Abstract
BACKGROUND/OBJECTIVES
This study aimed to evaluate the food sources of zinc and the usual intake of dietary zinc among Korean toddlers and preschool children.
SUBJECTS/METHODS
A total of 2,679 children aged 1–5 years was selected from the 2009–2013 Korea National Health and Nutrition Examination Survey (KNHANES) data. Dietary data collected from a single 24-h recall were used to evaluate the food sources of zinc. To estimate usual zinc intake, the distribution obtained from single 24-h recall data in the total sample was adjusted using the ratio of within-to-between-person variance in zinc intake obtained from 2-day 24-h recall sub-sample data of the 2009 KNHANES. The proportion of children with usual zinc intake below the estimated average requirement (EAR) and above the tolerable upper intake level (UL) was assessed.
RESULTS
The main sources of zinc in Korean children were grains, dairy products, and meat. The mean usual intakes of zinc among all individuals, those aged 1–2 yrs, and those aged 3–5 yrs were 5.50, 5.01, and 5.83 mg/d, respectively. In all participants, 1.1% of the children consumed zinc below the EAR, whereas 10.7% exceeded the UL. The proportion of children with excessive zinc intake was 25.6% in the 1–2 yrs age group and 0.6% in the 3–5 yrs age group.
CONCLUSIONS
According to the current UL, the risk of excessive zinc intake appears to be high among Korean toddlers. Future studies that monitor the health effects of excessive zinc intake are needed to appropriately guide zinc intake in children.
Keywords: Zinc, nutritional status, diet, child, micronutrients
INTRODUCTION
Zinc is an essential nutrient that plays a central role in child growth and development through its versatile action on nutrient metabolism, taste and smell acuity, and the hormonal mediation of bone metabolism [1]. This trace element is necessary for the immune system and reproduction and also affects the regulation of appetite and food intake [2].
The overall causes of zinc deficiency include inadequate intake, malabsorption, impaired utilization, and increased losses and requirements [3]. Infants, children, adolescents, and pregnant and lactating women are at a high risk of zinc deficiency owing to increased requirements [3]. It has been estimated that half of the world’s population is at risk for inadequate zinc intake [4]. In some countries, the proportion of young children at risk for inadequate intake remains high [5,6,7]. However, information on zinc nutrition in young Korean children is limited.
Nutrient recommendations have been established to ensure the adequate intake of essential nutrients. Dietary reference intakes (DRIs) were introduced as a new paradigm for nutrient recommendations by the Institute of Medicine in 1997 [8]. This suggests a safe and adequate nutrient intake. DRIs include four reference values, among which the estimated average requirement (EAR) and tolerable upper intake level (UL) represent evaluation criteria for inadequate intake and excessive intake with potential toxicity, respectively. Dietary evaluation of inadequacy and potential toxicity in population groups was performed by comparing usual intake to DRIs (i.e., EAR for inadequacy and UL for potential toxicity). In Korea, a nutrition survey with nationally representative samples is conducted annually. However, only one day of dietary data was collected. Thus, usual intake estimations cannot be made, and the proportion of the population at risk is not suggested appropriately.
In addition, due to the absence of a zinc nutritional database, evaluation of zinc intake has not been conducted in Korea. Recently, a zinc nutritional database was constructed from foods consumed by Korean children aged 1–5 yrs to make dietary zinc assessment of children possible [9].
This study was performed to examine zinc nutritional status and dietary sources in young Korean children using dietary intake data from a nationally representative sample of the 2009–2013 Korea National Health and Nutrition Examination Surveys (KNHANES). We estimated the usual intake distribution of zinc from food and beverage sources to evaluate dietary zinc status. Another important purpose of this study was to present reference data for better insight into the recent changes in zinc intake levels.
SUBJECTS AND METHODS
Data and study subjects
This study used cross-sectional data from the 2009–2013 KNHANES, which food list is covered by the newly developed zinc database [9]. Supplementary results were presented using data from 2016–2021 KNHANES. The KNHANES is conducted by the Korea Disease Control and Prevention Agency (KDCA) annually to assess and monitor the nutritional health status of Koreans. The survey used a stratified, multistage probability sampling design to select nationally representative samples of the non-institutionalized civilian Korean population. The KNHANES has three parts: health interviews, health examinations, and nutrition surveys. Detailed explanations of the KNHANES are described elsewhere [10].
Among participants aged 1–5 yrs (n = 2,766) in the 2009–2013 survey, those who had an implausible energy intake (< 1st or > 99th percentile of energy intake, n = 55) and those who had no information on household income (n = 32) were excluded. Thus, 2,679 children were included in the data analyses. Through the same procedure for the selection of study subjects, supplementary analyses were conducted using data from 1,351 children for the 2016–2018 data and 839 children for the 2019–2021 data. This study was conducted in accordance with the principles of the Declaration of Helsinki. This study was approved by the KDCA Institutional Review Board (IRB No. 2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C, 2013-07CON-03-4C, 2018-01-03-P-A, 2018-01-03-C-A, 2018-01-03-2C-A, and 2018-01-03-3C-A). Written informed consent was obtained from the parents or guardians of all subjects.
Assessment of zinc intake
The dietary data used in this study were collected from a single 24-h dietary recall conducted as part of the KNHANES nutrition survey. Energy and macronutrient intake for each subject were calculated using the 7th and 8th food composition tables established by the Rural Development Administration (RDA) [11,12]. The KDCA distributed zinc intake data after the survey year 2016. Zinc intake for each subject from the 2009–2013 survey data was calculated using a zinc database developed in 2021 [9]. The newly developed zinc database was established to estimate the intake levels of zinc in Korean toddlers and preschool children. It contains the zinc content of 3,361 food items commonly consumed by young Korean children [9]. Information on zinc content used to develop the zinc database in 2021 was collected from the latest RDA (9th revision) food composition tables and the United States Department of Agriculture (legacy release). For the zinc content of each food item, the collected values were primarily used (n = 1,188). Missing values were replaced with calculated values or imputed values based on the collected values of food items listed in the database. For foods with an identical name but different origins or conditions from those of the collected values, the zinc content was calculated considering the moisture content (n = 350). For foods with different names, the zinc content of a food as similar as possible based on a biological classification system was imputed according to its moisture content (n = 1,727). For mixed foods containing several food ingredients, the sum of the zinc content of each food ingredient was calculated using the food recipe (n = 62). For the 34 food items, the zinc content was assumed to be zero. Zinc intake per food group was also evaluated according to age group.
