Abstract
Objective:
Telemedicine has been proposed to improve access to care in rheumatology, but few studies of tele-rheumatology have been published. The objective of this study was to evaluate outcomes and quality of care for rheumatoid arthritis (RA) in patients seen by video telemedicine follow-up compared to in-person only.
Methods:
Individuals in the Alaska Tribal Health System with a diagnosis of RA were recruited when seeing a rheumatologist either in-person or by video telemedicine, both of which were offered as part of usual follow-up care. At baseline, participants completed the RAPID3 and a telemedicine perception survey and agreed to medical record review. Participants repeated surveys by telephone at 6 and 12 months, and medical record abstraction was performed at 12 months for quality measures.
Results:
At the 12-month outcome assessment, 63 of 122 RA patients (52%) had ever used telemedicine for RA. In univariate analysis, functional status improved over 12 months in the telemedicine group. In multivariate analysis, RAPID3 and functional status were associated with telemedicine group (higher), with no statistically significant change over the 12-month period. The only quality measure that differed between groups at 12 months in univariate analysis was the proportion of visits in which disease activity was documented (higher in the in-person group, 40% vs. 25%, p=0.02), but this was not significant after multivariate analysis.
Conclusion:
In short-term follow-up, there was no significant difference in most outcome and quality measures in patients with RA who incorporated telemedicine follow-up in their care compared to in-person only.
In rheumatoid arthritis (RA), guidelines highlight the importance of early diagnosis and initiation of disease-modifying anti-rheumatic drugs (DMARDs), with frequent disease monitoring using a treat-to-target strategy setting a target of remission or low disease activity.1 Studies have supported the importance of rheumatologists in the care and monitoring of patients with RA, with several studies demonstrating improved quality of care when a rheumatologist is included.2–5 However, access to rheumatologists is limited, especially in rural areas.6,7 Leveraging telemedicine s been proposed as a method to address workforce issues in rheumatology, with the potential to improve access to care for underserved communities.8
Prior to the COVID-19 pandemic, adoption of telemedicine in rheumatology was slower than in other specialties, and few studies of tele-rheumatology had been published as of a systematic review in 2015.9 Since 2015 and prior to the pandemic, more rheumatologists were using telemedicine and a few additional studies were published.10–13 During the COVID-19 pandemic, there has been a dramatic increase in use of telemedicine in all specialties.14 Complicating research in this field, telemedicine encompasses many different methods of using technology to deliver health care, including different communication methods (synchronous or asynchronous), phases of care (initial consult or follow-up visit), types of presenters (physicians, other trained presenters, presenters without specific training, or no presenters), and disease states.9 Synchronous telemedicine can be conducted from clinic to clinic or directly to the patient’s home or mobile device. In the systematic review of tele-rheumatology, the most commonly studied form of telemedicine was synchronous, with RA or other inflammatory arthritis as the most common disease state.9 The most common presenters were physicians, and tele-rheumatology was most commonly studied in the initial consultation phase of care.9 Finally, telemedicine can be incorporated into rheumatology practices in many ways, but in most cases it is not used exclusively to replace in-person visits. In this observational study of tele-rheumatology in the Alaska Tribal Health System (ATHS), we focus on the practice model used in our system during the study, namely synchronous video telemedicine from clinic to clinic, to provide some but not all care in the follow-up phase of RA, with the use of a non-physician presenter who is not specifically trained in rheumatology.
In the ATHS, asynchronous telemedicine (otherwise known as store-and-forward or eConsult) was available for 20 years, but not widely used in rheumatology. Improved connectivity allowed for the expansion of synchronous video telemedicine for specialty care in the ATHS. In rheumatology, telemedicine has been available as part of usual care since 2015, as described previously.15 Rheumatologists are based at the Alaska Native Medical Center (ANMC) in Anchorage and provide care to the Alaska Native population statewide. Specialty care is provided using regional field clinics, telemedicine visits, and in-person visits at ANMC. The cost of travel from rural communities to Anchorage can be significant. Because of the need to provide care to patients residing in over 200 small communities, telemedicine is performed with a presenter who is not specifically trained in rheumatology. Telemedicine can be used for any disease state, but our study focused on RA because it is the most common condition seen.
This observational study was designed to evaluate the outcomes of and quality of care for RA in patients seen by video telemedicine at least once for follow-up compared to in-person only over the course of one year, when video telemedicine and in-person care were both available options in usual care. A previous publication from this study described the use of telemedicine in rheumatology in the ATHS, as well as factors associated with telemedicine use by RA patients at baseline.15 This analysis focuses on differences in outcomes (patient-reported disease activity and functional status) as well as quality of care (based on medical record abstraction) between individuals ever seen by video telemedicine compared to in-person only over the one-year study period.
