Abstract
Objectives:
The primary purpose of this study was to compare the rates of nonunion among different osteotomy designs (company brand) and the rates of nonunion between oblique and transverse osteotomies. We secondarily aimed to assess the differences in reoperation and hardware removal rates after ulnar shortening osteotomy (USO).
Methods:
A retrospective cohort study of patients undergoing ulnar shortening osteotomy between 2015 and 2022 in our institute amongst 17 providers resulted in 92 consecutive patients. We included skeletally mature patients who underwent USO for the ulnar impingement abutment diagnosis. Demographic information was collected, including age, gender, race/ethnicity, BMI, and medical comorbidities. Six brand-specific devices were used and compared to the conventional plate fixation. Nonunion was determined based on the final available radiograph with a minimum follow-up of four months.
Results:
Of the 92 patients, 83 (90%) had a bone union. There is a remarkable difference in union among implant brands, although statistical analysis was not performed due to the small number of patients in each group. Transverse osteotomy was significantly related to a higher nonunion rate. Out of nine patients with resultant nonunion (10%), three healed after revision surgery (3.2%), two were lost to follow-up (2.2%), and four remained asymptomatic despite radiographic nonunion (4.6%). Plate removal was performed in four patients (4.3%), all of whom were in the union group.
Conclusion:
Patients should be informed about the nonunion rate with possible subsequent secondary surgery. Using procedure-specific devices may have mitigated the risk of nonunion.
Key Words: Hand, Instrumentation systems, Osteotomy, Outcomes, Procedure-specific, Ulnar
Introduction
Painless load transmission along the forearm needs a relatively appropriate length of the radius and ulna. Ulnar length change by only 2.5 mm has been shown to alter the pattern of load transmission across the wrist substantially.1 Positive ulnar variance is presumed to cause ulnar impaction syndrome and ulnar-sided wrist pain.2,3 Milch (1942) pioneered the ulnar shortening osteotomy to address ulnar impaction syndrome.4 Since then, many authors have reported equivocal but overall satisfactory results from this intervention.5,6
Various devices and designs have been developed to address intraoperative and postoperative technical and device-related issues, facilitate surgery, and avoid nonunion.7-12 Technical concerns include rotational instability after osteotomy, under or over-shortening, over-compressing, overheating the cut surface, and cutting oblique versus transverse osteotomy. Device-related factors that can potentially influence clinical outcomes are the distance of the bone cut from the articular surface, the location of the cut relative to the distal oblique ligament, the number of screws, and the locking versus the non-locking system.7-12 The literature is inconclusive in this regard, and to date, no significant differences have been observed between different designs. The outcomes have been comparable between the freehand bone cut and the Rayhack technique (using osteotomy-specific jigs), except for the higher cost associated with the latter.13
A review of Acumed’s ulnar osteotomy system demonstrated a 100% union rate without delayed unions or hardware removal.14 The initial report of oblique osteotomies by Rayhack in 1993 showed a shorter union time than transverse osteotomy.9 However, recent studies have demonstrated that union rates did not significantly differ between the two methods, or between conventional versus procedure-specific designs.15-17 Additionally, no studies have evaluated the differences in union rates between the commonly used implant brands.
The primary purpose of this study was to compare the rates of nonunion among different USO plate manufacturers and the rates of nonunion between oblique and transverse osteotomies. We secondarily aimed to assess the differences in reoperation and hardware removal rates after ulnar shortening osteotomy.
Materials and Methods
After Institutional Review Board approval and a waiver of informed consent per institutional protocol, a retrospective cohort study of patients undergoing ulnar shortening osteotomy from October 2015 to February 2022 in a single institute, including 17 hand fellowship-trained providers. Patients were identified by query of our institutional database using the Current Procedural Terminology (CPT) codes 25360 and 25390, corresponding to repair, revision, and reconstruction procedures on the forearm and wrist. Cohort selection was further refined by confirming the pre-op diagnosis of ulnar impingement in skeletally mature patients who underwent USO. We excluded radial shortening osteotomies, Darrach, Wafer, and any procedures on the ulnar head. Patients with Madelung or congenital deformities were also excluded. We also excluded patients with less than four months of follow-up (two patients). Demographic information was collected, including age, gender, race/ethnicity, BMI, and medical comorbidities.
