Abstract
Somatosensory tinnitus (ST) is a type of tinnitus where changes in somatosensory input from the head-neck area are one of the influencing factors of a patient’s tinnitus. As there are often several influencing factors, identifying a clear somatosensory influence on an individual patient’s tinnitus is often a challenge. Therefore, a decision tree using four clinical criteria has been proposed that can help diagnose ST with an accuracy of 82.2%, a sensitivity of 82.5%, and a specificity of 79%. Once correctly diagnosed, patients can be successfully treated using a musculoskeletal physical therapy treatment. This type of treatment can either be directed at cervical spine dysfunctions, temporomandibular disorders, or both and consists of a combination of counseling, exercises, and manual techniques to restore normal function of the cervical spine and temporomandibular area. Other techniques have been suggested but need further investigation in larger RCTs. In most cases, ST treatment shows a decrease in tinnitus severity or loudness, but in rare cases, total remission of the tinnitus is achieved.
Keywords: Tinnitus, Somatosensory, Somatic
Background
Tinnitus, the perception of sound without external acoustic stimulation, occurs in 10 to 15% of adults [1]. Tinnitus is a symptom often related to hearing loss or noise trauma, but it can also be linked to depression, anxiety, or excessive stress [1]. Additionally, tinnitus can be influenced by somatosensory input from the cervical spine and temporomandibular area, then called somatic or somatosensory tinnitus (ST) [2, 3].
On a pathophysiological level, almost all cases of tinnitus appear to be associated with some degree of peripheral hearing loss, either resulting in impaired hearing or involving abnormal supra-threshold sound processing, which is often referred to as “hidden hearing loss” [4]. Despite this strong link between tinnitus and peripheral hearing loss, the brain is believed to play a key role in the pathophysiology of tinnitus [5]. More specifically for ST, a pathophysiological model was presented where brainstem connections between somatosensory and auditory nuclei are suggested as the means by which changes in somatosensory afference can alter the loudness and pitch of an existing tinnitus or can even cause tinnitus [6]. Since the presentation of this model, several studies in animals and humans have provided evidence for the involvement of cortical networks.
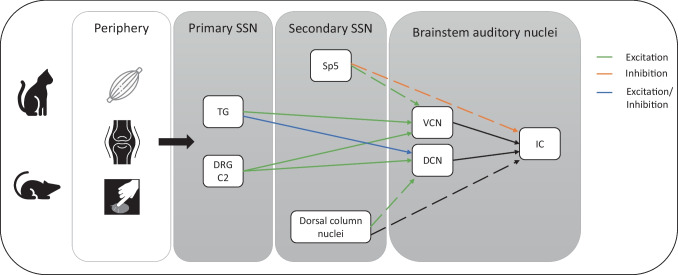
Studies in animal models identified projections from somatosensory neurons to the ventral and dorsal cochlear nucleus (CN) and inferior colliculus (IC), which are involved in auditory processing [7, 8] (see Fig. 1 for a comprehensive overview of all pathways retrieved from animal models). Through these projections, somatosensory afference from the head and neck region is able to alter both firing rate and synchrony of firing of CN neurons. Changes in firing rate are suggested to be associated with tinnitus loudness fluctuations, whereas changes in neural firing synchronicity are linked to alterations in tinnitus pitch [7]. Stimulation of cervical nerves in cats has shown that input from mechanoreception and proprioception has the largest influence on CN activity [9]. Nociception, on the other hand, does not appear to have a direct influence on CN activity since nociceptive projection cells are located in areas that do not directly project to the CN [10]. These findings suggest that tinnitus alterations in patients with ST are not caused by pain sensation but by changes in proprioceptive or mechanoreceptive input linked to increased muscle tension or restricted mobility in the neck or jaw region.
Fig. 1.
Animal model of auditory–somatosensory pathway interactions [7–10, 12, 13]. TG, trigeminal ganglion; DRG, dorsal root ganglion; Sp5, spinal trigeminal nucleus; VCN, ventral cochlear nucleus; DCN, dorsal cochlear nucleus; IC, inferior colliculus
Other animal research using light and electron microscopy suggests that the above-mentioned projections from the somatosensory neurons to the CN are an excitatory (glutamatergic) pathway [10–13]. Projections from the trigeminal ganglion can have both an excitatory and inhibitory (GABA-ergic) effect on dorsal CN activity [14]. Projections from the spinal trigeminal nucleus to the IC, on the other hand, seem to be mostly inhibitory [14, 15]. These findings suggest that, in most cases, increased activity in the connective fibers between the somatosensory nuclei and CN will cause an increase in firing rate in the CN.
In humans, Lanting et al. [16] identified activation differences restricted to the CN and IC between patients with temporomandibular-related ST and participants without tinnitus, assessed with functional magnetic resonance imaging during jaw protrusion, indicating the abovementioned mechanisms are also present in humans. Through this mechanism, the somatosensory system may cause tinnitus and/or alter the pitch or loudness of an existing tinnitus [7].
