Abstract
The use of multisensory stimulation in people with dementia is becoming increasingly popular in the last decades. The aim of this review is to analyze the therapeutic effectiveness of multisensory stimulation in people with dementia. We made a search on Medline and Web of Science databases referred to all researches published from the year 1990 to 2012, which used multisensory stimulation techniques in people with dementia. The revision of the 18 articles which fulfilled the inclusion/exclusion criteria seems to prove evidence that multisensory stimulation environments produce immediate positive effects on the behavior and mood of people with dementia. Based on the above, we think it can be a useful nonpharmacological intervention on neuropsychological symptoms though, in any case, it would be necessary to start more reliable protocols from the methodological point of view in order to establish its long-term effectiveness.
Keywords: multisensory stimulation, snoezelen, multisensory environmental therapy, dementia, elderly
Introduction
Pharmacological treatments are not particularly effective in controlling behavioral and psychological symptoms (BPS) associated with dementia. 1,2 As a result, the last decades have experienced the development of different nonpharmacological techniques whose main objective has been to somehow contribute to improve the well-being and consequently, the quality of life of people with dementia.3–5
One of these novel techniques, snoezelen, is based on the multisensory stimulation. Snoezelen was developed in the Netherlands in the 1970s; this type of multisensory stimulation was first introduced to people with learning difficulties. 6 The term snoezelen is a contraction of 2 Dutch words, the equivalent in English being “sniffing and dozing.” 7 It is an activity taking place in a dusky, attractively lit room where soft music is heard. There is an emphatic appeal to the senses that are stimulated individually. 7 Snoezelen usually occurs in a room specifically designed for that purpose known as snoezelen room or multisensory stimulation room (MSSR). The MSSRs are typically dimly lit and include many objects pertaining to the 5 senses: fiber-optic cables, aroma therapy, different music/sounds, and water columns of different colors, textured balls to touch, and screen projectors among others. 8 As the term snoezelen is a registered trademark referred to multisensory stimulation, in our review we will use the term multisensory stimulation environment (MSSE) to avoid confusion.
Since the beginning of the 1990s, the MSSE has been used as a nonpharmacological therapy in people with dementia. 9 From a biopsychosocial model, it is considered that BPS symptoms can be explained not only by the disease itself but also by the physical and psychosocial environment of the patients. 10 –12 Elderly people with dementia, in particular those institutionalized, have sensory deprivation or on the contrary are exposed to an excessive sensory stimulation. Kovach 13 suggested the “sensoristasis” model, which states that older adults with dementia experience intrapsychic discomfort because of imbalances in the pacing of sensory-stimulating or sensory-calming activity. Consequences of this intrapsychic discomfort include agitated behaviors and episodic or premature decline in instrumental and social function. According to this model, interventions in people with dementia must facilitate optimum sensoristasis, that is, to achieve a balance between the sensory-stimulating and the sensory-calming activities. In this sense, MSSE constitutes an adequate intervention providing a stress-free, entertaining environment both to stimulate and to relax. 14 One of the distinguishing elements of MSSE as opposed to other therapies is the one-to-one attention and the adoption of a nondirective approach, encouraging patients to engage with sensory stimuli of their choice. 15 The MSSE would then be compatible with the person-centered care, which places particular emphasis to acknowledge the personhood of the patient with dementia, the personalization of the person’s care, and the shared decision making, prioritizing the relationship as much as the care tasks. 16,17
The MSSE aims to stimulate the primary senses through pleasurable sensory experiences arranged to stimulate the primary senses without the need for intellectual activity in an atmosphere of trust and relaxation. 6 Stimuli used are nonsequential and unpatterned, experienced moment by moment without relying on short-term memory to link them to previous events. 15 Since it does not appeal to cognitive abilities, it is one of the few approaches suitable for reaching persons with severe or very severe dementia whose possibilities for verbal communication are limited. 3
In the recent years, the use of MSSE in the field of dementia has experienced a rapid development. Nevertheless, the scientific efficiency of this type of intervention is still fairly limited. It has been observed that it can be an effective treatment in the reduction of some neuropsychiatric symptoms such as apathy or agitation, but generally speaking, results are modest and have no longer term effects. 5,18 –20
The main objective of this study was to make a methodical review of the most important studies published about multisensory stimulation referred to people with dementia as well as about the effectiveness of the intervention technique on the patient symptomatology.
