Summary
Healthcare systems in Latin America are broadly heterogeneous, but all of them are burdened by a dramatic rise in liver disease. Some challenges that these countries face include an increase in patients requiring a transplant, insufficient rates of organ donation, delayed referral, and inequitable or suboptimal access to liver transplant programs and post-transplant care. This could be improved by expanding the donor pool through the implementation of education programs for citizens and referring physicians, as well as the inclusion of extended criteria donors, living donors and split liver transplantation. Addressing these shortcomings will require national shifts aimed at improving infrastructure, increasing awareness of organ donation, training medical personnel, and providing equitable access to care for all patients.
Keywords: Cirrhosis, Liver transplant, Latin America, MELD allocation, Extended criteria donor, Live donor, Split liver transplant, Normothermic machine perfusion
Introduction
Cirrhosis is the end stage of all chronic liver diseases and is characterized by the development of regenerative nodules in response to chronic liver injury, replacing functional parenchyma with fibrosis.1 In 2017, the global prevalence of cirrhosis was estimated at 10.6 million cases, and mortality increased from 1.9% of all deaths worldwide in 1990 to 2.4% in 2017, accounting for over two million deaths every year.2 Currently, cirrhosis is estimated to be the eleventh leading cause of death and the fifteenth cause of disability-associated life years.3 Viral hepatitis remains the leading cause of cirrhosis worldwide but is expected to be surpassed by metabolic liver diseases with the advent of direct-acting antivirals (DAAs) and the global obesity pandemic.3,4 Furthermore, the global prevalence of alcohol use disorder (AUD) is estimated at 5.1%, and alcohol-associated liver disease (ALD) is expected to increase as well.3
The burden of cirrhosis is likely underestimated, as patients with compensated cirrhosis are frequently asymptomatic and can remain undiagnosed until decompensation. Furthermore, liver transplantation (LT) is the only curative treatment for decompensated cirrhosis and acute liver failure and serves as a treatment for innate metabolic errors, liver cancer and colorectal tumours with liver metastases. The rise in patients with cirrhosis and other clinical indications for LT is concerning, as waiting lists grow.
Traditionally, LT is performed with a deceased donor graft, obtained after brain or circulatory death. Nonetheless, alternative types of transplantation (mainly extended criteria donors [ECDs], live donor liver transplantation [LDLT], and split liver transplantation [SLT]) were implemented to increase the donor organ pool. ECDs lack a precise definition but are generally considered as those with advanced age, macrovesicular steatosis, organ dysfunction at procurement, death from anoxia, transmissible diseases or a cold ischemia time above 12 h. Among ECDs, donors after cardiac death (DCD) are classified by the Maastricht classification into those who were pronounced dead on arrival (I), those who died after unsuccessful resuscitation before (IIA) or after (IIB) admission, those that were awaiting cardiac death (III) and those that died from cardiac arrest during brain death (IV). Among these, only DCD type III are controlled procurements for which withdrawal of life support can be planned for.5 The use of ECDs has been met with reluctance due to the associated complications, and the widespread use of LDLTs and SLTs has been limited by their complexity. Despite these challenges, global LT rates increased by 6.5% from 2020 to 2021, with 34,694 transplants performed.6 LT is complex even in ideal conditions, and warrants robust healthcare infrastructure. Therefore, countries without this framework face additional important challenges.
Despite the lack of a precise definition for Latin America, it is typically considered as a group of 33 Spanish or Portuguese-speaking countries in Central and South America, as well as Mexico and countries in the Caribbean, and has an estimated population of 654,981,699.7 Broadly speaking, developed Latin American countries are primarily afflicted by metabolic-dysfunction associated steatotic liver disease (MASLD) and ALD, whereas liver disease in developing countries is mainly infectious.8 However, infections as a cause of cirrhosis are expected to be surpassed by MASLD.9 Importantly, cirrhosis is a leading cause of death in Latin America, ranking between fifth and tenth, and the cost of care for a patient with cirrhosis without a LT can be high. Namely, a Mexican cost-analysis performed at the Mexican Social Security Institute estimated that the lifetime cost to treat a patient with cirrhosis can be as high as $65,000 USD.10
In this review, we first aim to identify the challenges in LT that are inherent to Latin American countries, including donor shortage, delayed referral and access to care. Next, we describe the current status of LT in individual countries and potential solutions, such as the use of ECDs, the use of machine perfusion, LDLT and SLT. Finally, we discuss the impact of the COVID-19 pandemic on LT in Latin America.
Search strategy and selection criteria
References for this review were identified by searching through PubMed using the following terms: “liver transplantation”, “Latin America”, and individual country names (for example “Paraguay”). Articles were also identified through individual searches in PubMed depending on their relevance (for example “extended criteria donors”). Public governmental and international databases regarding liver transplantation were also queried. Articles and governmental databases published in English, Spanish and Portuguese were reviewed. The final reference list was generated based on originality and relevance to the broad scope of this review.
Challenges of liver transplantation in Latin American countries
Organ donor shortage
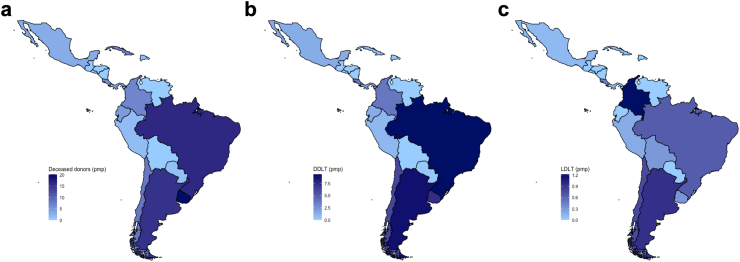
Organ donor shortage represents one of the main barriers to increasing LT rates in Latin America and worldwide. However, Latin America lags behind the rest of the world in donation rates. Fig. 1a shows the average rate of organ donation per million population (pmp) and Fig. 1b shows the average rate of LT from a deceased donor pmp in Latin America during the last five years, according to the International Registry on Organ Donation and Transplantation (IRODaT).11 The highest rates of deceased donor liver donation (DDLD) pmp globally were reported by the United States and the European Union, with rates of 28.4 and 21.9, respectively. In contrast, from 2018 to 2022, the highest rates of DDLD pmp per year in Latin America were reported in Uruguay (20.1), followed by Brazil (16.1), Argentina (15.1), and Chile (8.0). Unfortunately, some countries in Latin America fared worse, with Mexico, Peru and Paraguay reporting averaged yearly DDLD rates of 2.99, 1.36 and 1.2 pmp, respectively.11 This could be secondary to inadequate infrastructure for organ procurement and preservation, but also due to nescience regarding organ donation, or cultural and religious beliefs that discourage it.
Fig. 1.
(a) Averaged deceased donors in the last five years (2018–2022) in Latin America per million population (pmp). (b) Averaged deceased donor LT (DDLT) in the last five years (2018–2022) in Latin America per million population (pmp). (c) Averaged live donor LT (LDLT) in the last five years (2018–2022) in Latin America per million population (pmp).
In a Brazilian survey reported by Bittencourt and colleagues, 67% of surveyed citizens answered that they would willingly become organ donors, and only 52% had communicated their decision to their next of kin. In that study, those unwilling to donate attributed their decision to fear of physical mutilation (12%), no interest in organ donation or no desire to talk about death-related issues with their families (11%), religious beliefs (9%), comorbidities that would exclude organ donation (6%), age (5%), fear of organ retrieval before death (5%), concerns about organ traffic (4%), family disapproval (4%), and other (16%) or unknown reasons (26%).12
Living donor liver donation (LDLD) is also severely underdeveloped in Latin America, lagging behind the rest of the world. For instance, countries such as South Korea, Turkey and Saudi Arabia lead LDLT with rates as high as 22.42, 16.32 and 10.13 pmp, respectively, surpassing their deceased donor rates in 2021. In contrast, the countries with the higher rates of LDLT in Latin America were Colombia (1.35 pmp) and Argentina (1.08 pmp), with the rest of the countries reporting rates below one pmp.11 Of note, LDLT in Chile has increased at an astonishing rate recently, with 20 LDLTs performed in 2022. Fig. 1c shows the average rate of LT from a living donor pmp in Latin America during the last five years according to the IRODaT.