Where ST was originally described as a subtype of tinnitus, nowadays, tinnitus experts agree that in most patients, tinnitus has a multifactorial origin with a multitude of potential influencing factors [17–19]. Consequently, ST can be defined as tinnitus that is influenced by the cervical or temporomandibular somatosensory system.
This review aims to give an overview of the diagnostic process and treatment possibilities for patients with ST.
Somatic Tinnitus Diagnosis
Since the first papers in the 1990s mentioned the possible influence of the somatosensory system on tinnitus complaints [2, 3, 6], several papers have described ways to identify these patients.
In 2011, Sanchez et al. [20] proposed a set of diagnostic criteria to help recognize patients with ST in clinical practice. These criteria include the presence of recurrent pain episodes in the head, neck, or shoulder girdle and a temporal coincidence of the appearance of both tinnitus and pain complaints [20]. Others state that so-called somatic modulation, where tinnitus is momentarily changed during voluntary movements or specific resistance tests, is essential in diagnosing ST [21, 22].
In 2018, a new set of diagnostic criteria was published based on a modified Delphi process with a consensus meeting [17]. Instead of asking the participating experts to suggest criteria from scratch, they were asked to review a long list of potential diagnostic criteria for ST [17].
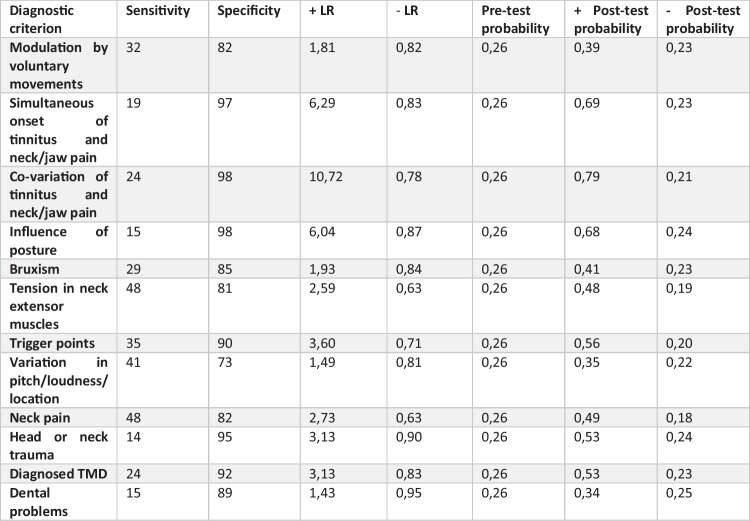
This process resulted in a set of 16 diagnostic criteria, subdivided into three categories (Fig. 2) [17]. These criteria came with some sidenotes from the consensus meeting panel. First, it was stated that although somatic modulation, especially through voluntary movements, was recognized as an important criterion, the absence of this ability does not rule out ST [17]. Therefore, somatic modulation should not be used as a single “yes or no” criterion to diagnose ST [17]. Second, the authors suggested using the criteria related to the presence of, for instance, neck pain or temporomandibular disorders with some prudence, as these complaints can also co-exist with tinnitus without there being a causal relation [23]. Although their presence strengthens the ST diagnosis in case it is combined with another criterion, such as tinnitus and neck or jaw pain complaints appeared simultaneously [17].
Fig. 2.
Diagnostic criteria for somatosensory tinnitus [17]
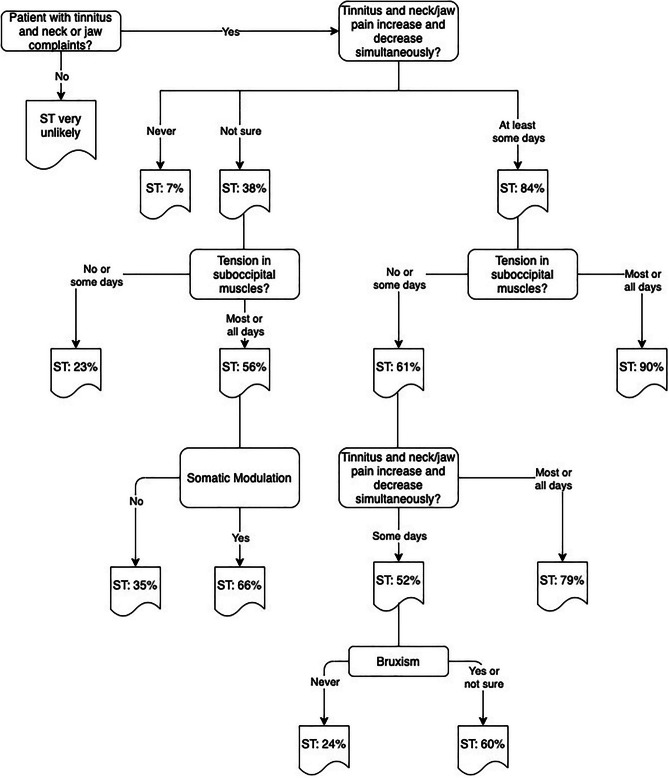
After publication of the new set of 16 criteria, the diagnostic value of all criteria separately was investigated in a group of 8221 participants with and without somatic influence on their tinnitus [24]. This analysis showed that the simultaneous onset or increase and decrease of both tinnitus and pain complaints have the highest positive likelihood ratio (LR) (6.29 and 10.72, respectively). These two criteria are thus the strongest to use as a single criterion.
