“Saree cancers” and “dhoti cancers” are rare forms of cutaneous squamous cell carcinoma (cSCC), named so for developing on the waistline of people wearing traditional South Asian clothing that requires a tight cotton cord drawstring around the waist; namely, sarees and dhotis (1). The resulting chronic pressure and friction can produce permanent secondary skin changes, including dyspigmentation, acanthosis, scaling, ulceration and scarring, known as saree/dhoti “lines” or “drawstring dermatitis” (2). Such clothing can also exacerbate pre-existing koebnerizing dermatoses, such as lichen planus and vitiligo (3). However, malignant transformation within the saree line is extremely rare and its pathogenesis is uncertain. We report here a case of a saree waistline cSCC arising on a background of biopsy-proven lichen simplex chronicus (LSC). We summarize the current literature on this under-recognized skin cancer.
CASE REPORT
A 67-year-old Bangladeshi woman presented with a 3-year history of a slowly growing, itchy plaque on her right flank (Fig. 1). She had worn sarees with a very tight drawstring until the age of 42 years, when she stopped as she had developed localized pruritus, depigmentation and superficial ulceration bilaterally around the waistline. Her medical background included type 2 diabetes mellitus. On examination, a fungating, ulcerated mass measuring 11 cm in diameter was present on the right flank. Depigmentation, scaling and scar-like changes were present in the surrounding skin. Similar changes were observed on the contralateral flank. Both affected areas corresponded with her saree drawstring line. Lichenified eczematous changes were also present on her upper thighs, with additional pseudo-vitiliginous changes on her lower legs. There was no local lymphadenopathy, no anogenital pathology and no other mucocutaneous changes.
Fig. 1.

Clinical Photograph: squamous cell carcinoma on theright flank. A fungating mass measuring 11.6 cm in its longest dimension originates from a depigmented patch within the drawstring line on the right flank, just above the iliac crest.
Wide local excision of the tumour and surrounding depigmented skin confirmed a squamoproliferative lesion with an exo-endophytic growth pattern, consistent with a well-differentiated verrucous cSCC. The size of the SCC was 116 mm in the maximum diameter, with an absolute thickness of 4.5 mm and depth of invasion of 1.5 mm, Clark level IV (Fig. 2). There was no perineural or lymphovascular invasion. This was consistent with TMN stage pT3, Brigham and Women’s Hospital (BWH) stage pT2a.
Fig. 2.
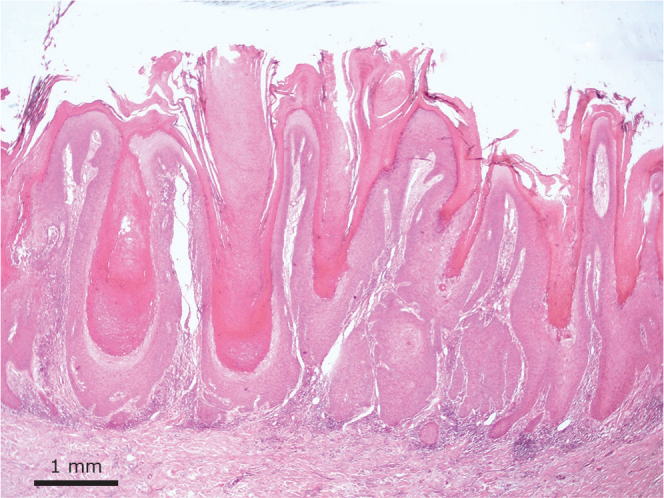
Pathology of lesion. Verrucous carcinoma (haematoxylin and eosin; H&E, low power) showing hyperkeratosis and a mixture of papillomatous and limited endophytic growth pattern. The tumour forms broad bulbous rete ridge-like processes with a pushing deep margin.
Skin biopsy from the left flank showed LSC, with psoriasiform acanthosis, hyperkeratosis, hypergranulosis and eosinophils. There was no evidence of epidermal dysplasia, lichen sclerosis or lichen planus. Further skin biopsies from the thigh and lower legs similarly showed features of LSC. LSC changes improved with topical corticosteroids. Staging CT scans of chest, thorax, abdomen and pelvis revealed no evidence of nodal or metastatic disease. There has been no evidence of locoregional cSCC recurrence 12 months after wide local excision.