Untimely diagnosis, faulty referral and cultural barriers
A timely diagnosis of cirrhosis is critical to initiate LT protocolization when appropriate. However, referrals to a LT center is often delayed. Many patients with compensated cirrhosis are asymptomatic, and therefore undiagnosed. A Brazilian survey by Bittencourt and colleagues found that ALD is incorrectly assumed to be the main cause of cirrhosis in Brazil, whereas viral hepatitis was neglected, and a considerable proportion of surveyed citizens felt that viral testing was unnecessary.13 After diagnosis, Latin American patients might remain reluctant to seek care due to cultural beliefs that might discourage LT. For instance, patients with ALD might be less likely to seek a transplant under the idea that they are undeserving of one. Likewise, prejudice from referring physicians can result in biased attitudes that result in greater referral of non-alcohol-related causes of cirrhosis.14 Similarly, patients who acquired Hepatitis C virus (HCV) infection from intravenous drug use may fear stigmatization on behalf of health care providers or might believe that they must be abstinent from drug use in order to receive care.15 In a Chilean survey by Vicente and colleagues, 40.7% and of patients diagnosed with AUD or those with intravenous drug use did not seek attention due to distrust in medical personnel. Likewise, 35.7% did not seek care due to fear of stigmatization.16 Interestingly, a cross-cultural study comparing substance abuse stigma young adults in Brazil and the United States found greater tendencies to stigmatize in Brazil, presumably due to different patterns in drug use.17
Compromised access to liver transplantation
Healthcare access in Latin America is diverse, and often limited. Table 1 summarises transplant activity in Latin American countries. A multicenter survey of 65 facilities in 16 countries within the region found that most facilities had adequate infrastructure for guideline-compliant care, but only 16 had LT units. These units were predominantly referral centers in urban regions.29 As such, even countries with high LT rates, such as Brazil and Argentina, might not be able to provide follow-up care for citizens living in rural or marginalized areas after LT.30 Post-LT patients are a complex group that requires close monitorization, and access to adequate healthcare facilities is essential. Immunosuppressants place these patients at risk for opportunistic infections and drug-associated toxicity, particularly early after transplant. Furthermore, frequent follow-up visits are needed to monitor serum levels of immunosuppressive drugs,31 and the centralization of transplant facilities can be a barrier to follow-up in patients living in rural and marginalized areas. Additionally, patients living in these areas have higher rates of poverty, and travel costs can be burdensome. Finally, inadequate follow-up also raises concerns for poor medication adherence. Non-adherence among LT recipients is favoured by inadequate social support, substance abuse before transplant, psychiatric illness, poverty, and lower degrees of literacy,32 such as observed for many in Latin America.
Table 1.
LT activity in Latin American countries.
| Country | Population18 | First LT | Active LT centers |
|---|---|---|---|
| Brazil | 214,326,223 | 196819 | 7820 |
| Mexico | 126,705,138 | 19858 | 238 |
| Argentina | 45,808,747 | 198821 | 2722 |
| Colombia | 51,516,562 | 197623 | 1023 |
| Chile | 19,493,184 | 196924 | 1125 |
| Peru | 33,715,471 | 197426 | 426 |
| Costa Rica | 5,153,957 | 199327 | 326 |
| Ecuador | 17,797,737 | 200026 | 2 |
| Venezuela | 28,199,867 | 1989 | 226 |
| Uruguay | 3,426,260 | 1998 | 128 |
| Panama | 4,351,267 | 201126 | 1 |
| Cuba | 11,256,372 | 198626 | 126 |
| Dominican Republic | 11,117,873 | 200726 | 126 |
| Paraguay | 6,703,799 | 201526 | 126 |
| Bolivia | 12,079,472 | 199626 | 2 |
Financial coverage
The considerable costs associated with LT in Latin America mandate healthcare systems with robust financial coverage, and variations in financial support likely contribute to the heterogeneity of LT across countries. For instance, according to the Argentine Law 27.447, the cost of transplantation is fully covered by the Instituto Nacional Central Único Coordinador de Ablación e Implante (INCUCAI), even subsidizing expenses from LT performed in private hospitals. Similarly, the Brazilian Unified Health System (Sistema Único de Saúde [SUS]) offers universal coverage and has employed private centers to perform LT.33 Contrastingly, other countries fail to provide timely reimbursement. Colombia's universal healthcare system, the Sistema General de Seguridad Social en Salud, gathers contributions from workers, employers and the Colombian government, which are then distributed to Empresas Promotoras de Salud, private health insurance companies responsible for providing insurance coverage. However, the Empresas Promotoras de Salud has faced criticism for denying coverage, overcharging for health services, and providing poor-quality healthcare, resulting in 197,000 tutelas (lawsuits) directed towards the healthcare sector in 2018.34
Graft allocation systems
Due to graft scarcity, it is of paramount importance to maintain equality and justice in liver allocation. In previous attempts to offer LT to the sickest patients, a system based on the Child-Turcotte-Pugh score was initially implemented in the United States in 1987. In 2002, the Model for End-Stage Liver Disease (MELD) score, originally meant to estimate patient survival after a TIPS procedure, was introduced as a more objective alternative.35 Although sicker patients were listed and the time on the waiting list was shortened,36 survival after LT was not improved.37 Furthermore, the original MELD equation faced several caveats, such as laboratory variation in INR determination38 and higher scores in men due to creatinine.19 The MELD-Na score was ensued, including serum sodium to address the higher mortality in those with hyponatremia.20 Until now, the MELD 3.0 score is the last version of the MELD score, which is yet to be implemented in Latin America. It addresses sex disparity and includes albumin as a marker of synthetic function, which could potentially lead to a more equitable allocation process.39 Nevertheless, patients with other liver diseases (namely those that are neoplastic or metabolic, or those with organ dysfunction that are not considered by MELD equations) have scores that might not accurately reflect disease severity, and it is still challenging to determine their priority. Although imperfect, the MELD system is an objective measure for predicting outcomes before transplant. However, allocation should be geographically organized and not center-oriented, as in the case of some Latin American countries.40
Liver transplantation in different countries of Latin America
LT in Latin America varies across countries and only fifteen (45%) remain active.11 In the following section, we discuss the current status of LT in different Latin American countries individually. Liver donation and transplantation rates by country during the last five years are shown in Tables 2 and 3, respectively.
Table 2.
Deceased donors, no. (pmp) per country from 2018 to 202210.
| Country | 2018 | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|
| Uruguay | 77 (23.47) | 75 (22.86) | 63 (19.2) | 43 (12.3) | 75 (22.7) |
| Brazil | 3529 (16.73) | 3768 (18.1) | 3330 (15.8) | 2953 (13.8) | 3528 (16.5) |
| Argentina | 701 (15.75) | 883 (19.5) | 444 (9.82) | 630 (13.9) | 767 (16.67) |
| Chile | 119 (6.54) | 188 (10.4) | 141 (7.38) | 147 (7.7) | N/A |
| Cuba | 130 (11.3) | 138 (12) | 51 (4.51) | 0 (0) | N/A |
| Colombia | 398 (8.04) | 417 (8.4) | 222 (4.4) | 268 (5.25) | N/A |
| Costa Rica | 35 (7) | 33 (6.6) | 27 (5.29) | 17 (3.3) | N/A |
| Ecuador | 133 (7.87) | 133 (7.88) | 29 (1.65) | 47 (2.63) | N/A |
| Mexico | 534 (4.08) | 564 (4.45) | 177 (1.37) | 260 (2) | 398 (3.05) |
| Panama | 27 (6.43) | 18 (4.29) | 3 (0.7) | 0 (0) | N/A |
| Peru | 65 (1.99) | 75 (2.28) | 17 (0.5) | 23 (0.69) | N/A |
| Paraguay | 13 (1.88) | 0 (0) | 0 (0) | 15 (2.1) | N/A |
| Dominican Republic | 9 (0.9) | 23 (2.2) | 4 (0.4) | 9 (0.86) | 11 (1) |
| Guatemala | 5 (0.29) | 6 (0.38) | 0 (0) | 1 (0.1) | N/A |
| Nicaragua | 1 (0.15) | 2 (0.32) | 0 (0) | 0 (0) | 1 (0.14) |
| Bolivia | 4 (0.36) | N/A | 0 (0) | 0 (0) | N/A |
| El Salvador | 0 (0) | 0 (0) | 0 (0) | 0 (0) | N/A |
| Honduras | N/A | N/A | N/A | 0 (0) | N/A |
| Venezuela | 0 (0) | 0 (0) | 0 (0) | N/A | N/A |
Table 3.