Estimation of usual zinc intake
As the KNHANES collects one-day 24-h dietary recall data for each subject, it was not possible to evaluate the usual intake of zinc. Thus, to estimate usual zinc intake among the study subjects, zinc intake obtained from single 24-h recall data was adjusted using within-person and between-person variations in zinc intake obtained from 2009 KNHANES 2-day 24-h recall data. In the 2009 KNHANES, 2-day 24-h recall data were collected from a sub-sample of the total survey participants. In the 1–5 yrs age group, a total of 167 children had 2-day 24-h recall data (n = 79 for 1–2 yrs and n = 88 for 3–5 yrs). The within-person and between-person variances in zinc intake were calculated using analysis of variance after the square root transformation of the zinc intake data [13]. The within- to between-person variance ratio in zinc intake was 0.59 for 1–2 yrs and 2.45 for 3–5 yrs.
The usual zinc intake in the study population was estimated according to the method described in a report of Nutrient Adequacy: Assessment Using Food Consumption Surveys published by the National Research Council in 1986 [13]. Adjusted (usual) zinc intake for each child was calculated using the following equations (Equations 1–3) [13,14] with the ratio of within- (Sw2) to between-person variance (Sb2) of zinc intake obtained from 2-day 24-h recall data of the 2009 KNHANES. The distribution of zinc intake was also skewed. Thus, zinc intake values were transformed using the natural logarithm (ln). The KDCA began to provide zinc intake data in 2023 for KNHANES years after 2016. The same ratio and procedures were applied to calculate the usual zinc intake in the supplementary analysis using 2016–2021 KNHANES data.
| (1) |
| (2) |
| (3) |
To evaluate usual zinc intake based on recommended levels, the EAR and UL values suggested in the 2020 DRIs for Koreans were used [15]. The EAR was 2 mg/d for children aged 1–2 yrs and 3 mg/d for children aged 3–5 yrs. The UL was 6 mg/d for children aged 1–2 yrs and 9 mg/d for children aged 3–5 yrs. The proportions of children with intake below the EAR and those with intake above the UL were calculated.
Systematic review of the ratio of within-to-between-person variance in zinc intake among young children
The variance data of Korean children were compared to those of foreign children of similar ages. Information on the ratio of within-to-between-person variance of zinc intake among young children was identified by searching for published articles in the PubMed database through June 2022. The following keywords were used for the primary literature search: (zinc or mineral or micronutrient or minerals or micronutrients in the title or abstract) and (children in title or abstract) and (intake or intakes in title or abstract) and (variation or variance or variability in title or abstract). An additional literature search through the PubMed database was conducted with the following keywords to identify relevant articles precisely: (usual in the title or abstract) and (intake or intakes in title or abstract) and (micronutrient or micronutrients or mineral or minerals or zinc in title or abstract) and (children in title or abstract). The references were screened from the retrieved articles. Two authors independently assessed the eligibility of the study based on the following selection criteria: 1) articles published in English or Korean; 2) articles included eligible age groups of participants; and 3) articles containing appropriate information on the ratio of within-to-between-person variance of zinc intake. The following information was extracted from the selected articles: 1) the first author’s name and publication year; 2) country in which the study was performed and number of study subjects; 3) data and study period; 4) dietary assessment methods; 5) study subjects’ age and gender; 6) ratio of within-to-between-person variance of zinc intake; and 7) intake levels of energy, protein, and zinc.
Statistical analyses
All statistical analyses were performed using the Statistical Analysis Systems (SAS), version 9.4 (SAS Institute, Cary, NC, USA). All data analyses conducted in this study considered the complex sampling design effect and used appropriate sampling weights. Dietary zinc intake per food group calculated based on one-day 24-h dietary recall data is presented as the mean, SE, 95% confidence limit (CL) for the mean, and 1st, 5th, 10th, 25th, 50th, 75th, 90th, 95th, and 99th percentiles. Adjusted (usual) zinc intake is presented as the mean and SE with 95% CL by children’s age group, gender, living area, and household income. For the distribution of adjusted (usual) zinc intake, 1st, 5th, 10th, 25th, 50th, 75th, 90th, 95th and 99th percentiles are also presented. The proportion of children who had usual dietary zinc intake below the EAR and above the UL was estimated, and differences in proportions by children’s age group, gender, living area, and household income were tested using the χ2 test. Statistical significance was set at α = 0.05.
RESULTS
Characteristics of study subjects
The characteristics of the study participants are listed in Table 1. Among the study subjects aged 1–5 yrs, the mean age was 3.0 years (SE = 0.03). Approximately 52% of the children were boys. About 83% of the children lived in urban areas, and 8.8% of the study subjects lived in low-income households. The average energy intake level was 1,203 kcal (SE = 10.4) in this study population. Macronutrient intake level was 192.2 g (SE = 1.7) for carbohydrate, 41.2 g (SE = 0.4) for protein and 30.1 g (SE = 0.4) for fat.
Table 1. Characteristics of study subjects (n = 2,679)1).
| Variables | Values | |
|---|---|---|
| Age group | ||
| 1–2 yrs | 40.4 | |
| 3–5 yrs | 59.6 | |
| Gender | ||
| Boys | 51.8 | |
| Girls | 48.2 | |
| Age group × Gender | ||
| 1–2 yrs, boys | 21.7 | |
| 1–2 yrs, girls | 18.8 | |
| 3–5 yrs, boys | 30.1 | |
| 3–5 yrs, girls | 29.4 | |
| Living area | ||
| Urban | 83.3 | |
| Rural | 16.7 | |
| Household income | ||
| Low | 8.8 | |
| Medium-low | 34.4 | |
| Medium-high | 33.3 | |
| High | 23.5 | |
| Energy and nutrient intake | ||
| Total energy (kcal) | 1,203 ± 10.4 | |
| Carbohydrate (g) | 192.2 ± 1.7 | |
| Protein (g) | 41.2 ± 0.4 | |
| Fat (g) | 30.1 ± 0.4 | |
Values are presented as % frequency or mean ± SE.
1)All analyses accounted for the complex sampling design effect and appropriate sampling weights.
Evaluation of zinc intake and its food sources
The dietary zinc intake per food group is shown in Table 2. Among all study subjects, about 2.2 mg of zinc intake came from grains and their products, with the remainder coming from milk and dairy products (1.1 mg), meat and its products (0.8 mg), eggs, vegetables, fish and shellfish and legumes and its products. By age group, young children had higher zinc intake from milk and dairy products but lower intakes from meat and grains and their products compared to older children. Recent 6 yrs data for the dietary zinc intake per food group is presented in Supplementary Table 1.
