | ||
| Heterosexual | 5076 | 92.6 |
| Lesbian | 46 | 0.8 |
| Bisexual | 295 | 5.4 |
| Other | 41 | 0.8 |
| Prefer not to say | 21 | 0.4 |
| Not answered | 3 | 0.05 |
| Education | ||
| No formal qualifications | 6 | 0.1 |
| GCSEs | 80 | 1.5 |
| A Levels | 299 | 5.5 |
| Diploma | 211 | 3.9 |
| Professional qualification | 322 | 5.9 |
| Undergraduate Degree | 2668 | 48.7 |
| Postgraduate Degree | 1710 | 31.2 |
| Doctorate | 185 | 3.4 |
| Not answered | 1 | 0.02 |
| Employment | ||
| Employed (full time) | 3953 | 72.1 |
| Employed (part time) | 514 | 9.4 |
| Self-employed | 299 | 5.5 |
| Homemaker | 113 | 2.1 |
| Student | 505 | 9.2 |
| Retired | 1 | 0.02 |
| Unemployed | 97 | 1.8 |
| Not answered | 0 | 0 |
Table 2.
Participant’s reproductive aspirations.
| Number (n) | % | |
|---|---|---|
| Do you have children? | ||
| No | 4456 | 81.3 |
| Yes | 1024 | 18.7 |
| Not answered | 2 | 0.04 |
| Do you wish to have a child in the future? | ||
| No | 398 | 7.3 |
| Yes | 4118 | 75.2 |
| Unsure | 959 | 17.5 |
| Not answered | 7 | 0.1 |
| What is your desired age to have your first child (if not yet had children)? | ||
| 20–24 | 27 | 0.5 |
| 25–29 | 680 | 12.4 |
| 30–35 | 2688 | 49.0 |
| 36–39 | 636 | 11.6 |
| 40–45 | 105 | 1.9 |
| >45 | 3 | 0.1 |
| Unsure | 247 | 4.5 |
| Not answered | 196 | 3.6 |
| What is your desired age to have your last child? | ||
| 20–24 | 1 | 0.02 |
| 25–29 | 71 | 1.3 |
| 30–35 | 1686 | 30.8 |
| 36–39 | 2425 | 44.2 |
| 40–45 | 512 | 9.3 |
| >45 | 24 | 0.4 |
| Unsure | 395 | 7.2 |
| Not answered | 368 | 6.7 |
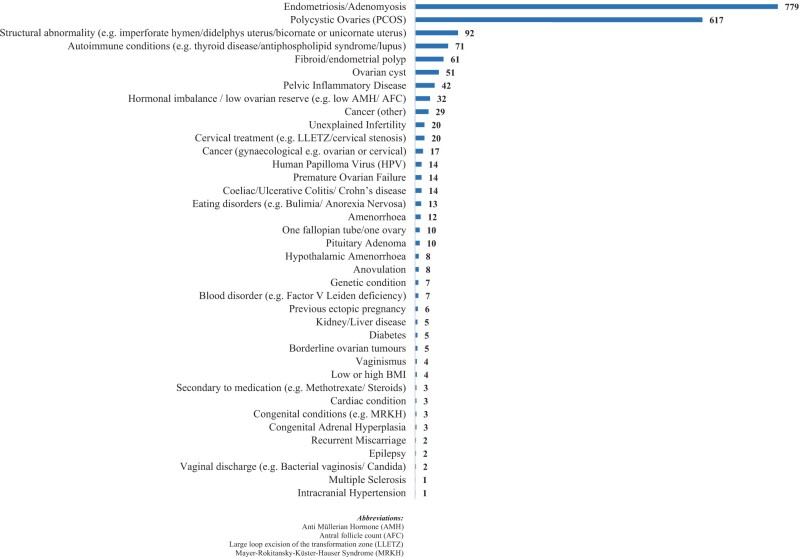
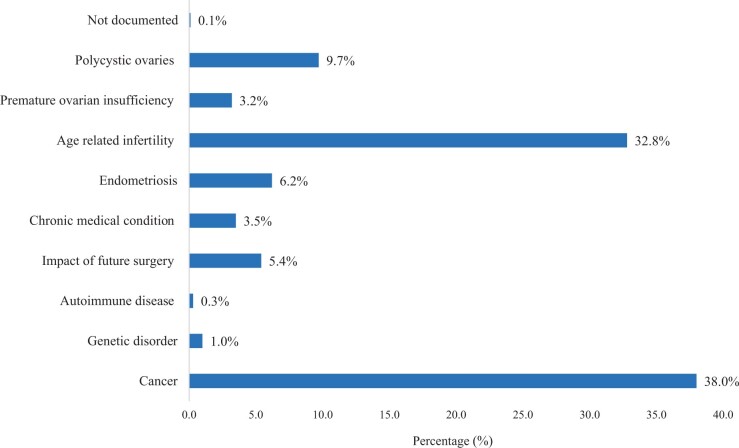
The women who perceived themselves to have a health condition which compromised their fertility accounted for 27.8% (n = 1521) of the cohort. Figure 1 lists the reported health conditions. The majority (90.5%; n = 4959) believed that having an underlying health condition would reduce the number of years they remain fertile; whilst 0.6% (n = 35) felt this was false and 8.8% (n = 484) were unsure. Figure 2 demonstrates the perceived reasons why women seek fertility preservation treatment in the UK: cancer (38%), ARFD (32.8%), and polycystic ovarian syndrome (PCOS) (9.7%).
Figure 1.
Number of women reporting health conditions perceived to affect fertility.
Figure 2.
Perceived common reasons women seek fertility preservation treatment in the UK.