Our primary outcome measure was union versus nonunion. Union was defined as bone bridging with trabeculation at >75% of the osteotomy in the view least obscured by the plate. Three authors determined the time to union and the presence of non-union. Two assessors reviewed each radiograph to increase the agreement. Explanatory variables were determined by surveying the operative notes to identify the brand of the implant and the amount of shortening (mm). Operative notes were also surveyed to identify any concurrent procedures. Patient chart records were thoroughly reviewed to determine if any revision surgeries or hardware removal had to be performed after the initial procedure. Moreover, the immediate post-operative radiographs at 7-12 days were reviewed to determine the number of proximal screws, distal screws, distance from the osteotomy to the distal ulna (mm), and the type of osteotomy (transverse or oblique). Subsequent radiographs at an average interval of 6, 10-12, and 16-20 weeks were reviewed to determine the time to union. In the case of a nonunion, the patient’s radiographs were reviewed until the final available follow-up.
A final cohort of 92 patients who met the inclusion and exclusion criteria was included in this study.
USO systems
Patients and outcomes were further subdivided by the implant brand to look at the impact of the overall system. This permitted assessment of the osteotomy location, osteotomy system, type of osteotomy, and the plate and screw design. The working distance of the most proximal and distal screws from the osteotomy site is another factor in each design. Six different osteotomy-specific designs were compared with the conventional osteotomy and fixation [Figures 1A-5B]. Total number of 92 patients included Aptus (Medartis, Basel, Switzerland) (n=22), TriMed (Santa Clarita, California, USA) (n=22), Synthes (Depuy-Synthes, Switzerland) (n=17), Rayhack (Wright Medical, Memphis, Tennessee, USA (n=18), Skeletal Dynamics (Miami, Florida, USA) (n=3), and Acumed (Hillsboro, Oregon, USA) (n=2). In eight patients, osteotomy was made freehand and was fixed using a conventional Synthes LC-DCP.
Figure 1.

A: Immediate postop radiograph using LC-DCP and transverse freehand ulnar osteotomy in a 50-year-old female/B: Follow-up radiograph after 17 months showing nonunion
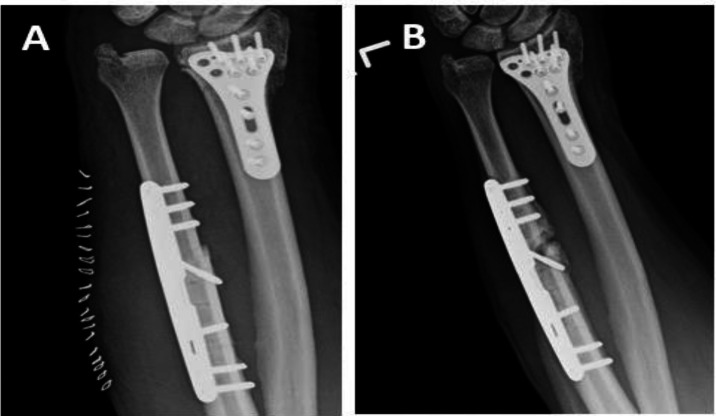
Figure 5.
A: Immediate postop radiograph using TriMed system with oblique osteotomy in a 69-year-old Male / B: Follow-up radiograph after 4 months showing nonunion
Figure 2.
A: Immediate postop radiograph using Rayhack system with oblique osteotomy in a 40-year-old female/ B: Follow-up radiograph after 4 months showing nonunion
Figure 3.
A: Immediate postop radiograph using Skeletal Dynamics system with transverse osteotomy in a 55-year-old Male / B: Follow-up radiograph after 8 months showing nonunion
Figure 4.
A: Immediate postop radiograph using Synthes system with transverse osteotomy in a 55-year-old Male / B: Follow-up radiograph after 6 months showing nonunion
Statistical Analysis
We performed a univariable analysis to assess the influence of each explanatory variable on union versus nonunion. Categorical data was presented as cell count (%), and continuous data was presented as mean (SD). Parametric continuous data were presented as mean (SD), and p-values were calculated by performing T-tests. Nonparametric continuous data was also presented as mean (SD) for easier interpretation, and p-values were calculated by performing Mann-Whitney tests. Chi-square or Fisher’s Exact tests were used to calculate p-values for categorical data. P-values < 0.05 were considered significant.