Table 2. Dietary zinc intake per food group by age group1),2) .
| Food group | Food group intake (g) | Zinc intake per food group (mg) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Mean ± SE | 95% CL | P1 | P5 | P10 | P25 | P50 | P75 | P90 | P95 | P99 | ||
| Total subjects (n = 2,679) | |||||||||||||
| Grains and its products | 182.0 | 2.22 ± 0.03 | 2.16–2.28 | 0.25 | 0.66 | 0.95 | 1.44 | 2.04 | 2.87 | 3.77 | 4.31 | 5.47 | |
| Potatoes and starch-rich foods | 22.3 | 0.07 ± 0.00 | 0.06–0.08 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.08 | 0.20 | 0.36 | 0.74 | |
| Sugar and sweets | 5.4 | 0.02 ± 0.00 | 0.02–0.03 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.03 | 0.09 | 0.43 | |
| Legumes and its products | 29.8 | 0.22 ± 0.01 | 0.20–0.24 | 0.00 | 0.00 | 0.00 | 0.00 | 0.08 | 0.28 | 0.60 | 0.86 | 1.89 | |
| Nuts and seeds | 1.8 | 0.04 ± 0.00 | 0.04–0.05 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.03 | 0.09 | 0.23 | 0.69 | |
| Vegetables | 76.7 | 0.29 ± 0.01 | 0.27–0.32 | 0.00 | 0.01 | 0.03 | 0.09 | 0.22 | 0.39 | 0.60 | 0.81 | 1.36 | |
| Mushrooms | 2.8 | 0.03 ± 0.00 | 0.02–0.03 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.06 | 0.13 | 0.40 | |
| Fruits | 162.2 | 0.16 ± 0.01 | 0.15–0.17 | 0.00 | 0.00 | 0.00 | 0.00 | 0.08 | 0.21 | 0.41 | 0.58 | 1.15 | |
| Meat and its products | 41.0 | 0.84 ± 0.03 | 0.79–0.89 | 0.00 | 0.00 | 0.00 | 0.10 | 0.51 | 1.20 | 2.18 | 2.90 | 4.69 | |
| Eggs | 23.7 | 0.31 ± 0.01 | 0.29–0.34 | 0.00 | 0.00 | 0.00 | 0.00 | 0.10 | 0.46 | 0.91 | 1.18 | 2.01 | |
| Fish and shellfish | 19.7 | 0.26 ± 0.02 | 0.21–0.30 | 0.00 | 0.00 | 0.00 | 0.02 | 0.10 | 0.26 | 0.56 | 0.87 | 1.96 | |
| Seaweeds | 3.6 | 0.04 ± 0.00 | 0.04–0.05 | 0.00 | 0.00 | 0.00 | 0.00 | 0.02 | 0.06 | 0.11 | 0.17 | 0.34 | |
| Milk and dairy products | 264.2 | 1.11 ± 0.03 | 1.04–1.17 | 0.00 | 0.00 | 0.00 | 0.45 | 0.84 | 1.48 | 2.18 | 2.80 | 5.26 | |
| Oils and fats | 3.4 | 0.00 ± 0.00 | 0.00–0.01 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.02 | 0.04 | |
| Beverages and alcohol | 28.1 | 0.04 ± 0.00 | 0.03–0.05 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.08 | 0.22 | 0.67 | |
| Seasonings | 11.7 | 0.08 ± 0.00 | 0.07–0.08 | 0.00 | 0.00 | 0.00 | 0.01 | 0.04 | 0.10 | 0.18 | 0.26 | 0.54 | |
| Processed foods | 0.8 | 0.01 ± 0.00 | 0.00–0.01 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.19 | |
| Total intake | 5.75 ± 0.06 | 5.63–5.87 | 1.60 | 2.56 | 3.05 | 4.10 | 5.41 | 7.02 | 8.73 | 9.92 | 12.01 | ||
| 1–2 yrs (n = 1,097) | |||||||||||||
| Grains and its products | 152.6 | 1.86 ± 0.04 | 1.78–1.95 | 0.07 | 0.44 | 0.69 | 1.17 | 1.67 | 2.43 | 3.22 | 3.87 | 4.84 | |
| Potatoes and starch-rich foods | 20.5 | 0.06 ± 0.01 | 0.05–0.07 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.07 | 0.19 | 0.32 | 0.64 | |
| Sugar and sweets | 3.9 | 0.02 ± 0.00 | 0.01–0.02 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.03 | 0.06 | 0.35 | |
| Legumes and its products | 39.8 | 0.22 ± 0.01 | 0.19–0.24 | 0.00 | 0.00 | 0.00 | 0.00 | 0.07 | 0.28 | 0.61 | 0.86 | 1.93 | |
| Nuts and seeds | 1.6 | 0.03 ± 0.00 | 0.03–0.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.06 | 0.14 | 0.61 | |
| Vegetables | 55.8 | 0.20 ± 0.01 | 0.19–0.22 | 0.00 | 0.00 | 0.01 | 0.05 | 0.14 | 0.28 | 0.45 | 0.58 | 1.05 | |
| Mushrooms | 2.4 | 0.02 ± 0.00 | 0.02–0.03 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.05 | 0.11 | 0.37 | |
| Fruits | 150.0 | 0.16 ± 0.01 | 0.14–0.17 | 0.00 | 0.00 | 0.00 | 0.00 | 0.08 | 0.21 | 0.39 | 0.56 | 0.99 | |
| Meat and its products | 30.2 | 0.63 ± 0.03 | 0.57–0.70 | 0.00 | 0.00 | 0.00 | 0.01 | 0.32 | 0.87 | 1.76 | 2.53 | 3.56 | |
| Eggs | 20.9 | 0.28 ± 0.02 | 0.24–0.31 | 0.00 | 0.00 | 0.00 | 0.00 | 0.06 | 0.40 | 0.81 | 1.07 | 1.71 | |
| Fish and shellfish | 15.7 | 0.21 ± 0.02 | 0.17–0.25 | 0.00 | 0.00 | 0.00 | 0.00 | 0.07 | 0.20 | 0.51 | 0.76 | 1.78 | |
| Seaweeds | 2.8 | 0.04 ± 0.00 | 0.03–0.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.05 | 0.09 | 0.14 | 0.30 | |
| Milk and dairy products | 273.2 | 1.37 ± 0.06 | 1.25–1.49 | 0.00 | 0.00 | 0.00 | 0.54 | 1.03 | 1.82 | 2.71 | 3.72 | 6.86 | |
| Oils and fats | 2.5 | 0.00 ± 0.00 | 0.00–0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.03 | |
| Beverages and alcohol | 20.2 | 0.03 ± 0.01 | 0.01–0.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.03 | 0.11 | 0.48 | |
| Seasonings | 7.4 | 0.05 ± 0.00 | 0.04–0.05 | 0.00 | 0.00 | 0.00 | 0.01 | 0.02 | 0.07 | 0.12 | 0.18 | 0.38 | |
| Processed foods | 0.5 | 0.00 ± 0.00 | 0.00–0.01 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.07 | |
| Total intake | 5.18 ± 0.09 | 5.01–5.35 | 1.44 | 2.34 | 2.76 | 3.59 | 4.91 | 6.41 | 7.86 | 8.78 | 11.48 | ||
| 3–5 yrs (n = 1,582) | |||||||||||||
| Grains and its products | 202.0 | 2.46 ± 0.03 | 2.39–2.53 | 0.47 | 0.93 | 1.22 | 1.69 | 2.25 | 3.06 | 4.00 | 4.55 | 5.93 | |