On the contrary, a patient’s ability to modulate their tinnitus through voluntary movements or pressure on the head or neck appeared to have very little diagnostic value when used as a single criterion (LR + : 1.81 and LR − : 0.82) [24].
Additionally, the mere presence of neck or jaw complaints in patients with tinnitus was shown to have limited additional value as well, as the presence of these criteria only increased the probability of a ST diagnosis to about 50% [24].
In general, the analysis showed that the specificity of the 16 criteria to diagnose ST was high, but the sensitivity was rather low [24] (see Fig. 3 for more details). This implicates a relatively high risk of false negatives, which is not ideal as we do not want to leave these patients without a referral for a potentially effective treatment.
Fig. 3.
Diagnostic value of diagnostic criteria for somatosensory tinnitus [24]
To solve this risk of false negatives, the authors advise using a combination of criteria before diagnosing a patient with ST. A follow-up study was completed to find the most ideal combination of diagnostic criteria to have the highest accuracy, sensitivity, and specificity.
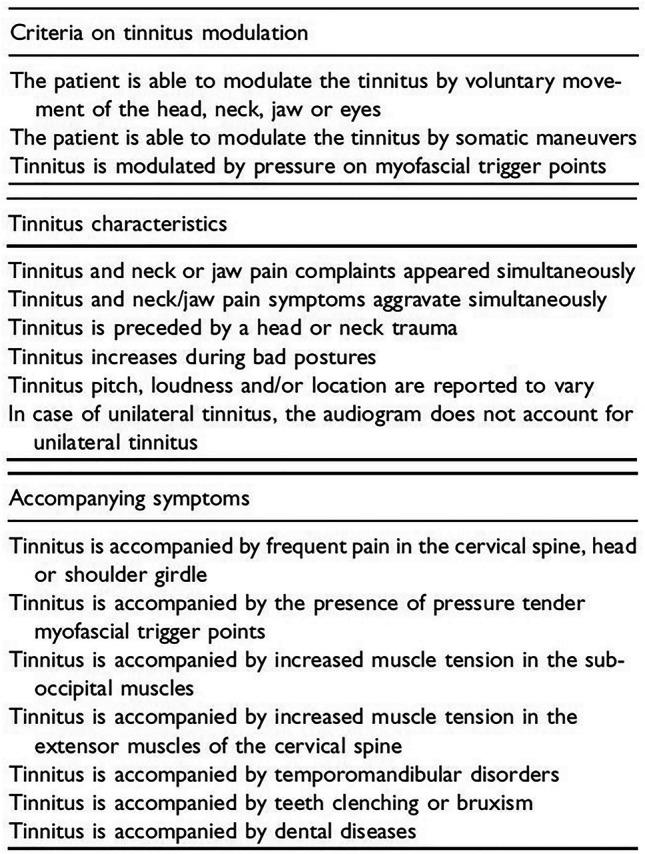
Based on data from 7981 participants with tinnitus, a decision tree for ST diagnosis was constructed [25]. The decision tree includes four of the sixteen original criteria: tinnitus and neck/jaw pain increase/decrease simultaneously, tension in suboccipital muscles, somatic modulation, and bruxism. The model presented in Fig. 4 has an accuracy of 82.2%, a sensitivity of 82.5%, and a specificity of 79% [25].
Fig. 4.
Rapid screening for somatosensory tinnitus tool [25]
Somatic Tinnitus Treatment
Musculoskeletal Treatment
Currently, most ST treatment approaches are based on techniques that are mainly applied by physiotherapists or in chiropractic or osteopathic care, depending on regional differences. The main rationale for using these techniques in patients with somatosensory tinnitus is to normalize somatosensory input. In patients with somatosensory tinnitus, this somatosensory afference is often altered by increased muscle tension or restricted movement in the upper cervical spine or temporomandibular joint. Specific techniques are then used to decrease muscle tension and increase mobility and stability so that somatosensory afference will be restored and tinnitus perception decreases. The choice of specific techniques will largely depend on the dysfunction that is found in an individual patient. Therefore, somatosensory tinnitus management should be seen as a patient-centered therapy that should be tailored to the specific patient’s needs.