Knowledge, awareness, and perceptions of fertility
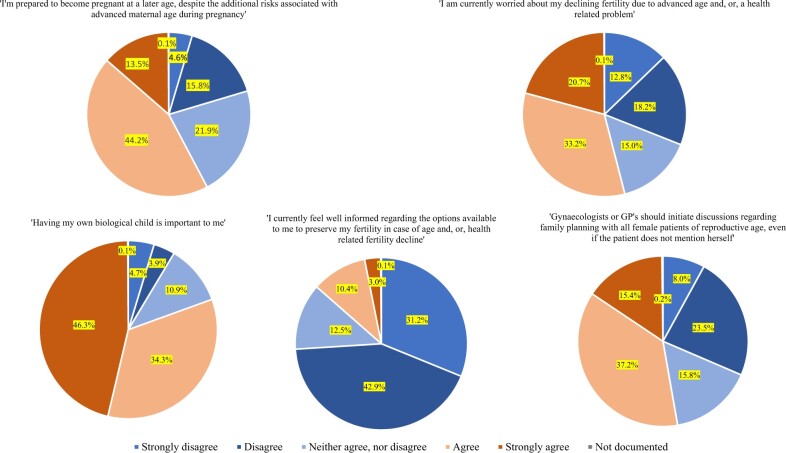
Supplementary Table S1 reports participant’s knowledge regarding various aspects of fertility, including the age of optimal fertility and percentage risk of miscarriage per age group. Table 3 summarizes this information demonstrating how many participants correctly answered each question regarding knowledge of fertility in the survey. When asked if participants were aware of the risks of high blood pressure, blood clots in the lungs and legs and risks of premature delivery associated with pregnancy at a later age, 28.7%, 22.0%, and 12.9% reported they were moderately, very and extremely aware respectively. Figure 3 summarizes women’s perceptions of fertility based on various responses to statements measured by a Likert scale. Amongst those who planned or were unsure about having children in the future, 60.4% (n = 3075/5093) agreed or strongly agreed they were prepared to become pregnant at a later age, despite the associated risks of advanced maternal age. More than half (57.4%; n = 2921/5093) agreed or strongly agreed they were worried at the time of completing the survey about their declining fertility because of advanced age or a health-related problem. The majority (82.3%; n = 4192/5093) agreed or strongly agreed that having their own biological child was important to them. Amongst the whole cohort, three-quarters (74.1%; n = 4055) disagreed or strongly disagreed they felt well informed regarding the options to preserve their fertility, in case of a health-related problem or ARFD. Just over a half (52.7%; n = 2881) agreed or strongly agreed that it is the responsibility of the gynaecologist or general practitioner to initiate discussions regarding fertility.
Table 3.
Participant’s knowledge of fertility.
| Questions | Correct n (%) | Incorrect n (%) |
|---|---|---|
| What age are women most fertile? | 1309 | 4173 |
| (15–19 years old) | (23.9%) | (76.1%) |
| At what age on average do you think a woman’s fertility begins to decline? | 1547 | 3935 |
| (35–39 years old) | (28.3%) | (71.7%) |
| What are the chances a woman of 30 years old will become pregnant after one year of unprotected sexual intercourse? | 1112 | 4370 |
| (70–80%) | (20.3%) | (79.7%) |
| What are the chances a woman of 40 years old will become pregnant after a year of unprotected sexual intercourse? | 430 | 5052 |
| (50–60%) | (7.9%) | (92.1%) |
| What are the chances of miscarriage in a woman ≥ 30 years old? | 792 | 4690 |
| (10–20%) | (14.5%) | (85.5%) |
| What are the chances of miscarriage in a woman ≥ 40 years old? | 1021 | 4461 |
| (50–60%) | (18.6%) | (81.4%) |
| From what age do you think doctors consider a pregnant woman ‘high risk’ due to advanced maternal age? | 858 | 4624 |
| (40 years old) | (15.7%) | (84.3%) |
Figure 3.
Perceptions of fertility.
Knowledge, awareness, and perceptions of OC for ARFD
Amongst the cohort, 73.2% (n = 4007) reported an awareness of social egg freezing (SEF), whereas 23.7% (n = 1298) had not heard of the procedure before and 3.2% (n = 173) were unsure. When asked if SEF should be accessible to all women on the NHS, 51.7% (n = 2827) reported yes, 19.5% (n = 1065) no, 28.9% (n = 1581) were unsure and the remaining did not answer (0.2%; n = 9).
The perception that SEF can significantly prolong a woman’s reproductive years was felt to be the case by 51.4% (n = 2809) of women, 20.1% (n = 1099) believed this was false, 28.5% (n = 1558) were unsure and 0.3% (n = 16) did not answer. The majority (97.5%; n = 5344) were aware that SEF does not guarantee pregnancy in the future.