| Potatoes and starch-rich foods | 23.5 | 0.07 ± 0.01 | 0.06–0.08 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.08 | 0.20 | 0.37 | 0.81 | |
| Sugar and sweets | 6.5 | 0.03 ± 0.00 | 0.02–0.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.04 | 0.10 | 0.45 | |
| Legumes and its products | 23.0 | 0.22 ± 0.01 | 0.20–0.25 | 0.00 | 0.00 | 0.00 | 0.00 | 0.08 | 0.28 | 0.58 | 0.85 | 1.73 | |
| Nuts and seeds | 2.0 | 0.05 ± 0.00 | 0.04–0.06 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.03 | 0.11 | 0.27 | 0.70 | |
| Vegetables | 90.9 | 0.35 ± 0.02 | 0.32–0.39 | 0.00 | 0.03 | 0.06 | 0.14 | 0.27 | 0.45 | 0.69 | 0.93 | 1.59 | |
| Mushrooms | 3.1 | 0.03 ± 0.00 | 0.02–0.03 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.02 | 0.07 | 0.15 | 0.41 | |
| Fruits | 170.4 | 0.16 ± 0.01 | 0.15–0.18 | 0.00 | 0.00 | 0.00 | 0.00 | 0.08 | 0.21 | 0.42 | 0.58 | 1.27 | |
| Meat and its products | 48.3 | 0.98 ± 0.03 | 0.92–1.05 | 0.00 | 0.00 | 0.00 | 0.19 | 0.64 | 1.42 | 2.33 | 3.20 | 4.83 | |
| Eggs | 25.6 | 0.34 ± 0.01 | 0.31–0.37 | 0.00 | 0.00 | 0.00 | 0.00 | 0.13 | 0.51 | 0.96 | 1.22 | 2.02 | |
| Fish and shellfish | 22.5 | 0.29 ± 0.04 | 0.22–0.36 | 0.00 | 0.00 | 0.00 | 0.03 | 0.13 | 0.29 | 0.61 | 0.92 | 2.05 | |
| Seaweeds | 4.1 | 0.05 ± 0.00 | 0.05–0.06 | 0.00 | 0.00 | 0.00 | 0.00 | 0.02 | 0.07 | 0.13 | 0.18 | 0.39 | |
| Milk and dairy products | 258.0 | 0.93 ± 0.03 | 0.88–0.98 | 0.00 | 0.00 | 0.00 | 0.38 | 0.78 | 1.35 | 1.91 | 2.25 | 3.09 | |
| Oils and fats | 4.0 | 0.01 ± 0.00 | 0.00–0.01 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.02 | 0.04 | |
| Beverages and alcohol | 33.5 | 0.05 ± 0.01 | 0.04–0.06 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.15 | 0.30 | 0.86 | |
| Seasonings | 14.6 | 0.09 ± 0.00 | 0.09–0.10 | 0.00 | 0.00 | 0.01 | 0.02 | 0.06 | 0.12 | 0.21 | 0.28 | 0.59 | |
| Processed foods | 1.1 | 0.01 ± 0.00 | 0.00–0.01 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.24 | |
| Total intake | 6.14 ± 0.08 | 5.99–6.30 | 1.80 | 2.86 | 3.38 | 4.53 | 5.88 | 7.56 | 9.19 | 10.40 | 12.12 | ||
CL, confidence limit; P, percentile.
1)All analyses accounted for the complex sampling design effect and appropriate sampling weights.
2)Dietary zinc intake per food group was calculated based on 1-day 24-h dietary recall data.
Estimation of usual zinc intake and its adherence to recommended levels
Table 3 presents distribution of usual zinc intake according to children’s characteristics. Among total subjects, the mean intake was 5.50 mg/d (SE = 0.04) after adjusting for the ratio of within- to between-person variation of zinc intake (0.59 for 1–2 yrs and 2.45 for 3–5 yrs). Older children, boys and children with higher household income showed higher zinc intake. However, there was no significant difference in zinc intake according to children’s living area. Recent 6 yrs data for the dietary zinc intake distribution is presented in Supplementary Table 2.
Table 3. Usual intake distribution of zinc (mg/d) among 1–5-year-old Korean children (n = 2,679)1),2) .
| Group | Mean ± SE | 95% CL | P1 | P5 | P10 | P25 | P50 | P75 | P90 | P95 | P99 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total subjects | 5.50 ± 0.04 | 5.42–5.57 | 2.17 | 3.10 | 3.65 | 4.56 | 5.46 | 6.39 | 7.30 | 7.84 | 9.10 | |
| Age group | ||||||||||||
| 1–2 yrs | 5.01 ± 0.06 | 4.88–5.14 | 1.84 | 2.71 | 3.08 | 3.80 | 4.87 | 6.02 | 7.07 | 7.72 | 9.55 | |
| 3–5 yrs | 5.83 ± 0.04 | 5.75–5.90 | 3.06 | 3.93 | 4.31 | 5.04 | 5.80 | 6.64 | 7.38 | 7.88 | 8.56 | |
| Gender | ||||||||||||
| Boys | 5.60 ± 0.05 | 5.50–5.70 | 2.24 | 3.08 | 3.63 | 4.64 | 5.59 | 6.58 | 7.50 | 8.02 | 9.11 | |
| Girls | 5.38 ± 0.05 | 5.29–5.48 | 2.13 | 3.20 | 3.66 | 4.47 | 5.35 | 6.24 | 7.07 | 7.45 | 8.97 | |
| Age group × Gender | ||||||||||||
| 1–2 yrs, boys | 5.07 ± 0.09 | 4.89–5.25 | 1.60 | 2.71 | 3.03 | 3.88 | 4.97 | 6.10 | 7.20 | 7.73 | 9.44 | |
| 1–2 yrs, girls | 4.94 ± 0.09 | 4.75–5.13 | 1.93 | 2.66 | 3.18 | 3.77 | 4.74 | 5.88 | 6.90 | 7.57 | 9.97 | |
| 3–5 yrs, boys | 5.98 ± 0.05 | 5.88–6.09 | 3.07 | 4.00 | 4.45 | 5.16 | 5.93 | 6.82 | 7.64 | 8.07 | 8.69 | |
| 3–5 yrs, girls | 5.66 ± 0.05 | 5.56–5.76 | 2.98 | 3.80 | 4.18 | 4.90 | 5.59 | 6.39 | 7.14 | 7.45 | 8.42 | |
| Living area | ||||||||||||
| Urban | 5.51 ± 0.04 | 5.43–5.59 | 2.23 | 3.18 | 3.66 | 4.57 | 5.46 | 6.42 | 7.32 | 7.86 | 9.11 | |
| Rural | 5.43 ± 0.09 | 5.26–5.61 | 1.94 | 2.79 | 3.63 | 4.53 | 5.47 | 6.21 | 7.21 | 7.63 | 8.70 | |
| Household income | ||||||||||||
| Low | 5.23 ± 0.14 | 4.95–5.50 | 2.09 | 2.90 | 3.36 | 4.21 | 5.15 | 6.24 | 7.07 | 7.44 | 8.61 | |
| Medium-low | 5.46 ± 0.07 | 5.33–5.59 | 2.17 | 3.18 | 3.67 | 4.53 | 5.38 | 6.27 | 7.26 | 7.85 | 9.34 | |
| Medium-high | 5.49 ± 0.06 | 5.38–5.60 | 2.22 | 3.09 | 3.61 | 4.57 | 5.49 | 6.40 | 7.28 | 7.75 | 8.83 | |
| High | 5.66 ± 0.07 | 5.52–5.80 | 2.03 | 3.24 | 3.77 | 4.77 | 5.66 | 6.57 | 7.40 | 8.01 | 9.11 | |
CL, confidence limit; P, percentile.
