Abstract
Reports of children’s play-related injuries have remained stagnant according to epidemiology studies of the past 3 decades. This article provides a unique look into the context of playground injuries within an entire school district, demonstrating the prevalence of these injuries. This study reports that playgrounds are the leading location of school injury, comprising one-third of all elementary school injuries. This study found that while head/neck injuries were the most commonly injured body region within the playground environment, the proportion of head/neck injuries decreased with age, whereas the proportion of extremity injuries increased with age. At least 1 upper extremity injury required outside medical attention for every 4 that were treated on-site, making upper extremity injuries roughly twice as likely to require outside medical attention as injuries to other body regions. The data in this study are useful for interpreting injury patterns in the context and evaluation of existing safety standards for playgrounds.
Keywords: playground, injury, pediatric, emergency department, child, school
Introduction
The magnitude of unintentional pediatric injuries is a public health concern across the world. Each year, more than 8.6 million children are treated for unintentional injuries in emergency departments (EDs) 1 and cost estimates have been reported at $405 billion. 2 Playground injuries are reported to be the leading location of unintentional recreation injuries to children aged 1 to 10 years with over 200 000 children each year treated in EDs for playground injuries. 1 ,3-8
Playground injury data have been drawn solely from ED and epidemiologic monitoring surveillance systems, such as the National Electronic Injury Surveillance System (NEISS),1,3,4,6,7,9-13 Nationwide Emergency Department Sample (NEDS),2,10 Nationwide Inpatient Sample (NIS),2,10 Canadian Hospitals Injury Reporting and Prevention Program (CHIRPP),5,8 or National Hospital Ambulatory Medical Care Survey (NHAMCS). 14 Information within NEISS, NEDS, and CHIRPP represents injuries that have warranted medical treatment within the ED, while NIS focuses on hospital inpatient admissions. The NHAMCS includes both ED and outpatient ambulatory medical services, although past playground epidemiology studies using NHAMCS were restricted to ED visits. Each of these databases may underestimate the full spectrum of playground injuries that may also be treated at school, childcare settings, home, or other locations without seeking external medical care.
To develop a comprehensive understanding of playground injuries, it is important to utilize a variety of techniques to monitor injury patterns and trends. Past studies have established the significance of playground injuries within the ED and hospital setting. However, without information pertaining to nonemergency injuries, it is impossible to fully contextualize the severity of incidents in the playground environment. Understanding the distribution and severity of playground injuries could help inform governmental and nongovernmental agencies and encourage playground safety prevention at the local, state, and national levels. This is particularly important because epidemiological data are often used as the motivation or justification for safety initiatives.
This study investigates the epidemiological characteristics of playground injuries occurring in 1 of the largest school districts in the United States. This data source captures the range of injury severities, allowing for investigation of the types of playground injuries that are not being reported in national data sources. The objective of the study was to examine sex, age, body region, and injury severity distributions of playground injuries within a school district to better understand the magnitude of their emergent and nonemergent incidences.
Methods
The data for this study were collected from 1 of the largest US school districts, which involves over 150 facilities and a population of over 190 000 students. The school district utilizes an electronic accident reporting form that collects information regarding injuries sustained by students, staff, and visitors which occurs on district property. Personally identifiable data were removed prior to analysis. Data handling and analysis procedures were reviewed and approved by the institutional review board (IRB# 1920-020).
Data utilized for this study focused on a 22-month period between September 2016 and June 2018. This period was selected for study as the school district implemented new injury coding, which allowed for distinction between injuries treated on-site within the school (eg, school nurse, health professional) and those that were referred or treated by emergency services or other health care professionals offsite. For the purposes of this study, injuries treated by school health care providers were coded as “grade I.” Injuries treated by emergency services or other medical/health services nonaffiliated with the school district were coded as “grade II.”
The accident reporting form records information at the time of the incident including the facility, the individual, accident location, body region injured, and injury severity (Table 1). Sex and age were also recorded and used for analysis, with age being grouped into 4 age categories (4-5, 6-7, 8-9, and 10-11 years). The analysis focused on student injuries within the elementary school setting, excluding staff and visitors. For analyses related to body region, if 2 or more body regions were injured, the first-listed (principal) body region was utilized for analysis (Table 2).
Table 1.
Classifications Utilized for Facility, Individual, Accident Location, Body Region, and Injury Severity.
| Facility | Elementary school, middle school, high school, transportation, other/unknown |
| Individual | Student, staff, visitor, other/unknown |
| Accident location a | Administrative area, auditorium, bathroom, cafeteria, classroom, gymnasium, offsite, pavilion, physical education (PE) field, playground, recess (not playground), transportation, walkway, other/unknown |
| Body region | Head/Neck, trunk, upper extremity, lower extremity, other/unknown |
| Severity |
Grade I injury: injuries treated by school health care providers Grade II injury: injuries treated by emergency services or other medical/health services nonaffiliated with the school district |
Accident location hereafter referred to as location.
Table 2.
