Abstract
AIM:
The aim of the study was to determine whether ocular movement can affect the shape of the globe and lead to measurable change in axial and peripheral eye length.
METHODS:
Ten subjects aged 18–30 years (6 M/4 F) participated with informed consent. The mean spherical equivalent refractive error was ≤−1.00 DS with cylindrical refraction <−1.25 DC. One drop of tropicamide hydrochloride 1% was instilled 20 min before measurement to induce mydriasis and mild cycloplegia. Using IOLMaster, eye length was measured centrally and temporally (25° off-axis) in four different positions. Subjects then rotated their eyes 25° in the temporal direction to fixate on a target for 10 min. After that, the same measurements were repeated.
RESULTS:
Before rotation, the group mean peripheral eye length was significantly shorter than the central eye length (P < 0.05). There was no significant variation in central or peripheral eye length due to off-axis fixation, either after the initial eye rotation or after fixation for 10 min at the off-axis point. The difference between central and peripheral eye lengths was maintained after 10 min of temporal fixation (P < 0.05).
CONCLUSION:
Peripheral eye length was shorter than central eye length showing the prolate shape associated with myopia. The action of the extraocular muscles on the globe has no significant effect upon the retinal shape assessed by off-axis eye length measurement in myopic subjects.
Keywords: Central eye length, eye rotation, eye shape, IOLMaster, myopia, peripheral eye length
Introduction
Previous work suggests that peripheral blur signals can influence eye growth, and peripheral blur is the result of a mismatch between the retinal profile and peripheral optical characteristics of the eye.[1,2,3,4,5,6] Animal models have shown that defocus in local retinal areas can lead to eye growth in that area only.[7,8,9,10,11,12]
Studies have shown that subjects with axial myopia tend to have relative peripheral hyperopia, whereas hyperopic subjects have relative peripheral myopia.[3,4,13] The presence of relative peripheral hyperopia is thought to drive ocular growth leading to increased axial length (AL) and myopia.[4,5,6,14] The possible link between myopia development and peripheral hyperopia has directed interest toward investigating peripheral refraction and peripheral length (PL) (corneoretinal length along an axis perpendicular to the retinal surface).
A number of studies have been conducted to assess the relationship between peripheral refraction and ocular rotation[2,4,13,15,16] by either keeping the eye stationary and rotating the instrument or by rotating the eye while keeping the instrument stationary. However, there are very limited data available on the relationship between PL and ocular rotation.
MacFadden et al. conducted the first study to determine the effect of eye rotation upon the measurement of PL on 23 healthy subjects (13 myopes and 10 hyperopes) using the IOLMaster (Carl Zeiss Meditec, Germany) mounted on a rotating platform. The age of the subjects ranged between 17 and 25 years, and the mean spherical equivalent (MSE) for the myopic group was −5.08D ±2.49D and for the hyperopic group was +4.77D ±1.97D. They measured eye length centrally, temporally, and nasally across the horizontal meridian up to 40° under two different experimental paradigms: first, with IOLMaster maintained stationary in a straight position while the subject rotated their eye to fixate off-axis, and second, where the subject maintained eye position straight ahead while the IOLMaster was rotated around the eye. Ocular rotation significantly altered the peripheral retinal profile in myopic subjects (P < 0.05) but had no effect on hyperopic subjects.[17]
Ehsaei et al. measured AL and PL up to 30° temporally and nasally for 27 emmetropic subjects (MSE =0.10 ± 0.31D; mean age =21.67 ± 3.23 years) and 52 myopic subjects (MSE = −5.29 ± 1.86D; mean age =22.37 ± 3.77 years) using a noncontact optical biometer (IOLMaster, Carl Zeiss Meditec, Germany). They found that the mean central AL for the emmetropic group was 23.55 ± 0.48 mm compared to 23.12 ± 0.47 mm (30° temporally) and 23.22 ± 0.49 mm (30° nasally). For the myopic group, the mean central AL was 25.45 ± 1.10 mm compared to 24.49 ± 1.00 mm (30° temporally) and 24.73 ± 1.11 mm (30° nasally), showing that in the myopic group, the length of the eye was significantly shorter in the periphery (P < 0.05).[18]
The aim of this study is to determine whether sustained ocular movement generated by the extraocular muscles affects the shape of the eye causing a change in peripheral eye length in young healthy subjects with axial myopic refractive error.