Methods
A systematic search was performed in the Medline and Web of Science databases using key words “snoezelen,” “multisensory stimulation,” “multi-sensory stimulation,” “multisensory environments,” “sensory integration” combined with the terms “dementia,” or “Alzheimer” to identify any papers on the topic. Unpublished data and conference proceedings were not included in the current review. All English language publications from 1990 to 2012 about multisensory stimulation in people with dementia were reviewed. The inclusion criteria were that articles should be original and include patients of age ≥65 with dementia diagnosis, considering the chronological age of 65 years as a definition of elderly individuals. The data analysis process was made using a manual checking of the results obtained in the search. Duplicates or articles without a complete experimental protocol were excluded from the review.
Data extraction was performed using a standardized form to extract the following characteristics of each documented study: type of intervention (sample size, type of study group—experimental or control, type of multisensory stimulation-behavior therapy or stimulation room), dementia stage, treatment intensity of the experimental group (one-to-one or group sessions, and number and duration of sessions), evaluation method (immediate, pre-, post-, or follow-up effects), areas of intervention (behavior, mood, communication, cognition, functional status), main outcomes of the experimental group, and if the articles were indexed in Journal Citation Report (JCR).
Results and Discussion
Totally, 63 studies were found in the search, but only 18 fulfilled the inclusion/exclusion criteria. Of the 18, 16 were indexed in the JCR (Figure 1). The main characteristics of these studies are shown in Table 1. Most of the studies follow a one-to-one format treatment and took place in a specifically designed room (MSSR); 2 of them carried out group interventions. 22 , 23 Three studies 24 - 26 carried out an MSSE integrated in the daily care, that is, intervention was carried out during morning care (period of time between 7:00 am and 12:00 am), when the staff were engaged with residents in activities relating to bathing, grooming, dressing, and toileting. 25 Only 10 researches 8,15,21,23 –25,29,33,35,36 were conducted in patients randomly assigned to either a control or a study group. Besides, the other 2 included control group 27,32 but not randomly assigned.
Figure 1.
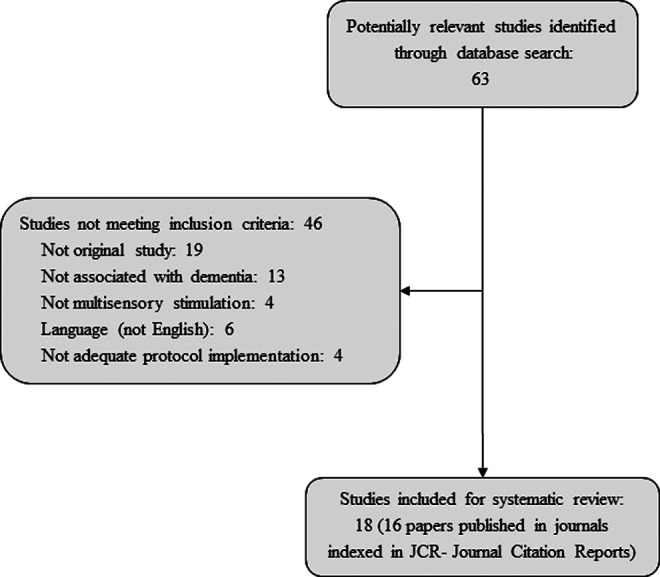
Flowchart of selection of studies for inclusion.
Table 1.
