Abstract
Penetrating diaphragmatic injuries pose diagnostic and management challenges. Computed tomography (CT) scans are valuable for stable patients, but concern exists for missed injuries and complications in nonoperatively managed cases. The objective of this study was to explore the diagnostic utility of multidetector CT scan (MDCT) in identifying diaphragmatic injuries resulting from penetrating trauma. A systematic review and meta-analysis were conducted, following established guidelines, by searching PubMed, Scopus, Web of Science, and Embase databases up to July 6, 2023. Eligible studies reporting MDCT's diagnostic accuracy in detecting penetrating diaphragmatic injuries were included. Relevant data elements were extracted and analyzed using STATA software. The study included 9 articles comprising 294 patients with confirmed penetrating diaphragmatic injuries through surgical procedures. MDCT's diagnostic performance revealed a pooled sensitivity of 74% (95% CI: 56%-87%) and a pooled specificity of 92% (95% CI: 79%-97%) (Fig. two), with significant heterogeneity in both sensitivity and specificity across the studies. The Fagan plot demonstrated that higher pre-test probabilities correlated with higher positive post-test probabilities for penetrating diaphragmatic injury diagnosis using MDCT, but even with negative results, there remained a small chance of having the injury, especially in cases with higher pre-test probabilities. This study highlights MDCT's effectiveness in detecting diaphragmatic injury from penetrating trauma, with moderate to high diagnostic accuracy. However, larger sample sizes, multicenter collaborations, and prospective designs are needed to address observed heterogeneity, enhancing understanding and consistency in MDCT's diagnostic capabilities in this context.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10140-023-02174-1.
Keywords: Computed tomography, Diagnosis, Diaphragmatic injuries
Introduction
Accurate diagnosis and appropriate management of penetrating trauma to the diaphragm present a significant challenge [1, 2]. Thoracoabdominal penetrating traumas often result in diaphragmatic injuries, occurring in approximately 30% of cases [1]. However, these injuries can be difficult to detect due to nonspecific signs and symptoms, and around 7% of cases may be occult when occurring in isolation [1, 3]. Additionally, the small size of these injuries further complicates diagnosis, as minor tears can enlarge over time due to negative intrathoracic pressures, potentially leading to herniation of abdominal contents and subsequent complications [4–6].
The approach to thoracoabdominal trauma caused by penetrating injuries can be complex. Immediate operative exploration is necessary for hemodynamically unstable patients [2, 5] while patients with normal vital signs and no clear indications for surgery can be managed using various algorithms [2, 7, 8].
Despite the high sensitivity of operative exploration in detecting diaphragmatic injuries [2, 5, 6], this approach can still yield procedural complications in a significant number of cases [7, 9]. Therefore, a non-invasive approach to reliably detect diaphragmatic injuries in hemodynamically stable patients would help reduce unnecessary operations, minimize associated morbidity, and decrease costs [6, 9].
In the absence of clinical indications for surgery, stable patients with penetrating thoracoabdominal trauma are commonly evaluated using computed tomography (CT) scanning, particularly multidetector CT (MDCT) [2, 7, 11]. MDCT's high-resolution images in different planes have improved the detection accuracy of diaphragm injuries [2, 6, 8]. However, there remains a concern about missed diaphragmatic injuries in nonoperatively managed patients, as these injuries can go unnoticed and lead to life-threatening complications [7].
Considering these challenges and the potential benefits of MDCT in detecting penetrating diaphragm injuries, as supported by existing literature, this study aims to explore the diagnostic utility of MDCT in identifying diaphragmatic injuries resulting from penetrating trauma.
Methods
In accordance with the Preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [12], a comprehensive literature search was conducted on July 6, 2023, across PubMed, Scopus, Web of Science, and Embase databases. Customized search terms were used for each database, including ("CT scan" OR "CT-scan" OR "computed tomography" OR "computerized tomography" OR "tomography, x-ray computed") AND ("diaphragm*") AND ("penetration" OR "penetrating trauma" OR "penetrating injur*" OR "penetrating wound*" OR "gunshot wound*" OR "stab wound*" OR "penetrating abdominal trauma" OR "penetrating abdominal injur*" OR "penetrating chest trauma" OR "penetrating chest injur*" OR "penetrating thoracic trauma" OR "penetrating thoracic injur*" OR "penetrating thoracoabdominal trauma" OR "penetrating thoracoabdominal injur*"). Additionally, a manual search of references from included studies was performed to ensure thorough coverage. The AutoLit platform, developed by Nested Knowledge in St. Paul, Minnesota, USA, was utilized for deduplication, screening, and data extraction purposes.
All studies reporting at least one of the diagnostic accuracy measures of MDCT in detecting diaphragmatic injuries resulting from penetrating trauma, including accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV), were included. There were no restrictions regarding the date, country of origin, patient characteristics, reference standard type utilized, or study design. Exclusions encompassed duplicate papers, non-English literature, case series with fewer than five eligible patients, case reports, conference abstracts, editorial comments, author responses, review articles, nonhuman studies, and irrelevant papers pertaining to the topic of interest.
The screening process involved an evaluation of the title, abstract, and/or full text of each study. Two authors independently assessed the articles, and any uncertainties or ambiguities were resolved through consultation with a senior coauthor. The extracted data from each eligible paper included the first author's name, publication year, country of origin, study design, sample size and characteristics, characteristics of diaphragmatic and associated injuries, CT device specifications, utilization of contrast material, reference standard method, and diagnostic accuracy measures of MDCT.
The quality of the included studies was assessed using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool [13]. The QUADAS-2 tool evaluates the risk of bias and applicability concerns in four primary domains: patient selection, index test, reference standard, and flow and timing. Each domain was independently evaluated based on specific criteria outlined in the tool, such as representativeness of the study population, blinding of test results, and completeness of outcome data. Ratings of "low," "high," or "unclear" were assigned to each domain assessment.