For cervical spine treatment, clinical practice guidelines [26, 27] advise a combination of techniques to restore cervical spine function and reduce pain complaints. Primarily, counseling techniques are used to improve the patient’s knowledge about neck pain and to advise the patient towards good posture and movement habits. Additionally, exercises are recommended to improve the strength, coordination, and endurance of the stabilizing neck and shoulder girdle muscles. Training these small muscles, which are located close to the vertebrae, will not only increase cervical spine stability but will also result in long-term reduction of excessive tension in the larger, more superficially located muscles that are often involved in somatosensory tinnitus.
In addition to the core content of counseling and exercises, other techniques can be added depending on the neck dysfunctions that are most prominent in an individual patient. As such, manual mobilizations or manipulations can be used to improve cervical spine mobility when needed. Other techniques, such as ischemic pressure or dry needling to deactivate myofascial trigger points, can also be included in this approach, as long as they are used to support the effect of the core content.
For the treatment of temporomandibular disorders (TMD), three systematic reviews [28–30] show that a combination of exercises and manual techniques is effective. Exercises comprise passive and active stretching of the masticatory muscles and postural exercises to improve the head and neck posture. Myofeedback can be used during exercises to guide patients while relaxing their masticatory muscles. Manual techniques comprise manual mandibular traction or translation and myofascial release techniques of the masticatory muscles. Apart from local treatment of the temporomandibular area, adding cervical spine mobilizations and exercises is recommended when clinical investigation shows additional dysfunctions in the cervical spine.
Apart from the combination of exercises and manual techniques, TMD treatment should also include counseling to address the underlying causes of TMD. Often advice on mouth habits (bruxism, biting nails, chewing gum, etc.), stress reduction, and sleep hygiene will be added. As bruxism is often related to TMD, unlearning clenching or grinding habits will be essential in TMD treatment. In case of nighttime bruxism, occlusal splint therapy can be added. When stress reduction is needed, relaxation therapies such as mindfulness and breathing exercises can be added to the treatment.
In previous years, seven studies [31–37] were published that investigated such a patient-centered multimodal musculoskeletal approach. All studies used a combination of techniques and exercises to treat the neck and/or jaw region according to the current state-of-the-art and tailored the exact content of the therapy to the patient’s specific dysfunctions. Neck or temporomandibular disorder counseling, to advise patients in controlling their neck or jaw pain complaints, is always part of such a multimodal approach. Additionally, techniques are applied to decrease muscle tension in the neck or masticatory muscles. These techniques can be passive, such as ischemic pressure techniques or dry needling on myofascial trigger points, but active stretching exercises are also frequently used. Additionally, selective strengthening of deep neck flexor and extensor muscles is often used to achieve a long-term reduction in muscle tension of the trapezius and sternocleidomastoid muscles. Furthermore, manual mobilizations or manipulations of the cervical spine and temporomandibular joint are often used to treat limited mobility.
In patients with neck-related somatosensory tinnitus, this approach showed a significant decrease in tinnitus functional index (TFI) score after 6 weeks of treatment (p = 0.04) [33] and a significant decrease in VAS for tinnitus loudness (p = 0.01) after a maximum of 12 treatment sessions [34]. Additional analysis showed that patients whose tinnitus increases during episodes of neck pain or certain postures and patients with low-pitched tinnitus were more likely to benefit from this type of treatment [38].
In patients with primary temporomandibular-related ST, the multimodal approach showed a significant decrease in TFI score after 9 weeks of treatment in 80 patients (p < 0.001) [35]. Similar results were found in two other studies, showing a significant decrease in VAS-loudness (p < 0.001), VAS-annoyance (p < 0.001), and Tinnitus Handicap Inventory (THI) (p < 0.001) in 31 patients [31] and a significant decrease in VAS-severity (p < 0.001) in 61 patients [32].
Apart from the multimodal approach, specific musculoskeletal techniques have also been studied as single treatment options for somatosensory tinnitus [39–42].
Atan et al. [39] investigated the effect of Kinesiotape application on the sternocleidomastoid, upper trapezius, and levator scapulae muscles in 15 patients with neck-related somatosensory tinnitus. Kinesiotape is a type of elastic tape that is applied to decrease muscle tension or provide proprioceptive input. The use of this tape on all three muscles resulted in an average decrease in THI score of 13.06 points (p = 0.001).
Four other studies used myofascial trigger point deactivation techniques on muscles in the head-neck region as a way to decrease muscle tension. Rocha et al. [42] treated 37 patients with somatosensory tinnitus using ischemic pressure to deactivate the myofascial trigger points. They showed a significant decrease in THI and VAS-annoyance after 5 sessions (p < 0.001).