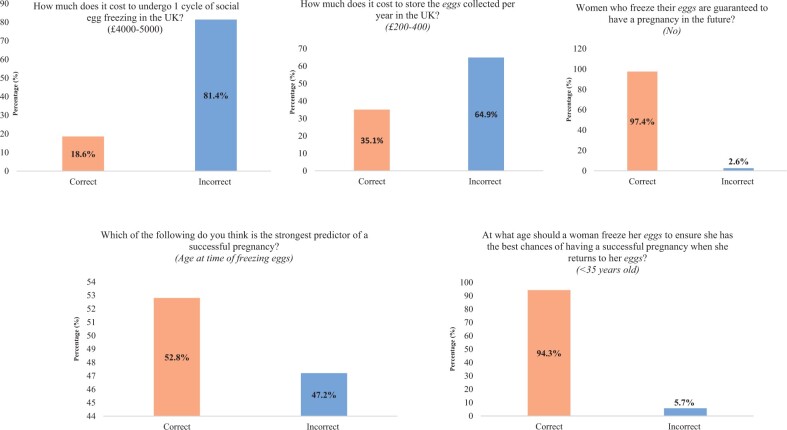
With regards to knowledge of the underlying process of SEF, 10.4% (n = 566) believed that a single cycle of ovarian stimulation would be adequate enough to retrieve sufficient oocytes for cryopreservation. Whereas 51.9% (n = 2839) believed more than one cycle is needed and 37.7% (n = 2062) were unsure, with the remaining not answering 0.3% (n = 15). Furthermore, 11.0% (n = 599) of the cohort believed that SEF may pose significant risks to the woman’s health and future fertility. Although 51.8% (n = 2834) believed this statement was not true, 37.2% (n = 2035) were unsure and 0.3% (n = 14) did not answer. Supplementary Table S2 reports participant’s knowledge regarding various aspects of OC for ARFD. Figure 4 summarizes this information demonstrating how many participants correctly answered each question regarding knowledge of OC for ARFD in the survey.
Figure 4.
Participant’s knowledge of elective oocyte cryopreservation.
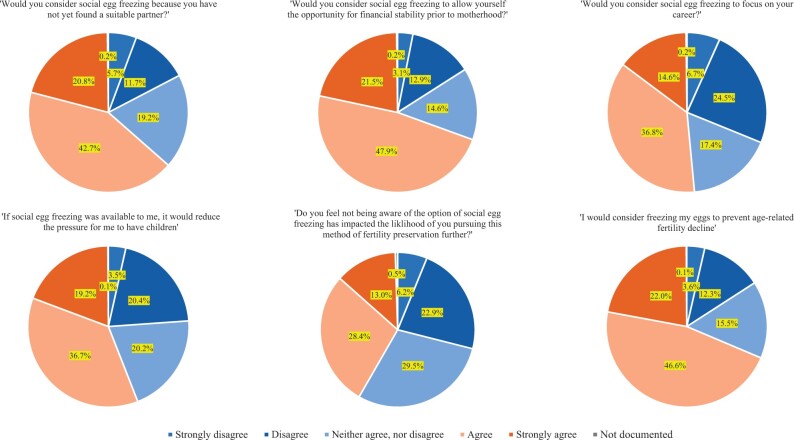
Figure 5 summarizes women’s perceptions of OC for ARFD based on various responses to statements measured by a Likert scale. Just under two thirds agreed or strongly agreed that they would consider OC for ARFD if they had not yet found a suitable partner (63.3%; n = 3469), or to allow the opportunity for financial stability prior to motherhood (69.4%; n = 3797). Just over half (51.4%; n = 2813) agreed or strongly agreed they would consider OC for ARFD to focus on their career or felt it would reduce the pressure for them to have children (55.9%; n = 3063). Over two thirds (68.6%; n = 3756) agreed or strongly agreed they would consider OC for ARFD to mitigate the risks of ARFD. Less than half agreed or strongly agreed the lack of awareness regarding OC for ARFD has impacted the likelihood of pursuing this method of fertility preservation further (41.4%; n = 2259).
Figure 5.
Perceptions of elective oocyte cryopreservation.
When asked at what age the participant would consider freezing their oocytes, 65.8% (n = 3605) of the cohort responded with the following: 8.3% (n = 300) 18–25 years old, 35.8% (n = 1289) 26–30 years old, 45.9% (n = 1654) 31–35 years old, 9.6% (n = 347) 36–40 years old, 0.3% (n = 13) 41–45 years old, and 0.1% (n = 2) 46–50 years old. The remaining did not answer (34.2%; n = 1877).
Discussion
We have presented the largest national cohort to date regarding the knowledge and attitudes towards fertility and OC for ARFD in the UK. The evidence suggests that overall awareness of ARFD has improved, as exemplified by over a third of women now recognizing this is a common reason for undergoing fertility preservation, compared to a study from more than a decade ago, whereby over half the cohort were unaware of the possibility of ARFD (Lampic et al., 2006). Previous studies have suggested that globally, women’s knowledge and awareness of fertility is considered either poor or low to moderate (Daniluk et al., 2012; Pedro et al., 2018). Our study demonstrates some improvement with participants recognizing that certain underlying gynaecological pathology such as endometriosis, PCOS, and pelvic inflammatory disease (PID) is related to infertility, as characterized by 26% of women reporting these conditions as a potential compromise to their fertility. A separate study of college and university students from England, demonstrated that only one participant from 60 was aware that Chlamydia could cause PID, and the remaining had never heard of the condition (Goundry et al., 2013). Furthermore, the overall general knowledge of why sexually transmitted infections (STIs) lead to fertility complications reported was poor (Goundry et al., 2013). A minority of women amongst our cohort however, also considered a number of benign medical conditions as incorrectly affecting their chances of conceiving, such as human papilloma virus, presence of a benign ovarian cyst or experiencing vaginal discharge. This reflects the importance of clinicians adequately counselling their patients regarding gynaecological pathology, to ensure they are not misinformed about aspects of their reproductive potential, causing unnecessary anxiety. Given that 89% of the cohort had a higher degree, it is perhaps unsurprising that awareness of fertility overall has improved, considering evidence also suggests higher fertility awareness is associated with higher education (Bunting and Boivin, 2008; Uddin and Choudhury, 2008; García et al., 2016; Pedro et al., 2018).