A Categorization of Body Parts by Each of the 5 Body Regions Utilized in This Study.
| Head/Neck | Ear, eye/eyelid, face, head, mouth/lip, neck, nose, teeth |
| Upper extremity | Arm, elbow, hand/finger, shoulder, wrist |
| Trunk | Abdomen, back, chest, groin, ribs/torso |
| Lower extremity | Ankle, foot, hip, knee, leg/thigh |
| Other/Unknown | Internal injuries, unknown |
Data analysis was broken into 2 principal portions to address the study’s objectives. In part I, analysis was conducted to understand the profile of injury statistics within the elementary school setting, investigating (1) sex, (2) body region, and (3) injury severity across the leading locations of injury within the elementary school. In part II, analysis was limited to the reported injuries within the playground environment of the elementary school to investigate the interrelationships of (1) age and body region, (2) body region and injury severity, and (3) age and injury severity.
Data analysis was performed using Microsoft Excel 2019 pivot tables and Analysis ToolPak (Microsoft Corporation, Redmond, Washington). Results are reported as percentage estimates, including 95% confidence intervals (CIs). Chi-squared tests of independence were calculated in comparative discussions to determine statistical significance, with 2-sided P values of .05 or less being considered significant. SAS statistical analysis software (SAS Institute Inc, Cary, North Carolina) was used to perform Cochran-Armitage trend tests that are used to determine statistical significance for increasing or decreasing trends, with 2-sided P values of .05 or less being considered significant.
Results
During the 22-month period, a total of 15 868 incidents were filed through the accident report form for the entire school district. Of these, 98.5% (n = 15 632, 95% CI = 98.3%-98.7%) were student injuries. Of the student injuries, 68.5% (n = 10 708, 95% CI = 67.8%-69.2%) were reported within district elementary schools. These elementary school injuries are the basis of comparison for the following analysis and discussion.
Part I: A Profile of Injury Statistics Within the Elementary School Setting
The playground was found to be the leading location of injuries within the elementary school setting, comprising 32.6% of all elementary school injuries within the school district (Table 3). The next highest injury locations were the classroom (26.1%) and physical education (PE) field (10.7%). Although excluded from further analysis, the remainder of incident locations within elementary schools were as follows: cafeteria (6.7%), walkway (6.7%), pavilion (3.6%), transportation (1.8%), bathroom (1.7%), offsite (0.4%), administrative area (0.1%), and unreported/unknown (9.6%).
Table 3.
Incident Reports by Location for All Student Injuries Within the Elementary School Setting.
| All locations | 10 708 (100%) |
|---|---|
| Playground | 3494 (32.6%) 95% CI: (31.7%-33.5%) |
| Classroom | 2798 (26.1%) 95% CI: (25.3%-27.0%) |
| PE field | 1143 (10.7%) 95% CI: (10.1%-11.3%) |
| Cafeteria | 716 (6.7%) 95% CI: (6.2%-7.2%) |
| Walkway | 713 (6.7%) 95% CI: (6.2%-7.1%) |
| Pavilion | 389 (3.6%) 95% CI: (3.3%-4.0%) |
| Transportation | 196 (1.8%) 95% CI: (1.6%-2.1%) |
| Bathroom | 180 (1.7%) 95% CI: (1.4%-1.9%) |
| Offsite | 42 (0.4%) 95% CI: (0.3%-0.5%) |
| Administrative area | 13 (0.1%) 95% CI: (0.1%-0.2%) |
| Unreported/Unknown | 1024 (9.6%) 95% CI: (9.0%-10.1%) |
Reporting includes the number of reported injuries, percentage relative to total reported injuries, and 95% CIs.
Abbreviations: CI, confidence interval; PE, physical education.
Part IA: Injury reports by sex and location
The most frequently reported injury locations (playground, classroom, and PE field) within an elementary school setting were analyzed by reported sex to investigate injury trends between the sexes (Table 4). For each of the leading 3 injury locations, injuries to males were reported more frequently than injuries to females. Overall, reported injuries to males accounted for 58.6% of all reported elementary school injuries. In the playground location, males comprised 58.1% of all reported injuries. Similar trends were reported for classroom (59.3%) and PE fields (61.6%).
Table 4.
Injury Reports by Sex for the Leading 3 Locations of Injury (Playground, Classroom, PE Field) and Total for All Locations Within an Elementary School Setting.
| Overall | Playground | Classroom | PE field | All locations |
|---|---|---|---|---|
| 3494 (100%) | 2798 (100%) | 1143 (100%) | 10708 (100%) | |
| Female | 1284 (36.7%) 95% CI = 35.2%-38.3% |
957 (34.2%) 95% CI = 32.4%-36.0% |
369 (32.3%) 95% CI = 29.6%-35.0% |
3805 (35.5%) 95% CI = 34.6%-36.4% |
| Male | 2030 (58.1%) 95% CI = 56.5%-59.7% |
1660 (59.3%) 95% CI = 57.5%-61.1% |
704 (61.6%) 95% CI = 58.8%-64.4% |
6276 (58.6%) 95% CI = 57.7%-59.5% |
| Unreported sex | 180 (5.2%) 95% CI = 4.4%-5.9% |
181 (6.5%) 95% CI = 5.6%-7.4% |
70 (6.1%) 95% CI = 4.7%-7.5% |
627 (5.9%) 95% CI = 5.4%-6.3% |
Reporting includes the number of reported injuries, percentage relative to total reported injuries, and 95% CIs.