Results
We included 92 patients in this study with a mean age of 48 years (SD=15), including 58 females and 34 males. Of the 92 patients, 83 (90%) had a bone union, with an average time to the union being 83 days (range 20-494 days) [Table 1]. All patients had a minimum of four months follow-up after surgery.
Table 1.
Summary Descriptive Table Comparing Union and Nonunion Groups
| Total Data | No | Yes | OR | P Value | |
|---|---|---|---|---|---|
| N=92 | N=9 | N=83 | |||
| Age | 47.8 (14.8) | 55.4 (8.90) | 47.0 (15.1) | 0.96 [0.91;1.01] | 0.026 |
| Race: | 0.646 | ||||
| White | 63 (80.8%) | 6 (75.0%) | 57 (81.4%) | Ref. | |
| Other | 15 (19.2%) | 2 (25.0%) | 13 (18.6%) | 0.66 [0.13;5.44] | |
| Ethnicity: | 1.000 | ||||
| Not Hispanic | 76 (97.4%) | 9 (100%) | 67 (97.1%) | ||
| Hispanic | 2 (2.56%) | 0 (0.00%) | 2 (2.90%) | ||
| Sex: | 0.282 | ||||
| Female | 58 (63.0%) | 4 (44.4%) | 54 (65.1%) | Ref. | |
| Male | 34 (37.0%) | 5 (55.6%) | 29 (34.9%) | 0.44 [0.10;1.84] | |
| BMI | 27.4 (4.64) | 29.0 (4.84) | 27.2 (4.62) | 0.92 [0.80;1.07] | 0.333 |
| Ulnar shortening osteotomy: Yes | 92 (100%) | 9 (100%) | 83 (100%) | ||
| Transverse vs Oblique: | 0.003 | ||||
| Oblique | 84 (91.3%) | 5 (55.6%) | 79 (95.2%) | Ref. | |
| Transverse | 8 (8.70%) | 4 (44.4%) | 4 (4.82%) | 0.07 [0.01;0.38] | |
| # Screws Distal | 3.21 (0.43) | 3.11 (0.60) | 3.22 (0.41) | 1.91 [0.31;11.8] | 0.619 |
| # Screws Distal: | 0.118 | ||||
| 2 | 1 (1.09%) | 1 (11.1%) | 0 (0.00%) | ||
| 3 | 71 (77.2%) | 6 (66.7%) | 65 (78.3%) | ||
| 4 | 20 (21.7%) | 2 (22.2%) | 18 (21.7%) | ||
| # Screws Proximal | 3.14 (0.53) | 3.00 (0.50) | 3.16 (0.53) | 1.80 [0.47;6.96] | 0.396 |
| # Screws Proximal: | 0.605 | ||||
| 2 | 7 (7.61%) | 1 (11.1%) | 6 (7.23%) | Ref. | |
| 3 | 65 (70.7%) | 7 (77.8%) | 58 (69.9%) | 1.51 [0.05;11.4] | |
| 4 | 20 (21.7%) | 1 (11.1%) | 19 (22.9%) | 3.01 [0.07;129] | |
| Distance from Osteotomy to Distal Ulna | 71.0 (17.5) | 68.4 (24.6) | 71.3 (16.8) | 1.01 [0.97;1.05] | 0.742 |
| Amount of Shortening (mm) | 3.69 (1.24) | 4.12 (1.58) | 3.64 (1.20) | 0.76 [0.45;1.28] | 0.498 |
| Locking Screws: | 0.713 | ||||
| No | 61 (66.3%) | 7 (77.8%) | 54 (65.1%) | Ref. | |
| Yes | 31 (33.7%) | 2 (22.2%) | 29 (34.9%) | 1.78 [0.39;13.9] | |
| Non-Locking Screws: | 0.733 | ||||
| No | 56 (60.9%) | 5 (55.6%) | 51 (61.4%) | Ref. | |
| Yes | 36 (39.1%) | 4 (44.4%) | 32 (38.6%) | 0.78 [0.19;3.51] | |
| Time to Union | 77.3 (35.3) | 77.3 (35.3) |
In a univariate analysis, factors that had a significant influence on a higher chance of union were age (younger) and type of osteotomy (oblique) [Table 1]. Other factors, including the number of proximal and distal screws, distance from osteotomy to the distal ulna, and amount of shortening, did not significantly affect union.