Three other studies investigated dry needling, a technique that uses acupuncture needles for myofascial trigger point deactivation. All studies showed good effects of dry needling on numerical rating scale (NRS) scores for tinnitus severity [40], NRS for tinnitus loudness [43], and THI [37, 43] in patients with ST.
Finally, Wu et al. [41] showed a decrease of 44 point on the THI after deep neck flexor exercises in one case of neck-related somatosensory tinnitus.
Other Management Techniques
Apart from the studies on musculoskeletal management of somatosensory tinnitus, other techniques to normalize somatosensory afference have been investigated. It must be noted that these treatments were often investigated in small samples without a control group and risk of bias of these studies is high. Some of them have not been repeated in the literature, so the effect needs to be confirmed in larger controlled studies before general use can be recommended.
Two studies used transcutaneous electrical nerve stimulation (TENS) as a comparison to musculoskeletal treatment of the cervical spine. One study comparing 2 groups of 20 patients showed similar significant decreases in THI score after TENS treatment of the cervical spine then after cervical spine manipulation [44]. As second non-randomized trial showed significant improvement on a self-developed questionnaire when comparing the effect of cervical spine exercises to TENS applied to the ear in two groups of 40 patients [45]. No significant differences between groups were found in both studies.
One case study showed positive effects of intermittent cervical collar application (15 to 30 min, 3–5 times a day), with complete tinnitus remission within 4 weeks [46]. This remission lasted for 5 months. Afterward, the tinnitus slightly resurged occasionally but disappeared again after short-term application of the cervical collar (15 min once every 2–4 weeks).
In 2005, one study reported the use of subcutaneous botulinum toxin type A injections around the ear for treatment in patients with unilateral or bilateral non-pulsatile tinnitus [47]. The author’s rationale for using these injections as a treatment for tinnitus was the blockage of autonomic pathways [47]. This study showed a significant decrease in average THI scores from baseline to 4 months after the injection in a group of 26 patients. No significant decrease was found in the group receiving a placebo injection. The authors indicated that further research was necessary to confirm these results. Unfortunately, no additional studies have been published on the topic in the meantime.
Another study used a cervical epidural steroid injection at level C4 to reduce tinnitus intensity by 75% in one patient [48]. This effect persisted for 5 weeks; hereafter, tinnitus intensity gradually increased again to get back to baseline after another 9 weeks. The authors hypothesize that the observed effect of the injection is a result of a steroid-induced reduction in afferent signaling from the cervical region, resulting in decreased neural activity along the auditory-somatic pathway [48].
Contrary to most techniques that have been suggested for the management of somatosensory tinnitus, Marks et al. [49] proposed a technique to influence the medullary connection between the auditory and somatosensory pathways in a more direct way. The combination of auditory and electrical vagus nerve stimulation showed a significant reduction in TFI score in a group of 20 patients with unilateral pure-tone tinnitus that could be modulated by one or more somatic maneuvers. A larger study using the same technique was recently published, showing a clinically relevant decrease of at least 13 points on the TFI in 65% of a group of 99 patients [50]. Additional studies are needed to confirm these results and to investigate the effect of this treatment in a less-restricted sample of patients with somatosensory tinnitus.
Apart from the therapy options that are directed at normalizing somatosensory input or influencing the medullary auditory-somatosensory connection, one study investigated the effect of tinnitus retraining therapy (TRT) in patients with somatosensory tinnitus [51]. Patients underwent a 3-month TRT protocol, including daily use of white noise generators with or without amplifications, combined with four structured counseling sessions. An average decrease in THI score of 34.95 points was found (p < 0.05).
Conclusion
Somatosensory tinnitus, where changes in the somatosensory afference have an influence on the tinnitus pitch or loudness, can be recognized using the set of 16 diagnostic criteria published in 2018. As a single criterion, the Tinnitus and neck/jaw pain increase/decrease simultaneously criterion has the most value. But using the combination of four criteria presented in the decision tree will enable clinicians and researchers to recognize patients with ST with higher accuracy, sensitivity, and specificity.