Abbreviations: CI, confidence interval; PE, physical education.
Part IB: Body regions and location
Overall, head/neck injuries were consistently found to be the leading body region injured across all locations at 55.5%, including playgrounds (54.3%), classroom (58.6%), and PE fields (48.6%) (Table 5). Upper extremity injuries were next most frequently reported across all locations (20.9%), including playground (20.7%), classroom (21.8%), and PE field (23.0%). Lower extremity injuries followed in frequency for all locations (14.6%), including playground (17.1%), classroom (9.5%), and PE field (20.6%). Specifically within the playground environment, head/neck injuries were the leading body region injured at 54.3%, followed by upper extremities at 20.7%, lower extremities at 17.1%, and trunk at 5.2%.
Table 5.
Injury Reports, Within an Elementary School Setting, of the Leading 3 Locations of Injury (Playground, Classroom, PE Field), and Total for All Locations.
| Female | Male | Overall a | ||
|---|---|---|---|---|
| Playground | Total | 1284 (100%) | 2030 (100%) | 3494 (100%) |
| Head/Neck | 604 (47.0%) 95% CI = 44.3%-49.8% |
1194 (58.8%) 95% CI = 56.7%-61.0% |
1898 (54.3%) 95% CI = 52.7%-56.0% |
|
| Upper extremity | 271 (21.1%) 95% CI = 18.9%-23.3% |
415 (20.4%) 95% CI = 18.7%-22.2% |
722 (20.7%) 95% CI = 19.3%-22.0% |
|
| Lower extremity | 297 (23.1%) 95% CI = 20.8%-25.4% |
275 (13.5%) 95% CI = 12.1%-15.0% |
598 (17.1%) 95% CI = 15.9%-18.4% |
|
| Trunk | 74 (5.8%) 95% CI = 4.5%-7% |
95 (4.7%) 95% CI = 3.8%-5.6% |
181 (5.2%) 95% CI = 4.4%-5.9% |
|
| Other/Unknown | 38 (3.0%) 95% CI = 2.0%-3.9% |
51 (2.5%) 95% CI = 1.8%-3.2% |
95 (2.7%) 95% CI = 2.2%-3.3% |
|
| Classroom | Total | 957 (100%) | 1660 (100%) | 2798 (100%) |
| Head/Neck | 499 (52.1%) 95% CI = 49.0%-55.3% |
1027 (61.9%) 95% CI = 59.5%-64.2% |
1639 (58.6%) 95% CI = 56.8%-60.4% |
|
| Upper extremity | 235 (24.6%) 95% CI = 21.8%-27.3% |
337 (20.3%) 95% CI = 18.4%-22.2% |
609 (21.8%) 95% CI = 20.2%-23.3% |
|
| Lower extremity | 130 (13.6%) 95% CI = 11.4%-15.8% |
123 (7.4%) 95% CI = 6.1%-8.7% |
265 (9.5%) 95% CI = 8.4%-10.6% |
|
| Trunk | 60 (6.3%) 95% CI = 4.7%-7.8% |
115 (6.9%) 95% CI = 5.7%-8.1% |
183 (6.5%) 95% CI = 5.6%-7.5% |
|
| Other/Unknown | 33 (3.4%) 95% CI = 2.3%-4.6% |
58 (3.5%) 95% CI = 2.6%-4.4% |
102 (3.6%) 95% CI = 3.0%-4.3% |
|
| PE field | Total | 369 (100%) | 704 (100%) | 1143 (100%) |
| Head/Neck | 146 (39.6%) 95% CI = 34.6%-44.6% |
378 (53.7%) 95% CI = 50.0%-57.4% |
556 (48.6%) 95% CI = 45.7%-51.5% |
|
| Upper extremity | 97 (26.3%) 95% CI = 21.8%-30.8% |
151 (21.4%) 95% CI = 18.4%-24.5% |
263 (23.0%) 95% CI = 20.6%-25.4% |
|
| Lower extremity | 100 (27.1%) 95% CI = 22.6%-31.6% |
121 (17.2%) 95% CI = 14.4%-20.0% |
236 (20.6%) 95% CI = 18.3%-23% |
|
| Trunk | 19 (5.1%) 95% CI = 2.9%-7.4% |
29 (4.1%) 95% CI = 2.7%-5.6% |
52 (4.5%) 95% CI = 3.3%-5.8% |
|
| Other/Unknown | 7 (1.9%) 95% CI = 0.5%-3.3% |
25 (3.6%) 95% CI = 2.2%-4.9% |
36 (3.1%) 95% CI = 2.1%-4.2% |
|
| All locations | Total | 3805 (100%) | 6276 (100%) | 10708 (100%) |
| Head/Neck | 1860 (48.9%) 95% CI = 47.3%-50.5% |
3723 (59.3%) 95% CI = 58.1%-60.5% |
5940 (55.5%) 95% CI = 54.5%-56.4% |
|
| Upper extremity | 851 (22.4%) 95% CI = 21.0%-23.7% |
1260 (20.1%) 95% CI = 19.1%-21.1% |
2240 (20.9%) 95% CI = 20.1%-21.7% |
|
| Lower extremity | 739 (19.4%) 95% CI = 18.2%-20.7% |
745 (11.9%) 95% CI = 11.1%-12.7% |
1564 (14.6%) 95% CI = 13.9%-15.3% |
|
| Trunk | 211 (5.5%) 95% CI = 4.8%-6.3% |
334 (5.3%) 95% CI = 4.8%-5.9% |
580 (5.4%) 95% CI = 5.0%-5.8% |
|
| Other/Unknown | 144 (3.8%) 95% CI = 3.2%-4.4% |
214 (3.4%) 95% CI = 3.0%-3.9% |
384 (3.6%) 95% CI = 3.2%-3.9% |
For each location, distributions of injury are sorted by body region affected. Reporting includes the number of reported injuries, percentage relative to total reported injuries, and 95% CIs.
