Abstract
Background
Cervical pain has a high incidence and worldwide socio-economic effect. Its incidence is lower in men than in women. Conservative and non-pharmacological therapeutic options include strength training. Elastic bands are commonly used in physiotherapy clinics for strength work in patients. Consequently, the objective of this research was to analyse the efficacy of an exercise therapy programme using elastic bands on decreasing pain and increasing strength of the neck flexor musculature, cervical extensor, and scapular stabilizing musculature in women suffering from non-specific cervical pain.
Methods
A randomised clinical trial was carried out with 35 subjects with non-specific neck pain (age = 51.7 ± 9.5 and baseline intensity of pain in Visual Analogue Scale = 52.4 ± 9.6). The experimental group (n = 18) performed the exercise programme with elastic bands, consisting of a total of 16 sessions that lasted 45 min. The control group, consisting of 27 participants, reported that they maintained their usual lifestyle throughout the study. The evaluation tools used in this research included the Visual Analogue Scale, Neck Flexor Endurance Test, Neck Extensor Muscle Endurance Test, and Scapular Muscle Endurance Test.
Results
The experimental group obtained significant improvements in the measurements taken using the Visual Analogue Scale (p < 0.001, d = 4.2), the Neck Flexor Endurance Test (p < 0.001, d = 3.4), the Neck Extensor Endurance Test (p < 0.001, d = 6.3), in the Scapular Muscle Endurance Test (p = 0.016, d = 0.9).
Conclusions
The assessed exercise therapy program utilizing elastic bands demonstrated favorable outcomes in managing non-specific neck discomfort. This intervention resulted in pain reduction and enhanced endurance of the cervical flexor and extensor muscles, along with improved endurance of the scapular stabilizing muscles.
Protocol registration in ClinicalTrials.gov: NCT05433649 (registered prospectively, date of registration: June 27, 2022).
Keywords: Exercise therapy, Neck pain, Women health, Physiotherapy
List of abbreviations
- EBP
Elastic band exercise therapy programme
- NEET
Neck Extensor Muscle Endurance Test
- NFET
Neck Flexor Endurance Test
- NNP
Non-specific neck pain
- SMET
Scapular Muscle Endurance Test
- VAS
Visual Analogue Scale
Introduction
Non-specific neck pain (NNP) is a common condition among the general population and one of the leading diseases that pose a burden in terms of overall years lived with disability (9th place for women and 11th place for men) [1,2]. NNP has a higher incidence in adult women and among individuals aged 39–69 years [3,4]. The socio-economic consequences of neck pain are considerable and this cost has increased in recent years due to lost productivity, increased sick leave and healthcare costs [1,5,6].
It is important to treat this condition effectively, not only for symptom relief but also for the prevention of recurrent episodes of neck pain, personal suffering and loss of work productivity [3,7]. The osteoligamentous system contributes 20 % to the mechanical stability of the cervical spine, while 80 % of such stability is provided by the neck musculature [8]. Several investigations [[9], [10], [11], [12], [13], [14], [15]] suggest that a lack of strength in the muscles of the neck and shoulder girdle stabilisers can cause neck pain. These studies have found significant reductions in isometric strength in the neck flexor and extensor muscles in patients with chronic neck pain compared to healthy controls [9,10,12,13,15]. Leading clinical practice guidelines emphasise the importance of resistance and strength exercise in the treatment of NNP [16,17]. Conventional strength training equipment is relatively large and expensive, whereas elastic resistance bands can be used as a viable alternative for strength endurance work in small clinics or at home, as they are inexpensive and easy to transport [[18], [19], [20], [21]].
Thus, the objective of this investigation was to evaluate the impact of an elastic band exercise therapy programme (EBP) on pain levels and endurance of the cervical flexor musculature, cervical extensor musculature, and scapular stabilizing musculature in women aged 18–65 years with non-specific neck pain (NNP). This population group was chosen because, according to the literature, adult women are the ones who suffer the most from this condition [3,22]. The research hypothesis posited that implementing EBP would lead to favorable outcomes in terms of reducing pain and enhancing the strength endurance of the cervical flexor, cervical extensor, and scapular stabilizing muscles in female individuals with NNP when compared to patients with the same condition who did not undergo the EBP intervention.