Methods
Subjects
Ten healthy myopic adults (six males and four females) were recruited from a university population. The age of the participants ranged between 18 and 28 years (mean ± standard deviation [SD] =21.6 ± 2.98 years). The refractive error ranged between −2.00D and −4.50D (mean ± SD = −2.92 ± 0.77 DS). Subjects were excluded who had any history of ocular or systemic disease, ocular surgery, or had astigmatism <−1.25DC. All participants had best-corrected visual acuity of 6 / 6 or better in both eyes. One drop of tropicamide hydrochloride 1% was installed in the right eye, before measurement, to induce mydriasis. A further drop was installed 20 min later if mydriasis was inadequate. The left eye was occluded during the experiment.
The experiment was approved by the School of Health and Life Sciences Ethics Committee at Glasgow Caledonian University and was conducted in accordance with the Declaration of Helsinki for research involving human subjects. All participants completed a consent form after having verbal explanation about the nature of the study and any possible consequences.
Instrumentation
All measurements were obtained using IOLMaster ocular biometer (Carl Zeiss Meditec, Germany) aligned with the center of the pupil. This instrument has been found to be accurate and reliable to measure the distance between the cornea and the retina.[19,20] To meet the requirements of our experiment, the instrument was especially mounted on a rotating platform with an angular scale to allow it to rotate accurately around the eye.
Fixation targets
The central fixation target was the internal fixation light of the instrument, whereas the horizontal fixation targets were a number of small LED lights attached to the front of the instrument. The distance between the targets produced eye rotation of 25° temporally along the horizontal meridian.
Experimental procedure
Eight measurements were collected from each participant at four different fixation positions (taking five readings of eye length at each position). At the beginning of the experiment, eye length measurements were taken for each fixation position as baseline measurements. The subjects were then asked to fixate on the temporal target 25° from the center for 10 min.
All the measurements were taken from the right eye, while the left eye was occluded. Furthermore, none of the participants wore any form of optical correction during the procedure. The LED targets are clearly visible and close to the subject, so even if they were not completely clear, subjects were instructed to fixate at the center of the light to ensure steady fixation.
The subject's head was kept stationary all the times by the head and chinrest, and subjects were asked to view each target by turning their eyes only. The time required to complete one set of measurements was approximately 1 min, with a further minute required for adjusting the position of the eye. The average of five readings was calculated for each position at all measurement points [Figure 1a-d].
Figure 1.

The infrared beam entering the right eye at 0˚ to measure the central AL (a), how both the eye and the instrument were rotated 25˚ temporally to measure the central AL again (b), eye rotation 25˚ temporally with the infrared beam entering the right eye at 0˚ to measure the PL (c), and how the instrument was rotated 25˚ nasally in order to measure the PL again (d), It can be seen that both beams entered the eye through the central curvature of the cornea and passed close to the nodal point
Eye length was measured centrally along the visual axis and at 25° horizontally in the temporal retina. These measurements were repeated with the eye in four different positions as follows:
Baseline measurements were obtained in the central and peripheral locations with the subject fixating upon the central target with no eye rotation
The subject then rotated their eye to fixate on the peripheral target placed at 25° temporally and the measurements were repeated, rotating the IOLMaster as necessary to obtain the measurements
The subject was then asked to maintain fixation on the peripheral target with the eye rotated for 10 min. Measurements were repeated while the subject continued fixating on the peripheral target
Finally, the subject then returned to fixate on the central target and measurements of central and peripheral eye lengths were repeated at this position.
Data analysis
SPSS software version 22 for Windows (SPSS Inc., Chicago, IL, USA) was used to perform statistical analysis for our data (www.ibm.com/software/analytics/spss/).
A Shapiro–Wilk test was performed to determine the normality which showed that the data were normally distributed. A two-way repeated measures ANOVA was used to analyze the data, with time as the repeated measure and retinal location as a factor. Results were considered statistically significant if P < 0.05.
Results
Before subjects were asked to rotate the eye, the central AL varied from 24.10 to 26.20 mm (mean ± SD =25.06 ± 0.61 mm) and temporal PL varied from 23.49 mm to 25.43 mm (mean ± SD =24.31 ± 0.64 mm), with all subjects having shorter eye length in the peripheral retina [Table 1].
Table 1.