Our data establishes that the majority of the respondents correctly identified their most fertile years to be between the ages of 15 and 29 years. Interestingly, previous studies have suggested that women often underestimate the age at which they think fertility declines, as characterized by a study whereby 42% of participants reported this to be from the age of 40, with only 26% recognizing it to be from 35 years and above (Hammarberg et al., 2013). Considering 45.7% of women also correctly identified the age of fertility decline to be from 30 to 34 years, further emphasizes a shift towards improved knowledge. Such awareness is important, because women who underestimate the effect of age on fertility are more likely to attempt pregnancy at a later age, and consequently increase their risk of involuntary childlessness (Vassard et al., 2016).
Given the variability in answers however, there remains a lack of knowledge regarding the success rates of pregnancy amongst specific age groups. Only 20% of the cohort correctly identified the chances of successful conception following one year of unprotected sexual intercourse in a woman aged 30 as between 70% and 80%, with the majority underestimating success rates. This is inconsistent with separate studies assessing the knowledge of fertility amongst Israeli and Canadian students, whereby chances of spontaneous conception were often over-estimated across all age groups (Bretherick et al., 2010; Hashiloni-Dolev et al., 2011), which was attributed to the influence of the media, encouraging a false sense of belief and misconceptions that pregnancy at an advanced age is without risks. Furthermore, in another study, half the respondents from a cohort of 400, overestimated a young woman’s chances of becoming pregnant in one year (Svanberg et al., 2006). Amongst the women who already had children in our study, knowledge of success rates fared slightly better with 25.8% correctly answering the above question, compared to 19% amongst those who did not have children. It is possible that knowledge of fertility amongst women who do not yet have children may be worse, because they have not yet sought the information. This could be because it is not perceived to be relevant to them at their current stage of life (Bretherick et al., 2010). When asked what the chances of successful conception following one year of unprotected sexual intercourse in a woman aged 40 was, the majority were overly pessimistic in their views, as 10.5% of women who had children and 11.3% of those without, correctly answered between 53% and 55.5% (Steiner et al., 2016; Wesselink et al., 2017). This may be attributed to the fact the majority of the cohort were <40 years old and had therefore not yet attempted pregnancy beyond this age, and thus not yet aware of the success rates of pregnancy in this age group. This is consistent with a systematic review which deduced that higher levels of fertility awareness were demonstrated by women who reported difficulties conceiving, or in those who had planned their pregnancies (Pedro et al., 2018). It would be beneficial therefore, to implement educational programmes promoting the awareness of fertility on specifically women who have not yet started a family.
Our findings also suggest that as fertility awareness has improved, it is also associated with an exaggeratedly pessimistic interpretation of an older woman’s ability to conceive, as reflected by 73.9% of the overall cohort answering between 0% and 40%. Improving women’s knowledge of their chances of successful conception by age is important, as those who are pessimistic about their chances of conceiving naturally, tend to delay seeking medical help, and thus their chances of achieving a successful livebirth (Bunting and Boivin, 2007). Treatment beliefs are also associated with the likelihood of seeking health interventions sooner rather than later, as reflected by one study, where those who sought fertility treatment had a perceived high success rate and knowledge of how to get help (Bunting and Boivin, 2007). Given that treatment beliefs are dependent on the knowledge acquired, further emphasizes that fertility decision-making may be compromised if there is a lack of education or adequate access to accurate information (Okamura et al., 2002).
Participants also overestimated the risks of miscarriage in a woman aged 30 years, with only 14.5% correctly identifying this as 10–20%. Participants may have overestimated the risks, as many miscarriages occur before a woman is aware she is pregnant. Had the question specifically asked for the chances of miscarriage in this age group following ultrasound confirmation of pregnancy, may have increased the number of participants responding to the question correctly. Conversely, participants underestimated risks of miscarriage in a 40-year-old with only 18.6% reporting this correctly as 50–60%. It is possible that such findings are because women do not consider age the strongest risk factor for miscarriage (Bretherick et al., 2010). Therefore, such risks should also be reiterated to women during fertility counselling.
The transition in the awareness of fertility is perhaps unsurprising, considering the impact of social media as an easily accessible resource for health information. This differs from studies from almost a decade ago, which suggested that a woman’s healthcare provider was the preferred source of information regarding reproductive health (Hodes-Wertz et al., 2013). As our survey was completed during the COVID-19 induced lockdown in the UK, a noticeable shift towards digital medium was observed for access to healthcare information (Kaya, 2020). In a recent study, 710 fertility related social media accounts and influencers were identified, of which the fertility awareness and support groups made up 23.7% of these accounts, 59% accounted for personal stories or promotions and 20.2% accounted for accredited research and education groups (Blakemore et al., 2020). Therefore, whilst easy access to information may have contributed to overall awareness of ARFD, it is important to acknowledge that accuracy of the information pertaining to the risks of miscarriage and pregnancy rates disseminated, may be inconsistent, or worse still, incorrect. This is particularly important given that only a small number of the accounts in the aforementioned study were managed by certified reproductive specialists. It is imperative therefore, that misconceptions and incorrect information with respect to pregnancy and miscarriage rates are further addressed, with emphasis placed on directing social media users towards certified and accurate online resources.