Materials and methods
Study design and sample
A randomized controlled clinical trial was carried out to compare the scores on dependent variables before and after the intervention in two distinct groups: the experimental group (comprising individuals who participated in the EBP) and the control group (comprising individuals who did not partake in the EBP). The study protocol received approval from the University of León Research Ethics Committee under code 040–2022 and was prospectively registered on ClinicalTrials.gov (NCT05433649) on June 27, 2022. This study was conducted in accordance with the Declaration of Helsinki (2013 version). All participants were provided with information regarding the research's benefits and risks, and they willingly signed written informed consent documents.
We conducted a non-probabilistic purposive sampling at the Municipal Sports Centre of Pontevedra (Spain). A total of sixty volunteers were selected based on the following inclusion criteria: (i) age between 18 and 65 years; (ii) experiencing NNP for at least three months, with pain intensity ranging from 30 to 70 on the Visual Analogue Scale (VAS). Exclusion criteria were also applied, which included: (i) a history of previous neck or shoulder surgery, medical diagnosis of fibromyalgia, cervical radiculopathy/myelopathy, a prior history of whiplash injury, or cognitive disorders; (ii) missing more than two sessions of the BSP; (iii) failing to attend the measurement sessions.
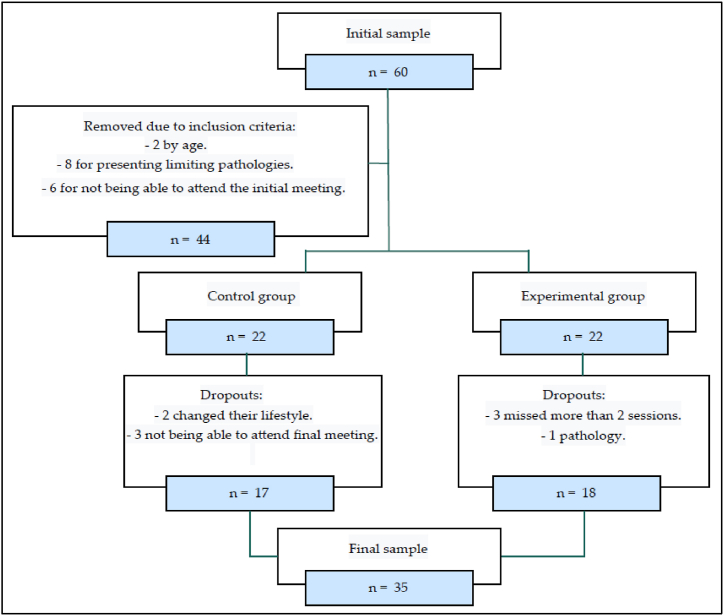
After applying the specified inclusion and exclusion criteria, the final sample comprised 44 participants. These participants were randomly assigned to two groups at a 1:1 ratio using a computer-generated random sequence, which was conducted in a blinded manner to the investigator. The allocation was concealed by sealing the group assignments in opaque envelopes. Participants and physical therapists were not blinded. Only the person who analysed the data was blinded. Throughout the course of the study, there were a total of nine dropouts, with five of them being from the control group (two individuals changed their lifestyle, and three were unable to attend the final meeting) and four belonging to the experimental group (three individuals missed more than two sessions, and another had bronchitis). The ultimate count of participants amounted to 35 (as depicted in Fig. 1).
Fig. 1.
Sample selection flowchart.
Study variables
Two assessment sessions were conducted at the commencement and the conclusion of the intervention, during which sociodemographic and anthropometric data were gathered, including age, gender, weight (measured with a Tanita™ b303 scale, Tokyo, Japan), and height (measured using a standardized Seca™ 709 height rod, Hamburg, Germany). Participants were instructed to stand with their feet together, barefoot, and with their head aligned with the Frankfort plane.
-
(a)
Pain Intensity: The VAS is a commonly used tool for pain measurement. Participants were asked to mark their perceived pain intensity on a 100 mm horizontal line. The left end represented the absence or lowest intensity of pain, while the right end denoted the highest intensity of pain [23].