Statistical analysis
The analysis involved calculating true positive, true negative, false positive, and false negative values, which were used to construct 2 × 2 tables presenting sensitivity and specificity data. To address cells in the 2 × 2 tables with zero values, a continuity correction was applied by adding 0.5 to each cell value. Summary effect estimates were obtained using a bivariate random effects model [14], allowing the creation of a summary receiver operating characteristic (SROC) curve and calculation of the area under the curve (AUC). Heterogeneity among studies was assessed using the I2 test [15], and subgroup analyses were conducted for I2 values exceeding 50% to explore potential sources of heterogeneity. Fagan plot analyses were performed, assuming pre-test probabilities of 25%, 50%, and 75%, to determine post-test probabilities for positive and negative results. Publication bias was evaluated using Deek's test [16], and if bias was present, the trim-and-fill method proposed by Duvall and Tweedie was used to create a symmetrical funnel plot and calculate an estimated summary value [17]. The statistical analysis was performed using the MIDAS user-made module for diagnostic test accuracy (DTA) meta-analysis [18] and STATA software (Version 17.0, Stata Corp, College Station, TX). A p-value less than 0.05 was considered statistically significant.
Results
Article screening and selection process
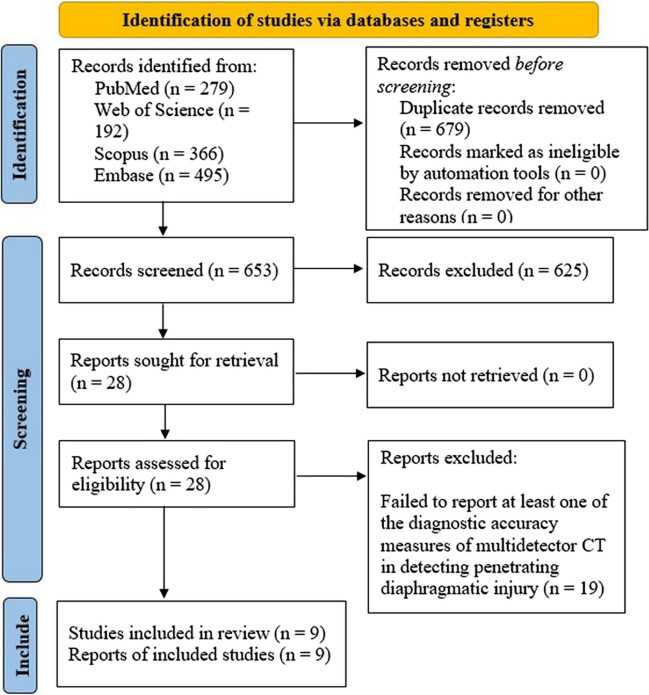
Using a predefined search strategy, 1332 articles were initially identified. After removing duplicates, 653 papers were screened based on title and abstract, resulting in the exclusion of 625 articles. The full text of the remaining 28 papers was thoroughly reviewed, leading to the exclusion of 19 articles not aligned with the study's aim. Ultimately, 9 articles meeting the inclusion criteria were identified. A flow diagram following PRISMA guidelines (Fig. 1) summarizes the screening process and eligibility criteria.
Fig. 1.
PRISMA flow diagram showing the review process. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Characteristics of the included studies
The selected studies included in our analysis comprised of 7 cohort studies [2, 5–8, 19, 20] and 2 case–control studies [1, 21]. These studies were conducted in various countries, including the United States (n = 4), France, Colombia, Canada, Brazil, and Turkey (each n = 1). The age range of patients across the studies varied from 13 to 86 years, with the majority of patients being male.
Among the nine articles selected, the majority of studies utilized thoracic, abdominal, or a combination of both types of MDCT scans. Three studies used oral contrast agents [2, 8, 20], three studies employed rectal administration of contrast material [2, 7, 8], and seven studies utilized IV contrast agents [1, 2, 7, 8, 19–21]. It is important to note that some studies incorporated multiple routes of contrast administration. Table 1 provides a summary of the general characteristics of the examined studies.
Table 1.
Characteristics of the included studies and patients
| First author, year of publication | Country | Study design | Age (years) | Male (%) | CT type | CT device/Slice thickness | Contrast material |
|---|---|---|---|---|---|---|---|
| Augustin, 2019 | France | Prospective cohort | NS | NS | Thoracoabdominal | A 64-row MDCT scanner/0.625 mm | NS (IV) |
| Bodanapally, 2009 | United States | Retrospective cohort | 29.6, (13–86) Mean, (Range) | 86 | Thoracic, Thoracoabdominopelvic, Abdominopelvic | MX 8000 or Brilliance 16 Power; Philips Medical Systems, Cleveland, OH (a 4- or 16-slice CT system)/3–5 mm | 2% sodium diatrizoate (Hypaque sodium; Nycomed, Princeton, NJ); 600 ml IV and 1–1.5 L enema |
| Dreizin, 2013 | United States | Case–control | 32.6, (16–85) Mean, (Range) | 92.6 | Thoracoabdominal | Somatom; Siemens, Malvern, Pa (64-section MDCT)/1.5 mm | 103 mL of IV ioversol, Optiray; Mallinckrodt, Hazelwood, Mo |
| Daza-Cajas, 2021 | Colombia | Prospective cohort | 23.2, (18–37) Mean, (Range) | 90.75 | Thoracic, Abdominal, Thoracoabdominal | GE LightSpeed; GE Healthcare, Milwaukee, WI, USA; 64 rows of detectors/ < 3 mm | NS (Non-contrast, IV or oral) |
| Leung, 2015 | Canada | Case–control | NS | NS | Abdominal | a 64-slice MDCT scanner/3 mm | 125 mL IV Omnipaque 300, GE Healthcare |
| Melo, 2011 | Brazil | Prospective cohort | 24.3, (6.8), (14–44) Mean, (SD), (Range) | 96.77 | Thoracoabdominal | GE LightSpeed; GE Healthcare, Milwaukee, WI, USA; 8 rows of detectors/1.25 mm | 100 mL IV iobitridol, Henetix 300, Guerbet, Rio de Janeiro, Brazil; 400 mL oral iodinated contrast solution; 200 mL of the same solution rectally |
| Stein, 2007 | United States | Retrospective cohort | 29.6, (11.4), (13–86) Mean, (SD), (Range) | 87.7 | Thoracic, Abdominal, Thoracoabdominal | MX 8000 or Brilliance 16 Power; Philips Medical Systems, Cleveland, OH (a 4- or 16-slice MDCT scanner)/3 mm | Oral, rectal and 150 mL of I2 mg/mL of IV contrast material |
| Uhlich, 2018 | United States | Retrospective cohort | NS | NS | NS | Koninklijke Philips NV, Amsterdam; a 256-slice CT scanner, and Philips Brilliance Power; a 64-slice machine/NS | NS |
| Yucel, 2015 | Turkey | Prospective cohort | 30, (15–61) Mean, (Range) | 91 | Thoracoabdominal | Multislice CT scanner | NS |
GE General Electric, IV Intravenous, MDCT Multidetector computed tomography, NS Not specified
Diaphragmatic injuries and CT findings
A total of 933 patients with penetrating trauma underwent both CT scan and the reference standard, resulting in the identification of 294 patients with penetrating diaphragmatic injury. Table 2 provides an overview of the general characteristics of diaphragmatic injuries resulting from penetrating trauma across all the included studies. Among these studies, bilateral injury was reported in only two studies [1, 20], while left-sided injury was the most commonly observed. Surgical exploration served as the reference standard in all of the studies included.