Characteristics of Included Studies.
| Refs | Intervention | Dementia stage | Treatment intensity (E) | Evaluation | Areas of intervention | Outcome | JCR |
|---|---|---|---|---|---|---|---|
| 8 | N = 18 | NA | One-to-one sessions | Pre, weeks 4 and 8, post and follow-up | Behavior | Significant differences with C | Yes |
| Randomized | 12 weeks | ||||||
| E1: MSSR 1 session/week | 30 min/session | ||||||
| E2: MSSR 3 sessions/week | |||||||
| C: usual care | |||||||
| 15,21 | N = 136 | NA | One-to-one sessions | Pre, mid, post and follow-up | Behavior | Limited short-term improvements for both groups. | Yes |
| Randomized | 4 weeks | Communication | |||||
| E: MSSR | Moderate to severe | 2 sessions/week | Immediate effects | Mood | No significant differences between E and C | ||
| C: activity sessions | 30 min/session | Cognition | |||||
| 22 | N = 27 | Mild | 4-5 people/session | Pre, post and follow-up | Mood: depression | Significant improvement | Yes |
| No randomized | 3 weeks | ||||||
| Multisensory stimulation | 4 sessions/week | Cognition | |||||
| No C | |||||||
| 23 | N = 40 | NA | Group sessions | Pre and post | Behavior | No significant effect | No |
| Randomized | 10 weeks | ||||||
| E: sensory integration | 3 sessions/week | Functional status: ADL | |||||
| C: usual leisure activities | 30-45 min/session | ||||||
| 24 | N = 125 | Moderate to severe | 15 months | Pre and post | Behavior | ↓ loss of decorum, apathetic, rebellious and aggressive behavior | Yes |
| Randomized | ↓ depression, ↑ well-being | ||||||
| E: MSSE integrated in daily care | 1 session daily | Mood | ↑ responding to speaking, relating to caregiver, normal-length sentences | ||||
| C: usual care | Communication | ||||||
| 25 | N = 117 | Moderate to severe | 15 months | Pre and post | Communication | ↑ smiling, duration of eye contact and verbal expressed autonomy | Yes |
| Randomized | |||||||
| E: MSSE integrated in daily care | 1 session daily | ↓ negative verbal behaviors | |||||
| C: usual care | |||||||
| 26 | N = 6 | Moderate to severe | 16 weeks | Pre and post | Behavior | No significant effect | Yes |
| No randomized | |||||||
| Motor and multisensory stimulation integrated in daily care | 1 session daily | Communication | |||||
| No C | |||||||
| 27 | N = 24 | NA | One-to-one sessions | Post Immediate effects | Mood | All three environments improved mood. No evidence that any was better than other | Yes |
| No randomized | |||||||
| E1: MSSR | 3 sessions of each activity | ||||||
| E2: garden | 16 min/session | ||||||
| C: normal living environment | |||||||
| 28 | N = 4 | Moderate to severe | One-to-one sessions 4 weeks | Immediate effects | Behavior | Positive effect (no statistical reported) | No |
| No Randomized | |||||||
| MSSR | 2 sessions/week | Mood | |||||
| No C | |||||||
| 29 | N = 20 | NA | One-to-one sessions | Immediate effects | Behavior | Significant improvement in both groups. No significant differences between E and C | Yes |
| Randomized | 2 weeks | ||||||
| E: MSSR | 3 sessions | Mood | |||||
| C: reminiscence | 40 min/session | ||||||
| 30 | N = 20 | NA | One-to-one sessions | Immediate effects | Behavior | Positive effect (no statistics reported) | Yes |
| No randomized | 1 year | ||||||
| MSSR | 30 min/session | ||||||
| No C | |||||||
| 31 | N = 29 | NA | One-to-one sessions | Immediate effects | Behavior | Positive effect (no statistics reported) | Yes |
| No randomized | 1-4 sessions | Mood | |||||
| MSSR | 20-30 min/session | Communication | |||||
| No C | |||||||
| 32 | N = 14 | NA | One-to-one sessions | Initial month and 3 months later | Behavior | Positive effect (no statistics reported) | Yes |
| No randomized | |||||||
| E: MSSR | Sporadic use | ||||||
| C: usual care | 15-20 min/session | ||||||
| 33 | N = 24 | Moderate to severe | One-to-one sessions | Pre and 6 post sessions | Behavior | Significant improvement compared with C | Yes |
| Randomized | |||||||
| E: MSBT | 6 sessions | Functional status: ADL | |||||
| C: recreational activity | 25-30 min/session | ||||||
| 34 | N = 10 | NA | 3 weeks | Pre and post | Behavior | Positive effect (no statistics reported) | Yes |