-
(b)
Neck Flexor Muscle Endurance: Neck flexor strength endurance was assessed using the Neck Flexor Endurance Test (NFET). In a supine position, participants were instructed to flex their upper cervical spine, lifting their head approximately 2.5 cm away from the table and maintaining this position for as long as possible. The duration of the test was recorded in seconds and concluded when participants either lowered their head or were unable to sustain craniocervical flexion [24].
-
(c)
Neck Extensor Muscle Endurance: The Neck Extensor Muscle Endurance Test (NEET) was employed to assess cervical extensor strength endurance. Participants assumed a prone position with their head in a neutral position, arms at their sides, and a Velcro stabiliser strap positioned at the level of the sixth dorsal vertebra. An inclinometer and strap were secured around the participants' heads, with a 2 kg weight suspended from it. Participants were instructed to support this weight for as long as possible while keeping their head in a neutral position. The test's duration was recorded in seconds and concluded when participants were unable to maintain the neutral head position [25].
-
(d)
Scapular Stabiliser Endurance: The Scapular Muscle Endurance Test (SMET) was employed to assess the endurance of the scapular stabilizing muscles. Participants assumed a standing position with their shoulders and elbows flexed at 90°. Their elbows were held approximately shoulder-width apart using a ruler, and they were instructed to pull on both ends of the dynamometer by externally rotating their shoulders until it registered a force of 1 kg. Participants were then asked to sustain this position for as long as possible, and the test's duration was recorded in seconds [26].
Intervention and procedure
The intervention involved a strength programme utilizing elastic bands. This programme was conducted over a duration of eight weeks, featuring two sessions each week, amounting to a total of 16 sessions, each lasting 45 min. These sessions were supervised by a registered physiotherapist and followed a structured format comprising a warm-up, the main portion, and a cool-down. The warm-up segment spanned 10 min, during which joint mobility exercises were performed. The main part occupied 30 min, involving exercises focused on strength endurance and proprioception, utilizing elastic bands to target the cervical and scapular regions. Active breaks within this segment included gentle joint mobility exercises. The Thera Band© elastic bands were utilized, including the yellow band (1.3 kg at 100 % elongation), red band (1.7 kg at 100 % elongation), green band (2.1 kg at 100 % elongation), and blue band (2.6 kg at 100 % elongation) [27]. The first five sessions involved the yellow band, sessions six to nine involved the red band, sessions 10 to 13 involved the green band, and the last three sessions involved the blue band. Following this, an increase of 25 % in the pull-force was introduced by adjusting the resistance of the elastic band. The cool-down period extended for 5 min, during which the emphasis was on flexibility and relaxation exercises.
Statistical analysis
We performed descriptive statistical analyses of the sample using mean values, standard deviations, and median values. Normal distribution of the data was assessed using the Kolmogorov-Smirnov test and checked for homogeneity of variance using Levene's test. Changes in baseline and between-group differences after the intervention were analysed using the Student's t-test for independent samples. Additionally, we calculated effect sizes using Cohen's d statistic, categorized as small (d = 0.1–0.5), medium (d = 0.5–0.8), or large (d > 0.8) [28]. The significance level was set at p < 0.05. All statistical analyses were conducted using Stata 16.0 software for MacOS® (Stata Corporation, College Station, TX, USA).
Results
The sample consisted of 35 women. Table 1 shows the pre-intervention values. At the commencement of the study, no significant differences were observed between the two groups. A post-hoc power analysis, based on the final sample size (n = 35), yielded a value of 0.9 for p < 0.05, indicating a strong statistical power [29]. There were no significant differences in the variables of interest between the final sample and the dropouts throughout the study.
Table 1.
