Abstract
Aims
To examine the level of resilience and burnout among British nurses during the second wave of the COVID‐19 pandemic and the influence of personal, social and organisational factors on nurses' resilience and burnout.
Background
Nurses experienced excessive workload and emotional demands over a prolonged period during the COVID‐19 pandemic which may have led to exhaustion. Little research has examined the correlation between the pandemic variables, nurses' resilience and burnout during the second wave of the COVID‐19 pandemic.
Design
This study utilised a descriptive, cross‐sectional research design.
Methods
A cross‐sectional and self‐report survey involved 111 staff nurses, who completed a self‐administrated questionnaire between January and April 2021. A STORBE checklist was used to report the study results.
Findings
The study found that nurses experienced a high level of burnout and low to moderate levels of resilience. The study revealed significant negative relationships between the level of burnout and perceived organisational support and nurses' resilience. The impact of the COVID‐19 pandemic on nurses' social roles and their worries about patient safety were positively correlated with burnout. The perceived organisational support, the impact of the COVID‐19 pandemic on nurses' social roles and the level of resilience were significant factors for burnout.
Conclusions
Nurses experienced a high level of burnout during the second wave of the COVID‐19 pandemic, which may be influenced by how they felt their organisations supported them. Nurses' feelings that the pandemic affected their social roles were associated with increasing their burnout.
Relevance to Clinical Practice
Strategies should be developed to address staff burnout and resilience. Nurse managers and educators should play leadership roles in creating professional training to include competencies and psychological preparedness for disasters and to implement strategies to increase the organisational commitments to staff safety and well‐being.
Keywords: burnout, COVID‐19 pandemic, nurses, organisational support, resilience, social support
1. INTRODUCTION
The World Health Organization (WHO) declared the COVID‐19 pandemic after the worldwide outbreak of Severe Acute Respiratory Syndrome Coronavirus‐2 (SARS‐CoV‐2) in March 2020. Healthcare systems were underprepared during the COVID‐19 pandemic and needed to make a major and sudden restructuring of their services and work routines (WHO, 2021a). Nurses endured a significant burden on their lives due to those sudden changes. They faced challenges regarding safeguarding their health and safety and those of their families. Nurses had to work with an exceptionally large number of patients with contagious and life‐threatening disease in high‐risk clinical environments that, at certain times, lacked adequate personal protective equipment (PPE) and resulted in several nurses dying in the line of duty (UK Government, 2022; WHO, 2021b). Many nurses were redeployed to work in unfamiliar settings or required to work with inexperienced redeployed staff (e.g. critical care nurses working with staff who were inexperience in critical care nursing), and many needed to self‐isolate or live away from their families. These factors, in addition to staff shortage, long working hours, heavy workloads, prolonged duration of the pandemic and being exposed to an increased rate of patient death, can have adverse effects on nurses' well‐being, physical and mental health (Jeleff et al., 2022; Labrague & de los Santos, 2020; Sumner & Kinsella, 2021). The high death rate among healthcare workers during the COVID‐19 pandemic also led to a significant increase in the levels of anxiety among nurses (Lin et al., 2022; Office of National Statistics, 2021; UK Government, 2022; WHO, 2021b). For example, studies found that after the first wave of the COVID‐19 pandemic, up to 45% of clinicians self‐reported post‐traumatic stress disorder symptoms (PTSD), and up to 50% reported psychological distress (Greenberg et al., 2021). Likewise, in a recent meta‐analysis, Pappa et al. (2020) reported that a considerable number of healthcare workers experienced insomnia, depression and anxiety during the COVID‐19 pandemic. This also concurs with findings from Ferry et al. (2020) study, which found increased levels of burnout among clinical staff in the United Kingdom during the first wave of the COVID‐19 pandemic. The prolonged and excessive levels of stressors nurses faced during the pandemic resulted in increased turnover and staff dissatisfaction (de los Santos & Labrague, 2021). It is important to investigate the experiences of front‐line nurses during consecutive waves of the pandemic and identify factors that affected their coping and adaptation to inform future nursing education, staff and system developments. This can enhance staff resilience, safety and well‐being.
2. BACKGROUND
Work overload and emotional demands during the pandemic caused a depletion in nurses' energy, which might have therefore led to exhaustion. Nevertheless, the lack of adequate resources might have caused further challenges and a sense of failure and frustration. Burnout syndrome (BOS) refers to the experience of fatigue and work‐related exhaustion for extended periods and a reduced level of motivation and interest in the job (Peterson et al., 2008). It results in feelings of increased disengagement with work and reduced personal accomplishment and commitment, which in turn can lead to short or even long‐term absenteeism. Burnout has implications for patient safety, and it is a conceptually different variable from well‐being (Delgadillo et al., 2018). Research on these associations is imperative now more than ever, due to increased pressures upon healthcare services causing growing concerns around working conditions and the well‐being of healthcare staff. There has been an increase in the levels of stress and burnout among nurses worldwide during the first wave of the COVID‐19 pandemic (Denning et al., 2021; Ferry et al., 2020; Rose et al., 2022; Sarboozi Hoseinabadi et al., 2020; Tan et al., 2020). But there are limited studies that examined nurses' burnout and the factors affected their adaptation during the second wave of the COVID‐19 pandemic (Ahmed et al., 2022). Staff who are burnt out are at increased risk of error‐making and are more likely to suffer from low engagement and compassion fatigue as reported before (Hall et al., 2016) and during the pandemic (Galanis et al., 2021). De Garcia et al. (2019), in their systematic review, identified that the increased level of burnout among healthcare workers was associated with excessive workloads and a decline in patient safety.
There is increasing recognition that a modern healthcare workforce needs to be resilient to cope with difficult situations (Robertson et al., 2016; WHO, 2021a). Some people are more ‘resilient’ than others, and therefore likely to cope better with challenging times, and therefore remain in the workplace. Previous research has framed healthcare staff resilience in relation to avoiding burnout, which is linked to workplace stress (Fertleman & Carroll, 2013). However, the broader literature on staff resilience appears to be more than not ‘burning out’; it involves positive adaptation and developing personal resources (Cooper et al., 2021). Adverse workplace conditions can affect professional resilience and building resilience among nurses has been considered to support staff retention and reduce their turnover (Ahmed et al., 2022; Hart et al., 2014). Zhang et al. (2021) reported the significant negative correlation between resilience and burnout among healthcare workers during the first wave of the COVID‐19 pandemic. Previous research revealed that nurses with a higher level of resilience had a positive impact on staff's abilities to mediate their stress level (Park et al., 2017), improve their mental well‐being and reduce their risk of burnout (Armstrong et al., 2022; Arrogante & Aparicio‐Zaldivar, 2017).