| No randomized | 1-2 times/d | ||||||
| MSSR (at home) | 15-45 min/session | Immediate effects | Communication | ||||
| No C | |||||||
| 35 | N = 30 | Moderate to severe | One-to-one sessions | Immediate effects | Functional status | Significant improvement in both groups. Participants in E improved significantly in motor skills for more sessions | Yes |
| Randomized | |||||||
| E: MSSR | 4 weeks | ||||||
| C: garden | 3 sessions/week | ||||||
| 36 | N = 19 | NA | One-to-one sessions | Pre, mid, and post | Functional status: balance | No significant effect | Yes |
| Randomized | 6 weeks | ||||||
| E: MSSR | 2 sessions/week | ||||||
| C: volunteer visits | 30 min/session |
Abbreviations: ADL, activities of daily living; C, control group; E, experimental group; MSBT, multisensory behavior therapy; MSSE, multisensory stimulation environment; MSSR, multisensory stimulation room; NA, not available data; JCR, Journal Citation Reports.
Sample size ranged between 4 and 136 patients. 21,28 Two studies 15,21 are presented simultaneously because both used the same study population but increased the sample size from 50 to 136 patients. 15,21 The intervention varied from 3 MSSE sessions 27 , 29 to a daily session for a period of 15 months. 24,25 The time for each session ranged from 16 to 45 minutes (approximately average of 30 minutes), although we must take into account that some studies 22,24 –26,28,35 did not include this information.
Effect on the Behavior
Intervention in MSSRs has reported positive effects on the behavior of patients with dementia during and after the sessions.28–31 There were short-term positive improvements in the behavior,28–30 but long-term benefits and the generalization of the results to other environments are more questinonable. 21 , 28
In some of the studies we have analyzed, 8,32,33 the MSSE results have been better than those in the control conditions. Milev et al 8 found a significant improvement in the behavior of patients with dementia who received 1 or 3 sessions a week in an MSSR compared to the control group who received normal care with the Daily Observation scale (DOS to supply information on the actual behavior of the patient) assessment tool in week 8, and the Clinical Global Impression–Improvement (CGI-I; to assess the overall severity of an individual’s symptoms as well as changes in his or her functioning over time) in week 12. This effect lasted even 12 weeks after finishing the treatment. In another research, 32 the patients with Alzheimer’s disease who received sporadic stimulation in MSSR showed a decrease in the number of disruptive behaviors compared to those patients in the control group who continued with the normal care. Furthermore, the combination of the standard psychiatric inpatient care and the multisensory behavior therapy (MSBT), 33 an integration of the MSSE and the conductivism, showed a significant decrease in agitation (P = .003) and apathy (P = .04) compared to patients in the control group who also carried out one-to-one leisure activities (ie, manipulative-bead mazes, sorting puzzles, and tactile tasks touch).
Other studies, however, did not find significant differences between the MSSE effects and the control conditions. Baker et al 21 compared the intervention in an MSSR with a control group receiving one-to-one activity sessions that required intellectual or physical skills (play cards, look at photographs, or do quizzes), and no differences were found between the groups. The same occurred in another study that compared the intervention in an MSSR with a traditional intervention with more cognitive demand, such as the reminiscence therapy, 29 in which no significant differences in the patients’ agitated behavior were found either. Likewise, another research based on a sensory integration program in which the multisensory stimulation was part of a group intervention, together with reality orientation and cognitive stimulation, 23 did not show significant differences in the patients’ behavior in comparison to the control group who participated in the usual leisure activities.