Table 2.
Included patients, characteristics of penetrating diaphragmatic injury, and reference standard utilized in each study
| First author, year of publication | Patients received both CT scan and reference standard (N) | Patients with PDI, confirmed by reference standard (N) | Right-sided injury (%) | Left-sided injury (%) | Bilateral injury (%) | Reference standard |
|---|---|---|---|---|---|---|
| Augustin, 2019 | 33 | 14 | 15.4 | 84.6 | NS | Surgical exploration |
| Bodanapally, 2009 | 136 | 47 | NS | mostly left-sided | NS | Surgical exploration |
| Dreizin, 2013 | 27 | 15 | 40.8 | 37 | 22.2 | Surgical exploration |
| Daza-Cajas, 2021 | 119 | 36 | 22.9 | 55.5 | 17.6 | Surgical exploration |
| Leung, 2015 | 17 | 9 | NS | NS | NS | Surgical exploration |
| Melo, 2011 | 31 | 8 | NS | NS | NS | Surgical exploration |
| Stein, 2007 | 154 | 50 | NS | NS | NS | Surgical exploration |
| Uhlich, 2018 | 373 | 104 | NS | NS | NS | Surgical exploration |
| Yucel, 2015 | 43 | 11 | 0 | 100 | 0 | Surgical exploration |
NS Not specified, N number, PDI Penetrating diaphragmatic injury
Regarding the mechanism of injury, two studies reported stab wounds [5, 19], while two studies specifically focused on gunshot injuries [8, 20]. Four studies documented cases involving both stab and gunshot wounds [1, 2, 7, 21], and one study did not provide specific information on the penetrating trauma mechanism [6]. Table 3 presents the diagnostic accuracy of MDCT scan in cases of diaphragmatic injury caused by penetrating trauma in the included studies.
Table 3.
Summary of findings in each study
| First author, year of publication | MOI | Important CT findings | Associated injuries | CT overall diagnostic accuracy |
|---|---|---|---|---|
| Augustin, 2019 | SW | NS | Thoracic new findings (pneumomediastinum, hemopneumothorax, pneumothorax, hemothorax, hemopericardium, ribs/scapula fracture) | Sen:50; Spe: 95; PPV:88; NPV: 72 |
| Bodanapally, 2009 | SW (43.38%) GSW (46.62%) Steel reinforcing bar injury (0.73%) | Contiguous injury sign on both sides of the diaphragm (the most accurate); Herniation of abdominal viscera into the thorax and the Collar sign (the most specific); Dependent viscera sign; Discontinuous diaphragm; Diaphragmatic thickening sign (the least specific) | Hemothorax, hemoperitoneum, splenic injury | Sen:87.2; Spe: 72.4; Accuracy: 77 |
| Dreizin, 2013 | SW (40.74%) GSW (59.26%) | Contiguous injury sign on both sides of the diaphragm (the most sensitive); Transdiaphragmatic trajectory (highly specific); Diaphragmatic discontinuity | NS | Sen: 86.67; Spe: 75; PPV: 81.25; NPV: 81.82 |
| Daza-Cajas, 2021 | GSW (85.71%) | Contiguous injury sign on both sides of the diaphragm (the most sensitive); Diaphragmatic discontinuity; Diaphragmatic thickening sign; Collar sign; Herniation of abdominal viscera into the thorax; Dependent viscera sign | Pleural effusion (n = 8)/Lung contusion (n = 12)/Pneumothorax (n = 23)/Hemoperitoneum (n = 40)/Liver injury (n = 32)/Splenic injury (n = 16)/Kidney injury (n = 17)/Hollow viscus injury (33)/Fracture (n = 7)/Pneumoperitoneum (n = 4) | Sen: 94.44; Spe: 46.84; PPV: 44.74; NPV: 94.87 |
| Leung, 2015 | SW (70.59)/ GSW (29.41) | Focal diaphragmatic defects; Collar sign; Dependent viscera sign; Herniation of abdominal viscera or fat into the thorax; Hump sign; Band sign (The latter two signs were observed in right-sided TDI) | Hemothorax; Pneumothorax; Hemoperitoneum; Pneumoperitoneum (total n = 16) | Sen: 33.3; Spe: 100; PPV:100; NPV: 57.1 |
| Melo, 2011 | GSW | Focal thickening and focal discontinuity of the diaphragm; Pleural effusion (in all TDI cases) | Pleural effusion (in all TDI cases), ipsilateral (in 3 cases), asymmetrically bilateral (remaining), larger on the injured side | Sen: 87.5; Spe: 100; PPV: 100; NPV: 95.83 |