Summary of the means for central and peripheral eye lengths in all positions before and after temporal fixation
| Position | Before temporal fixation |
After temporal fixation |
||||
|---|---|---|---|---|---|---|
| No rotation (mean±SD) | Rotation (mean±SD) | P | No rotation (mean±SD) | Rotation (mean±SD) | P | |
| Central (mm) | 24.91±0.74 | 24.92±0.75 | >0.05 | 24.91±0.74 | 24.90±0.75 | >0.05 |
| Temporal (mm) | 24.22±0.68 | 24.19±0.67 | >0.05 | 24.21±0.66 | 24.19±0.63 | >0.05 |
| AL versus PL | <0.05 | <0.05 | ||||
Values show mean±SD. SD: Standard deviation, AL: Axial length, PL: Peripheral length
A two-way repeated measures ANOVA shows no significant variation in the eye length over time (F=1.368; df=3.27; P=0.274). There is a significant difference between the group mean central and peripheral eye lengths at all time points (F = 38.530; df =1.9; P < 0.0001) with central eye length being longer than peripheral. There was no significant interaction between the factors of time and retinal location (F = 0.955; df =3.27; P = 0.428).
At the beginning of the experiment, the baseline central AL was significantly longer than baseline temporal PL [P < 0.05; Figure 2].
Figure 2.

The relationship between central and peripheral eye lengths with no eye rotation and no temporal fixation at the beginning of the experiment. AL: Axial length, PL: Peripheral length
As expected, there was a significant negative relationship between central MSE and AL, where central AL increased with increasing myopia [Figure 3].
Figure 3.

The significant relationship between refractive error (mean spherical equivalent) and central axial length. AL: Axial length, MSE: Mean spherical equivalent
The difference between central AL (group mean =24.91 ± 0.74 mm) and temporal PL (group mean =24.21 ± 0.66 mm) remained significant after 10 min of continuous fixation at 25° temporal to the visual axis [P < 0.05; Figure 4].
Figure 4.

The relationship between central and peripheral eye lengths after temporal fixation with the eye in the straight-ahead position. AL: Axial length, PL: Peripheral length
The effect of eye rotation upon central AL was very small even with 10 min of off-axis fixation, as shown in Figure 5.
Figure 5.

The difference between rotated and nonrotated measurements of central axial length (AL) before and after 10 min of off-axis fixation against the baseline measurement of AL. AL: Axial length
Eye rotation caused small changes in temporal PL, even after 10 min of off-axis fixation, although some intersubject variability is apparent [Figure 6].
Figure 6.
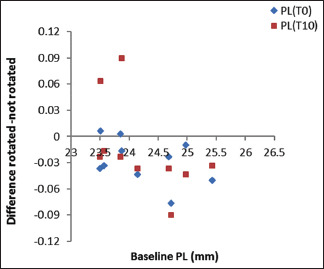
The difference between rotated and nonrotated measurements of peripheral length (PL) before and after 10 min of off-axis fixation against the baseline measurement of PL. PL: Peripheral length
Discussion
The results of the current study show little effect of eye rotation upon eye length in either the central or peripheral retinal locations, even after 10 min of continuous off-axis fixation. The range of the myopic subject group in the present study was −2.00D to −4.50D, and this may limit the effect of eye rotation upon retinal profile. This study is one of the first to examine the effect of prolonged eye rotation upon eye length, and while there was considerable intersubject variability, some subjects showed substantial changes which suggest that the action upon the sclera by the extraocular muscles may be affecting the length of the eye.
Previous studies on the effect of ocular rotation upon peripheral eye length measurement are limited. These studies investigated peripheral retinal profile either by keeping the eye in a fixed position and rotating the instrument or by keeping the instrument in a fixed position and rotating the eye. The results showed that peripheral retinal profile could be affected by ocular rotation, particularly in subjects with high myopia, such that eye rotation leads to increases in PL and hence an increase in relative peripheral myopia for these subjects.[4,17]
The aim of the present study was to investigate whether the force generated by the extraocular muscles during eye rotation could affect the measurement of eye length in myopic subjects. Examination of the individual changes suggests that certain subjects show increased PL as a result of eye rotation. Previous findings in our laboratory have shown that ocular rotation could increase PL and that the effect was noticeable with eye rotation ≥30° temporally and in subjects with myopia of more than −5.00D.[17]
They also found that while ocular rotation altered peripheral retinal shape in myopic subjects, hyperopic subjects showed no significant change. The MSE of the myopic subject group ranged from −2.00D to −9.13D, which is more myopia than in the current study, and they also measured further into the periphery (up to ~40°). This suggests that repeating the current experiment may be worthwhile in subjects with greater degrees of myopia.