1)All analyses accounted for the complex sampling design effect and appropriate sampling weights.
2)To estimate usual zinc intake, zinc intake obtained from 1-day 24-h recall data was adjusted using the method described in the Nutrient Adequacy: Assessment Using Food Consumption Surveys (National Research Council, 1986). The adjusted (usual) zinc intake for each child was calculated using the ratio of within-to-between-person variance of zinc intake obtained from 2-day 24-h recall data of the 2009 Korea National Health and Nutrition Examination Survey (0.59 for 1–2 yrs and 2.45 for 3–5 yrs).
Table 4 shows the proportion of participants with inappropriate or excessive consumption of zinc. Based on the usual zinc intake of the study population, 1.1% of the children showed an inadequate intake below the EAR, and 10.7% of the children exceeded the UL. By age group, the proportion of children who had excessive zinc intake above the UL was 25.6% in children aged 1–2 yrs and 0.6% in children aged 3–5 yrs (P-value < 0.0001). The proportion of subjects with inappropriate or excessive intake of zinc did not differ by children’s gender, living area, or household income level. The zinc intake level in the study population was approximately 154% of the recommended nutrient intake (RNI) (SE = 1.1). Younger children had a higher % of RNI (mean = 167.0%, SE = 2.2) than older children (mean = 145.6%, SE = 1.0). In terms of gender, boys had a higher % of RNI (mean = 157.7%, SE = 1.6) than girls (mean = 150.6%, SE = 1.5). Recent change in proportion of subjects who had zinc intake above the UL among Korean young children is presented in Supplementary Fig. 1.
Table 4. Assessment of dietary zinc intake according to Dietary Reference Intakes for Koreans (n = 2,679)1),2) .
| Group | % RNI | Below EAR | Above UL | ||||
|---|---|---|---|---|---|---|---|
| Mean ± SE | 95% CL | % | P-value‡ | % | P-value‡ | ||
| Total subjects | 154.3 ± 1.1 | 152.1–156.4 | 1.1 | 10.7 | |||
| Age group | 0.0937 | < 0.0001 | |||||
| 1–2 yrs | 167.0 ± 2.2 | 162.8–171.2 | 1.6 | 25.6 | |||
| 3–5 yrs | 145.6 ± 1.0 | 143.7–147.5 | 0.8 | 0.6 | |||
| Gender | 0.4973 | 0.2223 | |||||
| Boys | 157.7 ± 1.6 | 154.7–160.8 | 1.0 | 11.6 | |||
| Girls | 150.6 ± 1.5 | 147.6–153.6 | 1.3 | 9.7 | |||
| Age group × Gender | 0.3157 | < 0.0001 | |||||
| 1–2 yrs, boys | 169.0 ± 3.0 | 163.1–174.9 | 1.4 | 26.9 | |||
| 1–2 yrs, girls | 164.7 ± 3.2 | 158.5–170.9 | 1.9 | 24.0 | |||
| 3–5 yrs, boys | 149.6 ± 1.3 | 147.0–152.2 | 0.7 | 0.6 | |||
| 3–5 yrs, girls | 141.6 ± 1.3 | 139.0–144.1 | 0.9 | 0.5 | |||
| Living area | 0.3038 | 0.6811 | |||||
| Urban | 154.6 ± 1.2 | 152.2–157.0 | 1.0 | 10.8 | |||
| Rural | 152.6 ± 2.6 | 147.4–157.8 | 1.7 | 10.1 | |||
| Household income | 0.9014 | 0.6371 | |||||
| Low | 147.9 ± 4.4 | 139.2–156.6 | 1.0 | 12.1 | |||
| Medium-low | 153.7 ± 2.0 | 149.7–157.6 | 1.0 | 9.6 | |||
| Medium-high | 154.4 ± 1.7 | 151.0–157.8 | 1.4 | 11.7 | |||
| High | 157.5 ± 2.1 | 153.3–161.6 | 1.0 | 10.3 | |||
CL, confidence limit; EAR, estimated average requirement; RNI, recommended nutrient intake; UL, tolerable upper intake level.
1)All analyses accounted for the complex sampling design effect and appropriate sampling weights.
2)To estimate usual zinc intake, zinc intake obtained from 1-day 24-h recall data was adjusted using the method described in the Nutrient Adequacy: Assessment Using Food Consumption Surveys (National Research Council, 1986). The adjusted (usual) zinc intake for each child was calculated using the ratio of within-to-between-person variance of zinc intake obtained from 2-day 24-h recall data of the 2009 Korea National Health and Nutrition Examination Survey (0.59 for 1–2 yrs and 2.45 for 3–5 yrs).
‡P-values were obtained from the χ2 test.
Systematic review on the ratio of within- to between-person variance of zinc intake among young children
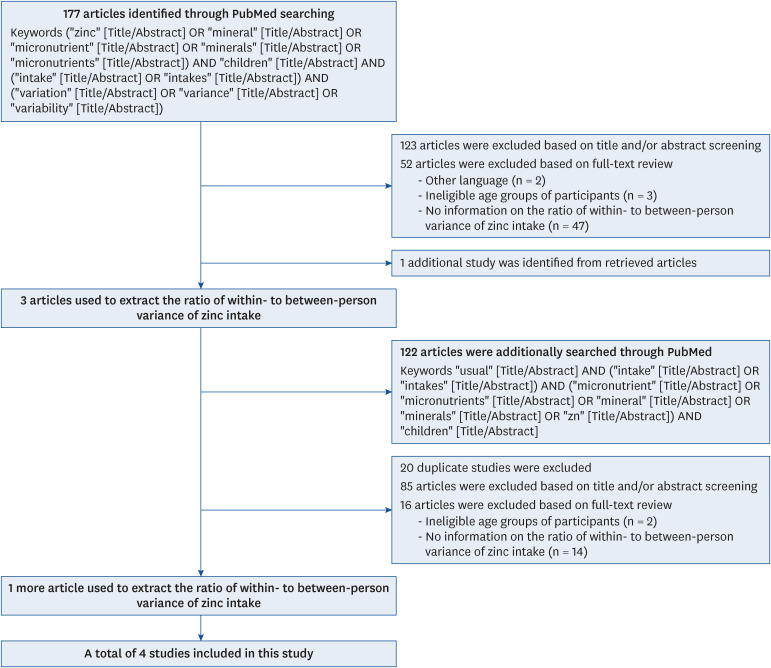
Our primary literature search identified 177 articles in the PubMed database. Of these, 123 articles were excluded after screening their titles and/or abstracts. Based on a full-text review of 54 articles, 52 were excluded according to the selection criteria. In addition, one article was identified from the reference lists of the retrieved articles. A secondary literature search identified 122 articles. After excluding 20 duplicated articles from the primary search, 85 articles were excluded after screening titles and/or abstracts, and 16 articles were excluded based on full-text review. Finally, four studies were selected to extract information on the ratio of within- to between-person variance in zinc intake among young children (Fig. 1).