| Stein, 2007 | SW (63.76%) GSW (36.24%) | Discrete diaphragmatic disruption; Herniation of abdominal viscera or fat into the thorax; Contiguous injury sign on both sides of the diaphragm; Foreign body within the muscle of the diaphragm | NS | Sen: 76; Spe: 98.1; PPV: 95; NPV: 89.5; Accuracy: 90.9 |
| Uhlich, 2018 | NS | Herniation of abdominal viscera or into the thorax; Collar sign; Dependent viscera sign; Contiguous injury sign on both sides of the diaphragm; Diaphragmatic thickening sign; Curled diaphragm; Hump sign; Band sign; Discontinuous diaphragm; Dangling diaphragm | Hemothorax, traumatic brain injury, liver, renal, gastric, intestinal, pancreatic, and plenic injuries | Sen: 39.42; Spe: 96.65; PPV: 82; NPV: 80.5 |
| Yucel, 2015 | SW | Injury line crossing the diaphragm; Loss of diaphragmatic integrity; Diaphragmatic irregularity | NS | Sen: 82; Spe: 88; PPV:70.14; NPV: 93.43 |
GSW Gunshot wound, MOI Mechanism of injury, NS Not specified, N Number, NPV Negative predictive value, PPV Positive predictive value, Sen sensitivity, Spe specificity, SW stab wound, TDI Traumatic diaphragmatic injury
Among the included studies, the presence of a contiguous injury sign on both sides was found to be the most sensitive indicator of penetrating diaphragmatic injury. Common signs observed on MDCT scans indicating potential penetrating diaphragmatic injury included herniation of abdominal viscera or fat into the thorax, the collar sign, dependent viscera sign, transdiaphragmatic trajectory, diaphragmatic discontinuity, and diaphragmatic thickening. Additionally, associated injuries frequently observed with penetrating diaphragmatic injury included pleural effusion, pneumothorax, hemothorax, hemoperitoneum, and pneumoperitoneum (Table 3).
Publication bias
Deek's funnel plot asymmetry test indicated no significant evidence of publication bias (P = 0.81) among the analyzed studies. As a result, we did not proceed with the trim-and-fill test (Supplementary Fig. 1).
Quality assessment
Supplementary Fig. 2 provides a visual representation of the quality assessment of the included studies. Further details regarding the quality assessment for each individual study can be found in Supplementary Table 1. Overall, the majority of studies included in this review exhibited satisfactory methodological quality, indicating a low risk of bias and minimal concerns regarding applicability.
Meta-analysis
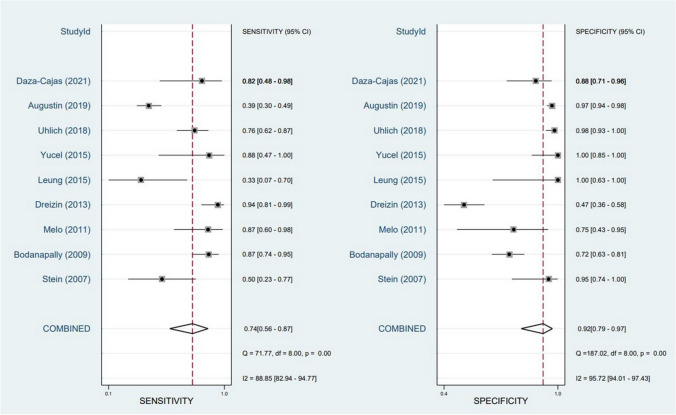
The meta-analysis of nine studies investigating the diagnostic performance of MDCT in assessing diaphragmatic injury in penetrating trauma revealed a pooled sensitivity of 74% (95% CI: 56%-87%) and a pooled specificity of 92% (95% CI: 79%-97%) (Fig. 2). However, significant heterogeneity was observed in both sensitivity (I2 = 88.85%, 95% CI: 82.94–94.77) and specificity (I2 = 95.72%, 95% CI: 94.1–97.43) across the included studies. The SROC curve demonstrated an AUC of 0.90 (95% CI: 0.88–0.93) (Fig. 3).
Fig. 2.
Forest plot and summary statistics of diagnostic test accuracy (DTA) meta-analysis of the included studies. CI: Confidence Interval
Fig. 3.
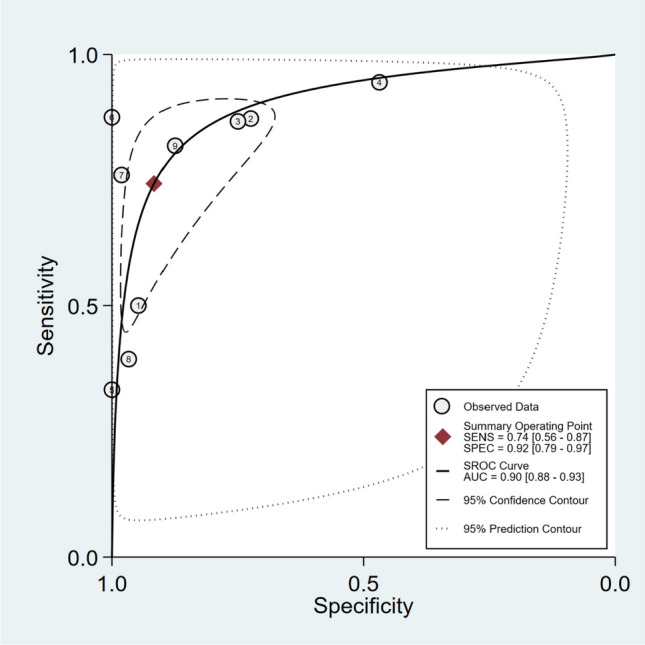
Summary receiver operating characteristic curve (SROC) of diagnostic test accuracy (DTA) meta-analysis of the included studies. AUC: Area Under the Curve. SENS: Sensitivity. SPEC: Specificity. SROC: Summary Receiver Operating Characteristic
We conducted univariate meta-regression analyses on several covariates, including mean age, mechanism of injury, and gender, to explore potential factors contributing to the heterogeneity observed. However, none of these covariates could account for the observed heterogeneity.