Abbreviations: CI, confidence interval; PE, physical education.
Overall includes all injuries (female, male, and unreported).
It should be noted that some gender differences did exist within reported injuries. Males consistently sustained a greater proportion of head/neck injuries compared with females, confirmed by a chi-squared test of independence (P < .001). Also, females consistently sustained a greater proportion of lower extremity injures across accident locations, confirmed by a chi-squared test of independence (P < .001).
Part IC: Location and injury severity
Of all reported elementary school injuries, 87.5% were classified as grade I injuries, which were treated by school health care providers (Table 6). Grade II injuries, referred for outside medical attention, comprised 12.5% of all reported elementary school injuries. In investigating the trends for grades I and II injuries, the PE field displayed a greater probability, 16.7% of a reported grade II injury than the playground, 13.0%, as confirmed by a chi-squared test of independence (P = .002). However, while the PE field led in probability of referral for offsite medical treatment, the playground was the leading location of total reported injuries (n = 3494) and cumulative numbers of grade II injuries (n = 454), during the 22-month period. Of the playground injuries, 87.0% were classified as grade I, while 13.0% were classified as grade II.
Table 6.
Injury Severity Reports, Within an Elementary School Setting, of the Leading 3 Locations of Injury (Playground, Classroom, PE Field), and Total for All Locations.
| Female | Male | Overall a | ||
|---|---|---|---|---|
| Playground | Total | 1284 (100%) | 2030 (100%) | 3494 (100%) |
| Grade I | 1120 (87.2%) 95% CI = 85.4%-89.1% |
1758 (86.6%) 95% CI = 85.1%-88.1% |
3040 (87.0%) 95% CI = 85.9%-88.1% |
|
| Grade II | 164 (12.8%) 95% CI = 10.9%-14.6% |
272 (13.4%) 95% CI = 11.9%-14.9% |
454 (13.0%) 95% CI = 11.9%-14.1% |
|
| Classroom | Total | 957 (100%) | 1660 (100%) | 2798 (100%) |
| Grade I | 867 (90.6%) 95% CI = 88.7%-92.4% |
1475 (88.9%) 95% CI = 87.3%-90.4% |
2506 (89.6%) 95% CI = 88.4%-90.7% |
|
| Grade II | 90 (9.4%) 95% CI = 7.6%-11.3% |
185 (11.1%) 95% CI = 9.6%-12.7% |
292 (10.4%) 95% CI = 9.3%-11.6% |
|
| PE field | Total | 369 (100%) | 704 (100%) | 1143 (100%) |
| Grade I | 313 (84.8%) 95% CI = 81.2%-88.5% |
582 (82.7%) 95% CI = 79.9%-85.5% |
952 (83.3%) 95% CI = 81.1%-85.5% |
|
| Grade II | 56 (15.2%) 95% CI = 11.5%-18.8% |
122 (17.3%) 95% CI = 14.5%-20.1% |
191 (16.7%) 95% CI = 14.5%-18.9% |
|
| All locations | Total | 3805 (100%) | 6276 (100%) | 10708 (100%) |
| Grade I | 3365 (88.4%) 95% CI = 87.4%-89.5% |
5450 (86.8%) 95% CI = 86.0%-87.7% |
9372 (87.5%) 95% CI = 86.9%-88.1% |
|
| Grade II | 440 (11.6%) 95% CI = 10.5%-12.6% |
826 (13.2%) 95% CI = 12.3%-14.0% |
1336 (12.5%) 95% CI = 11.9%-13.1% |
For each location, distributions of injury are sorted by injury severity. Reporting includes the number of reported injuries, percentage relative to total reported injuries, and 95% CIs.
Abbreviations: CI, confidence interval; PE, physical education.