With the MSSE integrated in the daily care, van Weert et al 24 found a significant improvement in different aspects after 15 months of treatment, such as their level of apathetic behavior, loss of decorum, rebellious, and aggressive behavior compared to the control group who received the usual care. Cruz et al, 26 in a later study lasting 16 weeks and consisting of a motor and multisensory stimulation integrated in the daily care, found a tendency to increase the residents’ engagement in morning care routines, but the results were not significant.
Effect on Mood
The intervention in MSSRs has demonstrated to improve the mood of people with dementia during the sessions and at short term 27 –29,31 but long-term effects were not evident. 28
In those studies that compared the effect of one-to-one intervention in an MSSR with a control group which also received one-to-one attention, 21,27,29 no significant differences in the mood were found between the experimental and the control group, and the reason could be that what really improved the patient’s mood was the one-to-one interaction with the staff. 27 However, Ozdemir et al 22 in a multisensory stimulation program carried out in groups of 4 or 5 people based on the combination of musical therapy, painting, and sensory stimulation observed a significant improvement (P = .001) in the levels of depression assessed with the Geriatric Depression scale (GDS) in mildly affected patients with Alzheimer’s disease. Furthermore, this effect lasted for 3 weeks following completion of the study. Nevertheless, precautions must be taken with the results of this study as it lacks control group.
The MSSE integrated in the daily care 24 suggested a generalizing effect on the mood and well-being of people with dementia. Patients receiving the intervention demonstrated a significant improvement in their level of depression (P < .05) in comparison to the control group who received the usual care. Likewise, they showed a higher degree of happiness and enjoyment, a better mood, and less sadness than patients in the control group.
Effect on Cognitive Level
The effects of multisensory stimulation on the cognitive status of elderly people with dementia have been hardly studied. In people with moderate to severe dementia, Baker et al 21 did not find significant differences between the intervention in an MSSR and the control group receiving activity sessions that required intellectual or physical skills, neither in short term nor in long term. In the case of mildly affected patients with Alzheimer’s disease, the cognitive status assessed with Mini-Mental State Examination (MMSE) showed a significant improvement (P = .001) after a group multisensory intervention, which effect lasted for 3 weeks following the completion of the study. 22 Considering these results, an early multisensory stimulation treatment in the first stages of dementia may be useful in the intervention on the cognitive decline of these patients.
Effect on Communication/ Interaction
The effectiveness of MSSRs intervention in the communication and social interaction of people with dementia is still not clear. Hope 31 found that intervention in an MSSR offered the potential to increase meaningful communication as well as a higher communication spontaneity and level of eye contact. Also, in a qualitative study in which an MSSR was installed in the home of people with dementia, 34 the family caregivers reported an improvement in the family interactions and described themselves as feeling more connected with their loved ones while interacting with them in the MSSR. However, Baker et al 21 in a randomized controlled trial did not find significant differences in the communication and interaction between the group participating in an MSSR and the control group receiving one-to-one activity sessions that required intellectual or physical skills.
van Weert et al 24,25 suggested that the MSSE integrated in the daily care could be an adequate approach to improve the communicative environment in the nursing homes of elderly patients. These authors found significant improvements in the verbal and nonverbal communication with caregivers in comparison to the control group who received the usual care. During the morning care, patients of the experimental group showed an increase in the duration of eye contact and in the number of smiles, a decrease in verbal disapproval and anger, and an increase in taking autonomy (giving opinion, making a choice). Furthermore, they had a better interaction with caregivers, a better approach for communication, and used normal length sentences more often than patients of the control group. Cruz et al 26 found that a motor and multisensory stimulation integrated in the daily care resulted in an increase in residents’ levels of caregiver-direct gaze, laughing, and engagement and a reduction of closed eyes. Nevertheless, these results were not statistically significant comparing the results before and after the intervention.
Effect on Functional Status
Staal et al 33 observed that hospitalized patients with moderate to severe dementia who received multisensory behavior therapy achieved greater independence in activities of daily living (ADLs) assessed with the Katz index in comparison to patients in the control group who carried out one-to-one leisure activities.