Baseline of the studied variables.
| Variable | All (n = 35) |
EG (n = 18) |
CG (n = 17) |
pv | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD | P50 | Mean ± SD | P50 | Mean ± SD | P50 | ||
| Age (Years) | 51.7 ± 9.5 | 53 | 51.9 ± 7.8 | 51.5 | 51.4 ± 11.3 | 54 | 0.86 |
| Weight (kg) | 56 ± 3.4 | 55.5 | 55.3 ± 3.1 | 54.6 | 56.7 ± 3.7 | 56 | 0.22 |
| Height (cm) | 157.1 ± 3.5 | 156 | 156.1 ± 2.2 | 156 | 158.1 ± 4.4 | 156 | 0.08 |
| BMI (kg/m2) | 22.7 ± 0.1 | 22.7 | 22.7 ± 0.9 | 22.7 | 22.7 ± 1.3 | 22.8 | 0.99 |
| VAS | 52.4 ± 9.6 | 50 | 50.8 ± 10.6 | 50 | 54.1 ± 8.3 | 55 | 0.32 |
| NFET | 47.8 ± 8 | 50 | 47.1 ± 7.9 | 47.5 | 48.5 ± 8.3 | 50 | 0.62 |
| NEET | 164.7 ± 38.2 | 167 | 161.8 ± 35.3 | 158 | 167.9 ± 41.8 | 168 | 0.64 |
| SMET | 64.5 ± 10.1 | 68 | 64.3 ± 9.4 | 65.5 | 64.8 ± 11 | 68 | 0.88 |
VAR: Dependent variable; CG: Control group; EG: Experimental group; SD: Standard deviation; P50: Median; BMI: Body mass index; NFET: Neck flexor muscle endurance test; NEET: Neck extensor muscle endurance test; SMET: Scapular muscle endurance test.
As shown in Table 2, we found statistical differences in the measures obtained in the VAS between groups (mean difference: −18.3, 95 % CI: −24.7 to −11.8, p < 0.001, d = 4.2). We observed a large effect size and a 21.9 % improvement in pain. In the NFET, we identified significant differences between the groups (mean difference: 6.4, 95 % CI: 5.1 to 7.6, p < 0.001, d = 3.4). This was associated with a significant effect size and a 14.8 % enhancement in the strength of the flexor neck musculature (see Table 2).
Table 2.
Inferential statistics in the secondary outcomes between groups from baseline to post-test.
| Variable | Group | Mean ± SD Pre-test |
Mean ± SD Post-test |
Mean ± SD difference | Mean difference between groups | P value | ES |
|---|---|---|---|---|---|---|---|
| VAS | CG | 54.1 ± 8.3 | 32.6 ± 10.3 | −21.5 ± 11.1 | −18.3 | <0.001 | 4.2 |
| EG | 50.8 ± 10.6 | 11.1 ± 8.3 | −39.7 ± 7.4 | ||||
| NFET | CG | 48.5 ± 8.3 | 49.1 ± 8.4 | 0.6 ± 1.9 | 6.4 | <0.001 | 3.4 |
| EG | 47.1 ± 7.9 | 54.1 ± 6.7 | 6.9 ± 1.8 | ||||
| NEET | CG | 167.9 ± 41.8 | 168.7 ± 41.3 | 0.8 ± 6.8 | 34.5 | <0.001 | 6.3 |
| EG | 161.8 ± 35.3 | 197 ± 32.3 | 35.2 ± 3.9 | ||||
| SMET | CG | 64.8 ± 11 | 65.5 ± 11 | 0.8 ± 2.7 | 2.2 | 0.016 | 0.9 |
| EG | 64.3 ± 9.4 | 67.3 ± 9.4 | 3 ± 2.5 |
SD: Standard deviation; ES: Effect size; CG: Control group; EG: Experimental group; NFET: Neck flexor muscle endurance test; NEET: Neck extensor muscle endurance test; SMET: Scapular muscle endurance test.
In the NEET, we found statistical differences between groups (mean difference: 34.5, 95 % CI: 30.7 to 38.2, p < 0.001, d = 6.3). This was associated with a significant effect size and a 21.8 % enhancement in the strength of the extensor neck musculature (Table 2).
In the SMET, we found statistical differences between groups (mean difference: 2.2, 95 % CI: 0.5 to 4, p = 0.016, d = 0.9). This was associated with a significant effect size and a 4.7 % enhancement in the strength of the extensor neck musculature (Table 2).
Discussion
The objective of this study was to assess the impact of an intervention involving elastic bands in the treatment of NNP among adult women. The findings of the research indicate a positive outcome, encompassing pain reduction and enhancements in the strength endurance of the neck flexor, neck extensor, and scapular stabilizing musculature.
