Abstract
What is already known about this topic?
The advent of antiretroviral therapy (ART) has markedly decreased mortality rates among patients infected with human immunodeficiency virus (HIV). Globally, there has been a 43% reduction in acquired immunodeficiency syndrome (AIDS)-related deaths from 2010 to 2022. Additionally, prior research indicates that the initiation of ART at an early stage within China has substantially lowered mortality rates.
What is added by this report?
Over the previous decade, following the implementation of China’s universal ART access strategy, the patterns of mortality causes among HIV-infected individuals across the country have undergone significant alterations. In 2022, the all-cause mortality rate among this population was reported at 2.7%, with the non-AIDS-related mortality rate at 1.8%. However, it is important to consider that the accuracy of death reporting could contribute to potential misclassification of the underlying causes of death.
What are the implications for public health practice?
Efforts to enhance health outcomes should persist in emphasizing the advancement of ART strategies, with a particular focus on mitigating non-AIDS-related mortality in the future.
Keywords: Mortality, HIV, Death causes
The advent of antiretroviral therapy (ART) has markedly increased life expectancy and decreased mortality rates in individuals living with human immunodeficiency virus (HIV). Before, or at the onset of, the ART era, the predominant causes of death were acquired immune deficiency syndrome (AIDS)-related illnesses, including defining opportunistic infections and malignant tumors. However, with the progression of the ART era, there has been a significant shift towards non-AIDS-related mortality. Data from the United Nations Programme on AIDS (UNAIDS) indicates a global reduction of 43% in AIDS-related deaths, falling from 1,100,000 in 2010 to 630,000 in 2022 (1). Within China, AIDS has emerged as a principal cause of death from infectious diseases in recent times. Earlier research emphasizes that initiating ART at early stages significantly diminishes the mortality rates (2). By 2020, ART coverage among those infected with HIV peaked at 92.9%. Over the past decade, China’s implementation of a universal ART access strategy has occurred without a comprehensive analysis of mortality rates and changing patterns of cause of death among the national HIV-infected population. Utilizing data from the nationwide HIV/AIDS Comprehensive Response Information Management System (CRIMS), this retrospective analysis investigates mortality rates across the HIV-infected cohort from 2013 to 2022. The insights gained from this study are instrumental in pinpointing challenges and enhancing health outcomes moving forward.
Data for this study were obtained from the CRIMS database, administered by the National Center for AIDS/STD Control and Prevention (NCAIDS). The system mandates the reporting of all confirmed HIV-positive individuals, encompassing initial diagnosis and follow-up data. In the event of a patient’s death, local healthcare workers must submit a specialized death registration form. Further, data specific to patients commencing ART should be entered into the ART database subsystem. This study implemented a multiple cross-sectional design to investigate changes in mortality rates and causes of death from 2013 to 2022. Data extraction for the manuscript occurred on June 30, 2023, allowing a six-month period to account for any reporting delays in death records. Due to modifications in the death registration system in 2012, consistent reporting of death causes only commenced in 2013. We calculated annual mortality rates using the total number of survivors and new diagnoses for the year as the denominator, and the total deaths in the same year as the numerator. The Cochran-Armitage trend test was employed to assess changes in the mortality rate, while the normal approximation method provided the 95% confidence intervals (CI) for these rates. ART coverage rate was defined as the percentage of patients on treatment at year-end relative to all living HIV-positive patients, ascertained from historical data. We analyzed the correlation between ART coverage rate and mortality rate using Pearson’s correlation coefficient.