Fagan plot analysis
The Fagan plot analysis demonstrated that with pre-test probabilities of 25%, 50%, and 75%, the corresponding positive post-test probabilities were 75%, 90%, and 96%, respectively. Conversely, the negative post-test probabilities were 9%, 22%, and 46%, respectively. These findings are visually represented in Figs. 4, 5, and 6.
Fig. 4.
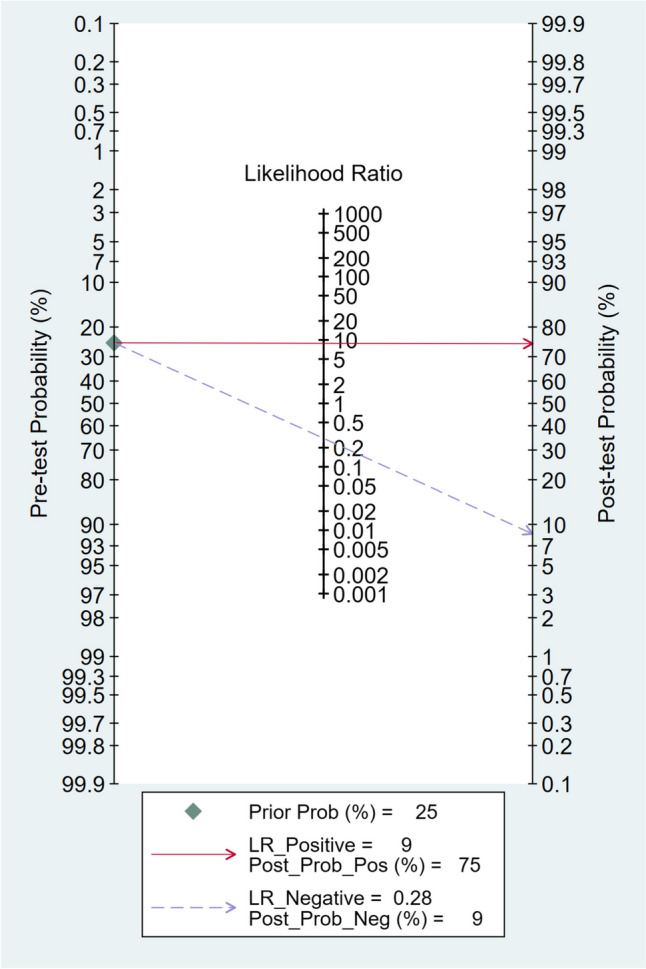
Fagan plot analysis using summary sensitivity and specificity results of the meta-analysis of the included studies with a pre-test probability of 25%
Fig. 5.
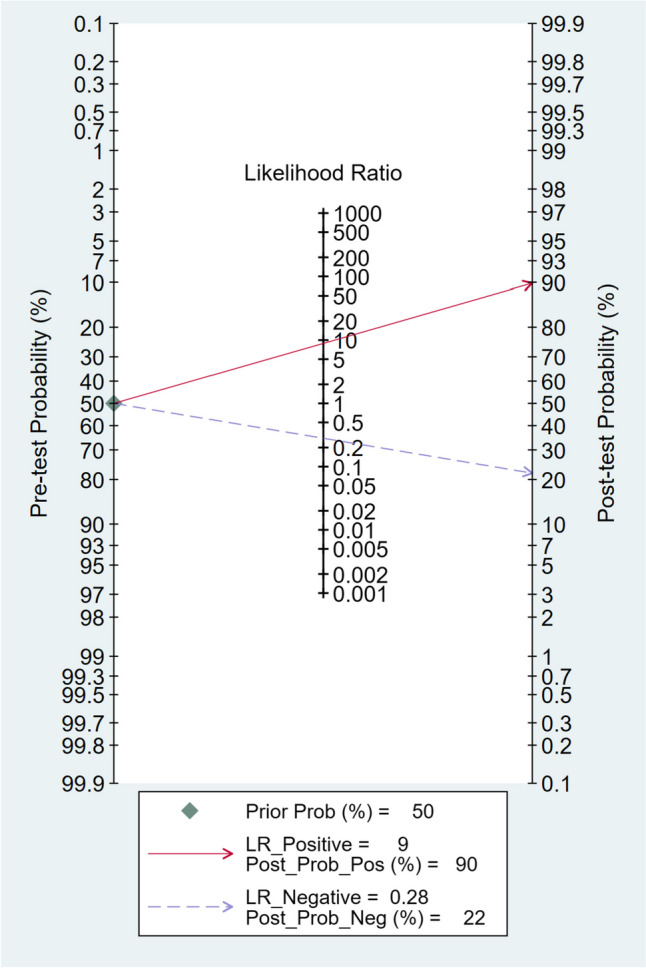
Fagan plot analysis using summary sensitivity and specificity results of the meta-analysis of the included studies with a pre-test probability of 50%
Fig. 6.