Various other factors can contribute to people's burnout and resilience when exposed to high job demands and stressful work environments among those are organisational and social support. Employees' perception of organisational support is based on how much their employers consider their needs and value their work (Eisenberger et al., 1986). High levels of perceived organisational support among healthcare workers have been positively correlated with reducing work‐related stress and increasing the quality of patient care, staff performance, job satisfaction and commitment (de los Santos & Labrague, 2021; Ture & Akkoc, 2021). Low levels of perceived organisational support are associated with work absenteeism and intent to turnover (Wang & Wang, 2020). Social support is equally important, and it is related to the quality and function of social relationships that one receives from other people. There are different sources of social support such as family and friends. Social support helps individuals develop close social bonds with other people, provides a sense of belonging and supports people feeling that their life is meaningful. Having adequate social support help people cope with adversities in their life, enhance people's health, well‐being, resilience and reduce the risk of burnout (Galanis et al., 2021; Garcia & Calvo, 2021; Nitschke et al., 2021; Zhang et al., 2021, 2022).
To help understand some of the consequences of the COVID‐19 pandemic on nurses during the second wave of the pandemic, we assessed levels of burnout and resilience and explored some of the factors (e.g. nurses perceived social and organisational support) and pandemic‐related variables (e.g. worries about their safety and patient safety) and explored that may be associated to staff levels of resilience and burnout.
3. THE STUDY
3.1. Aims
To examine the level of resilience and burnout among British nurses during the second wave of the COVID‐19 pandemic and the influence of personal, social and organisational factors on nurses' resilience and their level of burnout.
3.2. Design
This study adopted a quantitative methodology, using a self‐report and cross‐sectional survey design for data collection.
3.3. Sampling and recruitment
A convenience sampling technique was used to recruit study participants. The potential study population included Registered Nurses working in the UK National Health Service (NHS) and healthcare private sectors during the second wave of the COVID‐19 pandemic (January–April 2021) and attending a postgraduate course at a large university in England. The exclusion criteria included Registered Nurses who were not working in a nursing job during the second wave of the COVID‐19 pandemic. This population was selected because they were attending a course at the university where the researchers were based. The rationale for this approach was to reduce any delays in receiving Research Ethics Committee approval, accelerate recruitment from an accessible population and capture the levels of resilience and burnout during the peak of the second wave of the pandemic. Sampling frame of eligible nurses from which the final study sample of the participant was drawn consisted of around 294 participants. The survey was pilot tested on a sample of 10% of participants to ensure the face validity of the tools and the clarity of its content.
3.4. Data collection
After obtaining Research Ethics Committee approval, nurses attending a postgraduate course in the School of Nursing at a large University in England, were sent an email inviting them to participate in this study by the course administrator. The same invitation was released as announcements in the university learning management system to all legible post‐registration nursing modules by the module leaders of each module. The first two sections of the survey provided the participants with a participant information sheet (PIS), a consent form and the researcher's contact detail. Each participant needed to read the first two sections and sign the consent form before progressing to the survey questions. After the initial invitation, participants received six further reminders to complete the survey between January and April 2021.
3.5. Instruments
Data were collected using a self‐report questionnaire through an online secure survey that has five parts (Figure 1).
FIGURE 1.
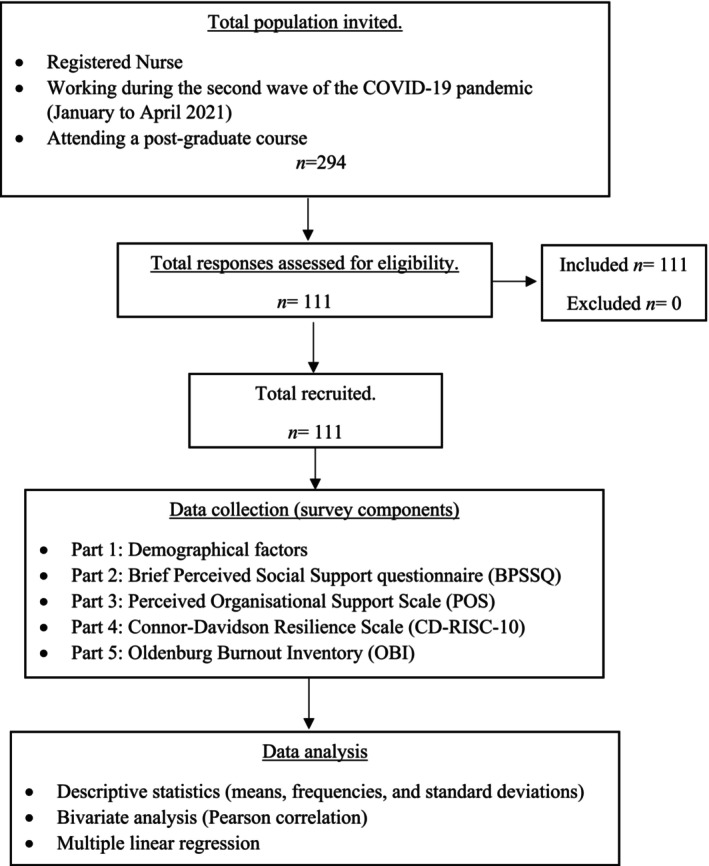
Study design.
3.5.1. Demographic characteristics
Participants' demographical characteristics such as age, gender, marital status, type of employment, healthcare sector, the field of nursing, length of service, professional rank, direct work with COVID‐19 patients, sudden change in work routines, worries about self or family or patient safety, previous resilience training and attendance of well‐being services during the COVID‐19 pandemic were collected.