During the study period, the eligibility criteria for initiating ART were modified: the threshold for CD4+T cell counts was raised from 350 cells/mm3 to 500 cells/mm3 in 2014 and then removed entirely in 2016, allowing initiation of ART regardless of CD4+T cell counts. These adjustments have potential implications for trends in ART coverage and mortality rates. Deaths related to AIDS and those not associated with AIDS were categorized based on the presence of specific diseases or events at the time of death, in accordance with the reporting guidelines of the system. AIDS-related diseases encompass pneumocystis pneumonia, cryptococcosis, tuberculosis, recurrent bacterial pneumonia, candidiasis, cytomegalovirus disease, AIDS-defining cancers (ADCs), toxoplasmosis, and HIV wasting syndrome, among others. Non-AIDS related events include cardiovascular and cerebrovascular diseases (CCVDs), non-AIDS defining cancers (NADCs), viral hepatitis, and various respiratory diseases, as well as fatalities due to accidents, which comprise suicide, drug overdose, and other non-disease related causes of death. China’s geographical landscape is segmented into seven regions for the purposes of this research: northeastern China [comprising Heilongjiang, Jilin, and Liaoning provincial-level administrative divisions (PLADs)], northern China (including Beijing, Tianjin, Hebei, Shanxi, and Inner Mongolia PLADs), central China (Hubei, Hunan, and Henan PLADs), southern China (Guangdong, Guangxi, and Hainan PLADs), eastern China (encompassing Shanghai, Shandong, Jiangsu, Anhui, Jiangxi, Zhejiang, and Fujian PLADs), northwestern (Shaanxi, Gansu, Ningxia, Xinjiang, and Qinghai PLADs), and southwestern (Chongqing, Sichuan, Guizhou, Yunnan, and Xizang PLADs). Data analysis for this study was conducted using SAS software (version 9.4, NC, SAS Institute Inc., USA).
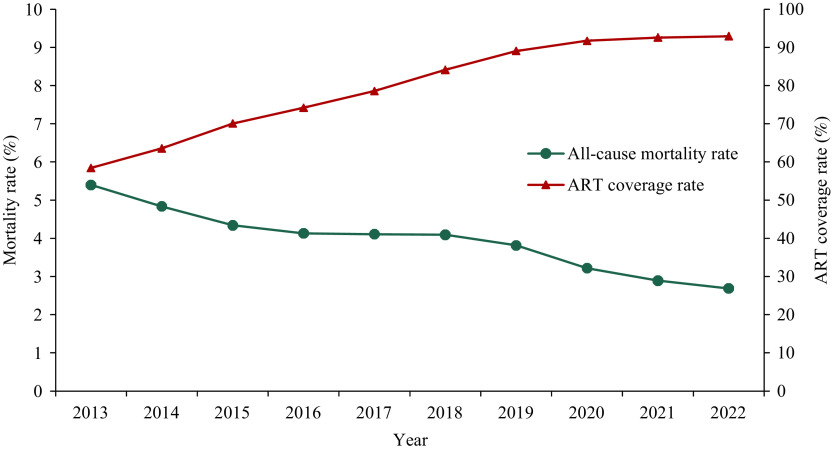
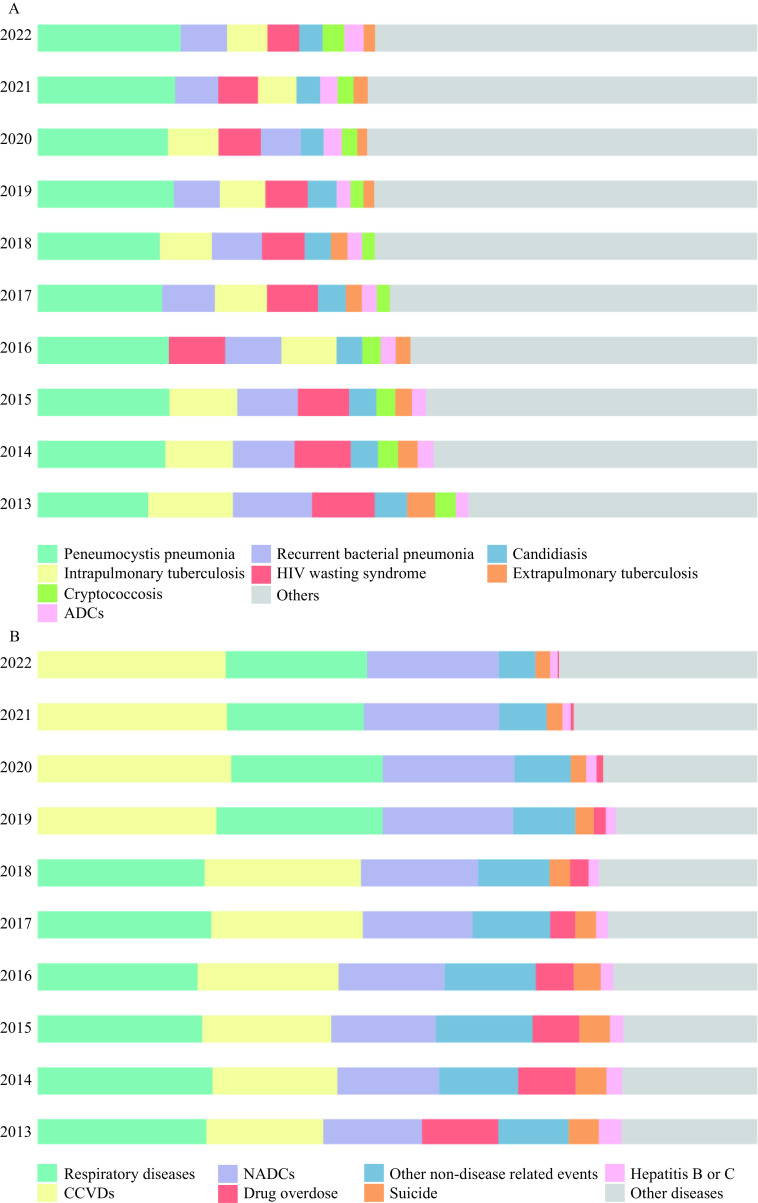