The benefits on pain reduction identified in the participants who underwent the EBP intervention were clinically important, as defined by Modarresi et al. [30]. This finding is congruent with the positive results obtained in other studies that performed exercise therapy in patients with neck pain, whose interventions also included strength endurance, proprioception and flexibility work [[31], [32], [33], [34]]. However, it is worth mentioning that these studies [[31], [32], [33], [34]] did not focus the exercise programme on elastic band work, and their samples included both sexes. A systematic review concluded that exercise is beneficial in reducing pain and disability, regardless of the exercise therapy dose, although the most common dosage of the programmes included in the mentioned review is between 12 and 24 sessions that lasted 30–60 min [35]. The intervention evaluated in this study is between these reference values. This improvement in neck pain could potentially reduce the significant socio-economic impact associated with neck pain. Neck pain poses a substantial burden on industries due to productivity losses attributed to absenteeism and presenteeism, in addition to the personal suffering stemming from pain, disability, or diminished quality of life [22]. It is worth noting that the results obtained in this study demonstrate a substantial effect size for the sample, particularly considering the mean age of 51 years, which aligns with the age group experiencing the highest incidence of NNP [3,4].
Furthermore, the improvements observed in the strength endurance of the musculature in the cervical and scapular regions are congruent. This is significant as one of the primary risk factors associated with neck pain is the deficiency in strength endurance of the neck musculature [[9], [10], [11]]; in particular, studies have shown that patients with chronic neck and shoulder pain had a decrease in the strength of the flexor and extensor muscles of the neck [12,13]. In addition, the cervical musculature has a fundamental role in stabilizing this region, especially in neutral or mid-range movements that are most commonly used in activities of daily living [36]. Previous studies have also established a connection between head posture, neck muscle strength, and the occurrence of neck pain [37]. They have emphasised the importance of the musculature in maintaining a correct cervical position and in reducing neck pain [37,38]. The high percentages and effect sizes of improvement in neck strength observed in this study align with findings from other exercise therapy research, even when the sample was not exclusively female [[39], [40], [41]].
Several studies have presented substantial evidence regarding the benefits of exercise therapy for the management of NNP [[31], [32], [33], [34]] The results from various variables in this study suggest that an EBP intervention could be advantageous for addressing NNP in women. Additionally, an examination of Clinical Practice Guidelines pertaining to neck pain treatment emphasizes the importance of exercise therapy in fostering favorable outcomes for individuals with NNP [42].
The methodological limitations of this study must be pointed out. Firstly, the dispersion
of the age of the participants, implies that ageing was not considered, and the results were not stratified by age due to the limited participant pool. Another limitation is the lack of any follow-up assessment after the two-month intervention, making it uncertain whether the observed benefits are sustained over time. Additionally, the lack of blinding, both for participants and therapists, is a notable factor to consider when analysing the results. Given the limited sample size utilized in this study, it would be prudent to suggest further research involving a larger and more diverse population, including male subjects, to attain results that can be more broadly applied. Moreover, future research should explore the potential of follow-up assessments and assess the impact of varying the duration of exercise programs. On the other hand, this is the first randomised controlled clinical trial to analyse the effects of an exercise therapy intervention with EBP on neck pain and muscle strength endurance in women with NNP.
In summary, the assessed exercise therapy program involving the use of elastic bands yielded positive outcomes in the treatment of non-specific neck pain, resulting in pain reduction and enhanced strength endurance of the cervical flexor and extensor muscles, along with improved strength endurance of the scapular stabiliser muscles. This program holds potential for implementation in physiotherapy clinics, primary care facilities, or hospitals, potentially mitigating the significant socioeconomic burdens associated with non-specific neck pain in women.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki (2013 version). Following a detailed explanation of the research's potential benefits and risks, participants provided their informed consent by signing written consent forms. Additionally, the study received approval from the University of León Research Ethics Committee under the code 040–2022.
Consent to publication
The authors attest that informed consent from all subjects and/or their legal guardians for publication of identifying information/images in an online open-access publication was obtained.
Funding support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
CRediT authorship contribution statement
Pablo Hernandez-Lucas: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Raquel Leirós-Rodríguez: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Juan Lopez-Barreiro: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. José L. García-Soidán: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Methodology, Investigation, Formal analysis, Data curation, Conceptualization.