PATIENTS AND METHODS:
Inclusion criteria:
Individuals age 18 and older with a diagnosis of RA confirmed by a rheumatologist who were being seen by a rheumatologist at the Alaska Native Medical Center (ANMC), either in person or by telemedicine, were invited to participate in this study. Telemedicine had been available for rheumatology care for approximately one year prior to initial recruitment, with clinical practice described previously.15 Telemedicine was not used exclusively, but as an option to supplement in-person care. As an observational study of existing practice, we were unable to randomize patients to receive telemedicine, nor control how and when clinic staff offered telemedicine to patients. Enrollment occurred from August 2016 until March 2018. Recruitment relied on clinic staff introduction of the study to eligible patients and flyers in clinic, with research staff providing more detailed information to interested patients when clinic staff indicated possible interest. Research staff obtained written or oral informed consent from participants. For enrolled participants, follow-up continued for one year, and all follow-up was completed by March 2019. The study was approved by the Alaska Area Institutional Review Board. Tribal approval was obtained from participating Tribal Health Organizations.
Baseline study visit and clinical data:
After providing informed consent, participants completed a baseline study assessment at the time of enrollment, which could be conducted by research staff either in-person or by telephone and often coincided with a rheumatology clinic visit. A study procedure flow diagram is provided in Figure 1. The baseline data collection included two surveys (telemedicine perception survey and the Routine Assessment of Patient Index Data 3 (RAPID3)). The telemedicine perception survey questions and results have been described previously.15 Participants also agreed to medical record abstraction at baseline for demographics, disease characteristics, comorbidities, and measures of access to and quality of care. Medical record abstraction was performed using a standardized abstraction form, as described previously.15 Health care-related elements included the number of visits with a rheumatologist in the preceding year, whether each visit was conducted by telemedicine or in-person, and which rheumatologist was seen. Quality measures selected for this study included those endorsed by the American College of Rheumatology at the time of study design.16,17 Measures abstracted included: 1) whether disease activity was documented at each visit (by composite disease activity score or categorized without a composite score, similar to methods of Desai et al.18); 2) if the disease activity was moderate or high, whether a change in therapy was prescribed; 3) whether a functional status assessment was documented at each visit; 4) whether a DMARD was prescribed in the past year; 5) whether tuberculosis screening was performed prior to first biologic DMARD initiation; and 6) whether prolonged glucocorticoids were prescribed without a management plan.
Figure 1:
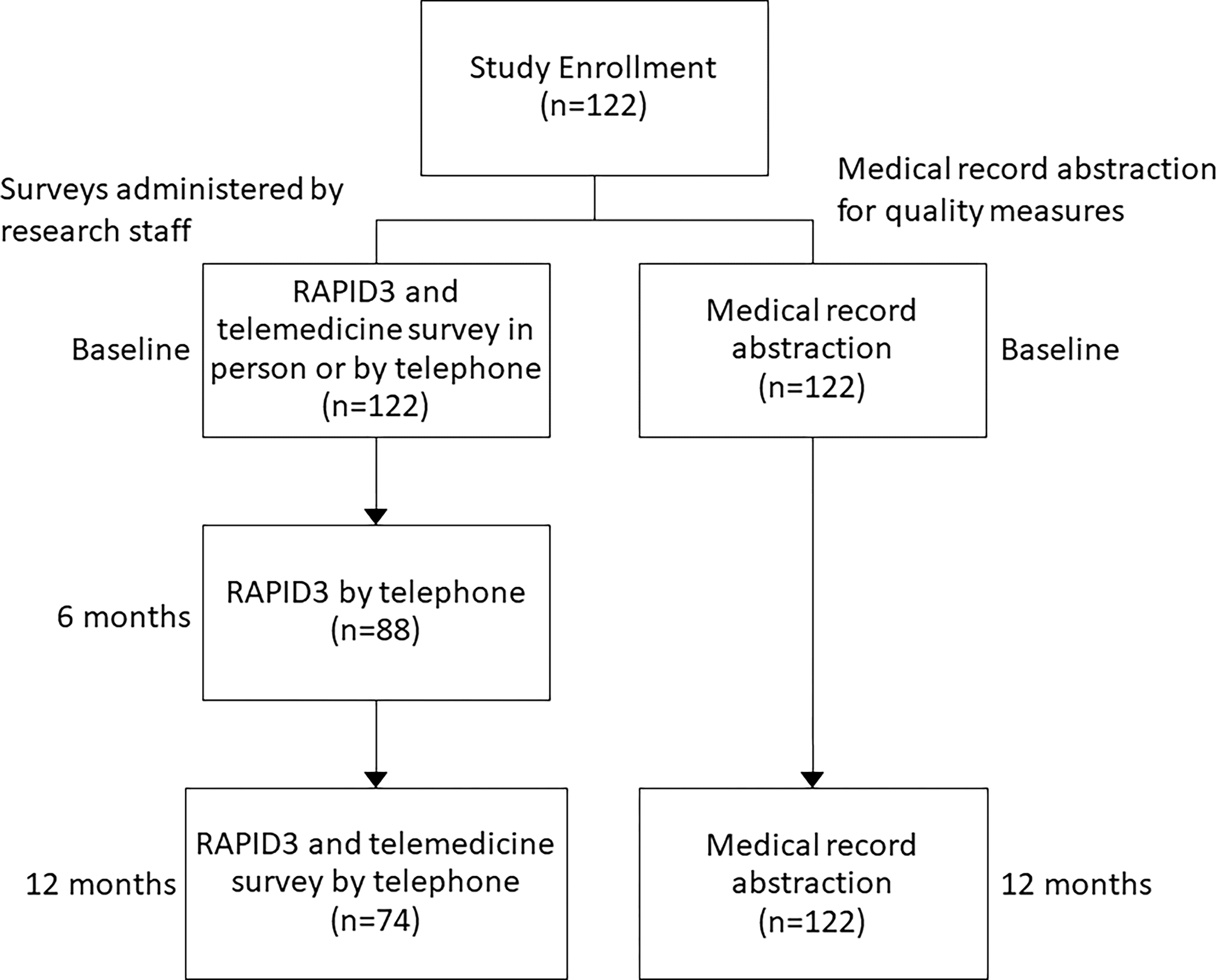
Flowchart for study procedures after study enrollment. The study included two forms of data collection, surveys administered by research staff and medical record abstraction for information about clinical care provided. On the left are the procedures for study surveys administered by research staff at baseline, 6 months, and 12 months, and the number of participants completing each step. On the right are the procedures for medical record abstraction at baseline and 12 months, and the number of participants for whom the abstraction was completed at each time point.
Longitudinal data collection:
Participants were contacted by research staff by telephone at 6 and 12 months for outcome assessment. This included RAPID3 by telephone at both time points and a repeat telemedicine perception survey at 12 months. Medical record abstraction of quality measures was repeated at 12 months for all participants. Patient-level variables included: 1) the number of visits with a rheumatologist in the year after study enrollment; 2) whether a DMARD was prescribed in the past 12 months; 3) whether the patient had been prescribed prolonged glucocorticoids without a documented glucocorticoid management plan; and 4) whether the first biologic DMARD had been initiated in the past year, and if so, whether tuberculosis screening had been performed within 6 months prior. Visit-level variables included: 1) whether the visit was performed by telemedicine; 2) whether disease activity was documented); 3) whether a medication change was prescribed if disease activity was moderate or high; and 4) whether functional status assessment was documented.
Statistical analysis:
Statistical analysis was performed using SAS version 9.4 (Cary, NC). A two-sided p-value less than 0.05 was considered significant. The study was designed to have 86% power to detect a difference in functional status by group, assuming mean and variability as determined in other populations. Participants were categorized as being in the telemedicine group if they had ever had a telemedicine visit with a rheumatologist. Otherwise, they were categorized in the in-person only group. Factors that differed between groups were analyzed at the one year time period, similar to baseline analysis.15 Two composite scores were included in this analysis (“Mean Rheumatologist Telemedicine Rate” and “Telemedicine Survey Score”), as previously described.15 Briefly, the Mean Rheumatologist Telemedicine Rate was defined as the weighted visit mean of rheumatologist telemedicine proportions, to account for differing proportion of overall visit load of each rheumatologist conducted by telemedicine. For this analysis, it was dichotomized into “high” (≥5% of visits conducted by telemedicine) or “low” (<5% of visits conducted by telemedicine) for better fit in multivariate models. There were a total of 5 rheumatologists during the course of the study. The Telemedicine Survey Score is the average response to the 12 survey questions with values ranging from −2 to 2, with a higher score indicating more receptiveness to telemedicine and a zero score indicating a neutral response.
Initial comparisons between groups were performed with univariate methods. For patient-reported measures, the analysis only included patients who completed the study RAPID3 at 12 months. The change in RAPID3, functional status, and proportion of patients in low disease activity or remission by RAPID3 were analyzed from baseline, 6 month, and 12 month RAPID3 in the telemedicine and in-person groups using repeated measures analysis of variance (ANOVA) for the continuous variables and repeated measures logistic regression for categorical variables. Repeated linear measures mixed models were used to evaluate factors associated with the continuous variables over time. Covariates assessed included age, sex, group (telemedicine vs. in-person only), telemedicine survey score, number of rheumatologist visits in the preceding year, number of rheumatologist visits in the study year, rheumatologist telemedicine rate, ever seen by telemedicine by non-rheumatologist, and time point (baseline, 6 months, and 12 months). An interaction term between group and time point was included in the models. A significant interaction would mean the change in scores over time would be different by group. Models were selected based on the fit of the model and significance of individual covariate estimates in the model. General estimating equations (GEE) were used for the categorical variable to account for correlation between data from the same patient during multiple rounds of follow-up. The GEE results are based on an unstructured correlation matrix.