Awareness of OC for ARFD has increased significantly over the last decade, as demonstrated by a study of 973 women, whereby 83% reported knowledge of the process (Lallemant et al., 2016). Considering that 41.1% of our cohort felt that a lack of awareness of OC for ARFD impacted the likelihood of them pursuing it further, and that 93% of women in a separate study underwent OC for ARFD at a time when they were most worried about their declining fertility (Jones et al., 2020), strongly suggests that they embark on the procedure as a last measure to save declining fertility. This is exemplified by the fact that almost half (47.2%) of the women were misinformed in believing that the age at which they return to use their cryopreserved oocytes and undergo oocyte thaw, are the strongest predictors for future successful pregnancy, as opposed to the age at cryopreservation. This is particularly important as evidence suggests women are currently undergoing the procedure too late, thus reducing their chances of successful livebirth (Cobo et al., 2016). The livebirth rate per oocyte is 3.3% (Leonel et al., 2019), when cryopreservation is carried out in women >36 years of age, compared to 8.2% per cryopreserved oocyte when performed in women <36 years old (Cil et al., 2013; Bracewell‐Milnes et al., 2018). Considering this evidence and that many women who have undergone OC for ARFD regret not doing so at an earlier age (Hodes-Wertz et al., 2013; Stoop et al., 2015), it is imperative clinicians initiate earlier discussions regarding fertility, so that plans can be made to address fecundity in the future.
Interestingly, the majority (84.5%) of women believed the best age to freeze their oocytes was between 20 and 29 years old, with significantly less expectation of successful pregnancy if performed in women ≥35 years old. It is possible members of the general public may not consider that cryopreserving oocytes too early is counterproductive, if the chances of spontaneous conception are higher and the likelihood of returning to the cryopreserved oocytes low. Hence, although evidence suggests that earlier cryopreservation is associated with improved outcomes, it is also important to factor the economic implications, given that the cost effective time to undergo the procedure is considered when they reach the age of 35 years (van Loendersloot et al., 2011). It should also be acknowledged that the prevalence of aneuploidy is often higher (40%) in younger women aged 22–23, when compared to 20–27% in those aged 26–30 years of age (Franasiak et al., 2014), and therefore undergoing OC for ARFD too early can also be associated with other risk factors.
Not having a partner has consistently remained the most common motivating factor for undergoing OC for ARFD (Baldwin, 2019), with previous studies reporting 70–88% of women undergoing the procedure for this reason (Hodes-Wertz et al., 2013; Baldwin et al., 2015; de Groot et al., 2016; Jones et al., 2021). Our own findings suggest 63% agreed or strongly agreed they would consider OC for ARFD for the same reason. This is unsurprising given the survey was completed during the peak of the pandemic, notoriously a time preventing women from meeting new people, further delaying finding a suitable partner. Although the impact of the pandemic on women’s attitudes towards their fertility is not yet well understood, it is expected that it may have motivated more women to consider reproductive planning, as fears over finding a suitable partner may have been exacerbated. OC for ARFD has previously been described as an insurance of fertility, whereby social norms and expectations that women should become mothers is reinforced (Petropanagos et al., 2015). Undergoing OC for ARFD provides an opportunity and reassurance to feel that it is possible to have both a family and career when circumstances are not yet favourable for starting a family (Cattapan et al., 2014). It is unsurprising therefore, that over half our cohort (55.9%) felt that OC for ARFD would reduce the pressure to have children. This is consistent with various studies which have demonstrated that even when women undergo OC for ARFD and do not use their oocytes, it is not associated with regret (Stoop et al., 2015; Jones et al., 2020).
The majority of women underestimated the cost of undergoing one cycle of OC in the UK, with only 18.6% correctly identifying this as between £4000 and 5000 at the time of completing the survey. Slightly more (35.1%) women recognized that the annual cost of storage of the cryopreserved oocytes would cost between £200 and 400. Financial costs often contribute to the barrier in undergoing OC for ARFD (Daniluk and Koert, 2016; Lallemant et al., 2016). Therefore, general practitioners (GPs) and Gynaecologists should be encouraged to initiate earlier, and perhaps opportunistic reproductive counselling, so that women can consider the financial costs and prioritize reproductive planning sooner. Most women, however, only visit their healthcare provider once a year (Peterson et al., 2018), or wait to seek information on fertility and conception until they are older or faced with difficulties conceiving (Lundsberg et al., 2014). Given that Gynaecologists are considered the best source of information for patients, it is important they discuss reproductive options at any opportunity.
Further preventative measures of involuntary childlessness could include the incorporation of information about ARFD in sexual health programmes delivered within secondary schools. The World Health organization (Europe) acknowledges the significance of sex education, recommending this begins in early childhood and progresses throughout life (Europe W.H.O, 2010). However, most programmes focus solely on risks of STIs and unwanted pregnancies, as opposed to understanding fertility and reproductive planning. Consequently, this promotes gaps in knowledge and awareness of fertility, as well as misconceptions, with many unable to acknowledge their reproductive goals later in life (Daniluk and Koert, 2015; Maslowski et al., 2022). It is imperative therefore, that schools aim to reconceptualize and improve the provision of fertility education.
Strengths and limitations
To our knowledge, this is the largest sample size assessing women from the general public’s awareness of fertility and OC for ARFD in the UK. Limitations of this study include the online nature of participant recruitment, which may be subject to selection bias, considering women with access to social media are often from higher socioeconomic and education backgrounds, thus limiting generalizability of the findings. This was exemplified by the fact 89% of the participants had a higher degree and 72% were employed full time. The majority of questions were also close ended, which limits further exploration of ideas and attitudes. Further studies could include in depth exploration of the themes assessed through the process of interviews, however data collection would be less efficient and more time consuming.
Conclusion
This study reports that the awareness and knowledge of ARFD and fertility are higher than previous studies carried out over a decade ago. However, women still lack knowledge regarding the miscarriage and success rates of spontaneous conception. Women in the UK have increasing awareness of OC for ARFD. However, they most likely perceive the option as a final resort to save declining fecundity, rather than an early preventative measure of ARFD. Furthermore, knowledge regarding specific aspects of the procedure are lacking, such as the financial costs and age at which OC for ARFD offers optimal chances of successful livebirths, whilst remaining a cost-effective procedure.