3.5.2. Perceived social support
The Brief Perceived Social Support questionnaire (BPSSQ) (F‐SozU K‐6) was used to assess participants' perceptions of the extent of social support they receive from others when encountering challenging situations (Kliem et al., 2015). The BPSSQ is a 6‐item scale that the nurses answered by indicating the extent of their agreement with each item using a 5‐point Likert‐type scale, ranging from 1 (not true all) to 5 (true nearly all the time). Higher BPSSQ scores reflect higher levels of perceived social support. The psychometric validity of the BPSSQ scale has been supported in previous research across a range of diverse populations (Lin et al., 2019). The scale had excellent criterion validity and excellent reliability, with an internal consistency of 0.89 (Duan et al., 2019; Lin et al., 2019).
3.5.3. Perceived organisational support
The Perceived Organisational Support (POS) Scale (Eisenberger et al., 1997) was used to assess nurses' perceptions and opinions on the extent to which their organisations recognise and value their well‐being. The POS scale consisted of eight items in which nurses were asked to select their level of agreement or disagreement with each statement using a 7‐point Likert‐type scale ranging from 1 (strongly disagree) to 7 (strongly agree). The scale had a good validity, as supported by its positive association with psychological well‐being and quality of life (Labrague et al., 2018). The POS is widely used and a highly reliable scale with an internal consistency of 0.90 measured by Cronbach's alpha (Labrague et al., 2018).
3.5.4. Resilience
The Connor–Davidson Resilience scale (CD‐RISC‐10) was utilised to measure nurses' perceived level of resilience (Campbell‐Sills & Stein, 2007). The test contains items that describe a person's perceived level of flexibility, self‐efficacy, optimism, ability to regulate emotion and cognitive focus. The scale asks nurses to rate their degree of agreement with given items using a 5‐point Likert‐type, ranging from 0 (not true at all) to 4 (true all time). Higher CD‐RISC‐10 scores indicate a higher level of resilience. CD‐RISC‐10 has been demonstrated to be a valid and reliable measure of assessing resilience in clinical practice (Windle et al., 2011). The Cronbach's alpha score of the CD‐RISC was 0.85 in previous studies (Campbell‐Sills & Stein, 2007).
3.5.5. Burnout
Finally, the fifth part of the questionnaire included Oldenburg Burnout Inventory (OBI) (Bakker & Demerouti, 2007). The prolonged exposure to an extreme level of work‐related stress could lead to burnout. According to the demands–resource model of burnout (Bakker & Demerouti, 2007), burnout syndrome has two components—Disengagement and Exhaustion. Exhaustion is described because of intense cognitive, physical and affective strain commonly caused by excessive or prolonged exposure to work demands. Disengagement describes the relationship between individuals and their jobs by distancing themselves from their jobs, or individuals' negative attitudes or behaviour towards their work and their willingness to continue in the same job (Tipa et al., 2019). OBI items ask participants to rate their degree of agreement with a given item using a 4‐point Likert‐type scale, ranging from 1 (strongly agree) to 4 (strongly disagree). The scale has 16 items with equal positively and negatively worded items in both dimensions which is a strength of this scale. The test yields a total score between 16 and 64 and the higher OBI scores indicate a higher level of burnout. Half of the 16 questions on the OBI scale specifically measure disengagement from the workplace (out of 32 points); the other half specifically measures exhaustion related to and caused by work (out of 32 points). It is a widely used scale as a measure of burnout among different professionals including nurses (Sinval et al., 2019).
3.6. Ethical considerations
Participation in this study was voluntary. All participants were given a participant information sheet and supplied informed consent prior to completing the survey. The School Research Ethics Panel for Allied Health, Nursing and Midwifery and Medicine at Anglia Ruskin University reviewed and approved this study (approval number NM‐SREP‐20‐014).
3.7. Data analysis
Version 28 of the Statistical Package for Social Sciences (SPSS) software was used to analyse the data. The data were quantified using means, frequencies and standard deviations (SDs). Initially, data sets were analysed using histograms and Shapiro–Wilk's test to assess the approximate normality required for parametric tests. The test for normal distribution was satisfactory and supported the application of parametric tests. The analyses demonstrated no violation of the assumption of normality and linearity for multiple linear regression. Pearson's correlation coefficients were used to evaluate the correlations between the demographical variables and key study variables (see Result section). A multiple linear regression (MLR) model was used to identify potential factors that explain the level of burnout during the COVID‐19 pandemic. Variables that significantly correlated with the dependent variable (i.e. OBI) were used in the MLR model. The statistical significance was set for an alpha level at p < 0.05.
4. RESULTS
Responses were received from 111 participants of the 294 nurses invited to complete the survey (37.8% response rate). This study used an anonymous survey sent through announcements in the university learning system. During the peak of the second wave of the COVID‐19 pandemic, nurses were under significant pressure, and the high sickness rate may have affected the response rate. Furthermore, CD‐RISC‐10 manual recommends collecting data within a month of the event to accurately reflect participant resilience, which limited the data collection timeframe. Similar response rates were found in similar studies during the COVID‐19 pandemic (Armstrong et al., 2022; Labrague & de los Santos, 2020; Tan et al., 2020). Table 1 shows that most of the respondents are female (89.2%; N = 99), in a relationship (72.1%; N = 80), aged between 25 and 44 years (74%; N = 82), mainly working in a full‐time job (78.4%; N = 83); in secondary care settings (74.8%; N = 83), more than half are working at staff nurse level (50.6%; N = 56) with an equal distribution between the level of clinical experience among the participants. Table 1 also shows that most of the participants worked directly with COVID‐19 patients (80.2%; N = 89); the intensity of their work increased during the pandemic (75.7%; N = 84), nearly all of them described worries about their safety (97.3%; N = 108) and patient safety (89.2%; N = 99). Finally, half of the participants indicated that working during the pandemic negatively affected their social role (50.5%; N = 56).
TABLE 1.