The analysis of quality of care for RA by group included data from medical record abstraction at 12 months and included all study participants. Most quality measures were analyzed by visit, and some patients did not have a visit with a rheumatologist during the 12 months after enrollment. Only patients with a visit were included in the analyses conducted by visit. All patients were included in the analysis by patient.
For all quality measures, initial comparisons between groups were performed using univariate methods. We used poisson regression to examine factors associated with the number of rheumatology visits during the study, controlling for age and sex. We evaluated the following variables in the model: group (telemedicine or in-person only), number of visits in the year prior to enrollment, baseline RAPID3 score, baseline telemedicine survey score, and rheumatologist telemedicine rate. Multivariable logistic regression was conducted for each of the remaining quality measures. We controlled for age (linear), sex, and group in all models, and evaluated the covariates listed above, in addition to whether the visit was conducted by telemedicine or not for visit-level analyses. Models were selected based on the fit of the model and of individual covariate estimates in the model.
RESULTS:
The characteristics of study participants at one year after study enrollment are presented in Table 1. Baseline characteristics, including disease characteristics, were described previously.15 As demonstrated in Table 1 and consistent with baseline, participants in the telemedicine group had a higher mean rheumatologist telemedicine rate and more positive perceptions of telemedicine. Although the telemedicine group had a higher mean RAPID3 score than the in-person group at one year (12.1 vs. 10.0), the difference was not statistically significant, while the difference had been significant at baseline (12.6 vs. 10.4, p=0.037).15 Not all participants completed the final RAPID3 (n=74 out of 122), so the power to detect differences was lower. In addition, variability in RAPID3 and functional status were higher than expected. Demographic and disease characteristics of those lost to follow-up compared to those completing follow-up surveys were similar, except that a higher proportion of those completing follow-up were female (89% vs. 76%, p=0.05). Six participants who had never used telemedicine prior to study enrollment had telemedicine visits during the study. These participants were categorized in the telemedicine group.
Table 1:
Characteristics of Patients with RA seen by Telemedicine vs. In-Person Only at One Year
| Characteristic | Telemedicine (n=63) | In-Person Only (n=59) | p-value |
|---|---|---|---|
|
| |||
| Female, n (%) | 52 (83%) | 50 (85%) | 0.74 |
| RAPID3 score (0–30 scale), mean (SD), (n=74) | 12.1 (5.8) n=33 |
10.0 (5.1) n=41 |
0.12 |
| Number of rheumatology visits in past year, mean (SD) | 1.8 (1.2) | 1.7 (1.4) | 0.78 |
| DMARD in past year, n (%) | 61 (97%) | 58 (98%) | 0.6 |
| Rheumatologist telemedicine rate in past year, mean (SD) | 21.7 (23.1) | 8.4 (11.2) | 0.0001 |
| Telemedicine survey score at one year (range −2 to +2), mean (SD), (n=74) | 0.50 (0.41) n=33 |
0.07 (0.41) n=41 |
<0.0001 |
| Change in telemedicine survey score from baseline to one year, mean (SD), (n=74) | 0.02 (0.5) n=33 |
0.05 (0.5) n=41 |
0.84 |
| Remission or low disease activity by RAPID3 at one year, n (%), (n=74) | 10 (25%) | 10 (29%) | 0.57 |
Patient-reported outcomes, including RAPID3 and functional status, are presented from baseline, 6 month, and 12 month surveys in Table 2. In the telemedicine group, there was no change in RAPID3 or the proportion of patients in low disease activity over time in univariate analyses, but there was a statistically significant improvement in functional status over time. In the in-person group, there was no significant change in any measures over time. Multivariate analyses of patient-reported outcomes are presented in Table 3, including details about the models and variables included. In the repeated linear measures mixed model for RAPID3, telemedicine group, increasing age, a lower number of visits during the year, and a lower telemedicine survey score were significantly associated with a higher RAPID3 score. There was no significant association of RAPID3 with time or group over time. The multivariate model of functional status score over time had significant associations with telemedicine group and age, but the decline in functional status score over time that was evident for the telemedicine group in univariate analysis was no longer significant in multivariate analysis. Being in low disease activity or remission was significantly associated with male sex and telemedicine survey score, and negatively associated with age, but not associated with group or time.