Once diagnosed, ST can be successfully treated using a variety of techniques. Currently, musculoskeletal treatment of the cervical spine and temporomandibular area has the highest level of evidence. Other techniques have been suggested but need further investigation in large RCTs, as their level of evidence is currently low. Mostly, somatosensory tinnitus treatment shows a decrease in tinnitus severity or loudness, but in rare cases, total remission of the tinnitus is achieved.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Baguley D, McFerran D, Hall D. Tinnitus. Lancet. 2013;382(9904):1600–1607. doi: 10.1016/S0140-6736(13)60142-7. [DOI] [PubMed] [Google Scholar]
- 2.Hiller W, Janca A, Burke KC. Association between tinnitus and somatoform disorders. J Psychosom Res. 1997;43(6):613–624. doi: 10.1016/s0022-3999(97)00188-8. [DOI] [PubMed] [Google Scholar]
- 3.Pinchoff RJ, Burkard RF, Salvi RJ, Coad ML, Lockwood AH. Modulation of tinnitus by voluntary jaw movements. Am J Otol. 1998;19(6):785–789. [PubMed] [Google Scholar]
- 4.van Dijk P, Vanneste S. Neuroimaging as a window on the heterogeneity of tinnitus. ENT Audiol News. 2016;24:73–74. [Google Scholar]
- 5.Elgoyhen AB, Langguth B, De Ridder D, Vanneste S. Tinnitus: perspectives from human neuroimaging. Nat Rev Neurosci. 2015;16(10):632–642. doi: 10.1038/nrn4003. [DOI] [PubMed] [Google Scholar]
- 6.Levine RA. Somatic (craniocervical) tinnitus and the dorsal cochlear nucleus hypothesis. Am J Otolaryngol. 1999;20(6):351–362. doi: 10.1016/S0196-0709(99)90074-1. [DOI] [PubMed] [Google Scholar]
- 7.Shore S, Zhou J, Koehler S (2007) Neural mechanisms underlying somatic tinnitus. In: Langguth B, Hajak G, Kleinjung T, Cacace A, Møller AR (eds) Tinnitus: pathophysiology and treatment. Progress in Brain Research volume 166, pp 107–123; Elsevier [DOI] [PMC free article] [PubMed]
- 8.Zhou J, Shore S. Convergence of spinal trigeminal and cochlear nucleus projections in the inferior colliculus of the guinea pig. J Comp Neurol. 2006;495(1):100–112. doi: 10.1002/cne.20863. [DOI] [PubMed] [Google Scholar]
- 9.Kanold PO, Young ED. Proprioceptive information from the pinna provides somatosensory input to cat dorsal cochlear nucleus. J Neurosci. 2001;21(19):7848–7858. doi: 10.1523/JNEUROSCI.21-19-07848.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou J, Shore S. Projections from the trigeminal nuclear complex to the cochlear nuclei: a retrograde and anterograde tracing study in the guinea pig. J Neurosci Res. 2004;78(6):901–907. doi: 10.1002/jnr.20343. [DOI] [PubMed] [Google Scholar]
- 11.Wright DD, Ryugo DK. Mossy fiber projections from the cuneate nucleus to the cochlear nucleus in the rat. J Comp Neurol. 1996;365(1):159–172. doi: 10.1002/(SICI)1096-9861(19960129)365:1<159::AID-CNE12>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 12.Shore SE, Vass Z, Wys NL, Altschuler RA. Trigeminal ganglion innervates the auditory brainstem. J Comp Neurol. 2000;419(3):271–285. doi: 10.1002/(sici)1096-9861(20000410)419:3<271::aid-cne1>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 13.Zhan X, Pongstaporn T, Ryugo DK. Projections of the second cervical dorsal root ganglion to the cochlear nucleus in rats. J Comp Neurol. 2006;496(3):335–348. doi: 10.1002/cne.20917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shore SE. Multisensory integration in the dorsal cochlear nucleus: unit responses to acoustic and trigeminal ganglion stimulation. Eur J Neurosci. 2005;21(12):3334–3348. doi: 10.1111/j.1460-9568.2005.04142.x. [DOI] [PubMed] [Google Scholar]
- 15.Jain R, Shore S. External inferior colliculus integrates trigeminal and acoustic information: unit responses to trigeminal nucleus and acoustic stimulation in the guinea pig. Neurosci Lett. 2006;395(1):71–75. doi: 10.1016/j.neulet.2005.10.077. [DOI] [PubMed] [Google Scholar]
- 16.Lanting CP, de Kleine E, Eppinga RN, van Dijk P. Neural correlates of human somatosensory integration in tinnitus. Hear Res. 2010;267(1–2):78–88. doi: 10.1016/j.heares.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 17.Michiels S, Ganz Sanchez T, Oron Y, Gilles A, Haider HF, Erlandsson S, et al. Diagnostic criteria for somatosensory tinnitus: a Delphi process and face-to-face meeting to establish consensus. Trends Hear. 2018;22:2331216518796403. doi: 10.1177/2331216518796403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van de Heyning P, Gilles A, Rabau S, Van Rompaey V. Subjective tinnitus assessment and treatment in clinical practice: the necessity of personalized medicine. Curr Opin Otolaryngol Head Neck Surg. 2015;23(5):369–375. doi: 10.1097/MOO.0000000000000183. [DOI] [PubMed] [Google Scholar]