There is a trend towards higher union with specific brands. However, because of the low numbers in each group, statistical analysis was not possible [Table 2]. Table 2 presents the details of the nine patients with nonunion. Most patients had concomitant procedures alongside their ulnar shortening osteotomy, including an open or arthroscopic TFCC repair/debridement [Table 3].
Table 2.
Patients with Nonunion
| Number | Age | Sex | Implant Brand | Osteotomy type | Concomitant Surgery | Months to final FW | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | 60 | M | Synthes | T | Scope w/ TFCC debridement, pisotriquetral cyst drainage | 6 | Nonunion |
| 2 | 46 | F | Synthes | O | Scope w/ synvectomy and TFCC repair | 14 | Nonunion |
| 3 | 50 | F | LC-DCP | T | Scope w/ debridement | 21 | Nonunion |
| 4 | 59 | F | Synthes | O | Scope w/ TFCC debridement | 25 | Nonunion |
| 5 | 55 | M | Skeletal Dynamics | T | Scope w/ TFCC debridement | 28 | Partial union after revision surgery (healed on lateral view but nounion on PA view. |
| 6 | 57 | M | Skeletal Dynamics | T | Scope w/ TFCC debridement | 14 | Union after revision surgery |
| 7 | 63 | F | LC-DCP | O | Scope w/ TFCC debridement, fluoroscopy | 8.5 | Union AFTER revision surgery |
| 8 | 40 | F | Rayhack | O | DRUJ ligament reconstruction, posterior interosseous nerve neurectomy | 4 | Lost to Fw before confirmation of bone union |
| 9 | 69 | M | TriMed | O | Open repair of TFCC tear | 4 | Lost to FW before confirmation of bone union |
*FW = Follow-up/*TFCC = Triangular fibrocartilage complex/*DRUJ = distal radioulnar joint/*ORIF = Open reduction and internal fixation/*O = Oblique/*T = Transverse
Table 3.
Concomitant Procedures of Participants
| Concomitant Procedure | Number of Participants (N=94 but some participants had more than on concomitant procedure) |
|---|---|
| Open or arthroscopic TFCC repair/debridement | 82 |
| Flexor tenosynovectomy | 3 |
| Pisotriquetral cyst drainage | 1 |
| Arthroscopic wrist debridement | 6 |
| Ulnar styloid excision | 2 |
| Hardware removal | 5 |
| Lunate chondropalasty | 7 |
| 1st extensor compartment release | 3 |
| Distal Radius osteotomy | 1 |
| DRUJ ligament reconstruction | 1 |
| Posterior interosseous nerve neurectomy | 1 |
*TFCC=Triangular fibrocartilage complex/*DRUJ=distal radioulnar joint
Subsequent surgeries included three surgeries to revise nonunion, which resulted in union in all three patients. Hardware removal was performed in four patients in the union group due to hardware irritation [Table 4].
Table 4.
Patients with Removal of Hardware
| Number | Age | Sex | Implant Brand | Osteotomy type | Concomitant Surgery | Months to final FW |
|---|---|---|---|---|---|---|
| 1 | 69 | F | Rayhack | O | Scope w/ synovectomy and TFCC debridement | 12 |
| 2 | 31 | F | Rayhack | O | Scope w/ TFCC debridement | 13 |
| 3 | 21 | M | Synthes | O | Scope w/ TFCC debridement, open ulnar styloid tip excision | 11 |
| 4 | 33 | M | LC-DCP | O | 1st extensor compartment release, scope w/ TFCC debridement, partial lunotriquetral ligament debridement, lunate and triquetrum chondroplasty | 36 |
Discussion
This study aimed to determine the overall nonunion rate and the influencing factors after an ulnar shortening osteotomy. We specifically looked at the union rate among different systems available in the market, each including a combination of several factors. There was a significant difference in union rate among the brands, with oblique osteotomy showing a higher union rate.