Effect on the functional status was also observed by Collier et al 35 when compared to the effect of an intervention in an MSSR with a control group doing gardening and assessed with the Assessment of Motor and Process Skills (AMPS). Despite the fact that both groups showed significant improvements in functional performance, participants in the MSSR group improved significantly in motor skills for more sessions than in the control group (P = .03).
Nevertheless, on the contrary, other study found that in a 6-week intervention period in a MSSR, 36 there were no significant changes in balance or reduction in falls’ rate frequency. There were no significant differences in the control group participants who received one-to-one visits by volunteers.
Methodology, Limitations, and Implications for Future Research
Notwithstanding the fact this review has included all papers published up to date according to the inclusion criteria, we find that, in general, they present lots of methodological limitations. In some cases, the number of intervention sessions was very limited 27,29,31 or the sample size was very small to establish the benefits at different stages of dementia; in other cases the lack of control group 22,26,28,30,31,34 (even when included comparisons of results on pre- and post- interventions in a single group) or the assignment of patients to the different groups was not randomly made. 27,32 Besides, some studies did not apply statistically significant tests or used qualitative methodology. 28,30,31,32,34
For all the above, we understand we face a new intervention field with very good prospects where more strict methodological studies should be developed, with larger samples and with comparable control groups. Also, blinded evaluation (regarding assignment of participants to the control/intervention groups) must be assured to avoid biases. Likewise, it would be positive that the research includes assessment of biomedical parameters such as blood pressure or heart rhythm, indicators of stress situations.
Due to the limited number of studies that examine the long-term effects, 8,15,21,22 future research must have a length sufficient enough to study the maintenance of the MSSE benefits throughout a long period of time and the generalization of the results to other contexts such as the ward and/or at home.
It is necessary to study the MSSE effects on people in different stages of dementia. There are very few studies on patients in the first stages of dementia which clarify whether the MSSE can positively affect the disease prognosis. More studies are also needed focusing on the people in advanced stages of dementia which help to clarify the role of the MSSE in those patients who are unable to participate in more cognitively demanding activities. 21
On the other hand, new research lines should be developed allowing to examine the similarities and differences between the MSSE carried out in MSSRs and the MSSE integrated in the daily care and to compare their effects. 37
It would also be interesting to assess the combined and separated impact of the MSSE and the pharmacotherapy (eg, antipsychotics) in people with dementia. 19
Furthermore, the literature about the clinical intervention in the MSSE sessions in people with dementia is still rare 38 ; hence, more research is needed to provide information about the assessment process (ie, in-session sensory preference assessment or sensory profile of the patient) and the intervention techniques used during the MSSE sessions.
Conclusions
The MSSRs seem to provide evidence of immediate positive effects on the behavior and mood of people with dementia. However, there are no conclusive data about their long-term effectiveness or about the generalization of results to other environments. The evidence of the MSSE effects on the cognitive status, the communication and social interaction, and the functional state is still limited.