Deceased and living donor LT, no. (pmp) per country from 2018 to 202211.
| Country | 2018 | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|
| Brazil | |||||
| LT from DDLT, no. (pmp) | 2040 (9.67) | 2087 (10) | 1933 (9.09) | 1893 (8.9) | 1.951 (9.1) |
| LT from LDLT, no. (pmp) | 175 (0.83) | 158 (0.8) | 141 (0.6) | 50 (0.23) | 167 (0.8) |
| Argentina | |||||
| LT from DDLT, no. (pmp) | 432 (9.71) | 479 (10.7) | 286 (6.31) | 397 (8.7) | 384 (8.34) |
| LT from LDLT, no. (pmp) | 40 (0.9) | 41 (0.9) | 30 (0.68) | 41 (0.9) | 59 (1.29) |
| Uruguay | |||||
| LT from DDLT, no. (pmp) | 27 (8.23) | 23 (7) | 26 (7.92) | 20 (5.7) | 25 (7.6) |
| LT from LDLT, no. (pmp) | 2 (0.61) | 2 (0.6) | 1 (0.3) | 0 (0) | 0 (0) |
| Chile | |||||
| LT from DDLT, no. (pmp) | 87 (4.78) | 145 (8.07) | 104 (5.45) | 110 (5.73) | N/A |
| LT from LDLT, no. (pmp) | 0 (0) | 19 (1.05) | 23 (1.2) | 15 (0.8) | N/A |
| Colombia | |||||
| LT from DDLT, no. (pmp) | 201 (4.06) | 261 (5.3) | 128 (2.54) | 160 (3.2) | N/A |
| LT from LDLT, no. (pmp) | 50 (1.01) | 54 (1.1) | 72 (1.42) | 69 (1.35) | N/A |
| Costa Rica | |||||
| LT from DDLT, no. (pmp) | 25 (5) | 19 (3.8) | 14 (2.75) | 15 (2.94) | N/A |
| LT from LDLT, no. (pmp) | 2 (0.4) | 0 (0) | 1 (0.2) | 5 (1) | N/A |
| Ecuador | |||||
| LT from DDLT, no. (pmp) | 29 (1.72) | 27 (1.58) | 9 (0.51) | 27 (1.51) | N/A |
| LT from LDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | N/A |
| Mexico | |||||
| LT from DDLT, no. (pmp) | 224 (1.71) | 213 (1.68) | 61 (0.47) | 124 (0.5) | 238 (1.82) |
| LT from LDLT, no. (pmp) | 17 (0.13) | 10 (0.07) | 10 (0.08) | 11 (0.1) | 20 (0.15) |
| Panama | |||||
| LT from DDLT, no. (pmp) | 16 (3.81) | 9 (2.14) | 3 (0.7) | 0 (0) | N/A |
| LT from LDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | N/A |
| Peru | |||||
| LT from DDLT, no. (pmp) | 40 (1.23) | 46 (1.4) | 11 (0.3) | 16 (0.48) | N/A |
| LT from LDLT, no. (pmp) | 5 (0.15) | 6 (0.18) | 6 (0.2) | 6 (0.18) | N/A |
| Cuba | |||||
| LT from DDLT, no. (pmp) | 12 (1.04) | 10 (0.87) | 0 (0) | 0 (0) | N/A |
| LT from LDLT, no. (pmp) | 1 (0.09) | 1 (0.09) | 2 (0.18) | 0 (0) | N/A |
| Dominican Republic | |||||
| LT from DDLT, no. (pmp) | 3 (0.3) | 5 (0.5) | 1 (0.1) | 1 (0.1) | 1 (0.09) |
| LT from LDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | 1 (0.09) | 0 (0) |
| Paraguay | |||||
| LT from DDLT, no. (pmp) | 3 (0.42) | 0 (0) | 0 (0) | 0 (0) | N/A |
| LT from LDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | N/A |
| Bolivia | |||||
| LT from DDLT, no. (pmp) | 0 (0) | N/A | 0 (0) | 0 (0) | N/A |
| LT from LDLT, no. (pmp) | 1 (0.79) | N/A | 0 (0) | 1 (0.8) | N/A |
| El Salvador | |||||
| LT from DDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | N/A |
| LT from LDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | N/A |
| Guatemala | |||||
| LT from DDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | N/A |
| LT from LDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | N/A |
| Honduras | |||||
| LT from DDLT, no. (pmp) | N/A | N/A | N/A | 0 (0) | N/A |
| LT from LDLT, no. (pmp) | N/A | N/A | N/A | 0 (0) | N/A |
| Nicaragua | |||||
| LT from DDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| LT from LDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Venezuela | |||||
| LT from DDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | N/A | N/A |
| LT from LDLT, no. (pmp) | 0 (0) | 0 (0) | 0 (0) | N/A | N/A |
Brazil
Brazil leads Latin America in terms of LT, performing approximately two-thirds of all LT in Latin America.41 With 78 active transplant centers,42 Brazil is only surpassed by the United States and China in terms of the absolute number of LTs performed per year. Furthermore, LDLT is widely performed, especially in the pediatric setting.41 However, its large population resulted in rates of 9.1 for DDLT and 0.8 for LDLT pmp in 2022, respectively.11 Organ transplantation is coordinated by the Ministry of Health through the National Transplant System (Sistema Nacional de Trasplantes), and since 2006, the MELD/PELD (Paediatric End-stage Liver Disease) allocation systems have been implemented. This has decreased time and mortality in the waitlist and increased LT in patients with hepatocellular carcinoma and other conditions where MELD exception points are awarded, such as refractory ascites or intractable pruritus.22 In order to address concerns about underestimation of mortality risk in pediatric patients with biliary atresia and failure to thrive, paediatric allocation policies were modified so that the final PELD score was multiplied by three, which resulted in an increase in LT in the paediatric population.43
Despite their success, access to LT is extremely uneven, with transplant centers largely concentrated in the South and Southeast regions. Case volume also varies widely across centers, with some performing over one hundred LT per year and others performing less than five. Since 1998, family consent has been required for organ procurement, after there were concerns regarding organ trafficking with the previous law.44 In March 2023, 1302 patients were waiting for a LT.42 Published on September 12, 2023, GM/MS Ordinance No. 1262 introduces a system of performance-based financial incentives for transplant centers, designed to raise transplant numbers and improve patient outcomes. Performance will be assessed using metrics such as patient survival and complication rates and will be reviewed annually.45
Argentina
According to the IRODAT, 8.34 DDLT and 1.28 LDLT were performed pmp in Argentina in 2022.11 Transplantation in Argentina is coordinated by the INCUCAI, and LT is performed in 27 transplant centers.46 Since 2005, their allocation policy has been determined by the MELD system, becoming the first country after the United States to implement it.47 However, conflicting reports on the effect of the MELD score in Argentinean LT exist. In a study comparing the five years before and after 2005, Cejas and colleagues found that after adopting the MELD system, an increase in the number of patients listed (from 1210 to 2062) resulted in a decrease in LT accessibility (from 57.4% to 50.7%). However, waitlist mortality decreased from 28.5% in 2000–2005 to 21.9% in 2005–2010, with a decrease in dropout rates as well (38.6%–29.1%).48 In contrast, a report from the same database by McCormack and colleagues concluded that the MELD system resulted in an increase in waitlist mortality (from 12.0% to 15.6%), particularly affecting those with a MELD score that was lower than 10.49 Nevertheless, these results might be secondary to underestimation of death rates before the MELD system was in place, as well as a lack of renewal in MELD scores, which was addressed in the study by Cejas.48 Incidentally, both studies found that patients with hepatocellular carcinoma had a greater chance of LT and lower waitlist mortality compared to patients listed with a calculated MELD score of 22.48,49
In 2018, a national law (colloquially known as “the Justina law”) was passed, establishing that all citizens over 18 years old are automatically enrolled as organ donors unless they officially register as non-donors.50 After the implementation of the Justina law, deceased donors increased by 25%, from 701 in 2018 to 883 in 2019.11 Currently, it is estimated that 884 patients need a LT, and 24 patients are in need of a combined transplant that includes a liver.46
Uruguay
The Hospital Central de las Fuerzas Armadas in Montevideo is the only active LT center in Uruguay. Since 2013, organ donation consent has been presumed and donation rates increased over the past decade. Despite high donation rates pmp, the small population limits the absolute number of donations. Consequentially, ECDs have been utilized, particularly for receptors with acute liver failure. According to the Instituto Nacional De Donación Y Trasplante De Células, Tejidos Y Órganos (INDT), 41 patients were waiting for a LT at the end of 2022.51
Chile
Chile has a presumed consent system in place since 2010, where it is presumed that individuals consent to organ donation unless explicitly stated otherwise. Healthcare in Chile is provided by the public and private sectors that provide care for approximately 70% and 30% of the population, respectively. Thus, since seven of the eleven centers that perform LT in Chile are private, public insurance oftentimes pays for private healthcare. Additionally, the national transplant program is centralized, and because of Chile's geographic length, LT recipients who do not live in Santiago (where most transplant centers are located) must travel greater distances for care.23 LT in Chile is overseen by the Coordinación Nacional de Procuramiento y Trasplante de Órganos y Tejidos (CNPT) from the Ministry of Health. Since October 2011, Chile has adopted the MELD/PELD allocation system. Although a higher mortality in patients with higher MELD scores justifies its use, inequities from exception scenarios have been observed in Chile, which warrant further adjustment.27 Also, the MELD/PELD system has resulted in reduced access to LT in paediatric candidates under two years, with considerable waitlist mortality.18 In February 2022, 186 patients were waiting to receive a LT.52 The Hospital Clínico de la Universidad Católica de Chile is the leading center in the country with 66 LT and 19 LDLT in 2022, becoming since 2018, one of the largest LDLT centers in Latin America, with a total of 82 LDLT so far. Of note, LDLT at this center is done almost exclusively by laparoscopy.