Sample characteristics (N = 111).
| Variables | N | (%) |
|---|---|---|
| Gender | ||
| Male | 12 | 10.8 |
| Female | 99 | 89.2 |
| Marital status | ||
| Single | 31 | 27.9 |
| Married or in partnership | 80 | 72.1 |
| Age (years) | ||
| <24 | 4 | 3.6 |
| 25–34 | 44 | 39.6 |
| 35–44 | 38 | 34.2 |
| 45–54 | 16 | 14.4 |
| 55–65 | 9 | 8.1 |
| Length of experience (years) | ||
| 0–3 | 39 | 35.1 |
| 4–7 | 33 | 29.7 |
| >7 | 39 | 35.1 |
| Healthcare settings | ||
| NHS secondary healthcare | 83 | 74.8 |
| NHS primary healthcare | 27 | 24.3 |
| Private healthcare | 1 | 0.9 |
| Type status | ||
| Full time (37.5 per week) | 87 | 78.4 |
| Part time (< 37.5 h per week) | 24 | 21.6 |
| Job title | ||
| Staff nurse | 56 | 50.5 |
| Senior staff nurse | 24 | 21.6 |
| Advanced practice or specialist nurse | 27 | 24.3 |
| Managerial, research or administration | 4 | 3.6 |
| Directly working with COVID‐19 patients | ||
| Yes | 89 | 80.2 |
| No | 22 | 19.8 |
| Change in the intensity of work | ||
| Increased | 84 | 75.7 |
| Increased through redeployment | 17 | 15.3 |
| Decreased | 8 | 7.2 |
| No changes | 2 | 1.8 |
| Worries about own or family safety | ||
| Yes | 108 | 97.3 |
| No | 3 | 2.7 |
| Worries about patient safety | ||
| Yes, frequently | 33 | 30 |
| Yes, occasionally | 66 | 59.5 |
| No | 12 | 10.5 |
| Pandemic impact on staff social role | ||
| Yes | 56 | 50.5 |
| No | 55 | 49.5 |
4.1. Description of study variables
Table 2 shows Cronbach's alpha, the mean score and standard deviations (SD) for all the scales used in the survey. The results illustrate an excellent level of reliability demonstrated by Cronbach's alpha equal to or above 0.85 for all the used scales (BPSSQ, CD‐RISC‐10, OBI and POS). These findings are consistent with previously reported levels of reliability of the scales tested on samples from diverse populations (see Instruments section). The Cronbach's alpha for Disengagement was 0.74 and Exhaustion was 0.77, which is also still considered a high level of internal consistency. The overall mean score of OBI in this study sample was 2.62 (SD = 0.41), with the Disengagement level being 2.47 (SD = 0.44) and the Exhaustion level being 2.77 (SD = 0.46). Peterson et al. (2008) considered an average cut‐off score of ≥2.25 for Exhaustion and ≥2.1 for Disengagement. One hundred and three nurses (93%) had a high score for Exhaustion, that is, a score of ≥2.25 based on cut‐off points, and 91 nurses (82%) had a high score for Disengagement, that is, a score of ≥2.1. This indicates that between 80% and 90% of the nurses experienced a high level of burnout related to work or caused by work during the COVID‐19 pandemic, with a higher level of exhaustion than disengagement.
TABLE 2.
Descriptive statistics.
| Measure | Mean (SD) | Minimum | Maximum | Cronbach's alpha |
|---|---|---|---|---|
| CD‐RSIC | 28.23 (5.54) | 15 | 40 | 0.85 |
| BPSSQ | 22.60 (4.79) | 10 | 30 | 0.86 |
| POS | 4.00 (1.29) | 1.13 | 6.5 | 0.89 |
| OBI‐overall | 2.62 (0.41) | 1.56 | 2.61 | 0.85 |
| OBI‐Exhaustion | 2.77 (0.46) | 1.63 | 3.88 | 0.77 |
| OBI‐Disengagement | 2.47 (0.44) | 1.50 | 3.50 | 0.74 |
Abbreviations: BPSSQ: Brief Perceived Social Support questionnaire, CD‐RISC: Connor–Davidson Resilience scale, OBI: Oldenburg Burnout Inventory, POS: Perceived Organisational Support.
The mean resilience score in this sample was 28.23 (SD = 5.54). Scoring lower or equal to the 25th percentile is considered a low level of resilience. Twenty‐two per cent (N = 24) were of low resilience; 50% (N = 56) were of moderate resilience level (scoring above the 25th percentile but less than the 75th percentile), and 28% (N = 31) were of high resilience level (scoring above 75th percentile).
4.2. Correlations between study variables
Bivariate analysis revealed significant negative correlations between the level of burnout and both the perceived organisational support (r = −0.436, p < 0.001) and the level of resilience (r = −0.227, p < 0.02) (See Table 3). Therefore, lower levels of resilience and perceived organisational support are associated with higher levels of burnout. In addition, a positive correlation was also found between the level of resilience and perceived social support (r = 0.362, p < 0.001). Thus, an increased level of social support is associated with an increase in the level of resilience. The perceived organisational support was positively correlated to the perceived social support (r = 0.244, p = 0.01). However, it was negatively correlated to nurses' worries about patient safety (r = −0.306, p = 0.001) and the impact of the pandemic on their social roles (r = −0.273, p < 0.004). Pearson's correlation analysis also showed significant positive relationships between the level of burnout and the impact of the COVID‐19 pandemic on nurses' social role (r = 0.344, p < 0.001) and their worries about patient safety (r = 0.265, p = 0.005). In other words, nurses who had more worries about patient safety or perceived the pandemic to have negatively affected their social role had higher levels of burnout. Finally, there was a negative correlation between the Disengagement dimension of burnout and age (r = −0.197, p = 0.038). Therefore, young age was associated with higher levels of burnout. There were no other significant relationships between demographical variables and measures of resilience.
TABLE 3.
Significant Pearson's correlation coefficient between the variables and levels of resilience and burnout.
| Variables | 1. OBI overall | 2. OBI‐ disengagement | 3. OBI‐ exhaustion | 4. CD‐RSIC | 5. POS | 6. BPSSQ | 7. Pandemic impact on social role | 8. Worries about patient safety |
|---|---|---|---|---|---|---|---|---|
| 1. OBI overall | ||||||||
| 2. OBI‐ Disengagement | 0.916*** | |||||||
| 3. OBI‐ Exhaustion | 0.919*** | 0.684*** | ||||||
| 4. CD‐RSIC | −0.227* | −0.145 | −0.269** | |||||
| 5. POS | −0.436*** | −0.435*** | −0.367*** | 0.091 | ||||
| 6. BPSSQ | −0.180 | −0.115 | −0.214* | 0.362*** | 0.244** | |||
| 7. Pandemic impact on social role | 0.344*** | 0.296*** | 0.330*** | 0.081 | −0.273** | −0.150 | ||
| 8. Worries about patient safety | 0.265** | 0.236* | 0.249** | −0.004 | −0.306*** | −0.065 | 0.221* | |
| 9. Age | −0.163 | −0.197* | −0.100 | 0.053 | 0.115 | −0.021 | 0.53 | 0.024 |
Abbreviations: BPSSQ, Brief Perceived Social Support questionnaire; CD‐RISC, Connor–Davidson Resilience scale; OBI, Oldenburg Burnout Inventory; POS, Perceived Organisational Support.
p ≤ 0.05;
p ≤ 0.01;
p ≤ 0.001.