Supplementary Material
Contributor Information
L S Kasaven, Department of Gynaecological Oncology, Queen Charlotte’s and Chelsea Hospital, London, UK; Department of Metabolism, Digestion and Reproduction, Imperial College London, London, UK; Department of Cutrale Perioperative and Ageing Group, Imperial College London, London, UK.
A Mitra, Department of Gynaecological Oncology, Queen Charlotte’s and Chelsea Hospital, London, UK.
P Ostrysz, Department of Metabolism, Digestion and Reproduction, Imperial College London, London, UK.
E Theodorou, Department of Reproductive Medicine, Centre for Reproductive and Genetic Health, London, UK.
S Murugesu, Department of Metabolism, Digestion and Reproduction, Imperial College London, London, UK.
J Yazbek, Department of Gynaecological Oncology, Queen Charlotte’s and Chelsea Hospital, London, UK.
T Bracewell-Milnes, Department of Gynaecology and Reproductive Medicine, Lister Fertility Clinic, The Lister Hospital, London, UK.
J Ben Nagi, Department of Reproductive Medicine, Centre for Reproductive and Genetic Health, London, UK.
B P Jones, Department of Gynaecological Oncology, Queen Charlotte’s and Chelsea Hospital, London, UK.
S Saso, Department of Gynaecological Oncology, Queen Charlotte’s and Chelsea Hospital, London, UK.
Supplementary data
Supplementary data are available at Human Reproduction online.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Authors’ roles
L.S.K. drafted and revised the article for important intellectual content and carried out data interpretation. A.M., P.O., E.T., S.M., J.Y., T.B.M., and J.B.N. and revised the article for important intellectual content. B.P.J. provided substantial contribution to the analysis and interpretation of evidence and revised the manuscript critically for important intellectual content. S.S. conceived the idea of the manuscript, helped revise the article and provided final approval of the version to be published.
Funding
No funding was required for this paper.
Conflict of interest
The authors have no conflicts of interests to declare.
References
- Baldwin K. Motivations for Social Egg Freezing. Egg Freezing, Fertility and Reproductive Choice (Emerald Studies in Reproduction, Culture and Society). Bingley, UK: Emerald Publishing Limited 2019, 69–85.
- Baldwin K, Culley L, Hudson N, Mitchell H, Lavery S.. Oocyte cryopreservation for social reasons: demographic profile and disposal intentions of UK users. Reprod Biomed Online 2015;31:239–245. [DOI] [PubMed] [Google Scholar]
- Blakemore JK, Bayer AH, Smith MB, Grifo JA.. Infertility influencers: an analysis of information and influence in the fertility webspace. J Assist Reprod Genet 2020;37:1371–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bracewell‐Milnes T, Norman‐Taylor J, Nikolaou D.. Social egg freezing should be offered to single women approaching their late thirties: AGAINST: Women should be freezing their eggs earlier. BJOG 2018;125:1580–1580. [DOI] [PubMed] [Google Scholar]
- Bretherick KL, Fairbrother N, Avila L, Harbord SH, Robinson WP.. Fertility and aging: do reproductive-aged Canadian women know what they need to know? Fertil Steril 2010;93:2162–2168. [DOI] [PubMed] [Google Scholar]
- Bunting L, Boivin J.. Decision-making about seeking medical advice in an internet sample of women trying to get pregnant. Hum Reprod 2007;22:1662–1668. [DOI] [PubMed] [Google Scholar]
- Bunting L, Boivin J.. Knowledge about infertility risk factors, fertility myths and illusory benefits of healthy habits in young people. Hum Reprod 2008;23:1858–1864. [DOI] [PubMed] [Google Scholar]
- Cattapan A, Hammond K, Haw J, Tarasoff LA.. Breaking the ice: young feminist scholars of reproductive politics reflect on egg freezing. IJFAB 2014;7:236–247. [Google Scholar]
- Cil AP, Bang H, Oktay K.. Age-specific probability of live birth with oocyte cryopreservation: an individual patient data meta-analysis. Fertil Steril 2013;100:492–499.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobo A, García-Velasco JA, Coello A, Domingo J, Pellicer A, Remohí J.. Oocyte vitrification as an efficient option for elective fertility preservation. Fertil Steril 2016;105:755–764.e8. [DOI] [PubMed] [Google Scholar]
- Cobo A, Garrido N, Pellicer A, Remohí J.. Six years' experience in ovum donation using vitrified oocytes: report of cumulative outcomes, impact of storage time, and development of a predictive model for oocyte survival rate. Fertil Steril 2015;104:1426–1434.e8. [DOI] [PubMed] [Google Scholar]
- Cobo A, Meseguer M, Remohí J, Pellicer A.. Use of cryo-banked oocytes in an ovum donation programme: a prospective, randomized, controlled, clinical trial. Hum Reprod 2010;25:2239–2246. [DOI] [PubMed] [Google Scholar]
- Cooke A, Mills TA, Lavender T.. ‘Informed and uninformed decision making’—women's reasoning, experiences and perceptions with regard to advanced maternal age and delayed childbearing: a meta-synthesis. Int J Nurs Stud 2010;47:1317–1329. [DOI] [PubMed] [Google Scholar]
- Crawford S, Boulet SL, Kawwass JF, Jamieson DJ, Kissin DM.. Cryopreserved oocyte versus fresh oocyte assisted reproductive technology cycles, United States, 2013. Fertil Steril 2017;107:110–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniluk JC, Koert E.. Fertility awareness online: the efficacy of a fertility education website in increasing knowledge and changing fertility beliefs. Hum Reprod 2015;30:353–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniluk JC, Koert E.. Childless women's beliefs and knowledge about oocyte freezing for social and medical reasons. Hum Reprod 2016;31:2313–2320. [DOI] [PubMed] [Google Scholar]