Table 2:
Disease Activity and Functional Status over 12 Months in Patients with RA seen by Telemedicine vs. In-Person Only
| Telemedicine | In-Person Only | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline (n=62) | 6 months (n=48) | 12 months (n=39) | p-value | Baseline (n=60) | 6 months (n=40) | 12 months (n=35) | p-value | |
|
| ||||||||
| RAPID3, Mean (SD) | 12.4 (5.3) | 11.5 (5.0) | 12.1 (5.7) | 0.7* | 10.4 (5.6) | 9.8 (4.7) | 10.0 (5.4) | 0.50* |
| Low disease activity or remission, n (%) | 11 (18) | 10 (21) | 9 (23) | 0.5** | 17 (28) | 9 (23) | 11 (31) | 0.42** |
| Functional status score, mean (SD) | 2.9 (1.9) | 2.5 (1.7) | 2.4 (1.8) | 0.02* | 1.9 (1.9) | 2.1 (2.0) | 1.8 (1.3) | 069 * |
repeated measures ANOVA
Repeated measures logistic regression
Table 3:
Multivariate Analyses of Disease Activity and Functional Status over 12 Months in Patients with RA seen by Telemedicine vs. In-Person Only
| Dependent Variable Evaluated in Model | Model Type | Independent Variable | Estimate (95% CI) | p-value |
|---|---|---|---|---|
| RAPID3 score | Mixed model | Age, linear | 0.07 (0.01, 0.14) | 0.04 |
| Male sex | −0.16 (−2.60, 2.27) | 0.89 | ||
| Telemedicine group | 2.38 (0.47, 4.30) | 0.02 | ||
| Telemedicine survey score | −0.86 (−1.58, −0.14) | 0.02 | ||
| Visits during study | −1.22 (−2.36, −0.09) | 0.04 | ||
| Time 6 months | 0.25 (−1.18, 1.68) | 0.73 | ||
| Time 12 months | 0.47 (−1.26, 2.20) | 0.59 | ||
| Group*6 months interaction | −0.18 (−1.80, 1.43) | 0.82 | ||
| Group*12 months interaction | 0.41 (−1.75, 2.57) | 0.71 | ||
| Functional status score | Mixed model | Age, linear | 0.04 (0.02, 0.06) | 0.0007 |
| Male sex | 0.26 (−1.09, 0.57) | 0.39 | ||
| Telemedicine group | 1.02 (0.36, 1.68) | 0.003 | ||
| Time 6 months | 0.01 (−0.31, 0.33) | 0.95 | ||
| Time 12 months | 0.02 (−0.34, 0.39) | 0.91 | ||
| Group*6 months interaction | −0.36 (−0.79, 0.08) | 0.11 | ||
| Group*12 months interaction | −0.44 (−0.94, 0.06) | 0.08 | ||
| Odds ratio (95% CI) | ||||
| Low disease activity or remission | GEE | Age, linear | 0.96 (0.93,0.99) | 0.009 |
| Male sex | 2.39 (1.00,5.70) | 0.05 | ||
| Telemedicine group | 0.41 (0.17,1.04) | 0.06 | ||
| Time 6 months | 0.82 (0.37,1.82) | 0.62 | ||
| Time 12 months | 1.15 (0.54,2.46) | 0.73 | ||
| Group*6 months interaction | 1.59 (0.47,5.37) | 0.45 | ||
| Group*12 months interaction | 1.38 (0.42,4.53) | 0.6 | ||
| Telemedicine Survey Score | 1.65 (1.05,2.57) | 0.03 |
GEE: General estimating equations; CI: confidence interval
Univariate analysis of differences in quality measures between groups are presented in Table 4. There were 63 patients with 114 visits in the telemedicine group and 59 patients with 103 visits in the in-person group. Although the mean number of visits were similar for each group, the in-person group was somewhat more likely to have had no visits during the study period (p=0.06). There was no difference between groups in the measures analyzed at the patient level (number of rheumatologist visits and proportion prescribed a DMARD). For visit-level analysis, a higher proportion of visits had disease activity documented in the in-person group compared to the telemedicine group. Table 4 does not include glucocorticoid management plan and tuberculosis screening prior to first biologic because few patients were eligible for these measures (fewer than 10 patients for each, with at least 80% of those patients meeting the target for each measure).
Table 4:
Quality Measures from Medical Record Abstraction at One Year
| Quality Measure | Telemedicine (n=63 patients with 114 visits) | In-Person Only (n=59 patients with 103 visits) | p-value |
|---|---|---|---|
|
| |||
| Number of rheumatologist visits in year after study enrollment, mean (SD) | 1.8 (1.2) | 1.7 (1.4) | 0.67 |
| At least one visit to a rheumatologist in the study year, n (%) | 56 (89) | 45 (76) | 0.06 |
| Proportion of visits in which disease activity is documented (% of visits) | 28 (25) | 41 (40) | 0.02 |
| Proportion of visits with moderate or high disease activity documented in which a change in medications is prescribed (% of visits) | 19/23 (83) | 17/23 (74) | 0.47 |
| Proportion of visits in which functional status assessment is documented (% of visits) | 28 (25) | 30 (29) | 0.45 |
| DMARD prescribed in past year (% of patients) | 61 (97) | 58 (98) | 0.6 |
Multivariate analyses of quality measures are presented in Table 5. The number of visits in the past year was associated with number of visits in the year prior to the study, but not with group or other variables. Documentation of disease activity was less likely for those with higher RAPID3 at baseline and with a higher number of visits in the past year, but was not associated with group. A change in medications when disease activity was moderate or high was negatively associated with the number of visits in year prior to study, but was not associated with group or other variables. Having a functional status assessment was associated with number of visits in the year prior to the study and negatively associated with a high rheumatologist telemedicine rate, but not with group. Having a DMARD prescribed in the past year was associated with increased age, but not group or other factors. As shown in Table 4, 97% of patients in the telemedicine group and 98% of patients in the in-person only group were prescribed a DMARD in the past year.