From 2013 to 2022, there was a marked decline in the all-cause mortality rate among Chinese HIV-infected patients, decreasing from 5.4% to 2.7% (P<0.05 for trend) (Figure 1). Simultaneously, ART coverage in China saw a substantial rise, from 58.4% to 92.8% (P<0.05 for trend), exhibiting a strong inverse relationship with the mortality rate (r=−0.964, P<0.05). Subgroup analyses based on ART status were carried out across various categories, including age, gender, transmission route, geographical regions, and CD4+T cell counts in 2022 (Table 1). In the same year, the subgroups with the highest all-cause mortality rates included individuals with CD4+T cell counts below 200 cells/mm3 (7.5%), those aged 50 years or older (4.8%), people contracting HIV via heterosexual transmission (3.4%), residents of Southwest China (3.3%), and males (2.9%). Cause-specific mortality rates among ART recipients were lower compared to the overall patient population (all-cause mortality: 1.6% vs. 2.7%; AIDS-related mortality: 0.3% vs. 0.4%; non-AIDS related mortality: 1.1% vs. 1.8%; deaths from unknown causes: 0.3% vs. 0.4%). Between 2013 and 2022, pneumocystis pneumonia remained the most frequent cause of AIDS-related deaths, accounting for 15.4% to 19.9% of cases. Tuberculosis and recurrent bacterial pneumonia, both trending downward, were the second and third most common causes, respectively. Among non-AIDS causes of death, respiratory diseases, CCVDs, and NADCs were predominant from 2013 to 2018, but by 2019 CCVDs had emerged as the leading cause (Figure 2). Notably, the proportion of deaths attributable to CCVDs increased from 16.3% in 2013 to 26.1% in 2022.
Figure 1.
The trend of mortality rate and ART coverage among HIV-infected patients in China, 2013–2022.
Abbreviation: ART=antiretroviral therapy; HIV=human immunodeficiency virus.
Table 1. Cause-specific mortality rates among HIV-infected patients in China, 2022.