- Daniluk JC, Koert E, Cheung A.. Childless women’s knowledge of fertility and assisted human reproduction: identifying the gaps. Fertil Steril 2012;97:420–426. [DOI] [PubMed] [Google Scholar]
- de Groot M, Dancet E, Repping S, Goddijn M, Stoop D, van der Veen F, Gerrits T.. Perceptions of oocyte banking from women intending to circumvent age‐related fertility decline. Acta Obstet Gynecol Scand 2016;95:1396–1401. [DOI] [PubMed] [Google Scholar]
- Devine K, Mumford SL, Goldman KN, Hodes-Wertz B, Druckenmiller S, Propst AM, Noyes N.. Baby budgeting: oocyte cryopreservation in women delaying reproduction can reduce cost per live birth. Fertil Steril 2015;103:1446–1453.e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eriksson C, Larsson M, Skoog Svanberg A, Tydén T.. Reflections on fertility and postponed parenthood—interviews with highly educated women and men without children in Sweden. Ups J Med Sci 2013;118:122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Europe W.H.O. Standards for Sexuality in Europe. A Framework for Policy Makers, Educational and Health Authorities and Specialists. Cologne: WHO Europe and Federal Centre for Health Education BZgA, 2010. http://www.oif.ac.at/fileadmin/OEIF/andere_Publikationen/WHO_BZgA_Standards.pdf (18 September 2023, date last accessed). [Google Scholar]
- Faddy M, Gosden R, Gougeon A, Richardson SJ, Nelson J.. Accelerated disappearance of ovarian follicles in mid-life: implications for forecasting menopause. Hum Reprod 1992;7:1342–1346. [DOI] [PubMed] [Google Scholar]
- Franasiak JM, Forman EJ, Hong KH, Werner MD, Upham KM, Treff NR, Scott RT.. The nature of aneuploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril 2014;101:656–663. e651. [DOI] [PubMed] [Google Scholar]
- Garcia D, Brazal S, Rodriguez A, Prat A, Vassena R.. Knowledge of age-related fertility decline in women: a systematic review. Eur J Obstet Gynecol Reprod Biol 2018;230:109–118. [DOI] [PubMed] [Google Scholar]
- García D, Vassena R, Prat A, Vernaeve V.. Increasing fertility knowledge and awareness by tailored education: a randomized controlled trial. Reprod Biomed Online 2016;32:113–120. [DOI] [PubMed] [Google Scholar]
- Goundry ALR, Finlay ER, Llewellyn CD.. Talking about links between sexually transmitted infections and infertility with college and university students from SE England, UK: a qualitative study. Reprod Health 2013;10:47–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gürtin ZB, Morgan L, O'Rourke D, Wang J, Ahuja K.. For whom the egg thaws: insights from an analysis of 10 years of frozen egg thaw data from two UK clinics, 2008-2017. J Assist Reprod Genet 2019;36:1069–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammarberg K, Setter T, Norman RJ, Holden CA, Michelmore J, Johnson L.. Knowledge about factors that influence fertility among Australians of reproductive age: a population-based survey. Fertil Steril 2013;99:502–507. [DOI] [PubMed] [Google Scholar]
- Hashiloni-Dolev Y, Kaplan A, Shkedi-Rafid S.. The fertility myth: Israeli students' knowledge regarding age-related fertility decline and late pregnancies in an era of assisted reproduction technology. Hum Reprod 2011;26:3045–3053. [DOI] [PubMed] [Google Scholar]
- Hodes-Wertz B, Druckenmiller S, Smith M, Noyes N.. What do reproductive-age women who undergo oocyte cryopreservation think about the process as a means to preserve fertility? Fertil Steril 2013;100:1343–1349.e2. [DOI] [PubMed] [Google Scholar]
- Jones BP, Kasaven L, L'Heveder A, Jalmbrant M, Green J, Makki M, Odia R, Norris G, Bracewell Milnes T, Saso S. et al. Perceptions, outcomes, and regret following social egg freezing in the UK; a cross‐sectional survey. Acta Obstet Gynecol Scand 2020;99:324–332. [DOI] [PubMed] [Google Scholar]
- Jones BP, Rajamanoharan A, Vali S, Williams NJ, Saso S, Thum MY, Ghaem-Maghami S, Quiroga I, Diaz-Garcia C, Thomas P. et al. Perceptions and motivations for uterus transplant in transgender women. JAMA Netw Open 2021;4:e2034561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasaven LS, Jones BP, Heath C, Odia R, Green J, Petrie A, Saso S, Serhal P, Nagi JB.. Reproductive outcomes from ten years of elective oocyte cryopreservation. Arch Gynecol Obstet 2022;306:1753–1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaya T. The changes in the effects of social media use of Cypriots due to COVID-19 pandemic. Technol Soc 2020;63:101380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lallemant C, Vassard D, Nyboe Andersen A, Schmidt L, Macklon N.. Medical and social egg freezing: internet‐based survey of knowledge and attitudes among women in Denmark and the UK. Acta Obstet Gynecol Scand 2016;95:1402–1410. [DOI] [PubMed] [Google Scholar]
- Lampic C, Svanberg AS, Karlström P, Tydén T.. Fertility awareness, intentions concerning childbearing, and attitudes towards parenthood among female and male academics. Hum Reprod 2006;21:558–564. [DOI] [PubMed] [Google Scholar]