Fig. 1. Flowchart for the selection of studies on the ratio of within- to between-person variance of zinc intake among young children.
Table 5 lists characteristics of four selected articles [16,17,18,19]. Three studies collected dietary data through multiple 24-h dietary recalls [16,17,18] and one study used 3-day diet records [19]. The ratio of within- to between-person variance of zinc intake reported in selected studies ranged from 0.41 to 3.00. Children aged 2 yrs or younger showed the lowest ratio among all age groups, whereas children aged 2.5–3 yrs showed the highest ratio. Children older than 5 years had lower ratios than children aged 3–5 yrs. In a study by Nel et al. [18] using the same age groups as the current study, the ratio for children aged 1–2 yrs was 1.47 and 2.82 for children aged 3–5 yrs.
Table 5. Ratio of the within- to between-person variance of zinc intake among young children reported in selected studies.
| Author (year) | Country and study subjects | Data and study period | Dietary assessment | Age group | Ratio of the within- to between-person variance of zinc intake | Energy intake (kcal/d) | Protein intake (g/d) | Zinc intake (mg/d) |
|---|---|---|---|---|---|---|---|---|
| Arsenault & Brown (2003) | US, preschool children (n = 7,474) | Continuing Survey of Food Intakes by Individuals (CSFII), 1994–1996, 1998 | 2-day 24-h dietary recalls | < 1 yrs (n = 898, 12%) | 0.56 (0–6 mon), 1.06 (7–12 mon) | 852 ± 2771) | 6.6 ± 2.3 | |
| 1–3 yrs (n = 3,908, 52%) | 2.16 | 1,381 ± 442 | 7.6 ± 3.3 | |||||
| 4–5 yrs (n = 2,668, 36%) | 2.89 | 1,667 ± 485 | 9.1 ± 3.7 | |||||
| Huybrechts et al. (2008) | Belgium, preschool children (n = 661, 338 boys [51.1%] and 323 girls [48.9%]) | 2002–2003 | 3-day diet records | 2.5–3 yrs (n = 197, 29.8%) | 3.00 | 1,414 | 54.9 ± 1.1 | 7.9 ± 0.2 |
| 4–6.5 yrs (n = 464, 70.2%) | 2.70 | 1,483 | 56.7 ± 0.7 | 8.5 ± 0.2 | ||||
| Nel et al. (2022) | South Africa, children (n = 1,326) | Provincial Dietary Intake Study (PDIS), 2018 | 2-day 24-h dietary recalls | 1–2 yrs (n = 333, 25.1%) | 1.47 | 1,179 | 34.7 ± 1.5 | 6.5 ± 0.4 |
| 3–5 yrs (n = 514, 38.8%) | 2.82 | 1,344 | 40.4 ± 1.2 | 7.3 ± 0.1 | ||||
| 6–10 yrs (n = 479, 36.1%) | 2.23 | 1,560 | 46.3 ± 1.3 | 8.5 ± 0.2 | ||||
| Padilha et al. (2017) | Brazil, young children (n = 231, 127 boys [55.0%] and 104 girls [45.0%]) | BRISA project2), 2010–2012 | 3-day 24-h dietary recalls | 13–32 mon | 0.41 | 1,128 ± 289 | 50 ± 14 | 7.9 ± 4.9 |
1)Mean ± SD (or SE).
2)Aetiology of preterm birth and consequences of perinatal factors in child health: birth cohorts from 2 Brazilian cities, São Luís (MA) and Ribeirão Preto (SP) – BRISA.
DISCUSSION
Early childhood is a period of transition from milk to a family diet by accepting new foods through which eating habits are shaped. Once eating habits are formed, they tend to be maintained throughout their life cycle [20,21,22,23,24,25]. Therefore, diet in early childhood is important because it not only affects growth and development but also affects health in later life [20,26,27]. In particular, zinc plays an important role in metabolism related to growth and development. Therefore, adequate and safe intake is required for children [1]. In this study, we evaluated the dietary zinc intake levels in Korean toddlers and preschoolers based on the usual intake estimation of zinc.
The main sources of zinc intake in young children are meat, milk, and dairy products. The zinc content in milk and dairy products is much lower than that in other food sources, while infants and toddlers have relatively high dependence on milk and dairy products. Additionally, Asian children, including the subjects of this study, can obtain zinc from rice and other grain products, which serve as staple foods in Asia [5,16,28,29]. Cereals and legumes on the list of major sources of zinc have ambivalence for zinc nutrition because they contain high levels of phytate, which hinders zinc absorption. US preschool children consumed zinc mainly from ready-to-eat cereal, milk and dairy products, meat, eggs, and potatoes [16]. Young children in South Africa obtained about 30% of their zinc intake from maize porridge [18]. Fish and sugar-sweetened beverages are also major sources of zinc intake in young Filipino children [5]. The high ranking of fish reflects the dietary characteristics of that country, and sugar-sweetened beverages are often used as carriers for micronutrient fortification in that country.
When the average daily usual intake of Korean young children for the survey years 2009–2013 was compared with that of children of similar age in other countries, it was similar to the intake level of children in some Asian countries [5,6,29] but higher than that of Filipino young children [5]. The intake levels of Korean children in 2009–2013 survey years were lower than those of Western children [16,19,30] and children in industrialized areas of South Africa [18], while the recent levels were compared to those countries.
To estimate the proportion of inappropriate and excessive consumption in a population, it is necessary to determine the usual intake adjusted for within-to-between-variation ratio. The current study used the ratio obtained from the 2-day dietary data of young Korean children. In addition, a systematic review of the literature reporting the within-person and between-person variations of young children was conducted to compare the ratio values according to study populations. The within-to-between-variation ratio of zinc intake in young children selected through this systematic review differed depending on the country. A significant trend was found when comparing the age of the children in each study. In a study by Arsenault and Brown [16], American children had a within- to between-person ratio of less than 1 in the first 6 months of life and about 1 in the rest of infancy. This ratio then increased to 2.89 at 4–5 yrs of age. It then decreased. The ratio at 4–5 years of age in American children [16] was smaller than that at 2.5–4 yrs of age, but greater than that at 4–6.5 yrs of age in Belgian children [19]. The variation ratio of South African children [18] showed a trend consistent with those in 2 previous studies [16,19]. These results indicated that within- to between-person variation in young children’s zinc intake had the characteristic of being the highest at around the age of 3 yrs. Only the study by Padilha et al. [17] on Brazilian children showed a variation ratio of less than 1, even after infancy. Korean children aged 1–2 yrs also had such low variance ratios.