Colombia
In Colombia, LT is overseen by the Instituto Nacional de Salud and has ten authorized institutions for LT.53 In 2021, 3.2 DDLT and 1.35 LDLT pmp were performed according to the IRODAT.11 Since 1988, every citizen is presumed to be a donor unless otherwise specified, and in 2016, a law that determined that an individual's decision regarding organ donation could not be revoked by their family was passed.53 By August 2023, 108 patients were waiting for LT in Colombia.54
Costa Rica
Costa Rica's transplantation program is regulated by the Ministry of Health (El Ministerio de Salud). There are three active LT centers in Costa Rica's public system, which is known as the Caja Costarricense de Seguro Social (CCSS), and two private hospitals have authorization to perform LT. Organ donation shifted from an “Opt-Out” system in place since 1994 to an “Opt-In” system in 2014, addressing concerns about organ commercialization and trafficking.55,56 In 2011, an office dedicated to organ donation and transplant was established in CCSS. However, it has not been able to increase donation rates and in 2021, only 15 DDLTs and 5 LDLTs were performed.
Mexico
Coordinated by the Centro Nacional de Trasplantes (CENATRA), Mexico has 84 approved centers for LT, but unfortunately, only 23 remain active, and only seven perform over ten LTs per year. Like Brazil, Mexico's access to LT is unequal, as most centers with over ten LT per year are concentrated in Mexico City. Surprisingly, Mexico has one of the lowest rates of LT in the region, despite being the second-largest economy in Latin America.57 In 2022, only 1.82 DDLT and 0.15 LDLT pmp were performed, with LDLTs being mainly performed in paediatric patients.58 This reflects the low number of deceased donors, which was 3.05 pmp that same year.58 The low rates of LT and donation are attributed to Mexico's fragmented healthcare system, which, similarly to Chile, is divided into public and private sectors. Moreover, within the public sector, different institutions provide care depending on the employment and state affiliation (state workers, formal sector workers, informal sector workers, the Mexican Navy, and the Mexican army). As a result, allocation is center based, with each center having its own waiting list, limiting access to LT for patients with high MELD scores who receive care at less considered centers. The Mexican government has attempted to consolidate the public sector, but frequent reforms to health laws challenge continuity and progress.9 According to the CENATRA, 249 patients were waiting for a LT and seven were waiting for a liver-kidney transplant until November 2023.59
Peru
Peru has three active transplant centers and two of them (the Hospital Nacional Guillermo Almenara Irigoyen and the Hospital Nacional Edgardo Rebagliati Martins) are in Lima. A third transplant center outside Lima, the Hospital Regional Docente Clínico-Quirúrgico “Daniel Alcides Carrión” has only performed two LTs. Peruvian LT is, like other countries, limited by a poor donation rate (0.69 pmp in 2021).60 In 2022, 23 patients were listed for a LT.61 Peruvian LT is largely limited by its fragmented healthcare, consisting of private and public insurance, varying coverage and funding sources. Approximately 65% of the Peruvian population is insured by the Seguro Integral de Salud, mainly covering those living in poverty. However, it only provides healthcare for certain conditions, not including LT. Furthermore, EsSalud provides healthcare, as well as welfare and pension coverage to those working in the formal sector and is financed by employees through their salary. Similarly, those enrolled in the Army or in the Police are insured by the Ministry of Defense. Private insurance accounts for the minority of the population, insuring around 10%. Thus, even though virtually all Peruvians are insured, accessibility to healthcare varies considerably, and those insured by the Seguro Integral de Salud are particularly limited, which raises concern for LT accesibility.62
Other countries
Guatemala has one private center that performs a small number of LDLTs. Seventeen of thirty-three Latin American countries performed no LTs during the last five years. These include Bolivia, Honduras and Nicaragua, and those in the Caribbean. This is most likely a combination of a lack of donors, resources and access to care.
Areas of opportunity
Use of extended criteria donors
Livers from ECD are classically thought to be associated with a higher risk of primary non-function or delayed graft function. Historically, livers from ECDs have not been considered for LT. However, current trends favour the use of ECDs over no transplantation at all, given the higher risk of mortality on the ever-expanding waiting list.
Grafts from advanced-age donors have been associated with ischemia/reperfusion injury and biliary complications.63 Nevertheless, an observational study found that livers from older donors with short ischemia times and routine biopsies could achieve a 5-year graft survival of 81% after LT.64 Additionally, around 25.24% of the Latin American population has MASLD,65 and while increasing grades of steatosis have been associated with reperfusion injury and early graft dysfunction,66 several trials have yielded acceptable results using grafts with moderate to severe steatosis, as long as other risk factors were excluded. Thus, in a region where MASLD is highly prevalent,67 the inclusion of steatotic grafts can have a beneficial effect on the donor pool.
Furthermore, with the advent of effective antiviral therapy, grafts from patients with hepatitis B virus (HBV), HCV, and HIV can now be safely used.68
DCDs are procured after death from hemodynamic or respiratory failure and are therefore subject to a prolonged warm ischemia time, which results in additional graft injury. Recipients who received DCD grafts were historically thought to have worse outcomes compared to those who received a graft from a donor after brain death (DBD)69 and have been discarded. Specifically, recipients who received an allograft from a DCD have a greater risk of ischemic cholangiopathy and primary nonfunction.70, 71 However, selected organs can have acceptable outcomes, which can be improved through the use of novel organ preservation techniques, such as donor liver machine perfusion.72 This might be helpful in countries with a large geographic area where ischemia times can be prolonged.