Atchison and Charman investigated peripheral retinal shape using partial coherence interferometry, with three different schematic eyes (myopic, emmetropic, and accommodating). Their results indicated that, apart from the type of schematic eye, the peripheral eye length measurement was not affected up to 30° of lateral rotation. According to their model, measuring a peripheral point beyond 30° will cause the measurement beam to be directed away from the nodal point increasing the apparent path length and leading to a value of peripheral eye length which is larger than the true value.[21]
There are measurement errors which may affect the measurement of off-axis eye length using IOLMaster due to accommodation changes and variations in the crystalline lens thickness, where the instrument uses the average refractive index of the eye. Using Gullstrand's no. 1 schematic eyes, Atchison and Smith calculated that a 0.4 mm increase of intraocular lens thickness is likely to produce 18–26 µm for an accommodation of 10.90D for AL measurements obtained by the IOLMaster.[22] We restricted our measurements to a point 25° off-axis and showed some changes in individual subjects, which again suggest that repeating this experiment in subjects with greater amounts of myopia could be useful.
It has been established that ocular rigidity in myopic eyes is significantly lower than found in emmetropic and hyperopic eyes, and it decreases with increasing myopia.[23] A recent study revealed that the low rigidity of myopic eyes caused a significant decrease in the peak velocity of the eye during saccadic eye movements,[24] raising the question of how stable peripheral eye shape is in eyes with greater myopia and lower rigidity.
Previous work has also shown that high myopia is associated with increased eyeball size.[22,25] However, there is no corresponding increase in orbit size with increasing myopia.[26] It is worth considering, therefore, whether the movement of a myopic eye is restricted by the limited size of the orbital cavity compared to emmetropic eyes or hyperopic eyes.
When evaluating the results of earlier work on peripheral retinal profile to obtain off-axis measurements using eye turning, the variations between studies in terms of methods as well as data collection should be considered. As a matter of fact, individual differences in some other factors such as choroidal thickness as well as ocular rigidity may also contribute to the variations between previous studies and the current one.
Conclusion
Our data did not show any clear relationship between peripheral eye length and ocular rotation, even with prolonged and continuous off-axis fixation. The substantial changes observed in subjects with the largest amount of myopia suggest that the effect of the extraocular muscles upon the sclera during ocular rotation is dependent particularly upon ocular rigidity. We think that the effect of ocular rotation could be more apparent if the experiment was repeated in subjects with higher myopia and possibly with longer duration of eccentric fixation.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors disclosed no conflict of interest.
References
- 1.Smith EL, 3rd, Hung LF, Harwerth RS. Developmental visual system anomalies and the limits of emmetropization. Ophthalmic Physiol Opt. 1999;19:90–102. [PubMed] [Google Scholar]
- 2.Mutti DO, Sholtz RI, Friedman NE, Zadnik K. Peripheral refraction and ocular shape in children. Invest Ophthalmol Vis Sci. 2000;41:1022–30. [PubMed] [Google Scholar]
- 3.Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci. 2002;43:3633–40. [PubMed] [Google Scholar]
- 4.Seidemann A, Schaeffel F, Guirao A, Lopez-Gil N, Artal P. Peripheral refractive errors in myopic, emmetropic, and hyperopic young subjects. J Opt Soc Am A Opt Image Sci Vis. 2002;19:2363–73. doi: 10.1364/josaa.19.002363. [DOI] [PubMed] [Google Scholar]
- 5.Wallman J, Winawer J. Homeostasis of eye growth and the question of myopia. Neuron. 2004;43:447–68. doi: 10.1016/j.neuron.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Charman WN. Aberrations and myopia. Ophthalmic Physiol Opt. 2005;25:285–301. doi: 10.1111/j.1475-1313.2005.00297.x. [DOI] [PubMed] [Google Scholar]