Declaration of competing interest
None.
Acknowledgements
Not applicable.
Contributor Information
Pablo Hernandez-Lucas, Email: phernandez@uvigo.es.
Raquel Leirós-Rodríguez, Email: rleir@unileon.es.
Juan Lopez-Barreiro, Email: juan.lopez.barreiro@uvigo.es.
José L. García-Soidán, Email: jlsoidan@uvigo.es.
References
- 1.James S.L., Abate D., Abate K.H., Abay S.M., Abbafati C., Abbasi N., et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fejer R., Kyvik K.O., Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur. Spine J. 2006;15(6):834–848. doi: 10.1007/s00586-004-0864-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jahre H., Grotle M., Smedbråten K., Dunn K.M., Øiestad B.E. Risk factors for non-specific neck pain in young adults. A systematic review. BMC Musculoskelet Disord. 2020;21(1):1–12. doi: 10.1186/s12891-020-03379-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kazeminasab S., Nejadghaderi S.A., Amiri P., Pourfathi H., Araj-Khodaei M., Sullman M.J.M., et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 2022;23(1):26. doi: 10.1186/s12891-021-04957-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin B.I., Turner J.A., Mirza S.K., Lee M.J., Comstock B.A., Deyo R.A. Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997–2006. Spine. 2009;34(19):2077–2084. doi: 10.1097/BRS.0b013e3181b1fad1. [DOI] [PubMed] [Google Scholar]
- 6.Başer Ö.Ç., Ay S., Evcik D. Cost-effectiveness analysis of chronic mechanical back pain treatment modalities. Turk J Phys Med Rehabil. 2020;66(4):413. doi: 10.5606/tftrd.2020.4174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Falla D. Unravelling the complexity of muscle impairment in chronic neck pain. Man. Ther. 2004;9(3):125–133. doi: 10.1016/j.math.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 8.Panjabi M.M., Cholewicki J., Nibu K., Grauer J., Babat L.B., Dvorak J. Critical load of the human cervical spine: an in vitro experimental study. Clin. Biomech. 1998;13(1):11–17. doi: 10.1016/s0268-0033(97)00057-0. [DOI] [PubMed] [Google Scholar]
- 9.Lindstrøm R., Schomacher J., Farina D., Rechter L., Falla D. Association between neck muscle coactivation, pain, and strength in women with neck pain. Man. Ther. 2011;16(1):80–86. doi: 10.1016/j.math.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 10.Ylinen J., Salo P., Nykänen M., Kautiainen H., Häkkinen A. Decreased isometric neck strength in women with chronic neck pain and the repeatability of neck strength measurements. Arch. Phys. Med. Rehabil. 2004;85(8):1303–1308. doi: 10.1016/j.apmr.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 11.Chiu T.T., Lam T.H., Hedley A.J. Maximal isometric muscle strength of the cervical spine in healthy volunteers. Clin. Rehabil. 2002;16(7):772–779. doi: 10.1191/0269215502cr552oa. [DOI] [PubMed] [Google Scholar]
- 12.Rezasoltani A., Ali-Reza A., Khosro K.K., Abbass R. Preliminary study of neck muscle size and strength measurements in females with chronic non-specific neck pain and healthy control subjects. Man. Ther. 2010;15(4):400–403. doi: 10.1016/j.math.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 13.Schomacher J., Falla D. Function and structure of the deep cervical extensor muscles in patients with neck pain. Man. Ther. 2013;18(5):360–366. doi: 10.1016/j.math.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 14.Clael S., Campos L.F., Correia K.L., de Lucena J.M.S., Gentil P., Durigan J.L., et al. Exercise interventions can improve muscle strength, endurance, and electrical activity of lumbar extensors in individuals with non-specific low back pain: a systematic review with meta-analysis. Sci. Rep. 2021;11(1) doi: 10.1038/s41598-021-96403-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karaağaç A., Arslan S.A., Keskin E.D. Assessment of pain, scapulothoracic muscle strength, endurance and scapular dyskinesis in individuals with and without nonspecific chronic neck pain: a cross-sectional study. J. Bodyw. Mov. Ther. 2023;35:261–267. doi: 10.1016/j.jbmt.2023.04.008. [DOI] [PubMed] [Google Scholar]