Technical variant grafts
LDLT stemmed from the lessons learned from SLT. Initially used only for pediatric recipients, who received a left lateral segment from their donors, LDLT was eventually extended to adult recipients, who received a right lobe from their donors. However, LDLT declined in Western countries following the report of a donor death in the United States in 2002.73 LDLT holds some important advantages over DDLT. It can be performed electively, and ischemia times are shorter. This led to lower mortality compared to patients waiting for a DDLT.74 Additionally, LDLT can improve survival at comparable rates to DDLT. However, LDLT is technically complex and might be associated with biliary complications and small-for-size liver syndrome.75 More importantly, donors may have significant morbidity, particularly in right-lobe donors.76
Increasing LDLT and SLT as well as the use of ECDs is promising, and countries should make every effort to train local specialists in these techniques. Facilitating international rotations to high-volume transplant centers in developed countries through scholarships and financial support would eventually lead to foreign-trained experts that could return to their countries.
Addressing cultural barriers
Suboptimal donation rates in some countries are partly due to cultural barriers, which might be effectively addressed through community-wide education. Government-led organ donation campaigns might increase awareness regarding the scarcity of donors, help dispel myths and misconceptions about organ donation and ease concerns about organ trafficking. Transparency and promotion from their corresponding national transplant registry might encourage citizens to register as organ donors or at least to express their wishes in advance regarding organ donation to their families. Organ donation education might also include the concept of extended criteria donors, encouraging those who might believe that they are not candidates to register as well. With the advent of social media, organ donation campaigns through these platforms might be an efficient and practical way of disseminating information. Furthermore, organ donation education could be included in school curricula as a part of citizenship education.
Primary care physicians must be encouraged to refer patients with cirrhosis to transplant centers for prompt evaluation, and all efforts should be employed to decrease physician stigma in the case of cirrhosis due to alcohol, MASLD or viral infections. Furthermore, former paradigms such as a six-month abstinence rule for LT in AUD, or a lack of candidacy for LT in patients living with HIV must be discouraged. Underscoring the scarcity of organ donors during medical education might also be beneficial.
Improving follow-up through telemedicine
With important geographical distances, follow-up after LT can be challenging, especially for those living in marginalized or rural regions. Implementation of telemedicine services could reduce patient expenditures and time lost from work, improve contact between transplant centers and referring physicians, and reduce time intervals between evaluations.77
Health prevention and investment
Addressing the most common causes of cirrhosis and reinforcing public health campaigns could effectively reduce the burden of liver disease and consequently the need for LT. Prenatal screening for HBV and opportune prophylactic treatment of newborns with HBV-positive mothers through the use of hepatitis B immunoglobulin, antiretroviral therapy and neonatal vaccination can lead to a reduction in vertical transmission.78 Likewise, policymakers must facilitate universal screening for HCV and improved access to pan-genotypic DAAs.21 Furthermore, the current obesity epidemic and consequently MASLD can be mitigated through national programs that incentivize exercise and a healthy diet. These include government-subsided feeding programs, market-based food interventions (such as nutritional labelling or taxation of energy-dense products) and the construction of areas for recreation.24 Finally, although the implementation of federal policies to address ALD is paramount, a country-specific approach may be more effective than a generic one, targeting the at-risk population of each country. Effective strategies include regulating advertising, prices and access to alcohol.25
COVID-19 and liver transplant in Latin America
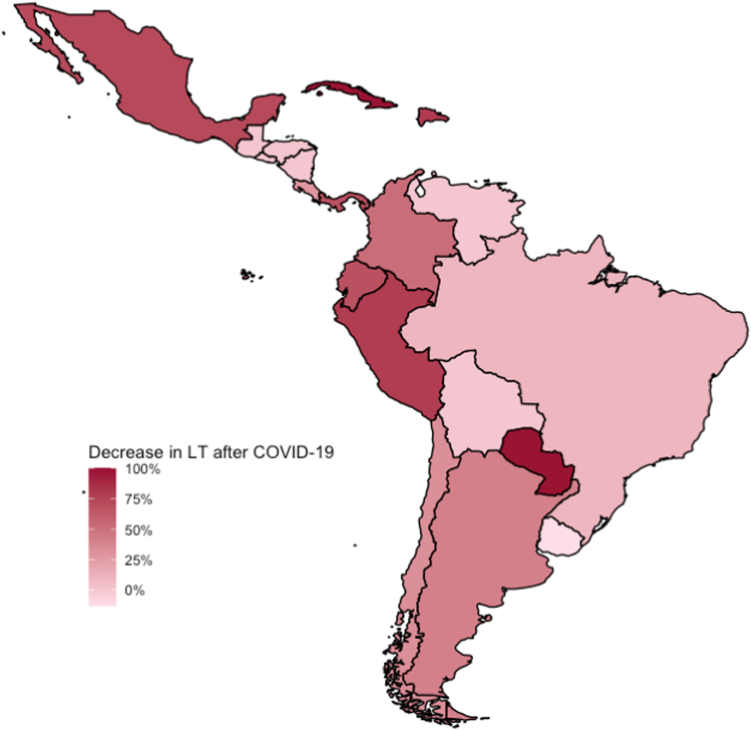
In 2020, the COVID-19 pandemic quickly and unexpectedly ravaged the world, overwhelming healthcare systems. Attempting to halt its spread, resource allocation resulted in hospital reconversions, saturated intensive care units and a shortage of healthcare workers, which resulted in variable decreases in LT worldwide. Fig. 2 depicts the decrease in LT in Latin America during COVID-19 pandemic, calculated using data from the years 2019 to 2020, also illustrated in Table 4.11 Brazil's national organ transplant system was severely affected by the pandemic. In 2020 and 2021, the organ experienced a reduction of 7.7% and 14.3% in LT, respectively. Additionally, the rate of rejection of solid organ transplant recipients increased by 47% in 2021.26 Similarly, Gondolesi and colleagues reported a reduction of 55% in LT in Argentina, with similar reductions in both organ donation and admission to the waiting list.79 Likewise, Mexico faced reductions in LT of 88% and 35% in the public and private sectors, respectively, possibly due to reconversion of transplant centers into COVID-19 care units and a decrease in organ donations.28 However, not all national LT programs were affected equally. A population-based study found an overall decrease in solid organ transplantation in 22 countries, but also found that some countries' LT programs were more affected than others. The authors stratified countries into three patterns; a large decrease in transplant activity despite of relatively few COVID-19-related deaths, a decrease in transplant activity that paralleled COVID-19 deaths and a smaller than expected decrease in transplant activity with a high number of COVID-19 deaths. Interestingly, Chile and Argentina were categorized as countries with a lesser than expected decrease in transplant activity compared to their COVID-19 deaths, whereas other Latin American countries were more affected, potentially as a consequence of already overburdened healthcare systems or less robust LT programs that were furtherly strained by the pandemic.80 As pandemics remain a looming threat, healthcare systems must be prepared to face them whilst maintaining provision of other emergency care procedures, including LT.
Fig. 2.
Decrease in LT during the COVID-19 pandemic (%) from 2019 to 2020.
Table 4.
Deceased donation and LT per country before and after COVID-1911.