Cashdan [31] reported that children’s acceptance of new foods expanded to 1–2 yrs of age and then rapidly decreased, showing the lowest level at 4–8 yrs of age. This can explain the tendency of within- to between-person variation to show the highest level around the age of three in the systematic review results of the present study. This suggests that the variation in dietary zinc intake in young children is greatly affected by age-related changes in dietary diversity. Diet diversity increased from infancy to toddlerhood. It then stabilized during early childhood.
When the within- and between-person variation was corrected for the 2009–2013 survey data, 1.1% of young Korean children had a high risk of inadequate intake below the EAR, whereas 10.7% of the children exceeded the UL with a high risk of excessive intake. In particular, 25.6% of children aged 1–2 yrs were at risk of excessive intake, whereas only 0.6% of children aged 3–5 yrs were at risk of excessive intake. In a study of the United Arab Emirates (UAE) children, 11% of children aged 12–23.9 mon, 5% of children aged 24–35.9 mon and 10% of children aged 36–47.9 mon were consuming zinc from foods and supplements above the UL [6]. The proportion of UAE infants (6–11.9 mon) with excessive zinc intake was much higher, at 22%, whereas 32% of infants consumed zinc below the EAR.
Recently, the KDCA reported zinc intake for Koreans since 2016 using 7th and 8th KNHANES data. These data show an increasing trend in zinc intake among children aged 1–5 yrs. In the KNHANES, as in this study, nutrient database based on the standard food composition table of the RDA, but a different revision of the food composition table was used. Therefore, direct comparison was not made, instead, 7th KNHANES data (2016–2018) and 8th KNHANES data (2019–2021) were analyzed in the same way as this study and supplementary tables were presented. In the recent survey, compared to the 2009–2013 data, the energy intake level of 1–5 yrs old children was higher, and among the main sources of zinc intake, intake levels from grains and their products and meat and its products increased, while intake from milk and dairy products and fish and shellfish was low. It seems to reflect the change in food intake behavior of young children, as it shows the same trend as the change in the intake level of the corresponding foods. In particular, high intake levels of meat and its products and zinc of children aged 1–2 yrs were prominent, and accordingly, it was analyzed that even after adjusting for within-person variance, half of the 1–2 yrs old children showed excessive intake above the UL. As it is estimated that there are significant changes in the food intake patterns of children aged 1–5 yrs, it is necessary to accurately evaluate zinc nutritional status based on the variance data of Korean children.
When DRIs were introduced as a new paradigm of nutrient recommendation in the US and the UL was set, it was reported that 51% of 1–3 yrs old children and 3% of 4–5 yrs old had greater usual zinc intake from food than the UL [16]. In infancy, the majority of infants exceeded the UL (92% of those aged 0–6 mon and 86% of those aged 7–12 mon) [16]. Zinc is an essential nutrient for children. Attention has been paid to whether zinc is consumed at a sufficient and safe level for growth and development. However, there have been reports of cases in which the intake level of young children exceeded the UL without any health problems or with beneficial results from zinc intervention. A recent systematic review reported that excessive zinc intake had no potentially harmful effects [32]. So far, approaches for setting UL for young children are based on limited evidence or extrapolated from adult reference values based on body weight. Accordingly, the UL of zinc for young children might have been too low.
This study had some limitations with regard to the usual intake estimation. Zinc intake data were collected a 1-day 24-h recall. Although within-person variation was adjusted using the within- to between-person variation ratios, the small sample of young Korean children was a limitation of the variation data. However, we systematically reviewed the literature and collected relevant data to verify our variation values for these young children. In addition, zinc intake level might have been underestimated, as the intake from dietary supplements was not included.
Despite these limitations, this study is significant in that it is the first to estimate the usual intake distribution of dietary zinc intake using a representative sample of Korean young children. In addition, this study presents the proportion of young children at a high risk of either inappropriate or excessive intake. The distribution of 1-day zinc intake overestimated the proportion of inappropriate or excessive intake. However, the estimation could be improved by adjusting for within-person variations. Above all, our study results provide a basis for inferring meaningful changes in intake levels that can be missed with only recent intake data, especially in identifying the clinical consequences of excessive consumption at the population level. Further research is needed to estimate the usual intake distribution in the Korean population. An evaluation that considers the difference in bioavailability according to the source of zinc intake is also required. Moreover, a prospective study is suggested to explore the relationship between the growth/health status of children and zinc intake levels, aiming to establish zinc dietary reference values for Korean young children.
Footnotes
Funding: This research was supported by the Daejeon University Research Grants (grant No. 20220185).
Conflict of Interest: The authors declare no potential conflicts of interests.
- Conceptualization: Shim JE.
- Formal analysis: Song S, Shim JE.
- Writing - original draft: Song S, Shim JE.
- Writing - review & editing: Song S, Shim JE.
- Funding acquisition: Shim JE.
- Supervision: Shim JE.
SUPPLEMENTARY MATERIALS
Dietary zinc intake per food group by survey years1),2)
Usual intake distribution of zinc (mg/d) among 1–5-year-old Korean children by survey years1),2)
Change in proportion of subjects who had zinc intake above tolerable upper intake level in Korean young children.