| Characteristic |
MR of total HIV infected patients (100.0%)
% (95% CI) |
MR of patients on ART (92.8%)
% (95% CI) |
|||||||||
| Proportion | All cause | AIDS related |
Non-AIDS
related |
Unknown cause | Proportion | All cause | AIDS related | Non-AIDS related | Unknown cause | ||
| Abbreviation: ART=antiretroviral therapy; AIDS=acquired immunodeficiency syndrome; HIV=human immunodeficiency virus; MTCT=mother-to-child transmission of HIV; MR=mortality rate; CI=confidence interval. | |||||||||||
| Total | 100 | 2.7 (2.66, 2.71) | 0.4 (0.44, 0.46) | 1.8 (1.78, 1.82) | 0.4 (0.39, 0.41) | 100 | 1.6 (1.62, 1.67) | 0.3 (0.28, 0.30) | 1.1 (1.08, 1.12) | 0.3 (0.29, 0.31) | |
| Current age, years | |||||||||||
| <15 | 0.6 | 1.0 (0.76, 1.22) | 0.3 (0.17, 0.41) | 0.5 (0.36, 0.69) | 0.2 (0.10, 0.30) | 0.6 | 0.6 (0.42, 0.78) | 0.2 (0.08, 0.27) | 0.3 (0.18, 0.44) | 0.1 (0.03, 0.17) | |
| 15–24 | 4.9 | 0.5 (0.46, 0.57) | 0.1 (0.09, 0.15) | 0.3 (0.25, 0.33) | 0.1 (0.08, 0.12) | 4.8 | 0.3 (0.22, 0.31) | 0.1 (0.06, 0.11) | 0.1 (0.10, 0.16) | 0.0 (0.00, 0.00) | |
| 25–49 | 54.7 | 1.3 (1.30, 1.35) | 0.3 (0.29, 0.31) | 0.8 (0.79, 0.84) | 0.2 (0.19, 0.21) | 54.7 | 0.7 (0.72, 0.76) | 0.2 (0.18, 0.20) | 0.4 (0.43, 0.46) | 0.1 (0.09, 0.11) | |
| ≥50 | 39.8 | 4.8 (4.79, 4.90) | 0.7 (0.67, 0.72) | 3.4 (3.31, 3.41) | 0.8 (0.78, 0.82) | 39.9 | 3.1 (3.01, 3.11) | 0.5 (0.44, 0.48) | 2.1 (2.09, 2.17) | 0.5 (0.48, 0.52) | |
| Gender | |||||||||||
| Male | 74.7 | 2.9 (2.88, 2.95) | 0.5 (0.47, 0.50) | 2.0 (1.93, 1.99) | 0.5 (0.49, 0.51) | 74.3 | 1.8 (1.77, 1.83) | 0.3 (0.30, 0.33) | 1.2 (1.19, 1.23) | 0.3 (0.29, 0.31) | |
| Female | 25.3 | 2.0 (1.97, 2.07) | 0.3 (0.32, 0.36) | 1.3 (1.29, 1.37) | 0.4 (0.38, 0.42) | 25.7 | 1.2 (1.16, 1.24) | 0.2 (0.20, 0.24) | 0.8 (0.76, 0.82) | 0.2 (0.18, 0.22) | |
| Transmission route | |||||||||||
| Heterosexual contact | 65.4 | 3.4 (3.38, 3.46) | 0.5 (0.53, 0.56) | 2.3 (2.28, 2.35) | 0.6 (0.58, 0.62) | 65.3 | 2.1 (2.06, 2.13) | 0.4 (0.34, 0.37) | 1.4 (1.39, 1.44) | 0.3 (0.29, 0.31) | |
| Male-to-male sexual contact | 26.0 | 0.8 (0.75, 0.81) | 0.2 (0.18, 0.21) | 0.5 (0.45, 0.49) | 0.1 (0.09, 0.11) | 26.4 | 0.4 (0.41, 0.46) | 0.1 (0.11, 0.13) | 0.3 (0.24, 0.28) | 0.1 (0.09, 0.11) | |
| Injection drug use | 4.9 | 3.2 (3.05, 3.33) | 0.5 (0.41, 0.52) | 2.2 (2.09, 2.33) | 0.5 (0.44, 0.56) | 4.6 | 2.2 (2.07, 2.32) | 0.3 (0.28, 0.38) | 1.5 (1.41, 1.62) | 0.4 (0.35, 0.45) | |