| Country | Pre-COVID-19 | COVID-19 era | Decrease (%) |
|---|---|---|---|
| Brazil | |||
| Deceased donors, no. (pmp) | 3768 (18.1) | 3330 (15.8) | 13% |
| LT from DDLT, no. (pmp) | 2087 (10) | 1933 (9.09) | 9% |
| Uruguay | |||
| Deceased donors, no. (pmp) | 75 (22.86) | 63 (19.2) | 16% |
| LT from DDLT, no. (pmp) | 23 (7) | 26 (7.92) | −13% |
| Costa Rica | |||
| Deceased donors, no. (pmp) | 33 (6.6) | 27 (5.29) | 20% |
| LT from DDLT, no. (pmp) | 19 (3.8) | 14 (2.75) | 28% |
| Chile | |||
| Deceased donors, no. (pmp) | 188 (10.4) | 141 (7.38) | 29% |
| LT from DDLT, no. (pmp) | 145 (8.07) | 104 (5.45) | 32% |
| Colombia | |||
| Deceased donors, no. (pmp) | 417 (8.4) | 222 (4.4) | 48% |
| LT from DDLT, no. (pmp) | 261 (5.3) | 128 (2.54) | 52% |
| Argentina | |||
| Deceased donors, no. (pmp) | 883 (19.5) | 444 (9.82) | 50% |
| LT from DDLT, no. (pmp) | 479 (10.7) | 286 (6.31) | 41% |
| Cuba | |||
| Deceased donors, no. (pmp) | 138 (12) | 51 (4.51) | 62% |
| LT from DDLT, no. (pmp) | 10 (0.87) | 0 (0) | 100% |
| Mexico | |||
| Deceased donors, no. (pmp) | 564 (4.45) | 177 (1.37) | 69% |
| LT from DDLT, no. (pmp) | 213 (1.68) | 61 (0.47) | 72% |
| Peru | |||
| Deceased donors, no. (pmp) | 75 (2.28) | 17 (0.5) | 78% |
| LT from DDLT, no. (pmp) | 46 (1.4) | 11 (0.3) | 79% |
| Ecuador | |||
| Deceased donors, no. (pmp) | 133 (7.88) | 29 (1.65) | 79% |
| LT from DDLT, no. (pmp) | 27 (1.58) | 9 (0.51) | 68% |
| Dominican Republic | |||
| Deceased donors, no. (pmp) | 23 (2.2) | 4 (0.4) | 82% |
| LT from DDLT, no. (pmp) | 5 (0.5) | 1 (0.1) | 80% |
| Panama | |||
| Deceased donors, no. (pmp) | 18 (4.29) | 3 (0.7) | 84% |
| LT from DDLT, no. (pmp) | 9 (2.14) | 3 (0.7) | 67% |
Conclusion
Latin American healthcare systems face significant challenges regarding LT, including an increasing number of patients requiring a LT and suboptimal donation rates. Factors that must be improved are access to LT programs, waiting list mortality and post-transplant care, potentially through telemedicine. Furthermore, the donor pool could include extended criteria donors, living donors and split liver grafts. Addressing these shortcomings requires a comprehensive approach that involves improving infrastructure, increasing organ donation awareness, training medical personnel, and providing equitable access to care.
Contributors
DAV–writing, conceptualization and editing MSR–writing, conceptualization and editing ASC–writing, conceptualization and editing MCV–writing, review and editing. RHA–writing, supervision, review and editing. JPA–writing, supervision, review and editing. IR–writing, conceptualization and editing KPAC–writing, review and editing. MAA–writing, review and editing. EAA–writing, review and editing. JDF–writing, review and editing. EFRA–writing, review and editing. VMPZ–writing, review and editing. AGC–writing, supervision, review and editing. MRADS—supervision, review and editing. MM–supervision, review and editing. CPO–supervision, review and editing. MN–supervision, review and editing. IGJ–writing, supervision, review and editing.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
None to be disclosed.
Acknowledgements
Funding: none to be disclosed.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2023.100633.
Appendix A. Supplementary data
References
- 1.Tapper E.B., Parikh N.D. Diagnosis and management of cirrhosis and its complications: a review. JAMA. 2023;329(18):1589–1602. doi: 10.1001/jama.2023.5997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sepanlou S.G., Safiri S., Bisignano C., et al. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(3):245–266. doi: 10.1016/S2468-1253(19)30349-8. https://www.thelancet.com/journals/langas/article/PIIS2468-1253(19)30349-8/fulltext [cited 2023 Mar 14]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Devarbhavi H., Asrani S.K., Arab J.P., Nartey Y.A., Pose E., Kamath P.S. Global burden of liver disease: 2023 update. J Hepatol. 2023;79(2):516–537. doi: 10.1016/j.jhep.2023.03.017. [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez-Chagolla A., Olivas-Martinez A., Ruiz-Manriquez J., et al. Cirrhosis etiology trends in developing countries: transition from infectious to metabolic conditions. Report from a multicentric cohort in central Mexico. Lancet Reg Health Am. 2022;7:100151. doi: 10.1016/j.lana.2021.100151. https://www.thelancet.com/journals/lanam/article/PIIS2667-193X(21)00147-2/fulltext [cited 2022 Sep 18]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le Dinh H., de Roover A., Kaba A., et al. Donation after cardio-circulatory death liver transplantation. World J Gastroenterol. 2012;18(33):4491–4506. doi: 10.3748/wjg.v18.i33.4491. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3435774/ [cited 2023 Jun 24]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Terrault N.A., Francoz C., Berenguer M., Charlton M., Heimbach J. Liver transplantation 2023: status report, current and future challenges. Clin Gastroenterol Hepatol. 2023;21(8):2150–2166. doi: 10.1016/j.cgh.2023.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Latin America & Caribbean | Data. https://data.worldbank.org/region/latin-america-and-caribbean [cited 2023 Mar 14]. Available from:
- 8.Devarbhavi H., Asrani S.K., Arab J.P., Nartey Y.A., Pose E., Kamath P.S. Global burden of liver disease: 2023 update. J Hepatol. 2023;79(2):516–537. doi: 10.1016/j.jhep.2023.03.017. [DOI] [PubMed] [Google Scholar]
- 9.Servin-Rojas M., Olivas-Martinez A., Toapanta-Yanchapaxi L., García-Juárez I. Liver transplantation in Mexico. Clin Liver Dis. 2022;19(2):53–58. doi: 10.1002/cld.1155. https://onlinelibrary.wiley.com/doi/abs/10.1002/cld.1155 [cited 2022 Sep 18]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quiroz M.E., Flores Y.N., Aracena B., et al. Estimating the cost of treating patients with liver cirrhosis at the Mexican Social Security Institute. Salud Publica Mex. 2010;52(6):493–501. [PubMed] [Google Scholar]
- 11.IRODaT - International Registry on Organ Donation and Transplantation. https://www.irodat.org/?p=database&c=UY#data [cited 2023 Mar 18]. Available from:
- 12.Bittencourt P.L., Codes L., Hyppolito E.B., Cesar H.F., Moura-Neto J.A., Gomes Ferraz M.L. Attitudes of the Brazilian population toward organ donation. Kidney Int Rep. 2022;7(12):2737–2740. doi: 10.1016/j.ekir.2022.09.009. https://www.sciencedirect.com/science/article/pii/S2468024922017703 [cited 2023 Mar 24]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bittencourt P.L., Codes L., Cesar H.F., Gomes Ferraz M.L. Public knowledge and attitudes toward liver diseases and liver cancer in the Brazilian population: a cross sectional study. Lancet Reg Health Am. 2023;23 doi: 10.1016/j.lana.2023.100531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aguirre-Villarreal D., García-Juarez I. Addressing transplant inequity for patients with alcohol abuse disorder in Mexico ... The elephant in the room. Lancet Reg Health Am. 2022;15 doi: 10.1016/j.lana.2022.100381. https://www.thelancet.com/journals/lanam/article/PIIS2667-193X(22)00198-3/fulltext#secsectitle0025 [cited 2023 Feb 1]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Austin E.J., Tsui J.I., Barry M.P., et al. Health care-seeking experiences for people who inject drugs with hepatitis C: qualitative explorations of stigma. J Subst Abuse Treat. 2022;137 doi: 10.1016/j.jsat.2021.108684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vicente B., Kohn R., Saldivia S., Rioseco P., Torres S. Patrones de uso de servicios entre adultos con problemas de salud mental, en Chile. Rev Panam Salud Publica. 2005;18(4–5):263–270. doi: 10.1590/s1020-49892005000900006. [DOI] [PubMed] [Google Scholar]