4.3. Predictors of burnout among nursing staff
After determining the significant correlations, a multiple linear regression analysis was performed to determine if their value was predictive of burnout. Based on multiple linear regression analyses, as illustrated in Table 4, organisational support (β = −0.343, p < 0.001), resilience (β = −0.217, p = 0.009) and the pandemic impact on social role (β = 0.268, p = 0.002) were significant predictors of nurses' level of burnout during the second wave of the COVID‐19 pandemic. In other words, decreased levels of personal resilience and organisational support measures were associated with increased levels of burnout during the COVID‐19 pandemic. Moreover, increased perceptions that the COVID‐19 pandemic impacted on the nurses' social role was associated with increased levels of burnout. The overall model fit was adjusted R 2 = 0.271, F(3, n = 109) =14.635, p < 0.001). In the regression model, Table 4, only three variables demonstrated significant associations with burnout and explained 27.1% of the variation in burnout.
TABLE 4.
Multiple linear regression analysis of the association of organisations support, resilience and impact of the pandemic on social role on burnout.
| B | SE | β | t | 95% confidence interval | Regression model | |
|---|---|---|---|---|---|---|
| Constant | 3.179 | 0.227 | 13.99 | 2.729 to 3.630 | ||
| POS | −0.014 | 0.003 | −0.343*** | −4.022 | −0.020 to −0.007 | |
| CD‐RISC | −0.016 | 0.006 | −0.217** | −2.643 | −0.028 to −0.004 | |
| Pandemic impacted on social role | 0.220 | 0.070 | 0.268** | 3.151 | 0.081 to 0.358 | |
| R 2 | 0.291 | |||||
| Adjusted R 2 | 0.271 | |||||
| F value | 14.635*** |
Abbreviations: CD‐RISC, Connor–Davidson Resilience scale; POS, Perceived Organisations Support.
p ≤ 0.05;
p ≤ 0.01;
p ≤ 0.001.
5. DISCUSSION
Healthcare worker burnout was already a concern before the COVID‐19 pandemic. The first wave of the pandemic resulted in nurses experiencing severe psychological distress (Greenberg et al., 2021; Pappa et al., 2020) and contributed to an increased risk of clinical errors and burnout. The second wave and the prolonged period of the COVID‐19 pandemic created excessive and persistent pressures on healthcare services and added a further burden on nurses (Roberts et al., 2022). There is limited research that examined the levels of burnout, resilience and the factors associated with those levels among nurses in the United Kingdom during the second wave of the COVID‐19 pandemic. Therefore, this research investigated those variables.
5.1. Levels of resilience and burnout
Our study reported high levels of burnout, work‐related exhaustion and disengagement. This is consistent with the findings that examined level burnout among nurses elsewhere using the same scale during the first wave of the COVID‐19 pandemic, such as studies undertaken in Singapore (Tan et al., 2020) and Iran (Sarboozi Hoseinabadi et al., 2020). Similarly, Ferry et al. (2020) conducted a study in the United Kingdom using Copenhagen Burnout Inventory and found that 245 (86%) out of 286 nurses reported having moderate to severe levels of burnout during the first wave of the COVID‐19 pandemic. In a meta‐analysis, Galanis et al. (2021) also found a high prevalence of emotional exhaustion among nurses during the COVID‐19 pandemic. As predicted, our study found slightly higher levels of burnout among nurses during the second wave of the COVID‐19 pandemic compared to studies conducted during the first wave of the pandemic. This is consistent with similar studies that discussed the prolonged pressure of work during the COVID‐19 pandemic led to nurses' physical fatigue, increased burnout and psychological symptoms (Sirkaras et al., 2022). Staff exhaustion and disengagement with their work could be explained by work‐related pressure or by a lack of staff preparedness to deal with this pandemic. Our study found a moderate level of resilience using the CD‐RISC 10‐ items scale. A finding slightly lower than the mean scores reported in most of the other published nursing research that used the same scale. For instance, studies undertaken in USA among nurses following a tornado (Brown et al., 2018; Turner, 2015) and New Zealand (Tabakakis et al., 2019). Ahmed et al. (2022) recently reported low to moderate levels of resilience among healthcare workers in United Arab Emirates during the second wave of the COVID‐19 pandemic which is consistent with this study. Our study results also concur with the findings from previous research conducted elsewhere using CD‐RISC 25‐items such as studies conducted in Australia (Guo et al., 2019) and Turkey (Alan et al., 2022).
5.2. The impact of organisational support and pandemic‐related factors on levels of burnout
This study reports that the independent factors of overall burnout among our sample are perceived organisational support (POS), staff resilience and the perceived impact the pandemic had on staff social roles. POS describes employees' perceptions of whether their organisations value their contributions and care about their well‐being. The perceived organisational support among nurses in our sample was negatively correlated with the level of burnout and significant predictor of burnout. This is consistent with the findings of previous research, for example, lower levels of POS are reported to have negative effects on the intention to leave the employment (de los Santos & Labrague, 2021). In contrast, higher levels of POS and a supportive work environment are reported to have a positive correlation with staff satisfaction and empowerment (Ahmed et al., 2022; Ture & Akkoc, 2021). Nurses' worries about safety their own and patients' safety and how the pandemic affected their social role within their families can increase the physical and psychological demands on staff and contribute to their exhaustion and burnout. Galanis et al. (2021) also identified staff perceptions of the impact of COVID‐19 on their safety and patient safety as contributing factors to increase risk of burnout.