Table 5:
Multivariate Analysis of Factors Associated with Quality Measures from Medical Record Abstraction at One Year
| Dependent Variable Evaluated in Model | Model Type | n | Independent Variable | Estimate | p-value |
|---|---|---|---|---|---|
|
| |||||
| Beta 95% CI) | |||||
| Number of rheumatologist visits in past year | Poisson regression | 122 patients | Age, linear | −0.002 (−0.012, 0.009) | 0.73 |
| Male sex | 0.01 (−0.357, 0.379) | 0.95 | |||
| Telemedicine group | −0.02 (−0.293,0.249) | 0.87 | |||
| Number of visits in year prior to study | 0.11 (0.016, 0.201) | 0.02 | |||
| Odds ratio (95% CI) | |||||
| Documentation of disease activity at the visit | Multivariate logistic regression | 217 visits | Age, linear | 0.99 (0.97,1.02) | 0.66 |
| Male sex | 0.52 (0.21,1.30) | 0.16 | |||
| Telemedicine group | 0.54 (0.29,1.02) | 0.06 | |||
| RAPID3 at baseline | 0.89 (0.83,0.95) | 0.0004* | |||
| Number of visits in year prior to study | 0.76 (0.60,0.97) | 0.02 | |||
| Change in medications is prescribed when disease activity is moderate or high | Multivariate logistic regression | 46 visits | Age (linear) | 1.03 (0.96,1.11) | 0.38 |
| Male sex | 1.92 (0.09,42.5) | 0.68 | |||
| Telemedicine group | 2.44 (0.45,13.2) | 0.3 | |||
| Number of visits in year prior to study | 0.42 (0.18,0.98) | 0.04 | |||
| Functional status assessment documentation | Multivariate logistic regression | 217 visits | Age, linear | 1.00 (0.97,1.03) | 0.85 |
| Male sex | 1.40 (0.60,3.2) | 0.44 | |||
| Telemedicine group | 1.48 (0.75,2.90) | 0.26 | |||
| High rheumatologist telemedicine rate | 0.04 (0.01,0.20) | <0.001* | |||
| Number of visits in year prior to study | 1.30 (1.04,1.62) | 0.02* | |||
| DMARD prescribed in past year | Multivariate logistic regression | 122 | Age, linear | 1.27 (1.03,1.55) | 0.02 |
| Male sex | 0.06 (0.002,1.72) | 0.1 | |||
| Telemedicine group | 1.04 (0.05,21.3) | 0.98 | |||
CI: Confidence Interval; DMARD: disease-modifying anti-rheumatic drug
DISCUSSION:
In this observational study comparing telemedicine incorporated into usual follow-up care for patients with RA to in-person only care, few differences were detected in patient-reported outcomes or quality of care. In univariate analysis, functional status improved over the study period in the telemedicine group. In multivariate analysis, RAPID3 and functional status were higher in the telemedicine group, but this did not change over time. The only quality measure that differed between groups was the proportion of visits in which disease activity was documented, but this was not significant in multivariate analysis. This study was limited in size and duration.
Few studies have evaluated the outcomes of telehealth in rheumatology, and many recently published studies in RA focus on modalities other than synchronous video telemedicine, such as text messaging19,20 or telephone-based interventions.21 A study evaluating synchronous video telemedicine for inflammatory arthritis in rural veterans, similar to our study, found no difference in RAPID3 between the telemedicine and usual care groups at baseline and no change in RAPID3 in longitudinal follow-up.10 There were significant savings in visit costs and distance traveled, leading to the conclusion that factors important to patients should be considered in structuring health care delivery.10 A survey-based study in pediatric rheumatology similarly found that families reported fewer financial burdens when telemedicine was used.22 In Australia, a study of the patient perspective on a program providing synchronous tele-rheumatology follow-up of stable patients found that patients reported a significant reduction in travel.23 Although patients expressed some reservations about the quality of telemedicine visits initially, they viewed tele-rheumatology as equivalent to in-person care.23
In this study, we found a higher RAPID3 score in the telemedicine group at baseline,15 and although functional status improved over time in the telemedicine group, multivariate analysis found higher RAPID3 and functional status scores in the telemedicine group. Given that our study was observational, we hypothesize that higher disease activity factored into the patient’s decision to have a telemedicine visit, when the alternative was likely to wait longer for an in-person visit. Although we attempted to control for patient factors in multivariate analyses, not all differences were measured by our study instruments. Patient views on telemedicine and more frequent use of telemedicine by the rheumatologist were the main factors associated with its use. We have ongoing qualitative studies to better inform our understanding of how patients and providers make decisions about using telemedicine. Overall, we concluded that there was no statistically significant improvement in RAPID3 or functional status over the study period in either group, and no difference in the change over time by group.