One obstacle to ulnar shortening osteotomies is prolonged healing time, as Rayhack (1993) reported.9 Since the procedure was introduced around 70 years ago, ulnar shortening osteotomies have been technically challenging and known to have hardware-related complaints. However, the procedure has evolved to facilitate more reliable fixation, decreasing hardware irritation, overall complications, and lower nonunion rate.14
The initial report of oblique osteotomy by Rayhack (1993) showed a lower time to union than transverse osteotomy. This is due to a 40% increased bony surface area that oblique osteotomy yields. Rayhack (1993) also reported that historically, the average healing time was 21 weeks, compared to the substantially shorter healing time of 11 weeks for oblique osteotomies.9 In our study, we could not statistically compare time to the union because there were few transverse osteotomies, which makes the analysis valueless. Our study also evaluated the difference in osteotomy technique, although we evaluated union or nonunion instead of healing time. Of the 94 participants, 85 had an oblique osteotomy, while nine had a transverse osteotomy. A substantial difference was found in the technique when looking at the union as the primary dependent outcome.
Clark and Geissler (2012) evaluated procedure-specific instruments in their study by utilizing Acumed’s ulnar shortening system in all their cases, which showed a 100% union rate when used by the designer.14 Follow-ups ranged from four to nine months, and no patients were known to have hardware problems or come in for hardware removal.17 Compared to Rayhack’s study, the average time to union reported by Clark and Geissler (2012) was only seven weeks, ranging from five to twelve weeks for all patients.14 Looking specifically at implant brands, Singhal (2020) designed a study that compared transverse osteotomies performed with a Synthes plate to oblique osteotomies performed with an Acumed plate. They found a significantly higher hardware removal rate of the transverse osteotomies than the oblique osteotomies. They also found that the oblique osteotomy with a procedure-specific plate had a shorter healing time, consistent with Rayhack’s, Clark’s, and Geissler’s findings.15 Our study also showed a higher union with oblique osteotomy.
Our results should be interpreted in light of the limitations. There was slight inconsistency in the follow-up times to calculate the time to union precisely. We included patients with a minimum follow-up of four months. However, the actual hardware removal might be underestimated because of the loss of follow-up. Another limitation of the present study is the disproportionate number of oblique versus transverse osteotomies (84 oblique versus 8 transverse), while most transverse osteotomies were freehand. This included three transverse osteotomies with conventional plating, three with a Skeletal Dynamic osteotomy-specific system, and two with a Synthes osteotomy-specific system. However, our study presents a diverse number of implant brands and several providers, which supports the generalizability of the study. We chose a wide range of providers to increase the generalizability of the study, and within our practice, only including one to two surgeons would not have included enough patients. Moreover, including one or two surgeons only may add surgeon bias, which might not be generalizable to the whole community.
Smokers were not excluded from our study, but we did not look at the relationship between smoking history and union rate because many patients did not have self-reported tobacco use answers.
Conclusion
Of the 92 patients, 83 (90%) had bone union. Still, with the advent of new devices and techniques, there is a 10% chance of nonunion, which is a high rate compared to the other bones. However, there is a low chance of a second surgery (3%) because most will remain asymptomatic and can be watched. Patients should be informed about the nonunion rate with possible subsequent secondary surgery. Using procedure-specific devices may have mitigated the risk of nonunion, although the risk is still noticeable.