5.3. The impact of social support on levels of resilience
The study found that nurses greatly value their social support, and this was correlated positively with sustaining their resilience. This study extends the findings of previous research showing that stronger social support during the pandemic helped nurses become more resilient. For instance, Nitschke et al. (2021) reported the benefit of social support in fostering resilience by buffering against negative physical and mental health outcomes. Zhang et al. (2022) and Zhang et al. (2021) also found a similar result that resilience was a mediator in the relationships between perceived social support and dimensions of burnout. Support from family, friends and colleagues is crucial for nurses to cope with the emotional demands of their work. Social support provides a sense of belonging, validation and reassurance that helps nurses maintain a positive outlook, feel less isolated and cope better with stress and emotional exhaustion. However, our study also found that nurses' worries about patient safety and how the pandemic affected their social role were associated with increasing their exhaustion and burnout. Likewise, Ferry et al. (2020) reported a high level of stress among healthcare staff during the first wave of the COVID‐19 pandemic was primarily associated with staff concern about the health of their families and their safety. De Garcia et al. (2019) also identified that a decline in patient safety was also associated with an increased level of burnout among healthcare workers. Healthcare organisations must prevent harm and ensure staff feels safe at work by enhancing their working conditions.
The staff working in the UK healthcare system are its greatest asset and are key to delivering safe and effective care. Although on most occasions and under normal circumstances, nurses are resilient to cope with work‐related pressure, they appear to need higher levels of resilience and psychological preparedness to cope with the challenging and extraordinary working conditions. Conditions resulted from pandemic‐related factors and potentially other chronic factors related to the capabilities of the healthcare system. In the last decay, the healthcare system in the United Kingdom struggled with longstanding staff shortages, staff turnover and inadequate investments that resulted in an underprepared system to effectively respond to and manage disasters as demonstrated during the COVID‐19 pandemic (The King's Fund, 2022). For healthcare workers to provide consistently high standards and safety, there is a need for the healthcare systems to focus on reducing turnover, recruiting and retaining staff to ensure any pre‐pandemic deficits in the workforce are filled and any predicted increase in demand which will widen workforce gaps are filled. Without staffing standards being maintained, there will be a longer term workforce crisis and a risk to patient safety due to the potential psychological harm and impact on staff experience.
5.3.1. Strengths and limitations
This study was conducted at the peak of the second wave of the COVID‐19 pandemic, provided comparative data on the levels of burnout and resilience to studies conducted during the first phase of the pandemic. It identified significant factors that affected clinically working nurses from range of healthcare settings. There are several limitations to this study. First, although the results of our study concur with the findings from previous studies conducted during the first wave of the COVID‐19 pandemic, the cross‐sectional design averts the inference of causality. Therefore, only an association, and not causation, can be inferred and further longitudinal and should be conducted to confirm the findings. Second, although the study participants worked in different healthcare settings including primary, second and tertiary care, they were recruited from one university in England. Therefore, the findings in this study might not be representative of the whole population and generalisable to other regions or countries. Third, the fact that participation is voluntary, and the self‐reported information has limitations for the interpretation of the study results. Selection and non‐response biases may be generated due to the study design and the data collection strategy. For example, if the participants who consent to participate in the study differ from those who do not, resulting in a sample that is not representative of the population. Fourth, in the multiple linear regression model, all variables explained 27.1% of the variance. This means that many other factors affecting burnout among nurses were not examined in this study. Future studies are recommended to avoid these limitations, for example, using longitudinal research designs or qualitative research to explore more relevant factors.
6. CONCLUSION
As a result of this study, it was determined that British nurses experienced a relatively high level of burnout during the second wave of the COVID‐19 pandemic, which may be influenced by how they felt their organisations supported them. Although nurses perceived being socially supported by their families and this type of support had a positive correlation with their level of resilience, their feelings that the COVID‐19 pandemic negatively impacted their social role towards their families were in contrary associated with increasing their level of burnout. More research is needed to gain an in‐depth understanding of the long‐term effect of the COVID‐19 pandemic on nurses and service delivery. There is a scope to improve organisational commitments so that nurses feel adequately valued by their employers and feel able to fulfil their social roles. Building a resilient system requires long‐term investments in developing the capacity and preparedness of the healthcare workforce to deal with disasters and mitigate the impact of future pandemics on staff well‐being and quality of patient care. Therefore, more research is needed on how staff perceived organisational support and the usefulness of a disaster preparedness training programme in developing nurses' capabilities and resilience.
6.1. Implication to practice
Based on the study finding, healthcare systems must value nurses as skilled professionals and acknowledge their critical role in providing high‐quality patient care. To achieve this, organisations should demonstrate more commitment to staff, foster a culture of appreciation and recognition and offer opportunities for career advancement and professional development. Nurse managers should provide support for nurses to maintain a healthy work–life balance, including flexible working, self‐care strategies and training opportunities. Nurse managers should also promote a nurturing and compassionate work environment by understanding staff needs and considering interventions tailored to individual needs and preferences. These interventions should be integrated into work plans and allocated the shift patterns to provide protected time and support staff in tackling staff work stress. A multilevel system, including resilience hubs, mental health support, clinical psychologists, professional advocacy provision and buddy systems (Albott et al., 2020), can support staff resilience and well‐being. This will contribute to building a more sustainable and effective healthcare system for the future.
There is currently a lack of disaster preparedness training for healthcare staff in the United Kingdom. Therefore, considering training that includes professional competencies and psychological preparedness (Alan et al., 2022) would have the benefits in enhancing nurses' capabilities and resilience to respond effectively to future disasters and reduce the risk of burnout. Nurse educators and managers should take a leadership role in developing and planning disaster preparedness training for nurses to enhance their capabilities and resilience in responding to future disasters and reduce the risk of burnout.
FUNDING INFORMATION
This research did not receive any specific grant from funding agencies in the public, commercial or not‐for‐profit sectors.
CONFLICT OF INTEREST STATEMENT
No conflict of interest exists in the submission of this article.
STATISTICS
An expert statistician checked the study statistics prior to submission by Dr Jufen Zhang, Ph.D., email: jufen.zhang@aru.ac.uk.
Statistical methods used in this study include descriptive statistics, Pearson's correlation coefficient and multiple linear regression.
NO PATIENT OR PUBLIC CONTRIBUTION
There was no active public or patient involvement in this study. The study explored nurses' burnout during the second wave of the COVID‐19 pandemic. The idea came from a discussion of the lead author as a nurse educator with clinical colleagues who described experiences of physical and psychological exhaustion caused by persistent work pressure during the pandemic. The participants did not have an active involvement in the study design.
ACKNOWLEDGEMENTS
We thank all nurses who participated in this study and all the administrator who support the distribution of this survey. We also thank Dr Jufen Zhang for their help and support with statistical analysis.