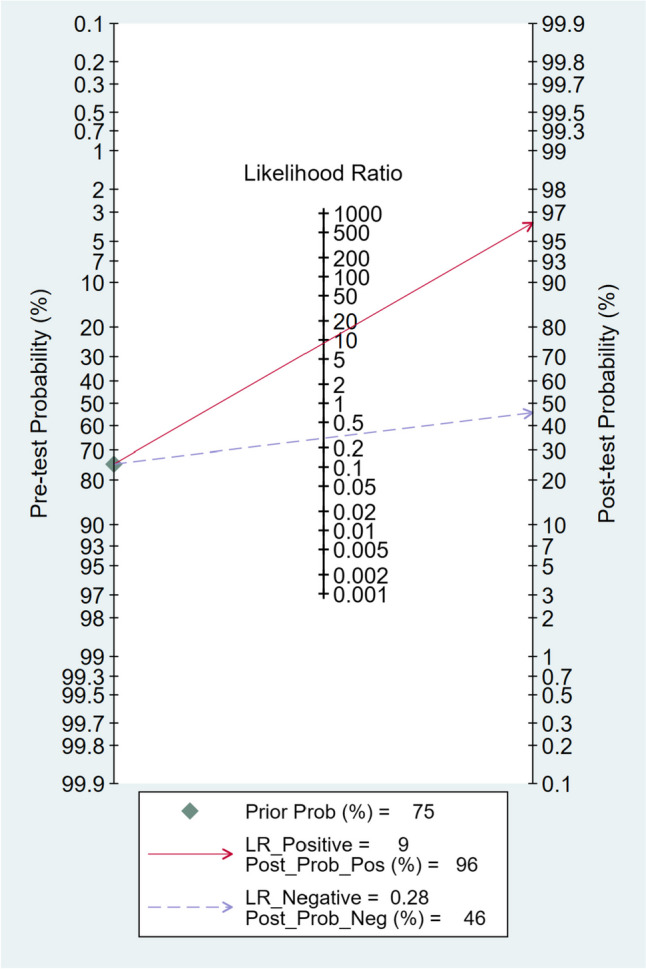
Fagan plot analysis using summary sensitivity and specificity results of the meta-analysis of the included studies with a pre-test probability of 75%
Discussion
This systematic review and meta-analysis expand upon previous studies in examining the diagnostic effectiveness of MDCT in the detection of traumatic diaphragmatic injuries caused by penetrating trauma. The primary objective was to gather comprehensive data on different measures of diagnostic accuracy associated with MDCT as an imaging modality in this context.
Diaphragmatic injuries caused by penetrating thoracoabdominal trauma may initially be small and without symptoms [6, 22, 23]. However, if not diagnosed and treated promptly, these injuries can expand over time, leading to the herniation of abdominal organs into the chest cavity and the development of symptoms [5, 6]. Delayed treatment of such herniation is associated with increased complexity, mortality, and morbidity risks [5]. Injuries to the left hemidiaphragm are considered more significant because of the greater likelihood of organ herniation and strangulation, although they are relatively easier to detect compared to right-sided injuries that may be obscured by the liver [6]. The identification of diaphragmatic injuries can be challenging, particularly in cases of gunshot or stab wounds that cause small lacerations [6, 24]. However, techniques like identifying associated injuries or using tractography have shown promise in improving diagnostic accuracy [1, 7, 8].
In the management of diaphragmatic injury resulting from penetrating trauma, there has been a shift from routine laparotomy to a more conservative approach due to studies demonstrating that routine laparotomy was unnecessary and associated with significant mortality and morbidity [25–29]. This conservative therapy approach involves urgent laparotomy for unstable patients or those with signs of peritonitis, while a wait-and-see policy is applied to the remaining patients. Non-operative treatment is pursued for patients who do not require surgical therapy at the end of the conservative therapy period [5]. However, visualizing the diaphragm in asymptomatic patients who do not require surgery poses a challenge. Diagnostic laparoscopy has emerged as a preferred method, exhibiting high sensitivity and specificity [5, 24, 30]. However, it is important to note that routine laparoscopy is therapeutic in only one-third of cases, rendering it unnecessary in the remaining two-thirds [5]. According to a study by Kones et al., the rate of unnecessary diagnostic laparoscopies for penetrating injuries to the left thoraco-abdominal region was relatively high at approximately 56% [31]. These findings highlight the need for cautious evaluation before deciding to proceed with diagnostic laparoscopy. Consequently, various less invasive or non-invasive methods have been investigated as potential alternatives to laparoscopy. These methods include ultrasonography, peritoneal lavage, and chest X-ray. However, studies have shown that none of these methods were sufficiently sensitive to be implemented in clinical practice [5, 32–35]. Although some advocate for the use of magnetic resonance imaging (MRI) in diagnosing diaphragmatic injuries, this technique has not gained widespread use in the acute setting [2, 33].
Over the past decades, advancements in CT technology, particularly the introduction of MDCT, have enhanced the ability to detect and evaluate diaphragmatic injury resulting from penetrating trauma [8]. While CT has already established its value in assessing hemodynamically stable blunt abdominal trauma patients and has become the preferred imaging modality in this context, its application in penetrating thoracoabdominal trauma cases is still an area of active study [8, 36]. MDCT allows for rapid scanning of a large region of interest within a breath-holding interval, reducing imaging time and minimizing artifacts caused by respiratory movement [37]. This results in improved image quality and the ability to obtain thinner sections. Furthermore, the use of special digital software enables reconstruction of axial images into coronal, sagittal, and oblique planes, aiding in the identification of challenging anatomical structures or injuries [32, 33]. Various signs, such as herniation of abdominal organs, focal diaphragmatic defects, and discontinuity of the diaphragm, have been described to aid in the detection of penetrating diaphragmatic injury on MDCT scans [8]. Despite the difficulties associated with visualizing diaphragmatic injuries, MDCT offers superior sensitivity and specificity compared to conventional CT in identifying small, asymptomatic diaphragmatic injuries after penetrating thoracoabdominal wounds [32, 33].