References
- 1.Brandão-Neto J, Stefan V, Mendonça BB, Bloise W, Castro AV. The essential role of zinc in growth. Nutr Res. 1995;15:335–358. [Google Scholar]
- 2.Salgueiro MJ, Zubillaga M, Lysionek A, Sarabia MI, Caro R, De Paoli T, Hager A, Weill R, Boccio J. Zinc as an essential micronutrient: a review. Nutr Res. 2000;20:737–755. [Google Scholar]
- 3.Roohani N, Hurrell R, Kelishadi R, Schulin R. Zinc and its importance for human health: An integrative review. J Res Med Sci. 2013;18:144–157. [PMC free article] [PubMed] [Google Scholar]
- 4.Brown KH, Wuehler SE, Peerson JM. The importance of zinc in human nutrition and estimation of the global prevalence of zinc deficiency. Food Nutr Bull. 2001;22:113–125. [Google Scholar]
- 5.Denney L, Angeles-Agdeppa I, Capanzana MV, Toledo MB, Donohue J, Carriquiry A. Nutrient intakes and food sources of Filipino infants, toddlers and young children are inadequate: findings from the national nutrition survey 2013. Nutrients. 2018;10:1730. doi: 10.3390/nu10111730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nassreddine LM, Naja FA, Hwalla NC, Ali HI, Mohamad MN, Chokor FA, Chehade LN, O’Neill LM, Kharroubi SA, Ayesh WH, et al. Total usual nutrient intakes and nutritional status of United Arab Emirates children (<4 years): findings from the Feeding Infants and Toddlers Study (FITS) 2021. Curr Dev Nutr. 2022;6:nzac080. doi: 10.1093/cdn/nzac080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walton J, Kehoe L, McNulty BA, Nugent AP, Flynn A. Nutrient intakes and compliance with nutrient recommendations in children aged 1-4 years in Ireland. J Hum Nutr Diet. 2017;30:665–676. doi: 10.1111/jhn.12452. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine (US), Food and Nutrition Board. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, D.C.: National Academy Press; 1997. [PubMed] [Google Scholar]
- 9.Yoon SI, Shim JE. Development of a zinc database to estimate the zinc intake levels in the Korean toddlers and preschool children. Korean J Community Nutr. 2021;26:103–110. [Google Scholar]
- 10.Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rural Development Administration, Rural Resources Development Institute. Food Composition Table. 7th rev. Suwon: Rural Development Administration; 2006. [Google Scholar]
- 12.Rural Development Administration, National Academy of Agricultural Sciences. Food Composition Table. 8th rev. Suwon: Rural Development Administration; 2011. [Google Scholar]
- 13.National Research Council (US) Subcommittee on Criteria for Dietary Evaluation. Nutrient Adequacy: Assessment Using Food Consumption Surveys. Washington, D.C.: National Academy Press; 1986. [PubMed] [Google Scholar]
- 14.Briefel RR, Bialostosky K, Kennedy-Stephenson J, McDowell MA, Ervin RB, Wright JD. Zinc intake of the U.S. population: findings from the third National Health and Nutrition Examination Survey, 1988-1994. J Nutr. 2000;130(Suppl):1367S–1373S. doi: 10.1093/jn/130.5.1367S. [DOI] [PubMed] [Google Scholar]
- 15.Ministry of Health and Welfare, Korean Nutrition Society. Dietary Reference Intakes for Koreans 2020. Sejong: Ministry of Health and Welfare; 2020. [Google Scholar]
- 16.Arsenault JE, Brown KH. Zinc intake of US preschool children exceeds new dietary reference intakes. Am J Clin Nutr. 2003;78:1011–1017. doi: 10.1093/ajcn/78.5.1011. [DOI] [PubMed] [Google Scholar]
- 17.Padilha LL, França AK, da Conceição SI, Carvalho WR, Batalha MA, da Silva AA. Nutrient intake variability and the number of days needed to estimate usual intake in children aged 13-32 months. Br J Nutr. 2017;117:287–294. doi: 10.1017/S0007114516004657. [DOI] [PubMed] [Google Scholar]
- 18.Nel JH, Steyn NP, Senekal M. Illustration of the importance of adjustment for within- and between-person variability in dietary intake surveys for assessment of population risk of micronutrient deficiency/excess using an example data set. Nutrients. 2022;14:285. doi: 10.3390/nu14020285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huybrechts I, De Bacquer D, Cox B, Temme EH, Van Oyen H, De Backer G, De Henauw S. Variation in energy and nutrient intakes among pre-school children: implications for study design. Eur J Public Health. 2008;18:509–516. doi: 10.1093/eurpub/ckn017. [DOI] [PubMed] [Google Scholar]
- 20.Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338:1650–1656. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 21.Cashdan E. Adaptiveness of food learning and food aversions in children. Soc Sci Inf (Paris) 1998;37:613–632. [Google Scholar]
- 22.Kelder SH, Perry CL, Klepp KI, Lytle LL. Longitudinal tracking of adolescent smoking, physical activity, and food choice behaviors. Am J Public Health. 1994;84:1121–1126. doi: 10.2105/ajph.84.7.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lien N, Lytle LA, Klepp KI. Stability in consumption of fruit, vegetables, and sugary foods in a cohort from age 14 to age 21. Prev Med. 2001;33:217–226. doi: 10.1006/pmed.2001.0874. [DOI] [PubMed] [Google Scholar]
- 24.Lytle LA, Seifert S, Greenstein J, McGovern P. How do children’s eating patterns and food choices change over time? Results from a cohort study. Am J Health Promot. 2000;14:222–228. doi: 10.4278/0890-1171-14.4.222. [DOI] [PubMed] [Google Scholar]
- 25.Skinner JD, Carruth BR, Wendy B, Ziegler PJ. Children’s food preferences: a longitudinal analysis. J Am Diet Assoc. 2002;102:1638–1647. doi: 10.1016/s0002-8223(02)90349-4. [DOI] [PubMed] [Google Scholar]
- 26.Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, Pfäffle R, Kiess W, Körner A. Acceleration of BMI in early childhood and risk of sustained obesity. N Engl J Med. 2018;379:1303–1312. doi: 10.1056/NEJMoa1803527. [DOI] [PubMed] [Google Scholar]
- 27.Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, Gortmaker SL. Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med. 2017;377:2145–2153. doi: 10.1056/NEJMoa1703860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kassis A, Chokor FA, Nasreddine L, Hwalla N, O’Neill L. Food sources of fiber and micronutrients of concern in infants and children in the United Arab Emirates: findings from the Feeding Infants and Toddlers Study (FITS) and the Kids Nutrition and Health Survey (KNHS) 2020. Nutrients. 2022;14:2819. doi: 10.3390/nu14142819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murakami K, Okubo H, Livingstone MB, Fujiwara A, Asakura K, Uechi K, Sugimoto M, Wang HC, Masayasu S, Sasaki S. Adequacy of usual intake of Japanese children aged 3-5 years: a nationwide study. Nutrients. 2018;10:1150. doi: 10.3390/nu10091150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eldridge AL, Catellier DJ, Hampton JC, Dwyer JT, Bailey RL. Trends in mean nutrient intakes of US infants, toddlers, and young children from 3 Feeding Infants and Toddlers Studies (FITS) J Nutr. 2019;149:1230–1237. doi: 10.1093/jn/nxz054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cashdan E. A sensitive period for learning about food. Hum Nat. 1994;5:279–291. doi: 10.1007/BF02692155. [DOI] [PubMed] [Google Scholar]
- 32.Wuehler S, Lopez de Romaña D, Haile D, McDonald CM, Brown KH. Reconsidering the tolerable upper levels of zinc intake among infants and young children: a systematic review of the available evidence. Nutrients. 2022;14:1938. doi: 10.3390/nu14091938. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Dietary zinc intake per food group by survey years1),2)
Usual intake distribution of zinc (mg/d) among 1–5-year-old Korean children by survey years1),2)
Change in proportion of subjects who had zinc intake above tolerable upper intake level in Korean young children.