- 7.Wallman J, Turkel J, Trachtman J. Extreme myopia produced by modest change in early visual experience. Science. 1978;201:1249–51. doi: 10.1126/science.694514. [DOI] [PubMed] [Google Scholar]
- 8.Wildsoet CF. Active emmetropization – Evidence for its existence and ramifications for clinical practice. Ophthalmic Physiol Opt. 1997;17:279–90. [PubMed] [Google Scholar]
- 9.Wallman J, Adams JI. Developmental aspects of experimental myopia in chicks: Susceptibility, recovery and relation to emmetropization. Vision Res. 1987;27:1139–63. doi: 10.1016/0042-6989(87)90027-7. [DOI] [PubMed] [Google Scholar]
- 10.Smith EL, 3rd, Kee CS, Ramamirtham R, Qiao-Grider Y, Hung LF. Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci. 2005;46:3965–72. doi: 10.1167/iovs.05-0445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith EL, Hung LF, Ramamirtham R, Huang J, Qiao-Grider Y. Optically imposed hyperopic defocus in the periphery can produce central axial myopia in infant monkeys. Investigative Ophthalmology & Visual Science. 2007;48:1533. [Google Scholar]
- 12.Smith EL, 3rd, Hung LF, Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res. 2009;49:2386–92. doi: 10.1016/j.visres.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Millodot M. Effect of ametropia on peripheral refraction. Am J Optom Physiol Opt. 1981;58:691–5. doi: 10.1097/00006324-198109000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Stone RA, Flitcroft DI. Ocular shape and myopia. Ann Acad Med Singap. 2004;33:7–15. [PubMed] [Google Scholar]
- 15.Radhakrishnan H, Charman WN. Refractive changes associated with oblique viewing and reading in myopes and emmetropes. J Vis. 2007;7:5. doi: 10.1167/7.8.5. [DOI] [PubMed] [Google Scholar]
- 16.Radhakrishnan H, Charman WN. Peripheral refraction measurement: Does it matter if one turns the eye or the head? Ophthalmic Physiol Opt. 2008;28:73–82. doi: 10.1111/j.1475-1313.2007.00521.x. [DOI] [PubMed] [Google Scholar]
- 17.Macfadden LA, Gray LS, Strang NC, Seidel D. Peripheral retinal shape measurements, using the IOLMaster, in myopia and hyperopia. Ophthalmic and Physiological Optics. 2008;28:101. [Google Scholar]
- 18.Ehsaei A, Chisholm CM, Pacey IE, Mallen EA. Off-axis partial coherence interferometry in myopes and emmetropes. Ophthalmic Physiol Opt. 2013;33:26–34. doi: 10.1111/opo.12006. [DOI] [PubMed] [Google Scholar]
- 19.Vogel A, Dick HB, Krummenauer F. Reproducibility of optical biometry using partial coherence interferometry: Intraobserver and interobserver reliability. J Cataract Refract Surg. 2001;27:1961–8. doi: 10.1016/s0886-3350(01)01214-7. [DOI] [PubMed] [Google Scholar]
- 20.Connors R, 3rd, Boseman P, 3rd, Olson RJ. Accuracy and reproducibility of biometry using partial coherence interferometry. J Cataract Refract Surg. 2002;28:235–8. doi: 10.1016/s0886-3350(01)01179-8. [DOI] [PubMed] [Google Scholar]
- 21.Atchison DA, Charman WN. Can partial coherence interferometry be used to determine retinal shape? Optom Vis Sci. 2011;88:E601–7. doi: 10.1097/OPX.0b013e318212ae56. [DOI] [PubMed] [Google Scholar]
- 22.Atchison DA, Smith G. Possible errors in determining axial length changes during accommodation with the IOLMaster. Optom Vis Sci. 2004;81:283–6. doi: 10.1097/00006324-200404000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Summers RJ, Shelton S, Norton T. The sclera and myopia. Exp Eye Res. 2006;82:185–200. doi: 10.1016/j.exer.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 24.Alhazmi M, Seidel D, Gray LS. The effect of ocular rigidity upon the characteristics of saccadic eye movements. Invest Ophthalmol Vis Sci. 2014;55:1251–8. doi: 10.1167/iovs.13-13688. [DOI] [PubMed] [Google Scholar]
- 25.Atchison DA, Pritchard N, Schmid KL, Scott DH, Jones CE, Pope JM. Shape of the retinal surface in emmetropia and myopia. Invest Ophthalmol Vis Sci. 2005;46:2698–707. doi: 10.1167/iovs.04-1506. [DOI] [PubMed] [Google Scholar]
- 26.Chau A, Fung K, Pak K, Yap M. Is eye size related to orbit size in human subjects? Ophthalmic Physiol Opt. 2004;24:35–40. doi: 10.1046/j.1475-1313.2003.00159.x. [DOI] [PubMed] [Google Scholar]