Overall includes all injuries (female, male, and unreported).
Part II: Playground Injury Trends
As previously noted, the playground was the leading location of injuries within an elementary school setting, and the 3494 reported injuries are the basis of comparison for the following sections (part IIA-IIC).
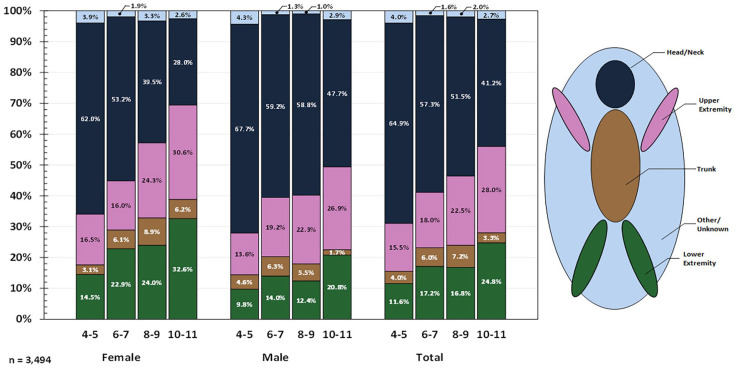
Part IIA: Body region and age
Investigating playground injuries by body region(s) injured and age, it was determined that as age increases, a decrease in the number of reported head/neck injuries was observed, whereas reported upper and lower extremity injuries became more prevalent (Figure 1). In total, the percentage of reported head/neck injuries decreases from 64.9% (n = 426 of 656, 95% CI = 61.3%-68.6%) of children aged 4 to 5 years to 41.2% (n = 228 of 553, 95% CI = 37.1%-45.3%) of 10- to 11-year-olds. The decreasing trend of head/neck injuries among age groups was confirmed by the Cochran-Armitage trend test (P < .001).
Figure 1.
Distribution of injured body region by age ranges, occurring on elementary school playgrounds. Each body region (head/neck, upper extremity, trunk, lower extremity, and other/unknown) coded to the key to the right.
In contrast, lower and upper extremity injuries increased as children aged. Children aged 4 to 5 years had a smaller percentage of lower extremity injuries (11.6% [n = 76 of 656, 95% CI = 9.1%-14%]) compared with those aged 10 to 11 years (24.8% [n = 137 of 553, 95% CI = 21.2%-28.4%]). Similarly, children aged 4 to 5 years had a lower percentage of upper extremity injuries (15.5% [n = 102 of 656, 95% CI = 12.8%-18.3%]) than children aged 10 to 11 years (28.0% [n = 155 of 553, 95% CI = 24.3%-31.8%]). The increasing trend of both lower and upper extremity injury reports among age groups was confirmed by the Cochran-Armitage trend test (P < .001).
Part IIB: Injury severity and body region
Investigating the percentages of grade II injuries reported for each body region illustrates the frequency at which different body regions required outside medical attention. Overall, 12.8% of female injuries (n = 164 of 1284, 95% CI = 10.9%-14.6%) and 13.4% of male injuries (n = 272 of 2030, 95% CI = 11.9%-14.9%) were grade II injuries treated by emergency services or other medical services outside the school system (Figure 2).
Figure 2.
Percentage of grade II injuries from total injuries by body region, occurring on elementary school playgrounds. Grade II injuries reflect injuries treated by emergency services or other health care professionals outside of the school district.
Upper extremity injuries an increased probability to require outside medical attention, compared with most other body regions. Female upper extremity injuries were deferred to outside medical attention in 20.7% of cases (n = 56 of 271, 95% CI = 15.8%-25.5%), a statistically significant increase compared with other body regions, as confirmed by a chi-squared test of independence (P < .001). Similarly, male upper extremity injuries were deferred to outside medical attention in 21.2% of cases (n = 88 of 415, 95% CI = 17.3%-25.1%), also a statistically significant increase compared with other body regions (P < .001). Although female trunk injuries were referred for outside medical attention in 18.9% of cases, the number of reports was small (n = 14 of 74, 95% CI = 10.0%-27.8%); this was not found to be statistically significant compared with other body regions (P = .102).
Part IIC: Injury severity and age
Investigating the percentages of grade II injuries compared with total injuries reported for different age ranges illustrates which age ranges require outside medical attention most frequently. Overall, females (all ages) were sent for outside medical attention in 12.8% (n = 164 of 1284, 95% CI = 10.9%-14.6%) of all reported female injury cases. Males (all ages) were sent for outside medical attention in 13.4% (n = 272 of 2030, 95% CI = 11.9%-14.9%) of all reported male injury cases (Figure 3). The differences between female and male rates of referral for outside medical care (grade II) were not found to be significant by a chi-squared test of independence (P = .577). The most cumulative playground injuries were reported for ages 6 to 7 years (n = 920), followed by 8- to 9-year-olds (n = 811), then 4- to 5-year-olds (n = 623), with the fewest injuries in the older age group of 10- to 11-year-olds (n = 539).
Figure 3.