In a meta-analysis focusing on blunt traumatic diaphragmatic injuries, Reitano et al. [34] demonstrated that contrast-enhanced computed tomography exhibited a notable level of sensitivity (80%) and specificity (98%) in the detection of such injuries. When it comes to diagnosing diaphragmatic injuries resulting from penetrating trauma, the reported sensitivity of MDCT displays considerable variability. This variability is illustrated by findings that range from as low as 33.3%, as observed in the study conducted by Lenung et al. [21], to as high as 94.44%, as reported in the investigation conducted by Daza-Cajas et al. [20]. Additionally, the specificity of this modality has been reported from 46.84% in Daza-Cajas et al.'s study [20] to 100% in the studies by Lenung et al. [21] and Melo et al. [8]. Our meta-analysis revealed a pooled sensitivity rate of 74% and specificity rate of 92% for MDCT in diagnosing penetrating diaphragmatic injury. However, significant heterogeneity was observed in both sensitivity and specificity among the included studies. Despite conducting univariate meta-regression analyses, none of the examined covariates could account for the observed heterogeneity. Due to limited data availability, it was not possible to include other covariates that could potentially address the heterogeneity. This variation in sensitivity and specificity across studies can be attributed to several other factors. Differences in study populations, including variations in the severity of penetrating trauma, as well as variances in methodology such as image acquisition protocols, interpretation criteria, type of CT scan utilized (e.g., thoracic, abdominal, thoracoabdominal), and characteristics of the MDCT device, can contribute to the observed variation in sensitivity and specificity. Factors such as the size and location of the injuries, as well as the level of expertise in interpreting MDCT images, may also impact the diagnostic performance. It is crucial to take into account the moderate to high level of diagnostic accuracy exhibited by MDCT in identifying diaphragmatic injury resulting from penetrating trauma, considering the specific patient population and clinical scenario. While MDCT demonstrates the ability to detect a significant proportion of penetrating diaphragmatic injuries and aid in ruling them out, there is still room for improvement. The observed heterogeneity, emphasize the need for further research and standardization in this area. Future studies should aim to clarify the factors contributing to the variability and work towards improving the consistency and reliability of MDCT in diagnosing penetrating diaphragmatic injuries.
Additionally, the Fagan plot analysis demonstrated that a higher pre-test probability was associated with a higher positive post-test probability, indicating a stronger association between a positive MDCT result and the presence of diaphragmatic injury. Conversely, when the MDCT scan produced a negative result, the probability of having diaphragmatic injury decreased. However, even with a negative result, there remained a small chance of having diaphragmatic injury, particularly in cases with higher pre-test probabilities. These findings acknowledge MDCT's value as a diagnostic tool for penetrating diaphragmatic injury. However, interpreting MDCT results necessitates taking into account the clinical presentation context and the initial likelihood of a fracture.
Conclusion
This study emphasized the diagnostic effectiveness of MDCT in detecting diaphragmatic injury caused by penetrating trauma, especially in hemodynamically stable patients with no clear indications for immediate operative exploration. The meta-analysis revealed moderate to high diagnostic accuracy, with a pooled sensitivity of 74% and specificity of 92% for MDCT. However, further research with larger sample sizes, multicenter collaborations, and prospective designs is needed to investigate the factors contributing to the observed heterogeneity. This will help enhance our understanding and improve the consistency of MDCT in diagnosing diaphragmatic injury resulting from penetrating trauma.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We recognize the utilization of ChatGPT, a language model developed by OpenAI employing the GPT-3.5 framework, to aid in refining language accuracy during the manuscript editing process. This collaboration led to enhanced readability and linguistic quality. However, the authors reviewed and edited the content as needed, assuming complete accountability for the publication's substance.
Author contributions
The contributions of all authors influenced the conception of the project. During the revision phase, scientific insights were provided by Ali Gholamrezanezhad, Lee A. Myers, and Liesl S. Eibschutz. Crucial roles in conducting database searches, data extraction, drafting, and critical revisions to include essential intellectual content were played by Amir Hassankhani and Melika Amoukhteh. Payam Jannatdoust and Parya Valizadeh made noteworthy contributions to data analysis and interpretation. The final manuscript underwent a comprehensive review by all authors and received their unanimous approval.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Financial and non-financial interests
The authors have no relevant financial or non-financial interests to disclose.
Leadership role
Ali Gholamrezanezhad serves as the Director of Clinical Research at the Department of Radiology in the Keck School of Medicine of USC.
Footnotes
Amir Hassankhani, Melika Amoukhteh Co-first authors.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dreizin D, Borja MJ, Danton GH, et al. Penetrating diaphragmatic injury: accuracy of 64-section multidetector CT with trajectography. Radiology. 2013;268:729–737. doi: 10.1148/radiol.13121260. [DOI] [PubMed] [Google Scholar]
- 2.Stein DM, York GB, Boswell S, Shanmuganathan K, Haan JM, Scalea TM. Accuracy of computed tomography (CT) scan in the detection of penetrating diaphragm injury. J Trauma. 2007;63:538–543. doi: 10.1097/TA.0b013e318068b53c. [DOI] [PubMed] [Google Scholar]
- 3.Leppäniemi A, Haapiainen R. Occult diaphragmatic injuries caused by stab wounds. J Trauma. 2003;55:646–650. doi: 10.1097/01.TA.0000092592.63261.7E. [DOI] [PubMed] [Google Scholar]
- 4.Nason LK, Walker CM, McNeeley MF, Burivong W, Fligner CL, Godwin JD. Imaging of the diaphragm: anatomy and function. Radiographics. 2012;32:E51–70. doi: 10.1148/rg.322115127. [DOI] [PubMed] [Google Scholar]