DISCUSSION
Saree and dhoti cancers were first described in India in 1945 as waistline cSCCs appearing within friction lines corresponding with waistline drawstrings (1). At least 11 further cases of saree/dhoti cancer have been published since then (2–13). Overall, 72% are reported in females, the median duration of saree/dhoti use before cSCC development is 50 years, the median diameter of cSCCs at the time of excision was 7 cm and, in 4 cases, other skin changes were noted, particularly involving the contralateral waistline skin and most commonly described as hypopigmentation and scaling, as in the current case. Furthermore there is 1 case of bilateral waistline cSCC (4). In 4 cases reactive inguinal lymphadenopathy was described (2, 4, 8, 12). In 2 cases nodal metastases were identified, 1 case was identified on inguinal block node dissection and no follow-up data is available, in the other case patient underwent chemotherapy with paclitaxel and carboplatin followed by surgical resection and chemotherapy and maintained remission at the time of report 2 years after treatment (7, 10).
Despite many millions of people wearing sarees and dhotis worldwide, the frequency of associated skin malignancy is very low. It is possible that this condition is under-reported.
The reasons for the development of saree cSCC and the possible pathomechanisms underlying malignant transformation are unclear. One hypothesis is that scarring from the effects of chronic skin irritation and inflammation from drawstrings predisposes to cSCC formation, similar to Marjolin’s ulcer formation associated with chronic ulcers. The current patient developed a verrucous cSCC on a background of biopsy confirmed LSC, which affected other anatomical areas as well as the waistline. Although LSC is not usually considered a pre-cancerous condition, there are reports of cSCC arising within LSC (14, 15). We propose that the effect of chronic inflammation due to the patient’s saree drawstring was the additional driver behind cSCC transformation in this case
In summary, although saree/dhoti cancers are rare and their pathogenesis uncertain, they should be considered as causes of squamoproliferative lesions occurring on the waistline. They are likely to be an under-recognized type of cSCC in these populations, resulting from differences in cultural practices rather than differences in skin tone, but with significant implications for public health recommendations (4).
Footnotes
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Khanolkar VR, Suryabai B. Cancer in relation to usages: three new types in India. Arch Path 1945; 40: 351–361. [PubMed] [Google Scholar]
- 2.Rai P, Ghag G, Sanjanwala S, Jain R, Nandu V. Saree Cancer: a rare case. Indian J Surg Oncol 2020; 11: 93–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Verma SB. Dermatological signs in South Asian women induced by sari and petticoat drawstrings. Clin Exp Dermatol 2010; 35: 459–461 [DOI] [PubMed] [Google Scholar]
- 4.Gargade CB, Desai AY. Saree cancer: a case report. S Asian J Cancer 2019; 08: 101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balasundaram S. Can a tight saree wear cause cancer? – a rare case report. J Clin Diagn Res 2014; 8: QD01–QD2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rao J, Midya M, Sukheeja D, Prakash G. Dhoti cancer revisited. J Family Med Prim Care 2019; 8: 1235–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaveri Shaw, Jagadishwar Goud G, Vikas Kumar MB, Arun Katari, Kiranmai Gottapu V. Waist line skin cancer: a case report. J Med Sci Res 2014; 2: 21–23. [Google Scholar]
- 8.Gadahire M (2015). Saree cancer….squamous cell carcinoma secondary to waist dermatosis induced by attire – a case report. SAS J Surg 2015; 1: 56–57. [Google Scholar]
- 9.Akhtar MA, Saxena DK, Chikhlikar AA, Bangde AP, Rangwala M. Dhoti cancer: a waistline skin cancer with review of literature. World J Surg Oncol 2015; 13: 281.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takalkar UV, Asegaonkar SB, Kodlikeri P, Kulkarni U, Borundiya V, Advani SH. Saree cancer in Indian woman treated successfully with multimodality management. Dermatol Reports 2014; 6: 5128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nirhale DS, Bhatia M, Athavale VS, Calcuttawala M. Saree cancer: a diagnosis! Arch Med Health Sci 2015; 3: 121–123. [Google Scholar]
- 12.Kamble AS, Gokhale S. Saree cancer: a case report. Int J Biol Med Res 2012; 3: 1540–1541. [Google Scholar]
- 13.Vagholkar K. Cutaneous squamous cell carcinoma at an unusual site. Internet J Dermatol 2009; 8. [cited 2023 Apr 2] Available from: http://ispub.com/IJD/8/1/13208. [Google Scholar]
- 14.Tiengo C, Deluca J, Belloni-Fortina A, Salmaso R, Galifi F, Alaibac M. Occurrence of squamous cell carcinoma in an area of lichen simplex chronicus: case report and pathogenetic hypothesis. J Cutan Med Surg 2012; 16: 350–352. [DOI] [PubMed] [Google Scholar]
- 15.Deshmukh P, Sharma YK, Chaudhari ND, Dogra BB, Deo KS. Multiple squamous cell carcinoma over lichen simplex chronicus: a rare entity. Indian J Dermatol 2013; 58: 329.. [DOI] [PMC free article] [PubMed] [Google Scholar]