Several measures of quality of care were abstracted from the medical record. The in-person group was slightly more likely to have no visits with a rheumatologist in the study period. This may indicate more availability of telemedicine visits or that people seen in-person only may not have needed as frequent follow-up. Disease activity documentation was more likely in the in-person group in univariate analysis. The logistics of documenting disease activity differ in a telemedicine visit compared to an in-person visit, which may make it less likely to be documented. With a presenter not trained in rheumatology, only some aspects of a joint examination can be performed such as visual inspection and range of motion, not a formal tender joint count and swollen joint count. Therefore, disease activity cannot be measured using disease activity scores commonly used in clinical practice such as the Clinical Disease Activity Index (CDAI) and Disease Activity Score with 28-joint counts (DAS28). A RAPID3 does not require a joint count and can be performed, but may be time-consuming if not collected prior to the start of the visit. Because the process of documenting disease activity in a telemedicine visit is more complex than an in-person visit, it might be expected that it would be less commonly performed. Other quality measures did not differ between groups. It is likely that quality measures captured by medical record abstraction do not adequately capture all aspects of the quality of a visit, especially in the case of visits conducted by telemedicine, and alternate measures designed for telemedicine visits should be considered. For example, because less time is typically spent on physical examination in a telemedicine visit, there is more time available for education about RA and medications, including shared decision-making.
This study had some limitations. First, this was an observational study in a setting where telemedicine was already in use, incorporated with in-person care, and we were unable to randomize patients to telemedicine or in-person only care, nor control how the option of telemedicine was presented to patients by clinic staff. We found that RAPID3 was higher in patients selecting telemedicine at baseline, but there are likely other unmeasured factors associated with the choice of telemedicine that could influence outcomes. We controlled for covariates when possible, but may not have accounted for all differences between groups in our analysis. A randomized controlled trial of telemedicine is no longer feasible in most practice settings, given the increase in use during the COVID-19 pandemic. Second, the study was small, with some attrition over time with respect to patient-reported outcome data and more variability than expected, restricting the conclusions that can be drawn from this preliminary study due to power limitations. Despite survey attrition, data on quality measures from medical record abstraction were available for all patients. In addition, the characteristics of patients lost to follow-up were similar to those who remained in the study. Because the patient-reported data were collected by telephone rather than in the clinic, there is a lower risk of bias. Third, the study provides a comparison of telemedicine incorporated into practice along with in-person care, not telemedicine alone, because we were constrained by the existing practice. However, this practice model is one we believe to be most appropriate for rheumatology. Finally, the duration of this study was short, and gains that may occur with telemedicine likely require a longer duration of follow-up.
In summary, in this preliminary study, we found few differences in outcomes and quality of care for RA in the short term in patients seen by telemedicine at least once compared to in-person only, when telemedicine was incorporated into usual care. These findings indicate that telemedicine can reasonably be offered as a component of care for RA and may provide the ability for patients to be seen more often. There are benefits of telemedicine, such as reducing costs and improving communication, which may make it attractive even if outcomes are not improved compared to in-person only care. Longer-term studies are needed to evaluate telemedicine in RA. Although randomized clinical trials would be ideal, telemedicine has already been incorporated into many rheumatology practices, with a dramatic increase due to the COVID-19 pandemic, and such studies are no longer feasible. Ongoing research by our group will expand on this study using mixed methods to evaluate patient and provider perceptions of telemedicine, as well as assessing outcomes and costs of telemedicine. If the costs of providing clinical care incorporating telemedicine are much lower than in-person only care or there are other benefits, with similar outcomes, then it becomes an increasingly viable option.
Significance and Innovation:
This study is one of few to provide data on disease activity, functional status, and quality of care for RA in patients with video telemedicine visits incorporated in their follow-up care, compared to in-person only care.
Overall, there were few differences between the groups in outcomes and quality of care, though the study was of a relatively small size and short duration.
The findings of this study suggest that video telemedicine is reasonable to incorporate into usual care for patients with RA.
This study was conducted prior to the onset of the COVID-19 pandemic, and since that time the uptake of telemedicine in rheumatology and other specialties has increased dramatically.
Financial support:
This project was supported by grant number R21HS024540 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Footnotes
Potential conflicts of interest: none.