- 16.Blanpied P.R., Gross A.R., Elliott J.M., Devaney L.L., Clewley D., Walton D.M., et al. Clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American physical therapy association. J. Orthop. Sports Phys. Ther. 2017;47(7):A1. doi: 10.2519/jospt.2008.0303. [DOI] [PubMed] [Google Scholar]
- 17.Corp N., Mansell G., Stynes S., Wynne‐Jones G., Morsø L., Hill J.C., et al. Evidence‐based treatment recommendations for neck and low back pain across Europe: a systematic review of guidelines. Eur. J. Pain. 2021;25(2):275–295. doi: 10.1002/ejp.1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iversen V.M., Mork P.J., Vasseljen O., Bergquist R., Fimland M.S. Multiple-joint exercises using elastic resistance bands vs. conventional resistance-training equipment: a cross-over study. Eur. J. Sport Sci. 2017;17(8):973–982. doi: 10.1080/17461391.2017.1337229. [DOI] [PubMed] [Google Scholar]
- 19.Aboodarda S.J., Page P.A., Behm D.G. Muscle activation comparisons between elastic and isoinertial resistance: a meta-analysis. Clin. Biomech. 2016;39:52–61. doi: 10.1016/j.clinbiomech.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 20.Joy J.M., Lowery R.P., Oliveira de Souza E., Wilson J.M. Elastic bands as a component of periodized resistance training. J Strength Cond Res. 2016;30(8):2100–2106. doi: 10.1519/JSC.0b013e3182986bef. [DOI] [PubMed] [Google Scholar]
- 21.Wilson J., Kritz M. Practical guidelines and considerations for the use of elastic bands in strength and conditioning. Strength Cond J. 2014;36(5):1–9. [Google Scholar]
- 22.Hoy D., March L., Woolf A., Blyth F., Brooks P., Smith E., et al. The global burden of neck pain: estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014;73(7):1309–1315. doi: 10.1136/annrheumdis-2013-204431. [DOI] [PubMed] [Google Scholar]
- 23.Cline M.E., Herman J., Shaw E.R., Morton R.D. Standardization of the visual analogue scale. Nurs. Res. 1992;41(6):378–380. [PubMed] [Google Scholar]
- 24.Harris K.D., Heer D.M., Roy T.C., Santos D.M., Whitman J.M., Wainner R.S. Reliability of a measurement of neck flexor muscle endurance. Phys. Ther. 2005;85(12):1349–1355. [PubMed] [Google Scholar]
- 25.Ljungquist T., Harms‐Ringdahl K., Nygren Å., Jensen I. Intra‐and inter‐rater reliability of an 11‐test package for assessing dysfunction due to back or neck pain. Physiother. Res. Int. 1999;4(3):214–232. doi: 10.1002/pri.167. [DOI] [PubMed] [Google Scholar]
- 26.Edmondston S.J., Wallumrød M.E., MacLéid F., Kvamme L.S., Joebges S., Brabham G.C. Reliability of isometric muscle endurance tests in subjects with postural neck pain. J. Manip. Physiol. Ther. 2008;31(5):348–354. doi: 10.1016/j.jmpt.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 27.Colado J.C., Garcia-Masso X., Triplett T.N., Flandez J., Borreani S., Tella V. Concurrent validation of the OMNI-resistance exercise scale of perceived exertion with Thera-band resistance bands. J Strength Cond Res. 2012;26(11):3018–3024. doi: 10.1519/JSC.0b013e318245c0c9. [DOI] [PubMed] [Google Scholar]
- 28.Cohen J. second ed. Hillsdale, N.J: L. Erlbaum Associates; 1988. Statistical Power Analysis for the Behavioral Sciences; p. 567. [Google Scholar]
- 29.Faul F., Erdfelder E., Buchner A., Lang A.G. Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 30.Modarresi S., Lukacs M.J., Ghodrati M., Salim S., MacDermid J.C., Walton D.M. A systematic review and synthesis of psychometric properties of the numeric pain rating scale and the visual analog scale for use in people with neck pain. Clin. J. Pain. 2022;38(2):132–148. doi: 10.1097/AJP.0000000000000999. [DOI] [PubMed] [Google Scholar]