- 17.Henderson N.L., Dressler W.W. Cultural models of substance use risk and attributed stigma: a comparison of young adults in Brazil and the United States. Cross Cult Res. 2020;54(2–3):209–237. [Google Scholar]
- 18.Díaz L.A., López M., Sin P., et al. Current situation of pediatric liver transplantation in Chile. Inequities associated with the MELD/PELD prioritization system. Rev Med Chil. 2020;148(9):1261–1270. doi: 10.4067/S0034-98872020000901261. [DOI] [PubMed] [Google Scholar]
- 19.Cholongitas E., Marelli L., Kerry A., et al. Female liver transplant recipients with the same GFR as male recipients have lower MELD scores--a systematic bias. Am J Transplant. 2007;7(3):685–692. doi: 10.1111/j.1600-6143.2007.01666.x. [DOI] [PubMed] [Google Scholar]
- 20.Kim W.R., Biggins S.W., Kremers W.K., et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359(10):1018–1026. doi: 10.1056/NEJMoa0801209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roblero J.P., Arab J.P., Mezzano G., Mendizabal M. Hepatitis C virus infection: what are we currently doing in Latin America about WHO's proposals for 2030? Clin Liver Dis. 2021;18(2):72–75. doi: 10.1002/cld.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arruda S., Chedid M.F., Jacinto M.M., Álvares-Da-Silva M.R. Meld exception points provide an ENOURMOUS advantage for receiving a liver transplant in Brazil. Arq Gastroenterol. 2020;57(3):254–261. doi: 10.1590/S0004-2803.202000000-48. [DOI] [PubMed] [Google Scholar]
- 23.Benítez C., Wolff R. Current status and future challenges of liver transplantation programs in Chile. Liver Transpl. 2018;24(12):1757–1761. doi: 10.1002/lt.25332. [DOI] [PubMed] [Google Scholar]
- 24.Melo G., Aguilar-Farias N., López Barrera E., et al. Structural responses to the obesity epidemic in Latin America: what are the next steps for food and physical activity policies? Lancet Reg Health Am. 2023;21 doi: 10.1016/j.lana.2023.100486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Díaz L.A., Roblero J.P., Bataller R., Arab J.P. Alcohol-related liver disease in Latin America: local solutions for a global problem. Clin Liver Dis. 2020;16(5):187–190. doi: 10.1002/cld.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Andrade L.G.M., Barbosa A.M.P., da Rocha N.C., et al. Impact of the COVID-19 pandemic on solid organ transplant and rejection episodes in Brazil's unified healthcare system. J Clin Med. 2022;11(21):6581. doi: 10.3390/jcm11216581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolff R., Díaz L.A., Norero B., et al. Análisis del sistema de alistamiento y priorización para trasplante hepático de adultos en Chile. Rev Med Chil. 2020;148(11):1541–1549. doi: 10.4067/S0034-98872020001101541. [DOI] [PubMed] [Google Scholar]
- 28.Servin-Rojas M., Olivas-Martinez A., Ramirez Del Val F., Torres-Gomez A., Navarro-Vargas L., García-Juárez I. Transplant trends in Mexico during the COVID-19 pandemic: disparities within healthcare sectors. Am J Transplant. 2021;21(12):4052–4060. doi: 10.1111/ajt.16801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vorobioff J.D., Contreras F., Tanno F., et al. A Latin American survey on demographic aspects of hospitalized, decompensated cirrhotic patients and the resources for their management. Ann Hepatol. 2020;19(4):396–403. doi: 10.1016/j.aohep.2020.03.007. https://www.sciencedirect.com/science/article/pii/S1665268120300296 [cited 2023 Mar 18]. Available from: [DOI] [PubMed] [Google Scholar]
- 30.Andraus W. Barriers and limitations to access to liver transplantation in Latin America. Clin Liver Dis (Hoboken) 2019;13(2):36–38. doi: 10.1002/cld.763. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6465792/ [cited 2023 Mar 18]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Panackel C., Mathew J.F., Fawas N.M., Jacob M. Immunosuppressive drugs in liver transplant: an insight. J Clin Exp Hepatol. 2022;12(6):1557–1571. doi: 10.1016/j.jceh.2022.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones L.S., Serper M. Medication non-adherence among liver transplant recipients. Curr Hepatol Rep. 2020;19(4):327–336. doi: 10.1007/s11901-020-00545-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8011544/ [cited 2023 Mar 24]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Santos NR dos, Amarante PD. de C. Gestão pública e relação público privado na saúde. 2010. Gestão pública e relação público privado na saúde; p. 324.http://bvssp.icict.fiocruz.br/lildbi/docsonline/get.php?id=2469 [cited 2023 Sep 3]. Available from: [Google Scholar]
- 34.Mendieta González D., Jaramillo C.E. El sistema general de seguridad social en salud de Colombia. Universal, pero ineficiente: a propósito de los veinticinco años de su creación. Rev Latinoam Derech Soc. 2019;29(2):201–218. [Google Scholar]
- 35.Salerno F., Merli M., Cazzaniga M., et al. MELD score is better than child-pugh score in predicting 3-month survival of patients undergoing transjugular intrahepatic portosystemic shunt. J Hepatol. 2002;36(4):494–500. doi: 10.1016/s0168-8278(01)00309-9. [DOI] [PubMed] [Google Scholar]
- 36.Freeman R.B., Wiesner R.H., Edwards E., et al. Results of the first year of the new liver allocation plan. Liver Transpl. 2004;10(1):7–15. doi: 10.1002/lt.20024. [DOI] [PubMed] [Google Scholar]
- 37.Model for end-stage liver disease (MELD) exception guidelines - PubMed. https://pubmed.ncbi.nlm.nih.gov/17123285/ [cited 2023 Jun 3]. Available from:
- 38.Trotter J.F., Olson J., Lefkowitz J., Smith A.D., Arjal R., Kenison J. Changes in international normalized ratio (INR) and model for endstage liver disease (MELD) based on selection of clinical laboratory. Am J Transplant. 2007;7(6):1624–1628. doi: 10.1111/j.1600-6143.2007.01822.x. [DOI] [PubMed] [Google Scholar]
- 39.Kim W.R., Mannalithara A., Heimbach J.K., et al. MELD 3.0: the Model for end-stage liver disease updated for the modern era. Gastroenterology. 2021;161(6):1887–1895.e4. doi: 10.1053/j.gastro.2021.08.050. https://www.gastrojournal.org/article/S0016-5085(21)03469-7/fulltext [cited 2023 Jun 3]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Contreras A.G., McCormack L., Andraus W., de Souza M Fernandes E. Latin America Liver Transplantation Group. Current status of liver transplantation in Latin America. Int J Surg. 2020;82S:14–21. doi: 10.1016/j.ijsu.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 41.Bittencourt P.L., Farias A.Q., Couto C.A. Liver transplantation in Brazil. Liver Transpl. 2016;22(9):1254–1258. doi: 10.1002/lt.24487. [DOI] [PubMed] [Google Scholar]
- 42.ABTO. https://site.abto.org.br/publicacao/xxviii-no4/ XXVIII - No4. [cited 2023 Jun 3]. Available from:
- 43.Neto J.S., Carone E., Pugliese R.P.S., et al. Modified pediatric end-stage liver disease scoring system and pediatric liver transplantation in Brazil. Liver Transpl. 2010;16(4):426–430. doi: 10.1002/lt.22000. [DOI] [PubMed] [Google Scholar]
- 44.Csillag C. Brazil abolishes “presumed consent” in organ donation. Lancet. 1998;352(9137):1367. doi: 10.1016/S0140-6736(05)60767-2. [DOI] [PubMed] [Google Scholar]
- 45.Nacional I. Portaria GM/MS no 1.262, de 12 de setembro de 2023 - DOU - imprensa nacional. https://www.in.gov.br/web/dou [cited 2023 Sep 13]. Available from:
- 46.INCUCAI - Sistema Nacional de Información. https://cresi.incucai.gov.ar/reporte/resumenestadistico/EjecutarConsultaTrasplante.do?reporte=hepatico [cited 2023 Jun 3]. Available from:
- 47.Haddad L., Marciano S., Cleres M., et al. Characteristics of liver transplantation in Argentina: a multicenter study. Transplant Proc. 2018;50(2):478–484. doi: 10.1016/j.transproceed.2017.11.072. [DOI] [PubMed] [Google Scholar]
- 48.Cejas N.G., Villamil F.G., Lendoire J.C., et al. Improved waiting-list outcomes in Argentina after the adoption of a model for end-stage liver disease–based liver allocation policy. Liver Transpl. 2013;19(7):711–720. doi: 10.1002/lt.23665. [DOI] [PubMed] [Google Scholar]