Percentage of grade II injuries from total injuries by age ranges, occurring on elementary school playgrounds. Grade II injuries reflect injuries treated by emergency services or other health care professionals outside of the school district.
The probability of a grade II injury was found to increase by age for both sexes. For females, the percentage of reported grade II injuries increased within each age group beginning with 9.4% (n = 24 of 255, 95% CI = 5.8%-13%) from ages 4 to 5 years, continuing with ages 6 to 7 years at 9.9% (n = 36 of 363, 95% CI = 6.8%-13%), ages 8 to 9 years at 12.8% (n = 39 of 304, 95% CI = 9.1%-16.6%), and ultimately reaching 21.2% (n = 41 of 193, 95% CI = 15.5%-27%) for females aged 10 to 11 years. For males, the percentage of reported grade II injuries also increased within each age group beginning with 9.0% (n = 33 of 368, 95% CI = 6.0%-11.9%) from ages 4 to 5 years, continuing with ages 6 to 7 years at 11.3% (n = 63 of 557, 95% CI = 8.7%-13.9%), ages 8 to 9 years at 15.8% (n = 80 of 507, 95% CI = 12.6%-19.0%), and ultimately reaching 17.3% (n = 60 of 346, 95% CI = 13.4%-21.3%) for males aged 10 to 11 years. The increasing trend of grade II injuries among age groups was confirmed by the Cochran-Armitage trend test (P < .001) for both females and males.
Discussion
Current knowledge of playground injuries has been limited based on the available samples developed from analysis on injuries reported only within the context of medical treatment. Past studies’ utilization of NEISS, NEDS, NIS, or NHAMCS data sets provides potentially disproportionate insight into injuries that trend toward more serious severities, given that they are constructed from health care–based surveillance systems.
Within this study, grade I injuries (reflecting injuries treated on-site) comprised 87.5% of the entire data set, while the remaining 12.5% grade II injuries were treated by emergency services or other health care professionals. A similar pattern was observed on the playground setting with 87.0% of injuries being reported as grade I and 13.0% being reported as grade II. Although the inclusion criterion for grade II injury classification is not identical to that of large surveillance systems, past study’s epidemiology data sets will most closely align with this study’s grade II data subset. This study illuminates significant issues that would be unnoticed in the context of surveillance derived solely from ED or other health care visits, and adds to previous reports of playground injury data. Phelan suggested that playground injuries are potentially underappreciated, and found that playgrounds lead to proportionately more severe injuries than other common injury locations. 14 The findings of this study support this assertion, with playgrounds leading all other locations within the elementary school environment for grade II injuries (34.0%, n = 454 of 1336).
Both upper extremity and head injuries are commonly reported injuries within past studies of the playground environment.4,6,9-11,13,14 It has been reported that the most commonly injured body regions are the upper extremities (42.9%-44.0%) followed by the head and neck (34.2%-35.8%).3,4 In addition, past studies have reported that within the playground setting, fractures to the upper limbs are the most common injury relative to other body regions, accounting for approximately one-third of all ED-treated injuries.10,11 The data from this study support these previous assertations, as head/neck injuries and upper extremity injuries are most widely reported overall, and also constitute the majority of injuries seen by emergency services or referred to other health care professionals outside the school district.
Although this study found that head/neck injuries lead upper extremity injuries by raw numbers, the likelihood of sustaining a grade II injury requiring outside medical attention is twice as likely for an upper extremity injury (20.7% female, 21.2% male) compared with a head/neck injury (10.1% female, 12.7% male). These findings would not be detected based solely on an ED-based surveillance system. Past studies have raised concerns regarding the potential lack of sensitivity for current playground testing methods to prevent all injury modalities, advocating for the development of injury criteria more closely considering upper extremity injury.4,6,15 Future investigations on the differences in injury mechanisms for different body regions would build understanding of the overall effectiveness of current injury prevention strategies.
Within this study, it is found that males sustained injuries at a rate nearly twice that of females—both on the playground setting (males = 2030 to females = 1284) and all locations combined (males = 6276 to females = 3805). However, the likelihood of an injury requiring outside medical attention (grade II) is similar for either sex. Within the playground setting, females and males each required outside medical attention (grade II) in approximately 13% of reported injuries (females = 12.8% and males = 13.4%). Overall, for all locations within the elementary school, females required outside medical attention (grade II) for 11.6% of reported injuries and males for 13.2% of reported injuries.
On the playground, the likelihood of injury requiring medical attention increases with increasing age. At the same time, the injury distribution by body region changes. Reported head/neck injuries decrease with age, whereas reports of upper and lower extremity injuries increase, tending to be more severe. The factors that lead to these changes warrant further attention and are likely due to a variety of cofactors such as changes to the nature of play, the equipment and activities available to different age ranges, musculoskeletal and motor skill development, psychological development, and perhaps the size of the student cohorts utilizing the space at a given time.