REFERENCES:
- 1.Singh JA, Saag KG, Bridges SL Jr., et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Rheumatol 2016;68:1–26. [DOI] [PubMed] [Google Scholar]
- 2.Smolen JS, Aletaha D, Bijlsma JW, et al. Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis 2010;69:631–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MacLean CH, Louie R, Leake B, et al. Quality of care for patients with rheumatoid arthritis. JAMA 2000;284:984–92. [DOI] [PubMed] [Google Scholar]
- 4.Lacaille D, Anis AH, Guh DP, Esdaile JM. Gaps in care for rheumatoid arthritis: a population study. Arthritis Rheum 2005;53:241–8. [DOI] [PubMed] [Google Scholar]
- 5.Ferucci ED, Donnithorne KJ, Koller KR, Swango-Wilson A, Pflaum J, Lanier AP. Performance on rheumatoid arthritis quality indicators in an Alaska Native healthcare system. Qual Saf Health Care 2010;19:387–91. [DOI] [PubMed] [Google Scholar]
- 6.Yazdany J, Tonner C, Schmajuk G, Lin GA, Trivedi AN. Receipt of glucocorticoid monotherapy among Medicare beneficiaries with rheumatoid arthritis. Arthritis Care Res (Hoboken) 2014;66:1447–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Battafarano DF, Ditmyer M, Bolster MB, et al. 2015 American College of Rheumatology Workforce Study: Supply and Demand Projections of Adult Rheumatology Workforce, 2015–2030. Arthritis Care Res (Hoboken) 2018;70:617–26. [DOI] [PubMed] [Google Scholar]
- 8.Schmajuk G, Tonner C, Yazdany J. Factors associated with access to rheumatologists for Medicare patients. Semin Arthritis Rheum 2016;45:511–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ward IM, Schmidt TW, Lappan C, Battafarano DF. How Critical is Tele-Medicine to the Rheumatology Workforce? Arthritis Care Res (Hoboken) 2016;68:1387–9. [DOI] [PubMed] [Google Scholar]
- 10.McDougall JA, Ferucci ED, Glover J, Fraenkel L. Telerheumatology: A Systematic Review. Arthritis Care Res (Hoboken) 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wood PR, Caplan L. Outcomes, Satisfaction, and Costs of a Rheumatology Telemedicine Program: A Longitudinal Evaluation. J Clin Rheumatol 2019;25:41–4. [DOI] [PubMed] [Google Scholar]
- 12.Taylor-Gjevre R, Nair B, Bath B, et al. Addressing rural and remote access disparities for patients with inflammatory arthritis through video-conferencing and innovative inter-professional care models. Musculoskeletal Care 2018;16:90–5. [DOI] [PubMed] [Google Scholar]
- 13.Nguyen-Oghalai TU, Hunter K, Lyon M. Telerheumatology: The VA Experience. South Med J 2018;111:359–62. [DOI] [PubMed] [Google Scholar]
- 14.Rostom K, Smith CD, Liddy C, Afkham A, Keely E. Improving Access to Rheumatologists: Use and Benefits of an Electronic Consultation Service. J Rheumatol 2018;45:137–40. [DOI] [PubMed] [Google Scholar]
- 15.Ferucci ED, Holck P, Day GM, Choromanski TL, Freeman SL. Factors associated with use of telemedicine for follow-up of rheumatoid arthritis. Arthritis Care Res (Hoboken) 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.ACR Endorsed Measures. 2016. (Accessed 9/16/2016, at http://www.rheumatology.org/Practice-Quality/Clinical-Support/Quality-Measurement/ACR-Endorsed-Measures.)
- 17.Yazdany J, Robbins M, Schmajuk G, et al. Development of the American College of Rheumatology’s Rheumatoid Arthritis Electronic Clinical Quality Measures. Arthritis Care Res (Hoboken) 2016;68:1579–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Desai SP, Liu CC, Tory H, et al. Rheumatoid arthritis quality measures and radiographic progression. Semin Arthritis Rheum 2014;44:9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mary A, Boursier A, Desailly Henry I, et al. Mobile Phone Text Messages and Effect on Treatment Adherence in Patients Taking Methotrexate for Rheumatoid Arthritis: A Randomized Pilot Study. Arthritis Care Res (Hoboken) 2019;71:1344–52. [DOI] [PubMed] [Google Scholar]
- 20.Kuusalo L, Sokka-Isler T, Kautiainen H, et al. Automated text message enhanced monitoring versus routine monitoring in early rheumatoid arthritis: a randomized trial. Arthritis Care Res (Hoboken) 2019. [DOI] [PubMed] [Google Scholar]
- 21.de Thurah A, Stengaard-Pedersen K, Axelsen M, et al. Tele-Health Followup Strategy for Tight Control of Disease Activity in Rheumatoid Arthritis: Results of a Randomized Controlled Trial. Arthritis Care Res (Hoboken) 2018;70:353–60. [DOI] [PubMed] [Google Scholar]
- 22.Kessler EA, Sherman AK, Becker ML. Decreasing patient cost and travel time through pediatric rheumatology telemedicine visits. Pediatr Rheumatol Online J 2016;14:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Devadula S, Langbecker D, Vecchio P, Tesiram J, Meiklejohn J, Benham H. Tele-Rheumatology to Regional Hospital Outpatient Clinics: Patient Perspectives on a New Model of Care. Telemed J E Health 2019. [DOI] [PubMed] [Google Scholar]