- 31.De Zoete R.M., Armfield N.R., McAuley J.H., Chen K., Sterling M. Comparative effectiveness of physical exercise interventions for chronic non-specific neck pain: a systematic review with network meta-analysis of 40 randomised controlled trials. Br. J. Sports Med. 2021;55(13):730–742. doi: 10.1136/bjsports-2020-102664. [DOI] [PubMed] [Google Scholar]
- 32.Sihawong R., Janwantanakul P., Sitthipornvorakul E., Pensri P. Exercise therapy for office workers with nonspecific neck pain: a systematic review. J. Manip. Physiol. Ther. 2011;34(1):62–71. doi: 10.1016/j.jmpt.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 33.Sarig-Bahat H. Evidence for exercise therapy in mechanical neck disorders. Man. Ther. 2003;8(1):10–20. doi: 10.1054/math.2002.0480. [DOI] [PubMed] [Google Scholar]
- 34.Arami J., Rezasoltani A., Khalkhali Zaavieh M., Rahnama L. The effect of two exercise therapy programs (proprioceptive and endurance training) to treat patients with chronic non-specific neck pain. J Babol Univ Med Sci. 2012;14(1):77–84. [Google Scholar]
- 35.Wilhelm M.P., Donaldson M., Griswold D., Learman K.E., Garcia A.N., Learman S.M., et al. The effects of exercise dosage on neck-related pain and disability: a systematic review with meta-analysis. J. Orthop. Sports Phys. Ther. 2020;50(11):607–621. doi: 10.2519/jospt.2020.9155. [DOI] [PubMed] [Google Scholar]
- 36.Harms-Ringdahl K., Ekholm J., Schüldt K., Németh G., Arborelius U.P. Load moments and myoelectric activity when the cervical spine is held in full flexion and extension. Ergonomics. 1986;29(12):1539–1552. doi: 10.1080/00140138608967267. [DOI] [PubMed] [Google Scholar]
- 37.Yip C.H.T., Chiu T.T.W., Poon A.T.K. The relationship between head posture and severity and disability of patients with neck pain. Man. Ther. 2008;13(2):148–154. doi: 10.1016/j.math.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 38.Edmondston S., Björnsdóttir G., Pálsson T., Solgård H., Ussing K., Allison G. Endurance and fatigue characteristics of the neck flexor and extensor muscles during isometric tests in patients with postural neck pain. Man. Ther. 2011;16(4):332–338. doi: 10.1016/j.math.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 39.Caputo G.M., Di Bari M., Naranjo Orellana J. Group-based exercise at workplace: short-term effects of neck and shoulder resistance training in video display unit workers with work-related chronic neck pain—a pilot randomized trial. Clin. Rheumatol. 2017;36(10):2325–2333. doi: 10.1007/s10067-017-3629-2. [DOI] [PubMed] [Google Scholar]
- 40.Falla D., Lindstrøm R., Rechter L., Boudreau S., Petzke F. Effectiveness of an 8‐week exercise programme on pain and specificity of neck muscle activity in patients with chronic neck pain: a randomized controlled study. Eur. J. Pain. 2013;17(10):1517–1528. doi: 10.1002/j.1532-2149.2013.00321.x. [DOI] [PubMed] [Google Scholar]
- 41.Ylinen J.J., Takala E.P., Nykänen M.J., Kautiainen H.J., Häkkinen A.H., Airaksinen O.V. Effects of twelve-month strength training subsequent to twelve-month stretching exercise in treatment of chronic neck pain. J Strength Cond Res. 2006;20(2):304–308. doi: 10.1519/R-17284.1. [DOI] [PubMed] [Google Scholar]
- 42.Bier J.D., Scholten-Peeters W.G., Staal J.B., Pool J., van Tulder M.W., Beekman E., et al. Clinical practice guideline for physical therapy assessment and treatment in patients with nonspecific neck pain. Phys. Ther. 2018;98(3):162–171. doi: 10.1093/ptj/pzx118. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.