- 19.Cederroth CR, Gallus S, Hall DA, Kleinjung T, Langguth B, Maruotti A, et al. Editorial: towards an understanding of tinnitus heterogeneity. Front Aging Neurosci. 2019;11:53. doi: 10.3389/fnagi.2019.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanchez TG, Rocha CB. Diagnosis and management of somatosensory tinnitus: review article. Clinics (Sao Paulo, Brazil) 2011;66(6):1089–1094. doi: 10.1590/S1807-59322011000600028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Biesinger E, Groth A, Hoing R, Holzl M. Somatosensoric tinnitus. HNO. 2015;63(4):266–271. doi: 10.1007/s00106-014-2971-9. [DOI] [PubMed] [Google Scholar]
- 22.Ward J, Vella C, Hoare DJ, Hall DA (2015) Subtyping somatic tinnitus: a cross-sectional UK cohort study of demographic, clinical and audiological characteristics. PLoS ONE 10(5). 10.1371/journal.pone.0126254 [DOI] [PMC free article] [PubMed]
- 23.Michiels S, Van de Heyning P, Truijen S, De Hertogh W (2015) Diagnostic value of clinical cervical spine tests in patients with cervicogenic somatic tinnitus. Phys Ther 95(11):1529–1535. 10.2522/ptj.20140457 [DOI] [PubMed]
- 24.Michiels S, Cardon E, Gilles A, Goedhart H, Vesala M, Schlee W. Somatosensory tinnitus diagnosis: diagnostic value of existing criteria. Ear Hear. 2022;43(1):143–149. doi: 10.1097/AUD.0000000000001105. [DOI] [PubMed] [Google Scholar]
- 25.Michiels S, Cardon E, Gilles A, Goedhart H, Vesala M, Van Rompaey V, et al. The rapid screening for somatosensory tinnitus tool: a data-driven decision tree based on specific diagnostic criteria. Ear Hear. 2022 doi: 10.1097/AUD.0000000000001224. [DOI] [PubMed] [Google Scholar]
- 26.Cohen SP, Hooten WM (2017) Advances in the diagnosis and management of neck pain. BMJ 358:j3221. 10.1136/bmj.j3221 [DOI] [PubMed]
- 27.Cote P, Wong JJ, Sutton D, Shearer HM, Mior S, Randhawa K, et al. Management of neck pain and associated disorders: a clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur Spine J : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2016;25(7):2000–2022. doi: 10.1007/s00586-016-4467-7. [DOI] [PubMed] [Google Scholar]
- 28.Martins WR, Blasczyk JC, Aparecida Furlan de Oliveira M, Lagôa Gonçalves KF, Bonini-Rocha AC, Dugailly PM et al (2016) Efficacy of musculoskeletal manual approach in the treatment of temporomandibular joint disorder: a systematic review with meta-analysis. Man Ther 21:10–7. 10.1016/j.math.2015.06.009 [DOI] [PubMed]
- 29.Armijo-Olivo S, Pitance L, Singh V, Neto F, Thie N, Michelotti A. Effectiveness of manual therapy and therapeutic exercise for temporomandibular disorders: systematic review and meta-analysis. Phys Ther. 2016;96(1):9–25. doi: 10.2522/ptj.20140548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Calixtre LB, Moreira RF, Franchini GH, Alburquerque-Sendin F, Oliveira AB. Manual therapy for the management of pain and limited range of motion in subjects with signs and symptoms of temporomandibular disorder: a systematic review of randomised controlled trials. J Oral Rehabil. 2015;42(11):847–861. doi: 10.1111/joor.12321. [DOI] [PubMed] [Google Scholar]
- 31.Côté C, Baril I, Morency C, Montminy S, Couture M, Leblond J, et al. Long-term effects of a multimodal physiotherapy program on the severity of somatosensory tinnitus and identification of clinical indicators predicting favorable outcomes of the program. J Am Acad Audiol. 2019;30(8):720–730. doi: 10.3766/jaaa.17147. [DOI] [PubMed] [Google Scholar]
- 32.Delgado de la Serna P, Plaza-Manzano G, Cleland J, Fernández-de-Las-Peñas C, Martín-Casas P, Díaz-Arribas MJ (2020) Effects of cervico-mandibular manual therapy in patients with temporomandibular pain disorders and associated somatic tinnitus: a randomized clinical trial. Pain Med 21(3):613–24. 10.1093/pm/pnz278 [DOI] [PubMed]
- 33.Michiels S, Van de Heyning P, Truijen S, Hallemans A, De Hertogh W. Does multi-modal cervical physical therapy improve tinnitus in patients with cervicogenic somatic tinnitus? Man Ther. 2016;26:125–131. doi: 10.1016/j.math.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 34.Oostendorp RA, Bakker I, Elvers H, Mikolajewska E, Michiels S, De Hertogh W, et al. Cervicogenic somatosensory tinnitus: an indication for manual therapy plus education? Part 2: A pilot study. Man Ther. 2016;23:106–113. doi: 10.1016/j.math.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 35.Van der Wal A, Michiels S, Van de Heyning P, Braem M, Visscher C, Topsakal V et al (2020) Treatment of somatosensory tinnitus: a randomized controlled trial studying the effect of orofacial treatment as part of a multidisciplinary program. J Clin Med 9(3). 10.3390/jcm9030705 [DOI] [PMC free article] [PubMed]