| Blood receptor or donor | 2.0 | 2.1 (1.97, 2.33) | 0.5 (0.40, 0.58) | 1.4 (1.29, 1.58) | 0.2 (0.14, 0.26) | 2.1 | 2.1 (1.88, 2.23) | 0.5 (0.40, 0.58) | 1.4 (1.21, 1.50) | 0.2 (0.14, 0.26) | |
| MTCT | 0.8 | 0.8 (0.72, 0.91) | 0.2 (0.19, 0.29) | 0.4 (0.34, 0.47) | 0.2 (0.15, 0.25) | 0.8 | 0.6 (0.41, 0.72) | 0.2 (0.09, 0.26) | 0.3 (0.18, 0.40) | 0.1 (0.03, 0.17) | |
| Unknown | 1.0 | 4.1 (3.73, 4.44) | 0.7 (0.53, 0.82) | 2.4 (2.17, 2.72) | 1.0 (0.82, 1.18) | 0.9 | 1.7 (1.41, 1.90) | 0.3 (0.23, 0.46) | 1.0 (0.79, 1.17) | 0.3 (0.19, 0.41) | |
| Geographical units | |||||||||||
| Southern | 16.3 | 3.2 (3.09, 3.24) | 0.6 (0.59, 0.65) | 2.0 (1.91, 2.03) | 0.6 (0.57, 0.63) | 15.7 | 1.6 (1.57, 1.69) | 0.4 (0.33, 0.38) | 1.0 (0.96, 1.05) | 0.3 (0.27, 0.33) | |
| Northern | 5.9 | 1.1 (1.01, 1.16) | 0.3 (0.26, 0.34) | 0.6 (0.55, 0.66) | 0.2 (0.17, 0.23) | 5.9 | 0.6 (0.55, 0.67) | 0.2 (0.12, 0.18) | 0.4 (0.32, 0.42) | 0.1 (0.08, 0.12) | |
| Eastern | 15.3 | 1.8 (1.73, 1.85) | 0.4 (0.35, 0.40) | 1.2 (1.15, 1.25) | 0.2 (0.18, 0.22) | 15.6 | 1.1 (1.01, 1.10) | 0.2 (0.22, 0.27) | 0.7 (0.65, 0.73) | 0.1 (0.09, 0.11) | |
| Central | 12.6 | 2.7 (2.65, 2.81) | 0.6 (0.52, 0.59) | 1.8 (1.77, 1.90) | 0.3 (0.27, 0.33) | 12.7 | 1.8 (1.71, 1.85) | 0.4 (0.37, 0.43) | 1.2 (1.10, 1.21) | 0.2 (0.18, 0.22) | |
| Southwestern | 38.5 | 3.3 (3.25, 3.35) | 0.4 (0.39, 0.43) | 2.3 (2.24, 2.33) | 0.6 (0.58, 0.62) | 39.1 | 2.1 (2.11, 2.19) | 0.3 (0.27, 0.30) | 1.5 (1.46, 1.53) | 0.4 (0.38, 0.42) | |
| Northwestern | 7.4 | 2.2 (2.08, 2.26) | 0.5 (0.43, 0.52) | 1.5 (1.37, 1.53) | 0.2 (0.17, 0.23) | 7.1 | 1.3 (1.22, 1.38) | 0.3 (0.27, 0.35) | 0.9 (0.81, 0.94) | 0.1 (0.08, 0.12) | |
| Northeastern | 4.1 | 1.5 (1.35, 1.56) | 0.3 (0.21, 0.30) | 1 (0.95, 1.13) | 0.2 (0.16, 0.24) | 4.0 | 0.8 (0.69, 0.84) | 0.1 (0.11, 0.18) | 0.5 (0.47, 0.60) | 0.1 (0.07, 0.13) | |
| Current CD4+T cell counts, cells/mm3 | |||||||||||
| ≥200 | 81.5 | 0.7 (0.70, 0.73) | 0.1 (0.07, 0.08) | 0.5 (0.52, 0.55) | 0.1 (0.10, 0.11) | 85.8 | 0.6 (0.57, 0.60) | 0.1 (0.06, 0.07) | 0.5 (0.43, 0.45) | 0.1 (0.07, 0.08) | |
| <200 | 10.7 | 4.7 (4.63, 4.85) | 1.3 (1.25, 1.37) | 2.7 (2.62, 2.79) | 0.7 (0.69, 0.78) | 10.9 | 3.6 (3.51, 3.71) | 1.0 (0.91, 1.02) | 2.1 (2.00, 2.16) | 0.6 (0.52, 0.61) | |
| Missing | 7.8 | 20.5 (20.25, 20.76) | 3.1 (3.03, 3.25) | 13.9 (13.63, 14.06) | 3.5 (3.41, 3.64) | 3.3 | 23.1 (22.65, 23.50) | 4.0 (3.81, 4.21) | 15.3 (14.95, 15.68) | 3.8 (3.56, 3.95) | |
Figure 2.