Abdulmohdi, N. (2024). The relationships between nurses' resilience, burnout, perceived organisational support and social support during the second wave of the COVID‐19 pandemic: A quantitative cross‐sectional survey. Nursing Open, 11, e2036. 10.1002/nop2.2036
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Ahmed, F. , Bani‐Issa, W. , Timmins, F. , Dias, J. M. , al‐Yateem, N. , Subu, M. A. , Alzahmi, S. M. , Saqan, R. , Abdul Rahman, H. , & AbuRuz, M. (2022). Managing during the COVID‐19 pandemic: A cross‐sectional study of health care workers' perceived organizational support and its consequences on their compassion, resilience and turnover intention. Journal of Nursing Management., 30(7), 2642–2651. 10.1111/jonm.13824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alan, H. , Eskici, G. , Sen, H. , Bacaksiz, F. E. , et al. (2022). Nurses' disaster core competencies and resilience during the COVID‐19 pandemic: A cross‐sectional study from Turkey. Journal of Nursing Management, 30(3), 622–632. 10.1111/jonm.13552 [DOI] [PubMed] [Google Scholar]
- Albott, C. , Wozniak, J. , McGlinch, B. , Wall, M. H. , Gold, B. S. , & Vinogradov, S. (2020). Battle buddies: Rapid deployment of a psychological resilience intervention for health care workers during the coronavirus disease 2019 pandemic. International Anesthesia Research Society, 131(1), 43–54. 10.1213/ANE.0000000000004912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong, S. , Porter, J. E. , Larkins, J. A. , & Mesagno, C. (2022). Burnout, stress and resilience of an Australian regional hospital during COVID‐19: A longitudinal study. BMC Health Services Research, 22, 1115. 10.1186/s12913-022-08409-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrogante, O. , & Aparicio‐Zaldivar, E. (2017). Burnout and health among critical care professionals: The mediational role of resilience. Intensive and Critical Care Nursing, 42, 110–115. [DOI] [PubMed] [Google Scholar]
- Bakker, A. B. , & Demerouti, E. (2007). The job demands‐resources model: State of the art. Journal of Managerial Psychology, 22(3), 309–328. [Google Scholar]
- Brown, R. , Wey, H. , & Foland, K. (2018). The relationship among change fatigue, resilience, and job satisfaction of hospital staff workers. Journal of Nursing Scholarship, 50, 306–313. 10.1111/jnu.12373 [DOI] [PubMed] [Google Scholar]
- Campbell‐Sills, L. , & Stein, M. B. (2007). Psychometric analysis and refinement of the Connor‐Davidson resilience scale (CD‐RISC): Validation of a 10‐item measure of resilience. Journal of Traumatic Stress, 20, 1019–1028. 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- Cooper, A. , Brown, J. , & Leslie, G. (2021). Nurse resilience for clinical practice: An integrative review. Journal of Advanced Nursing, 77, 2623–2640. 10.1111/jan.14763 [DOI] [PubMed] [Google Scholar]
- de Garcia, C. L. , de Abreu, L. C. , Ramos, J. L. S. , Castro, C. F. D. , Smiderle, F. R. N. , Santos, J. A. D. , & Bezerra, I. M. P. (2019). Influence of burnout on patient safety: Systematic review and meta‐analysis. Medicina, 55, 553. 10.3390/medicina55090553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de los Santos, J. A. A. , & Labrague, L. J. (2021). The impact of fear of COVID‐19 on job stress, and turnover intentions of frontline nurses in the community: A cross‐sectional study in The Philippines. Traumatology, 27(1), 52–59. 10.1037/trm0000294 [DOI] [Google Scholar]
- Delgadillo, J. , Saxon, D. , & Barkham, M. (2018). Associations between therapists' occupational burnout and their patients' depression and anxiety treatment outcomes. Depress and Anxiety, 35, 844–850. 10.1002/da.22766 [DOI] [PubMed] [Google Scholar]
- Denning, M. , Goh, E. T. , Tan, B. , Kanneganti, A. , Almonte, M. , Scott, A. , Martin, G. , Clarke, J. , Sounderajah, V. , Markar, S. , Przybylowicz, J. , Chan, Y. H. , Sia, C. H. , Chua, Y. X. , Sim, K. , Lim, L. , Tan, L. , Tan, M. , Sharma, V. , … Kinross, J. (2021). Determinants of burnout and other aspects of psychological well‐being in healthcare workers during the Covid‐19 pandemic: A multinational cross‐sectional study. PLoS One, 16(4), e0238666. 10.1371/journal.pone.0238666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan, X. , Ni, X. , Shi, L. , Zhang, L. , Ye, Y. , Mu, H. , Li, Z. , Liu, X. , Fan, L. , & Wang, Y. (2019). The impact of workplace violence on job satisfaction, job burnout, and turnover intention: The mediating role of social support. Health and Quality of Life Outcomes, 17(93), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger, R. , Cummings, J. , Armeli, S. , & Lynch, P. (1997). Perceived organizational support, discretionary treatment, and job satisfaction. Journal of Applied Psychology, 82, 812–820. 10.1037/0021-9010.82.5.812 [DOI] [PubMed] [Google Scholar]
- Eisenberger, R. , Huntington, R. , Hutchison, S. , & Sowa, D. (1986). Perceived organizational support. Journal Application Psycholology, 71(3), 500–507. [Google Scholar]
- Ferry, A. , Wereski, R. , Strachan, F. , & Mills, N. L. (2020). Predictors of healthcare worker burnout during the COVID‐19 pandemic. QJM, 114(6), 374–380. 10.1093/qjmed/hcab065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fertleman, C. , & Carroll, W. (2013). Protecting students and promoting resilience. BMJ, 347, f5266. [DOI] [PubMed] [Google Scholar]
- Galanis, P. , Vraka, I. , Fragkou, D. , Bilali, A. , & Kaitelidou, D. (2021). Nurses' burnout and associated risk factors during the COVID‐19 pandemic: A systematic review and meta‐analysis. Journal of Advanced Nursing, 77, 3286–3302. 10.1111/jan.14839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia, G. M. , & Calvo, A. (2021). The threat of COVID‐19 and its influence on nursing staff burnout. Journal of Advanced Nursing, 77, 832–844. 10.1111/jan.14642 [DOI] [PubMed] [Google Scholar]