Acknowledgment
Not applicable
Conflict of interest:
None
Funding:
None
References
- 1.Linscheid RL. Biomechanics of the distal radioulnar joint. 1992 ;(275) Clin Orthop Relat Res:46–55. [PubMed] [Google Scholar]
- 2.Moradi A, Binava R, Eslami Hasanabadi S, Vahedi E, Ebrahimzadeh MH. Introduction and Early Outcomes of Intraosseous Distal Radioulnar Joint Prosthesis: A Pilot Study and a Technique on a New Design of the Sauvé-Kapandji Procedure. Arch Bone Jt Surg. 2020;8(6):703–709. doi: 10.22038/abjs.2020.44520.2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Constantine KJ, Tomaino MM, Herndon JH, Sotereanos DG. Comparison of ulnar shortening osteotomy and the wafer resection procedure as treatment for ulnar impaction syndrome. J Hand Surg Am. 2000;25(1):55–60. doi: 10.1053/jhsu.2000.jhsu025a0055. [DOI] [PubMed] [Google Scholar]
- 4.Milch H. So-called dislocation of the lower end of the ulna. Ann Surg. 1942;116(2):282–292. doi: 10.1097/00000658-194208000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ebrahimzadeh MH, Moradi A, Vahedi E, Kachooei AR. Mid-term clinical outcome of radial shortening for kienbock disease. J Res Med Sci. 2015;20(2):146–149. [PMC free article] [PubMed] [Google Scholar]
- 6.Rodríguez-Merchán EC, Shojaie B, Kachooei AR. Distal Radioulnar Joint Instability: Diagnosis and Treatment. Arch Bone Jt Surg. 2022;10(1):3–16. doi: 10.22038/ABJS.2021.57194.2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sraj SA, Budoff JE. Ulnar or radial shortening osteotomy with a single saw cut. J Hand Surg Am. 2009;34(7):1248–1251. doi: 10.1016/j.jhsa.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Nagy L, Jungwirth-Weinberger A, Campbell D, Pino JG. The AO Ulnar Shortening Osteotomy System Indications and Surgical Technique. J Wrist Surg. 2014;3(2):91–97. doi: 10.1055/s-0034-1375965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rayhack JM, Gasser SI, Latta LL, Ouellette EA, Milne EL. Precision oblique osteotomy for shortening of the ulna. J Hand Surg Am. 1993;18(5):908–918. doi: 10.1016/0363-5023(93)90065-b. [DOI] [PubMed] [Google Scholar]
- 10.Lauder AJ, Luria S, Trumble TE. Oblique ulnar shortening osteotomy with a new plate and compression system. Tech Hand up Extrem Surg. 2007;11(1):66–73. doi: 10.1097/bth.0b013e3180336cc7. [DOI] [PubMed] [Google Scholar]
- 11.Baek GH, Chung MS, Lee YH, Gong HS, Lee S, Kim HH. Ulnar shortening osteotomy in idiopathic ulnar impaction syndrome. Surgical technique. J Bone Joint Surg Am. 2006;88 :212–220. doi: 10.2106/JBJS.F.00320. [DOI] [PubMed] [Google Scholar]
- 12.Ahsan ZS, Song Y, Yao J. Outcomes of ulnar shortening osteotomy fixed with a dynamic compression system. J Hand Surg Am. 2013;38(8):1520–1523. doi: 10.1016/j.jhsa.2013.04.040. [DOI] [PubMed] [Google Scholar]
- 13.Braun RM. A comparative study of ulnar shortening osteotomy by the freehand technique versus the Rayhack technique. J Hand Surg Am. 2006;31(8):1411–1412. doi: 10.1016/j.jhsa.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Clark SM, Geissler WB. Results of ulnar shortening osteotomy with a new plate compression system. Hand (N Y). 2012;7(3):281–285. doi: 10.1007/s11552-012-9417-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singhal R, Mehta N, Brown P, Cheung G, Brown DJ. A Study Comparing the Outcomes of Transverse Ulnar Shortening Osteotomy Fixed with a DCP to Oblique Osteotomy Fixed with a Procedure Specific Plate. J Hand Surg Asian Pac . 2020;25(4):441–446. doi: 10.1142/S2424835520500484. [DOI] [PubMed] [Google Scholar]
- 16.Jungwirth-Weinberger A, Borbas P, Schweizer A, Nagy L. Influence of Plate Size and Design upon Healing of Ulna-Shortening Osteotomies. J Wrist Surg. 2016;5(4):284–289. doi: 10.1055/s-0036-1582430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Owens J, Compton J, Day M, Glass N, Lawler E. Nonunion Rates among Ulnar-Shortening Osteotomy for Ulnar Impaction Syndrome: A Systematic Review. J Hand Surg Am. 2019;44(7):612.e1–612. doi: 10.1016/j.jhsa.2018.08.018. [DOI] [PubMed] [Google Scholar]