Detailed cause composition of reported AIDS related and non-AIDS related deaths in China, 2013–2022. (A) AIDS related deaths; (B) non-AIDS related deaths.
Abbreviation: AIDS=acquired immunodeficiency syndrome; HIV=human immunodeficiency virus; ADCs=AIDS-defining cancers; NADCs=non-AIDS-defining cancers; CCVDs=cardiovascular and cerebrovascular diseases.
DISCUSSION
The scale-up of ART has played a critical role in the reduction of mortality among individuals infected with HIV. The all-cause mortality rate has exhibited a downward trend. In 2022, the all-cause mortality rate decreased to 2.7%. A study from 2013 revealed that in the top 30 countries with the most significant AIDS-related mortality burden, rates varied from 22 per 1,000 to 91 per 1,000 HIV-infected individuals, in contrast to North America and Western Europe, where the rates were between 4.6 per 1,000 and 15 per 1,000 HIV-infected individuals (3). In the United States, AIDS-related deaths decreased to 4.7 per 1,000 HIV-infected patients in 2017 (4). Research indicates that factors such as viral replication, a lower CD4 count, advanced clinical stage, and injection drug use are consistently associated with increased all-cause mortality (5). To mitigate early mortality, comprehensive strategies, including expanded screenings, management of opportunistic infections, and expeditious initiation of ART, are imperative. Concurrently, non-AIDS-related deaths are almost four times greater than those related to AIDS. The mortality rate in 2022 was higher among individuals over 50 years of age, those infected through heterosexual contact or injection drug use, and those with a CD4 count below 200 cells/mm3. Regional disparities in mortality rates may be attributable to variations in medical infrastructure, professional capacity, and patient demographics.
In the era following the widespread adoption of ART, there has been an observable increase in mortality attributed to non-AIDS-related causes (6). Persistent inflammation and immune activation, consequences of chronic HIV infection, are now acknowledged as primary contributors to the pathogenesis of non-AIDS-related mortality. The risk factors for these conditions include a range of comorbidities, adverse effects associated with ART, the aging process, and lifestyle choices (5). Consequently, routine medical examinations, consistent adherence to ART regimens, lifestyle adjustments such as a nutritious diet, regular exercise, and smoking cessation, as well as proactive management of underlying health conditions, particularly cancer and cardiovascular diseases, are instrumental in decreasing the risk of both AIDS-related and non-AIDS-related deaths. Indeed, cancer constitutes a significant factor in mortality rates, with NADCs showing increased fatality rates, partly due to the advancing age of the HIV-infected population. One of the foremost challenges for clinicians treating HIV-infected individuals is to devise and apply efficacious strategies for the early detection, treatment, and prevention of cancers in this demographic (7).
China has made commendable progress in the expansion of ART and subsequent reduction in mortality rates. Nevertheless, challenges persist. A primary concern is the continued prevalence of late HIV diagnosis. Within Asia, it is estimated that between 34% and 72% of individuals diagnosed with HIV present late (8). Late presentation is associated with an elevated risk of treatment failure, higher mortality, and significant economic impacts. To bridge the diagnostic gap for all people living with HIV, China has launched significant initiatives geared towards early detection. These efforts include implementing anonymous urine testing for HIV, distributing HIV testing kits within MSM communities, advocating the use of novel rapid and self-testing methods among high-risk groups, and mandating health facilities to extend HIV testing to clinical attendees. Additionally, the issue of an aging population among HIV-positive individuals is more pronounced than ever. Between 2015 and 2022, a total of 221,621 cases of HIV-infected individuals aged 60 and older were reported (9). HIV infection may exacerbate the aging process due to sustained inflammatory responses, chronic immune activation, and prolonged use of ART. Older HIV-positive patients are at higher risk of cardiovascular events, opportunistic infections, malignancies, frailty, and mental health disorders compared to their younger and middle-aged counterparts (10). It is incumbent upon healthcare providers from various sectors to integrate management of age-related comorbidities within the regular HIV care framework.