Studies with more methodological quality are needed to clarify the long-term effectiveness of MSSE on patients in different stages of dementia. In any case, the MSSE opens a new nonpharmacological intervention field for people with dementia, which, no doubt, can yield results in an immediate future once the procedures for intervention have been more scientifically established.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Sink KM, Holden KF, Yaffe K. Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. JAMA. 2005;293(5):596–608. [DOI] [PubMed] [Google Scholar]
- 2. Poop J, Arlt S. Pharmacological treatment of dementia and mild cognitive impairment due to Alzheimer's disease. Curr Opin Psychiatry. 2011;24(6):556–561. [DOI] [PubMed] [Google Scholar]
- 3. Finnema E, Dröes RM, Ribbe M, Van Tilburg W. The effects of emotion-oriented approaches in the care for persons suffering from dementia: a review of the literature. Int J Geriatr Psychiatry. 2000;15(2):141–161. [DOI] [PubMed] [Google Scholar]
- 4. Vernooij-Dassen M, Vasse E, Zuidema S, Cohen-Mansfield J, Moyle W. Psychosocial interventions for dementia patients in long-term care. Int Psychogeriatr. 2010;22(7):1121–1128. [DOI] [PubMed] [Google Scholar]
- 5. Verkaik R, van Weert JC, Francke AL. The effects of psychosocial methods on depressed, aggressive and apathetic behaviors of people with dementia: a systematic review. Int J Geriatr Psychiatry. 2005;20(4):301–314. [DOI] [PubMed] [Google Scholar]
- 6. Burns I, Cox H, Plant H. Leisure or therapeutics? Snoezelen and the care of older persons with dementia. Int J Nurs Pract. 2000;6(3):118–126. [DOI] [PubMed] [Google Scholar]
- 7. Hulsegge J, Verheul A. Snoezelen: Another World. Chesterfield, UK: Rompa; 2005. [Google Scholar]
- 8. Milev RV, Kellar T, McLean M, et al. Multisensory stimulation for elderly with dementia: a 24-week single-blind randomized controlled pilot study. Am J Alzheimers Dis Other Demen. 2008;23(4):372–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moffat N, Barker P, Pinkney L. Snoezelen: An Experience for People with Dementia. Chesterfield, UK: Rompa; 1993. [Google Scholar]
- 10. Eriksson S. Impact of the environment on behavioral and psychological symptoms of dementia. Int Psychogeriatr. 2000;12(1):89–91. [Google Scholar]
- 11. Zuidema SU, de Jonghe JF, Verhey FR, Koopmans RT. Environmental correlates of neuropsychiatric symptoms in nursing home patients with dementia. Int J Geriatr Psychiatry. 2010;25(1):14–22. [DOI] [PubMed] [Google Scholar]
- 12. Kovach CR, Magliocco JS. Late-stage dementia and participation in therapeutic activities. Appl Nurs Res. 1998;11(4):167–173. [DOI] [PubMed] [Google Scholar]
- 13. Kovach CR. Sensoristasis and imbalance in persons with dementia. J Nurs Scholarsh. 2000;32(4):379–384. [DOI] [PubMed] [Google Scholar]
- 14. Chitsey AM, Haight BK, Jones MM. Snoezelen: a multisensory environmental intervention. J Gerontol Nurs. 2002;28(3):41–49. [DOI] [PubMed] [Google Scholar]
- 15. Baker R, Bell S, Baker E, et al. A randomized controlled trial of the effects of multi-sensory stimulation (MSS) for people with dementia. Br J Clin Psychol. 2001;40(pt 1):81–96. [DOI] [PubMed] [Google Scholar]
- 16. Edvardsson D, Winblad B, Sandman PO. Person-centred care of people with severe Alzheimer's disease: current status and ways forward. Lancet Neurol. 2008;7(4):362–367. [DOI] [PubMed] [Google Scholar]
- 17. Buron B. Levels of personhood: a model for dementia care. Geriatr Nurs. 2008;29(5):324–332. [DOI] [PubMed] [Google Scholar]
- 18. Livingston G, Johnston K, Katona C, Paton J, Lyketsos CG; and Old Age Task Force of the World Federation of Biological Psychiatry. Systematic review of psychological approaches to the management of neuropsychiatric symptoms of dementia. Am J Psychiatry. 2005;162(11):1996–2021. [DOI] [PubMed] [Google Scholar]
- 19. Lancioni GE, Cuvo AJ, O'Reilly MF. Snoezelen: an overview of research with people with developmental disabilities and dementia. Disabil Rehabil. 2002;10;24(4):175–184. [DOI] [PubMed] [Google Scholar]