Implications of Findings
The data in this study are useful for the interpretation of injury patterns in the context of existing safety standards for playgrounds. Many standard organizations such as ASTM International and the Canadian Standards Association publish standards related to playground injury prevention.16-18 These standards are then utilized for the certification of equipment and materials—and, while the standards are of themselves, nonbinding, they are often adopted as minimum performance requirements from national, statewide, or local agencies.
Currently, playground safety standards such as ASTM F1292 16 and US Consumer Product Safety Commission (CPSC) guidelines found in the Public Playground Safety Handbook 19 focus on playground safety and reducing the potential for a severe head injury via playground safety surfacing. In this study, the fact that head/neck injuries are less likely to require outside medical attention than the next most commonly injured body region (upper extremity) is a positive finding and may suggest the effectiveness of those safety efforts for head injury prevention. However, the findings from this study purport that upper extremity injuries requiring medical attention seem to be occurring at a rate disproportionate to other injury modalities. This study, and others investigating playground injuries, would benefit from the availability of more specific injury data. It is encouraged that accident report forms provide more information regarding playground surfacing, equipment type, activity at the time of injury, type of injury, injury mechanism (eg, falls, collisions), number of children and age(s) using the playground, and other details of the specific injury sustained.
Understanding injury incidence on playgrounds presents the opportunity to underscore the importance of supervised safe play for children. Play is widely acknowledged to provide children with various physical, emotional, social, and intellectual benefits.20-22 The importance of play within schools has been particularly recognized. 23 Best practices for providing safe play may involve supervision practices, physical design, fall protection surfacing, and equipment maintenance.24,25 To provide safe play experiences, increased emphasis should be placed on the development of supervision, design, and maintenance practices which align with a comprehensive understanding of injuries within a playground environment.
Limitations
The database used in this study was encumbered by several limitations, which present some opportunities for further investigation. First, as the database was designed for broad surveillance from within an entire school system, the specific detail provided about the nature of playground injuries (such as the involvement of specific equipment, details of the fall, impact, or other injury mechanism) was limited. The absence of data on the exact playground equipment where a child sustained an injury currently limits the ability for specific safety recommendations such as upper extremity injury mitigation. Also, as the data were reported internally from the school system, it did not include details of the specific injuries sustained. Therefore, it was only possible to determine the body region injured, as medical coding for the resulting injury diagnosis was not available. Improved sampling, perhaps initiated by injuries with specific attributes, could provide more specific information regarding the specific injury diagnosis, severity, involvement of equipment/surfacing, and injury mechanism.
Conclusions
Children’s play is integral in their cognitive, social, and physical development. Still, reported playground injuries over the past 3 decades have remained steady with approximately 200 000 ED visits per year in the United States. Past playground injury epidemiologic data have been drawn predominantly from ED-based and hospital admissions–based data, which complicates interpretation of the complete spectrum of injuries that children incur on a playground environment. Within the school environment of this study, reports of upper and lower extremity injuries are shown to increase with age, whereas head/neck injuries are shown to decrease with age. In addition, upper extremity injuries, while reported in fewer numbers than head/neck injuries, are shown to require outside medical treatment at a higher, disproportionate rate compared with other body regions, underscoring a need to better understand these upper extremity injury mechanisms and investigate potential injury mitigations. The observations of these playground injuries from the elementary school environment underscore the need for continued innovation in injury prevention, playground supervision training, and practices to provide enhanced play experiences that leverage the benefits of play.
Author Contributions
The overarching project was initiated by EAK and HMO. The principal data analysis team was DAF and ZDP, with technical guidance from EAK, and HMO providing insight into the implications of findings relative to the school and playground environments. All authors contributed to the final manuscript.
Acknowledgments
The authors wish to thank Jove Graham, PhD, and Luke Riexinger, PhD, for their statistical guidance, suggestions, and feedback on data analysis design and interpretation.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Data handling and analysis procedures were reviewed and approved by Bucknell University’s Institutional Review Board (IRB# 1920-020).