- 36.Eladl HM, Elkholi SM, Eid MM, Abdelbasset WK, Ali ZA, Bahey El-Deen HA (2022) Effect of adding a supervised physical therapy exercise program to photobiomodulation therapy in the treatment of cervicogenic somatosensory tinnitus: a randomized controlled study. Medicine (Baltimore) 101(31):e29946. 10.1097/MD.0000000000029946 [DOI] [PMC free article] [PubMed]
- 37.Campagna CA, Anauate J, Vasconoelos LGE, Oiticica J. Effectiveness of dry needling in bothersome chronic tinnitus in patients with myofascial trigger points. Int Arch Otorhinolaryngol. 2022;26(2):e233–e242. doi: 10.1055/s-0041-1730429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Michiels S, Van de Heyning P, Truijen S, Hallemans A, De Hertogh W. Prognostic indicators for decrease in tinnitus severity after cervical physical therapy in patients with cervicogenic somatic tinnitus. Musculoskelet Sci Pract. 2017;29:33–37. doi: 10.1016/j.msksp.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 39.Atan T, Atan D, Özel S (2020) Effectiveness of Kinesio taping in the treatment of somatosensory tinnitus: a randomized controlled trial. Complement Ther Clin Pract 39:101100. 10.1016/j.ctcp.2020.101100 [DOI] [PubMed]
- 40.Sajadi S, Forogh B, ZoghAli M. Cervical trigger point acupuncture for treatment of somatic tinnitus. J Acupunct Meridian Stud. 2019;12(6):197–200. doi: 10.1016/j.jams.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 41.Wu D, Ham D, Rosedale R. Physiotherapy assessment and treatment of chronic subjective tinnitus using mechanical diagnosis and therapy: a case report. J Man Manip Ther. 2020;28(2):119–126. doi: 10.1080/10669817.2020.1714160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rocha CB, Sanchez TG. Efficacy of myofascial trigger point deactivation for tinnitus control. Braz J Otorhinolaryngol. 2012;78(6):21–26. doi: 10.5935/1808-8694.20120028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Womack A, Butts R, Dunning J (2020) Dry needling as a novel intervention for cervicogenic somatosensory tinnitus: a case study. Physiother Theory Pract 38:1319–1327. 10.1080/09593985.2020.1825579 [DOI] [PubMed]
- 44.Bonaconsa A, Mazzoli M, Magnano SLA, Milanesi C, Babighian G. Posturography measures and efficacy of different physical treatments in somatic tinnitus. Intl Tinnitus J. 2010;16(1):44–50. [PubMed] [Google Scholar]
- 45.Mielczarek M, Konopka W, Olszewski J. The application of direct current electrical stimulation of the ear and cervical spine kinesitherapy in tinnitus treatment. Auris Nasus Larynx. 2013;40(1):61–65. doi: 10.1016/j.anl.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 46.Bechter K, Wieland M, Hamann GF. Chronic cervicogenic tinnitus rapidly resolved by intermittent use of cervical collar. Front Psych. 2016;7:43. doi: 10.3389/fpsyt.2016.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stidham KR, Solomon PH, Roberson JB (2005) Evaluation of botulinum toxin A in treatment of tinnitus. Otolaryngol Head Neck Surg 132(6):883–9. 10.1016/j.otohns.2005.02.015 [DOI] [PubMed]
- 48.McCormick ZL, Walega DR. Cervical epidural steroid injection for refractory somatic tinnitus. Pain Pract. 2015;15(2):e28–33. doi: 10.1111/papr.12255. [DOI] [PubMed] [Google Scholar]
- 49.Marks KL, Martel DT, Wu C, Basura GJ, Roberts LE, Schvartz-Leyzac KC et al (2018) Auditory-somatosensory bimodal stimulation desynchronizes brain circuitry to reduce tinnitus in guinea pigs and humans. Sci Transl Med 10(422). 10.1126/scitranslmed.aal3175 [DOI] [PMC free article] [PubMed]
- 50.Jones GR, Martel DT, Riffle TL, Errickson J, Souter JR, Basura GJ et al (2023) Reversing synchronized brain circuits using targeted auditory-somatosensory stimulation to treat phantom percepts: a randomized clinical trial. JAMA Netw Open 6(6):e2315914. 10.1001/jamanetworkopen.2023.15914 [DOI] [PMC free article] [PubMed]
- 51.Ostermann K, Lurquin P, Horoi M, Cotton P, Herve V, Thill MP. Somatic tinnitus prevalence and treatment with tinnitus retraining therapy. B-ENT. 2016;12(1):59–65. [PubMed] [Google Scholar]