- 20. Padilla R. Effectiveness of environment-based interventions for people with Alzheimer's disease and related dementias. Am J Occup Ther. 2011;65(5):514–522. [DOI] [PubMed] [Google Scholar]
- 21. Baker R, Holloway J, Holtkamp CC, et al. Effects of multi-sensory stimulation for people with dementia. J Adv Nurs. 2003;43(5):465–477. [DOI] [PubMed] [Google Scholar]
- 22. Ozdemir L, Akdemir N. Effects of multisensory stimulation on cognition, depression and anxiety levels of mildly-affected Alzheimer's patients. J Neurol Sci. 2009;283(1-2):211–213. [DOI] [PubMed] [Google Scholar]
- 23. Robichaud L, Hébert R, Desrosiers J. Efficacy of a sensory integration program on behaviors of inpatients with dementia. Am J Occup Ther. 1994;48(4):355–360. [DOI] [PubMed] [Google Scholar]
- 24. van Weert JC, van Dulmen AM, Spreeuwenberg PM, Ribbe MW, Bensing JM. Behavioral and mood effects of snoezelen integrated into 24-hour dementia care. J Am Geriatr Soc. 2005;53(1):24–33. [DOI] [PubMed] [Google Scholar]
- 25. van Weert JC, van Dulmen AM, Spreeuwenberg PM, Ribbe MW, Bensing JM. Effects of snoezelen, integrated in 24 h dementia care, on nurse-patient communication during morning care. Patient Educ Couns. 2005;58(3):312–326. [DOI] [PubMed] [Google Scholar]
- 26. Cruz J, Marques A, Barbosa AL, Figueiredo D, Sousa L. Effects of a motor and multisensory-based approach on residents with moderate-to-severe dementia. Am J Alzheimers Dis Other Demen. 2011;26(4):282–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cox H, Burns I, Savage S. Multisensory environments for leisure: promoting well-being in nursing home residents with dementia. J Gerontol Nurs. 2004;30(2):37–45. [DOI] [PubMed] [Google Scholar]
- 28. Cornell A. Evaluating the effectiveness of Snoezelen on women who have a dementing illness. Int J Psychiatr Nurs Res. 2004;9(2):1045–1062. [PubMed] [Google Scholar]
- 29. Baillon S, Van Diepen E, Prettyman R, Redman J, Rooke N, Campbell R. A comparison of the effects of Snoezelen and reminiscence therapy on the agitated behaviour of patients with dementia. Int J Geriatr Psychiatry. 2004;19(11):1047–1052. [DOI] [PubMed] [Google Scholar]
- 30. Minner D, Hoffstetter P, Casey L, Jones D. Snoezelen activity: the good shepherd nursing home experience. J Nurs Care Qual. 2004;19(4):343–348. [DOI] [PubMed] [Google Scholar]
- 31. Hope KW. The effects of multisensory environments on older people with dementia. J Psychiatr Ment Health Nurs. 1998;5(5):377–385. [DOI] [PubMed] [Google Scholar]
- 32. Ward-Smith P, Llanque SM, Curran D. The effect of multisensory stimulation on persons residing in an extended care facility. Am J Alzheimers Dis Other Demen. 2009;24(6):450–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Staal JA, Sacks A, Matheis R, et al. The effects of Snoezelen (multi-sensory behavior therapy) and psychiatric care on agitation, apathy, and activities of daily living in dementia patients on a short term geriatric psychiatric inpatient unit. Int J Psychiatry Med. 2007;37(4):357–370. [DOI] [PubMed] [Google Scholar]
- 34. Riley-Doucet CK. Use of multisensory environments in the home for people with dementia. J Gerontol Nurs. 2009;35(5):42–52. [DOI] [PubMed] [Google Scholar]
- 35. Collier L, McPherson K, Ellis-Hill C, Staal J, Bucks R. Multisensory stimulation to improve functional performance in moderate to severe dementia--interim results. Am J Alzheimers Dis Other Demen. 2010;25(8):698–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Klages K, Zecevic A, Orange JB, Hobson S. Potential of Snoezelen room multisensory stimulation to improve balance in individuals with dementia: a feasibility randomized controlled trial. Clin Rehabil. 2011;25(7):607–616. [DOI] [PubMed] [Google Scholar]
- 37. Chung JCC, Lai CKY. Snoezelen for dementia. Cochrane Database Syst Rev. 2009;(4):CD003152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Staal JA. Functional analytic multisensory environmental therapy for people with dementia. Int J Alzheimers Dis. 2012;2012:294801. [DOI] [PMC free article] [PubMed] [Google Scholar]