- Leonel ECR, Corral A, Risco R, Camboni A, Taboga SR, Kilbride P, Vazquez M, Morris J, Dolmans MM, Amorim CA.. Stepped vitrification technique for human ovarian tissue cryopreservation. Sci Rep 2019;9:20008–20012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leridon H, Slama R.. The impact of a decline in fecundity and of pregnancy postponement on final number of children and demand for assisted reproduction technology. Hum Reprod 2008;23:1312–1319. [DOI] [PubMed] [Google Scholar]
- Loke AY, Yu PL, Hayter M.. Experiences of sub‐fertility among Chinese couples in Hong Kong: a qualitative study. J Clin Nurs 2012;21:504–512. [DOI] [PubMed] [Google Scholar]
- Lundsberg LS, Pal L, Gariepy AM, Xu X, Chu MC, Illuzzi JL.. Knowledge, attitudes, and practices regarding conception and fertility: a population-based survey among reproductive-age United States women. Fertil Steril 2014;101:767–774.e2. [DOI] [PubMed] [Google Scholar]
- Mac Dougall K, Beyene Y, Nachtigall RD.. Age shock: misperceptions of the impact of age on fertility before and after IVF in women who conceived after age 40. Hum Reprod 2013;28:350–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslowski K, Biswakarma R, Reiss MJ, Harper J.. Sex and fertility education in England: an analysis of biology curricula and students’ experiences. J Biol Educ 2022;29:1–19. [Google Scholar]
- Navot D, Bergh RA, Williams MA, Garrisi GJ, Guzman IDA, Sandler B, Grunfeld L.. Poor oocyte quality rather than implantation failure as a cause of age-related decline in female fertility. Lancet 1991;337:1375–1377. [DOI] [PubMed] [Google Scholar]
- Nicoletti C, Tanturri ML.. Differences in delaying motherhood across European countries: Empirical evidence from the ECHP. Eur J Population 2008;24:157–183. [Google Scholar]
- Nouri K, Huber D, Walch K, Promberger R, Buerkle B, Ott J, Tempfer CB.. Fertility awareness among medical and non-medical students: a case-control study. Reprod Biol Endocrinol 2014;12:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamura K, Bernstein J, Fidler AT.. Assessing the quality of infertility resources on the world wide web: tools to guide clients through the maze of fact and fiction. J Midwifery Womens Health 2002;47:264–268. [DOI] [PubMed] [Google Scholar]
- Pedro J, Brandão T, Schmidt L, Costa ME, Martins MV.. What do people know about fertility? A systematic review on fertility awareness and its associated factors. Ups J Med Sci 2018;123:71–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson B, Gordon C, Boehm JK, Inhorn M, Patrizio P.. Initiating patient discussions about oocyte cryopreservation: attitudes of obstetrics and gynaecology resident physicians. Reprod Biomed Soc Online 2018;6:72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petropanagos A, Cattapan A, Baylis F, Leader A.. Social egg freezing: risk, benefits and other considerations. CMAJ 2015;187:666–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saumet J, Petropanagos A, Buzaglo K, McMahon E, Warraich G, Mahutte N.. No. 356-egg freezing for age-related fertility decline. J Obstet Gynaecol Can 2018;40:356–368. [DOI] [PubMed] [Google Scholar]
- Statista. Population of the United Kingdom in 2020 by age. 2021. https://www.statista.com/statistics/281174/uk-population-by-age/ (18 September 2023, date last accessed).
- Steiner AZ, Jukic AM. Impact of female age and nulligravidity on fecundity in an older reproductive age cohort. Fertil Steril 2016;105:1584–1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoop D, Maes E, Polyzos NP, Verheyen G, Tournaye H, Nekkebroeck J.. Does oocyte banking for anticipated gamete exhaustion influence future relational and reproductive choices? A follow-up of bankers and non-bankers. Hum Reprod 2015;30:338–344. [DOI] [PubMed] [Google Scholar]
- Svanberg AS, Lampic C, Karlström PO, Tydén T.. Attitudes toward parenthood and awareness of fertility among postgraduate students in Sweden. Gend Med 2006;3:187–195. [DOI] [PubMed] [Google Scholar]
- Ter Keurst A, Boivin J, Gameiro S.. Women's intentions to use fertility preservation to prevent age-related fertility decline. Reprod Biomed Online 2016;32:121–131. [DOI] [PubMed] [Google Scholar]
- Uddin MJ, Choudhury AM.. Reproductive health awareness among adolescent girls in rural Bangladesh. Asia Pac J Public Health 2008;20:117–128. [DOI] [PubMed] [Google Scholar]
- van Loendersloot LL, Moolenaar LM, Mol BWJ, Repping S, van der Veen F, Goddijn M.. Expanding reproductive lifespan: a cost-effectiveness study on oocyte freezing. Hum Reprod 2011;26:3054–3060. [DOI] [PubMed] [Google Scholar]
- Vassard D, Lallemant C, Nyboe Andersen A, Macklon N, Schmidt L.. A population-based survey on family intentions and fertility awareness in women and men in the United Kingdom and Denmark. Ups J Med Sci 2016;121:244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virtala A, Vilska S, Huttunen T, Kunttu K.. Childbearing, the desire to have children, and awareness about the impact of age on female fertility among Finnish university students. Eur J Contracept Reprod Health Care 2011;16:108–115. [DOI] [PubMed] [Google Scholar]
- Wesselink AK, Rothman KJ, Hatch EE, Mikkelsen EM, Sørensen HT, Wise LA.. Age and fecundability in a North American preconception cohort study. Am J Obstet Gynecol 2017;217:667.e1–667.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.