ORCID iD: Eric A. Kennedy  https://orcid.org/0000-0002-8323-7913
https://orcid.org/0000-0002-8323-7913
References
- 1. Schwebel DC, Brezausek CM. Child development and pediatric sport and recreational injuries by age. J Athl Train. 2014;49(6):780-785. doi: 10.4085/1062-6050-49.3.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zonfrillo MR, Spicer RS, Lawrence BA, Miller TR. Incidence and costs of injuries to children and adults in the United States. Inj Epidemiol. 2018;5(1):37. doi: 10.1186/s40621-018-0167-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nabavizadeh B, Hakam N, Holler JT, et al. Epidemiology of child playground equipment-related injuries in the USA: emergency department visits, 1995-2019. J Paediatr Child Health. 2022;58:69-76. doi: 10.1111/jpc.15644 [DOI] [PubMed] [Google Scholar]
- 4. Adelson SL, Chounthirath T, Hodges NL, Collins CL, Smith GA. Pediatric playground-related injuries treated in hospital emergency departments in the United States. Clin Pediatr (Phila). 2018;57(5):584-592. doi: 10.1177/0009922817732144 [DOI] [PubMed] [Google Scholar]
- 5. Keays G, Skinner R. Playground equipment injuries at home versus those in public settings: differences in severity. Inj Prev. 2012;18(2):138-141. doi: 10.1136/injuryprev-2011-040240 [DOI] [PubMed] [Google Scholar]
- 6. Vollman D, Witsaman R, Comstock RD, Smith GA. Epidemiology of playground equipment-related injuries to children in the United States, 1996-2005. Clin Pediatr. 2009;48:66-71. doi: 10.1177/0009922808321898 [DOI] [PubMed] [Google Scholar]
- 7. Tinsworth DK, McDonald JE. Special Study: Injuries and Deaths Associated With Children’s Playground Equipment. Washington, DC: US Consumer Product Safety Commission; 2001. [Google Scholar]
- 8. Macarthur C, Hu X, Wesson DE, Parkin PC. Risk factors for severe injuries associated with falls from playground equipment. Accid Anal Prev. 2000;32(3):377-382. doi: 10.1016/s0001-4575(99)00079-2 [DOI] [PubMed] [Google Scholar]
- 9. Hanway S. Injuries and Investigated Deaths Associated With Playground Equipment, 2009-2014. Washington, DC: US Consumer Product Safety Commission; 2016. [Google Scholar]
- 10. Tuckel P, Milczarski W, Silverman DG. Injuries caused by falls from playground equipment in the United States. Clin Pediatr (Phila). 2018;57(5):563-573. doi: 10.1177/0009922817732618 [DOI] [PubMed] [Google Scholar]
- 11. Loder RT. The demographics of playground equipment injuries in children. J Pediatr Surg. 2008;43(4):691-699. doi: 10.1016/j.jpedsurg.2007.12.061 [DOI] [PubMed] [Google Scholar]
- 12. Cheng TA, Bell JM, Haileyesus T, Gilchrist J, Sugerman DE, Coronado VG. Nonfatal playground-related traumatic brain injuries among children, 2001-2013. Pediatrics. 2016;137(6):e20152721. doi: 10.1542/peds.2015-2721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. O’brien C. Injuries and Investigated Deaths Associated With Playground Equipment, 2001–2008. Washington, DC: US Consumer Product Safety Commission; 2009. [Google Scholar]
- 14. Phelan KJ, Khoury J, Kalkwarf HJ, Lanphear BP. Trends and patterns of playground injuries in United States children and adolescents. Ambul Pediatr. 2001;1(4):227-233. doi: [DOI] [PubMed] [Google Scholar]
- 15. Sherker S, Ozanne -Smith J. Are current playground safety standards adequate for preventing arm fractures? Med J Aust. 2004;180(11):562-565. doi: 10.5694/j.1326-5377.2004.tb06092.x [DOI] [PubMed] [Google Scholar]
- 16. ASTM International. Standard Specification for Impact Attenuation of Surfacing Materials Within the Use Zone of Playground Equipment (F1292-18e1). West Conshohocken, PA: ASTM International; 2018. [Google Scholar]
- 17. ASTM International. Standard Consumer Safety Performance Specification for Playground Equipment for Public Use (F1487-17). West Conshohocken, PA: ASTM International; 2017. [Google Scholar]
- 18. Canadian Standards Association Group. Children’s playground equipment and surfacing (CAN/CSA-Z614). Published 2014. Accessed April 19, 2023. https://www.csagroup.org/store/product/CSA%20Z614:20/
- 19. US Consumer Product Safety Commission. Handbook for Public Playground Safety. Bethesda, MD: US Consumer Product Safety Commission; 2015. [Google Scholar]
- 20. Herrington S, Brussoni M. Beyond physical activity: the importance of play and nature-based play spaces for children’s health and development. Curr Obes Rep. 2015;4(4):477-483. doi: 10.1007/s13679-015-0179-2. [DOI] [PubMed] [Google Scholar]
- 21. Schaefer L, Plotnikoff RC, Majumdar SR, et al. Outdoor time is associated with physical activity, sedentary time, and cardiorespiratory fitness in youth. J Pediatr. 2014;165(3):516-521. doi: 10.1016/j.jpeds.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 22. Wells NM, Evans GW. Nearby nature: a buffer of life stress among rural children. Environ Behav. 2003;35(3):311-330. doi: 10.1177/0013916503035003001. [DOI] [Google Scholar]
- 23. Ramstetter CL, Murray R, Garner AS. The crucial role of recess in schools. J Sch Health. 2010;80(11):517-526. doi: 10.1111/j.1746-1561.2010.00537.x. [DOI] [PubMed] [Google Scholar]
- 24. Olsen HM, Hudson SD, Thompson D. Developing a playground injury prevention plan. J Sch Nurs. 2008;24(3):131-137. doi: 10.1177/1059840532143214. [DOI] [PubMed] [Google Scholar]
- 25. Olsen H, Kennedy E. Safety of school playgrounds: field analysis from a randomized sample. J Sch Nurs. 2020;36(5):369-375. doi: 10.1177/1059840519827364. [DOI] [PubMed] [Google Scholar]