- 49.McCormack L., Gadano A., Lendoire J., et al. Model for end-stage liver disease-based allocation system for liver transplantation in Argentina: does it work outside the United States? HPB (Oxford) 2010;12(7):456–464. doi: 10.1111/j.1477-2574.2010.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Love E. 2020. MultiplicateX7: a comparison of the organ donation and transplantation systems and attitudes in Argentina and the United States.https://dataspace.princeton.edu/handle/88435/dsp01b8515r42f [cited 2023 May 20]; Available from: [Google Scholar]
- 51.Organos IN de D y T de C Tejidos y INDT :: Portal Oficial. INDT ::Portal Oficial. https://indt.gub.uy [cited 2023 Jun 6]. Available from:
- 52.Instituto de Salud Pública de Chile. https://www.ispch.cl/ [cited 2023 Jun 6]. Available from:
- 53.Salinas Nova M.A., Rojas Meneses Á., Restrepo Gutierrez J.C. Liver transplant in Colombia. Liver Transpl. 2019;25(4):658–663. doi: 10.1002/lt.25427. [DOI] [PubMed] [Google Scholar]
- 54.Donación de órganos | SALUDATA. 2023. https://saludata.saludcapital.gov.co/osb/index.php/datos-de-salud/enfermedades-cronicas/donacion-de-organos/ [cited 2023 Nov 1]. Available from:
- 55.Catarinella-Gómez C., López-Jara V., Araya-Chavarría S., et al. Serie de casos de trasplante hepático ortotópico del Hospital “Dr. Rafael Ángel Calderón Guardia.”. Acta Médica Costarricense. 2021;63(1):21–28. http://www.scielo.sa.cr/scielo.php?script=sci_abstract&pid=S0001-60022021000100021&lng=en&nrm=iso&tlng=es [cited 2023 May 29]. Available from: [Google Scholar]
- 56.INS Colombia. https://www.ins.gov.co/Paginas/Inicio.aspx [cited 2023 Nov 1]. Available from:
- 57.World Bank Open Data World bank open data. https://data.worldbank.org [cited 2023 May 20]. Available from:
- 58.IRODaT - International registry on organ donation and transplantation. https://www.irodat.org/ [cited 2023 Aug 30]. Available from:
- 59.Centro Nacional de Trasplantes | Gobierno | gob.mx. https://www.gob.mx/cenatra [cited 2023 Jun 6]. Available from:
- 60.10 años de trasplante hepático en el Perú | Revista de Gastroenterología del Perú. https://revistagastroperu.com/index.php/rgp/article/view/423 [cited 2023 May 22]. Available from: [PubMed]
- 61.Ministerio de Salud - MINSA. 2023. https://www.gob.pe/minsa [cited 2023 Jun 6]. Available from:
- 62.Carrillo-Larco R.M., Guzman-Vilca W.C., Leon-Velarde F., et al. Peru – progress in health and sciences in 200 years of independence. Lancet Reg Health Am. 2022;7:100148. doi: 10.1016/j.lana.2021.100148. https://www.thelancet.com/journals/lanam/article/PIIS2667-193X(21)00144-7/fulltext [cited 2023 Sep 3]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Serrano M.T., Garcia-Gil A., Arenas J., et al. Outcome of liver transplantation using donors older than 60 years of age. Clin Transplant. 2010;24(4):543–549. doi: 10.1111/j.1399-0012.2009.01135.x. [DOI] [PubMed] [Google Scholar]
- 64.Cescon M., Grazi G.L., Cucchetti A., et al. Improving the outcome of liver transplantation with very old donors with updated selection and management criteria. Liver Transpl. 2008;14(5):672–679. doi: 10.1002/lt.21433. [DOI] [PubMed] [Google Scholar]
- 65.Castellanos-Fernandez M.I., Pal S.C., Arrese M., Arab J.P., George J., Méndez-Sánchez N. Nonalcoholic fatty liver disease in Latin America and Australia. Clin Liver Dis. 2023;27(2):301–315. doi: 10.1016/j.cld.2023.01.015. [DOI] [PubMed] [Google Scholar]
- 66.de Graaf E.L., Kench J., Dilworth P., et al. Grade of deceased donor liver macrovesicular steatosis impacts graft and recipient outcomes more than the Donor Risk Index. J Gastroenterol Hepatol. 2012;27(3):540–546. doi: 10.1111/j.1440-1746.2011.06844.x. [DOI] [PubMed] [Google Scholar]
- 67.Rojas Y.A.O., Cuellar C.L.V., Barrón K.M.A., Arab J.P., Miranda A.L. Non-alcoholic fatty liver disease prevalence in Latin America: a systematic review and meta-analysis. Ann Hepatol. 2022;27(6):100706. doi: 10.1016/j.aohep.2022.100706. https://www.sciencedirect.com/science/article/pii/S1665268122000485 [cited 2023 May 20]. Available from: [DOI] [PubMed] [Google Scholar]
- 68.Durand C.M., Florman S., Motter J.D., et al. HOPE in action: a prospective multicenter pilot study of liver transplantation from donors with HIV to recipients with HIV. Am J Transplant. 2022;22(3):853–864. doi: 10.1111/ajt.16886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Blok J.J., Detry O., Putter H., et al. Longterm results of liver transplantation from donation after circulatory death. Liver Transpl. 2016;22(8):1107–1114. doi: 10.1002/lt.24449. [DOI] [PubMed] [Google Scholar]
- 70.Taner C.B., Bulatao I.G., Perry D.K., et al. Asystole to cross-clamp period predicts development of biliary complications in liver transplantation using donation after cardiac death donors. Transpl Int. 2012;25(8):838–846. doi: 10.1111/j.1432-2277.2012.01508.x. [DOI] [PubMed] [Google Scholar]
- 71.DeOliveira M.L., Jassem W., Valente R., et al. Biliary complications after liver transplantation using grafts from donors after cardiac death: results from a matched control study in a single large volume center. Ann Surg. 2011;254(5):716–722. doi: 10.1097/SLA.0b013e318235c572. discussion 722-723. [DOI] [PubMed] [Google Scholar]
- 72.Dengu F., Abbas S.H., Ebeling G., Nasralla D. Normothermic machine perfusion (NMP) of the liver as a platform for therapeutic interventions during ex-vivo liver preservation: a review. J Clin Med. 2020;9(4):1046. doi: 10.3390/jcm9041046. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7231144/ [cited 2023 May 18]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Brown R.S. Live donors in liver transplantation. Gastroenterology. 2008;134(6):1802–1813. doi: 10.1053/j.gastro.2008.02.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Berg C.L., Gillespie B.W., Merion R.M., et al. Improvement in survival associated with adult-to-adult living donor liver transplantation. Gastroenterology. 2007;133(6):1806–1813. doi: 10.1053/j.gastro.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pomposelli J.J., Goodrich N.P., Emond J.C., et al. Patterns of early allograft dysfunction in adult live donor liver transplantation: the A2ALL experience. Transplantation. 2016;100(7):1490–1499. doi: 10.1097/TP.0000000000001240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ito T., Kiuchi T., Egawa H., et al. Surgery-related morbidity in living donors of right-lobe liver graft: lessons from the first 200 cases. Transplantation. 2003;76(1):158–163. doi: 10.1097/01.TP.0000072372.42396.47. [DOI] [PubMed] [Google Scholar]
- 77.Shroff H., Kulik L. Telemedicine for liver transplant evaluations: the benefits and risks. Clin Liver Dis (Hoboken) 2022;19(4):157–160. doi: 10.1002/cld.1175. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9053678/ [cited 2023 Jun 24]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Veronese P., Dodi I., Esposito S., Indolfi G. Prevention of vertical transmission of hepatitis B virus infection. World J Gastroenterol. 2021;27(26):4182–4193. doi: 10.3748/wjg.v27.i26.4182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gondolesi G.E., Reyes-Toso M.L., Bisigniano L., et al. [Impact of COVID-19 pandemic in liver transplantation in Argentina. Other collateral damage] Medicina (B Aires) 2020;80(Suppl 6):71–82. [PubMed] [Google Scholar]
- 80.Aubert O., Yoo D., Zielinski D., et al. COVID-19 pandemic and worldwide organ transplantation: a population-based study. Lancet Public Health. 2021;6(10):e709–e719. doi: 10.1016/S2468-2667(21)00200-0. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8460176/ [cited 2023 May 13]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.