This study presents certain limitations. First, the categorization of fatalities and the ascertainment of specific causes of death are contingent upon the reliability of the reporting individuals, despite them having undergone standardized training. This subjectivity may result in an undetermined number of HIV-positive individuals with causes of death that cannot be classified, potentially leading to an underrepresentation of the proportion of deaths related to AIDS or other causes. Second, as a real-world observational study that relies on routine reporting systems, there is a risk that mortality rates may be underestimated due to delays in death reporting. Moreover, temporal comparisons may be compromised due to the utilization of historical data from various time periods, thus potentially yielding inconsistent mortality outcomes. Furthermore, survivorship bias must be considered, as only those HIV-infected patients who survive can access ART, which may confound interpretations of mortality rates among those receiving treatment.
References
- 1.Joint United Nations Programme on HIV/AIDS. UNAIDS global AIDS update 2022. Geneva: Joint United Nations Programme on HIV/AIDS; 2022. https://www.unaids.org/sites/default/files/media_asset/2022-global-aids-update-summary_en.pdf.
- 2.Zhao Y, Wu ZY, McGoogan JM, Shi CX, Li AH, Dou ZH, et al Immediate antiretroviral therapy decreases mortality among patients with high CD4 counts in China: a nationwide, retrospective cohort study. Clin Infect Dis. 2018;66(5):727–34. doi: 10.1093/cid/cix878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Granich R, Gupta S, Hersh B, Williams B, Montaner J, Young B, et al Trends in AIDS deaths, new infections and ART coverage in the top 30 countries with the highest AIDS mortality burden;1990-2013. PLoS One. 2015;10(7):e0131353. doi: 10.1371/journal.pone.0131353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bosh KA, Johnson AS, Hernandez AL, Prejean J, Taylor J, Wingard R, et al Vital signs: deaths among persons with diagnosed HIV infection, United States, 2010-2018. MMWR Morb Mortal Wkly Rep. 2020;69(46):1717–24. doi: 10.15585/mmwr.mm6946a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trickey A, May MT, Vehreschild J, Obel N, Gill MJ, Crane H, et al Cause-specific mortality in HIV-positive patients who survived ten years after starting antiretroviral therapy. PLoS One. 2016;11(8):e0160460. doi: 10.1371/journal.pone.0160460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weber R, Ruppik M, Rickenbach M, Spoerri A, Furrer H, Battegay M, et al Decreasing mortality and changing patterns of causes of death in the Swiss HIV Cohort Study. HIV Med. 2013;14(4):195–207. doi: 10.1111/j.1468-1293.2012.01051.x. [DOI] [PubMed] [Google Scholar]
- 7.Horner MJ, Shiels MS, Pfeiffer RM, Engels EA Deaths attributable to cancer in the US human immunodeficiency virus population during 2001-2015. Clin Infect Dis. 2021;72(9):e224–31. doi: 10.1093/cid/ciaa1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong CS, Wei L, Kim YS HIV late presenters in Asia: management and public health challenges. AIDS Res Treat. 2023;2023:9488051. doi: 10.1155/2023/9488051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jin YC, Tang HL, Qin QQ, Cai C, Chen FF, Lyu F Epidemiological characteristics and trend of HIV-infected patients aged 60 years and older reported in China, 2015–2022. Chin J Epidemiol. 2023;44(11):1673–8. doi: 10.3760/cma.j.cn112338-20230314-00146. [DOI] [Google Scholar]
- 10.Kiplagat J, Tran DN, Barber T, Njuguna B, Vedanthan R, Triant VA, et al How health systems can adapt to a population ageing with HIV and comorbid disease. Lancet HIV. 2022;9(4):e281–92. doi: 10.1016/S2352-3018(22)00009-1. [DOI] [PubMed] [Google Scholar]