- 5.Yucel M, Bas G, Kulalı F, Unal E, et al. Evaluation of diaphragm in penetrating left thoracoabdominal stab injuries: The role of multislice computed tomography. Injury. 2015;46:1734–1737. doi: 10.1016/j.injury.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 6.Uhlich R, Kerby JD, Bosarge P, Hu P. Diagnosis of diaphragm injuries using modern 256-slice CT scanners: too early to abandon operative exploration. Trauma Surg Acute Care Open. 2018;3:e000251. doi: 10.1136/tsaco-2018-000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bodanapally UK, Shanmuganathan K, Mirvis SE, et al. MDCT diagnosis of penetrating diaphragm injury. Eur Radiol. 2009;19:1875–1881. doi: 10.1007/s00330-009-1367-9. [DOI] [PubMed] [Google Scholar]
- 8.Melo ELA, de Menezes MR, Cerri GG. Abdominal gunshot wounds: multi-detector-row CT findings compared with laparotomy—a prospective study. Emerg Radiol. 2012;19:35–41. doi: 10.1007/s10140-011-1004-1. [DOI] [PubMed] [Google Scholar]
- 9.Kones O, Akarsu C, Dogan H, et al. Is non-operative approach applicable for penetrating injuries of the left thoraco-abdominal region? Turk J Emerg Med. 2016;16:22–25. doi: 10.1016/j.tjem.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shanmuganathan K, Mirvis SE, Chiu WC, Killeen KL, Hogan GJ, Scalea TM. Penetrating torso trauma: triple-contrast helical CT in peritoneal violation and organ injury–a prospective study in 200 patients. Radiology. 2004;231:775–784. doi: 10.1148/radiol.2313030126. [DOI] [PubMed] [Google Scholar]
- 11.Como JJ, Bokhari F, Chiu WC, et al. Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma. 2010;68:721–733. doi: 10.1097/TA.0b013e3181cf7d07. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097 [PMC free article] [PubMed]
- 13.Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 14.Arends LR, Hamza TH, van Houwelingen JC, Heijenbrok-Kal MH, Hunink MGM, Stijnen T. Bivariate random effects meta-analysis of ROC curves. Med Decis Making. 2008;28:621–638. doi: 10.1177/0272989X08319957. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58:882–893. doi: 10.1016/j.jclinepi.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 17.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 18.Dwamena BA (2007) MIDAS: a program for meta-analytical integration of diagnostic accuracy studies in Stata. Division of Nuclear Medicine, Department of Radiology, University of Michigan Medical School. Ann Arbor, Michigan
- 19.Augustin P, Guivarch E, Tran-Dinh A, Pellenc Q, Tanaka S, Montravers P. Usefulness of CT-scan in the management of chest stab trauma: a prospective observational study. Eur J Trauma Emerg Surg. 2020;46:1385–1391. doi: 10.1007/s00068-019-01203-4. [DOI] [PubMed] [Google Scholar]
- 20.Daza-Cajas GF, Valdés-Torres F (2021) Diagnostic performance of multislice computed tomography to detect diaphragmatic injuries in hemodynamically stable patients. Preliminary results. Rev Fac Med 69:e78672. English
- 21.Leung VA, Patlas MN, Reid S, Coates A, Nicolaou S. Imaging of traumatic diaphragmatic rupture: Evaluation of diagnostic accuracy at a level 1 trauma centre. Can Assoc Radiol J. 2015;66:310–317. doi: 10.1016/j.carj.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 22.Hammer MM, Flagg E, Mellnick VM, Cummings KW, Bhalla S, Raptis CA. Computed tomography of blunt and penetrating diaphragmatic injury: sensitivity and interobserver agreement of CT Signs. Emerg Radiol. 2014;21:143–149. doi: 10.1007/s10140-013-1166-0. [DOI] [PubMed] [Google Scholar]
- 23.Liu J, Yue WD, Du DY. Multi-slice computed tomography for diagnosis of combined thoracoabdominal injury. Chin J Traumatol. 2015;18:27–32. doi: 10.1016/j.cjtee.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 24.Mjoli M, Oosthuizen G, Clarke D, Madiba T. Laparoscopy in the diagnosis and repair of diaphragmatic injuries in left-sided penetrating thoracoabdominal trauma. Surg Endosc. 2015;29:747–752. doi: 10.1007/s00464-014-3710-8. [DOI] [PubMed] [Google Scholar]
- 25.Inaba K, Demetriades D. The nonoperative management of penetrating abdominal trauma. Adv Surg. 2007;41:51–62. doi: 10.1016/j.yasu.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 26.Schmelzer TM, Mostafa G, Gunter OL, Jr, Norton HJ, Sing RF. Evaluation of selective treatment of penetrating abdominal trauma. J Surg Educ. 2008;65:340–345. doi: 10.1016/j.jsurg.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 27.Ohene-Yeboah M, Dakubo JCB, Boakye F, Naeeder SB. Penetrating abdominal injuries in adults seen at two teaching hospitals in Ghana. Ghana Med J. 2010;44:103–108. doi: 10.4314/gmj.v44i3.68893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Como JJ, Bokhari F, Chiu WC, et al. Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma. 2015;68:721–733. doi: 10.1097/TA.0b013e3181cf7d07. [DOI] [PubMed] [Google Scholar]
- 29.Jansen JO, Inaba K, Rizoli SB, Boffard KD, Demetriades D. Selective nonoperative management of penetrating abdominal injury in Great Britain and Ireland: survey of practice. Injury. 2012;43:1799–1804. doi: 10.1016/j.injury.2011.03.062. [DOI] [PubMed] [Google Scholar]
- 30.Cherry RA, Eachempati SR, Hydo LJ, Barie PS. The role of laparoscopy in penetrating abdominal stab wounds. Surg Laparosc Endosc Percutan Tech. 2005;15:14–17. doi: 10.1097/01.sle.0000153732.70603.f9. [DOI] [PubMed] [Google Scholar]
- 31.Kones O, Akarsu C, Dogan H, et al. Is non-operative approach applicable for penetrating injuries of the left thoracoabdominal region? Turk J Emerg Med. 2016;16:22–25. doi: 10.1016/j.tjem.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sliker CW. Imaging of diaphragm injuries. Radiol Clin North Am. 2006;44:199–211. doi: 10.1016/j.rcl.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 33.Mirvis SE. Imaging of acute thoracic injury: the advent of MDCT screening. Semin Ultrasound CT MRI. 2005;26:305–331. doi: 10.1053/j.sult.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 34.Se Z, Primack SL. Radiographic and CT findings in blunt chest trauma. J Thorac Imaging. 2000;15:87–96. doi: 10.1097/00005382-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Parreira JG, Rasslan S, Utiyama EM. Controversies in the management of asymptomatic patients sustaining penetrating thoracoabdominal wounds. Clinics (Sao Paulo) 2008;63:695–700. doi: 10.1590/S1807-59322008000500020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shanmuganathan K. Multi-detector row CT imaging of blunt abdominal trauma. Semin Ultrasound CT MR. 2004;25:180–204. doi: 10.1016/j.sult.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 37.Hu H, He HD, Foley WD, Fox SH. Four multidetector-row helical CT: image quality and volume coverage speed. Radiology. 2000;215:55–62. doi: 10.1148/radiology.215.1.r00ap3755. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.