- Greenberg, N. , Weston, D. , Hall, C. , Caulfield, T. , Williamson, V. , & Fong, K. (2021). Mental health of staff working in intensive care during Covid‐19. Occupational Medicine, 71(2), 62–67. 10.1093/occmed/kqaa220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo, Y. F. , Plummer, V. , Lam, L. , Wang, Y. , Cross, W. , & Zhang, J. P. (2019). The effects of resilience and turnover intention on nurses' burnout: Findings from a comparative cross‐sectional study. Journal of Clinical Nursing, 28(3–4), 499–508. 10.1111/jocn.14637 [DOI] [PubMed] [Google Scholar]
- Hall, L. H. , Johnson, J. , Watt, I. , Tsipa, A. , & O’Connor, D. B. (2016). Healthcare staff wellbeing, burnout, and patient safety: A systematic review. PLoS One, 11(7), e0159015. 10.1371/journalpone.0159015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart, P. L. , Brannan, J. D. , & Chesnay, M. D. (2014). Resilience in nurses' an integrative review. Journal of Nursing Management, 22, 720–734. [DOI] [PubMed] [Google Scholar]
- Jeleff, M. , Traugott, M. , Jirovsky‐Platter, E. , Jordakieva, G. , & Kutalek, R. (2022). Occupational challenges of healthcare workers during the COVID‐19 pandemic: A qualitative study. BMJ Open, 12, e054516. 10.1136/bmjopen-2021-054516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kliem, S. , Mößle, T. , Rehbein, F. , Hellmann, D. F. , Zenger, M. , & Brähler, E. (2015). A brief form of the perceived social support questionnaire (F‐SozU) was developed, validated, and standardized. Journal of Clinical Epidemiology, 68(2015), 551–562. 10.1016/j.jclinepi.2014.11.003 [DOI] [PubMed] [Google Scholar]
- Labrague, L. , & de los Santos, J. A. (2020). COVID‐19 anxiety among front‐line nurses: Predictive role of organisational support, personal resilience and social support. Journal of Nursing Management, 28(7), 1653–1661. 10.1111/jonm.13121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague, L. , McEnroe Petitte, D. , Leocadio, M. C. , van Bogaert, P. , & Tsaras, K. (2018). Perceptions of organizational support and its impact on nurses' job outcomes. Nursing Forum, 53, 339–347. 10.1111/nuf.12260 [DOI] [PubMed] [Google Scholar]
- Lin, M. , Hirschfeld, G. , & Margraf, J. (2019). Brief form of the perceived social support questionnaire (F‐SozU K‐6): Validation, norms, and cross‐cultural measurement invariance in the USA, Germany, Russia, and China. Psychological Assessment, 31(5), 609–621. 10.1037/pas0000686 [DOI] [PubMed] [Google Scholar]
- Lin, S. , Deng, X. , Ryan, I. , Zhang, K. , Zhang, W. , Oghaghare, E. , Gayle, D. D. B. , & Shaw, B. (2022). COVID‐19 symptoms and deaths among healthcare workers, United States. Emerging Infectious Diseases, 28(8), 1624–1632. 10.3201/eid2808.212200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitschke, J. , Forbes, P. , Ali, N. , Cutler, J. , Apps, M. A. J. , Lockwood, P. L. , & Lamm, C. (2021). Resilience during uncertainty? Greater social connectedness during COVID‐19 lockdown is associated with reduced distress and fatigue. British Journal of Health Psychology, 26(2), 553–569. 10.1111/bjhp.12485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of National Statistics . (2021). Coronavirus (COVID‐19) related deaths by occupation, England and Wales: Deaths registered between 9 March and 28 December 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/bulletins/coronaviruscovid19relateddeathsbyoccupationenglandandwales/deathsregisteredbetween9marchand28december2020
- Pappa, S. , Ntella, V. , Giannakas, T. , Giannakoulis, V. G. , Papoutsi, E. , & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. Brain, Behavior, and Immunity, 8, 901–907. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, J. H. , Lee, E. N. , Kong, K. R. , & Jang, M. J. (2017). Hardiness mediates stress and impact level in ED nurses who experienced a violent event. Journal of Emergency Nursing, 43, 539–544. [DOI] [PubMed] [Google Scholar]
- Peterson, U. , Demerouti, E. , Bergström, G. , Samuelsson, M. , Åsberg, M. , & Nygren, Å. (2008). Burnout and physical and mental health among Swedish healthcare workers. Journal of Advanced Nursing, 62, 84–95. 10.1111/j.1365-2648.2007.04580.x [DOI] [PubMed] [Google Scholar]
- Roberts, N. , McAloney‐Kocaman, K. , Lippiett, K. , Ray, E. , Welch, L. , & Kelly, C. A. (2022). Factors influencing fatigue in UK nurses working in respiratory clinical areas during the second wave of the Covid‐ 19 pandemic: An online survey. Journal of Clinical Nursing, 25, 1–11. 10.1111/jocn.16375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson, H. , Elliott, A. , Burton, C. , Iversen, L. , Murchie, P. , Porteous, T. , & Matheson, C. (2016). Resilience of primary healthcare professionals: A systematic review. British Journal of General Practice, 66(647), e423–e433. 10.3399/bjgp16X685261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose, S. , Hartnett, J. , & Pillai, S. (2022). A comprehensive dataset describing nurse's emotions, perceived stressors and coping mechanisms during the first surge of the COVID‐19 pandemic. Data in Brief., 40, 107814. 10.1016/j.dib.2022.107814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarboozi Hoseinabadi, T. , Kakhki, S. , Teimori, G. , & Nayyeri, S. (2020). Burnout and its influencing factors between frontline nurses and nurses from other wards during the outbreak of coronavirus disease – COVID‐19‐ in Iran. Nursing Research and Education, 38(2), e03. 10.17533/udea.iee.v38n2e03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinval, J. , Queiros, C. , Pasian, S. , & Maroco, J. (2019). Transcultural adaptation of the Oldenburg burnout inventory (OBI) for Brazil and Portugal. Frontiers in Psychology, 10, 1–28. 10.3389/fpsyg.2019.00338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirkaras, C. , Ilias, I. , Tselebis, A. , & Pachi, A. (2022). Nursing staff fatigue and burnout during the COVID‐19 pandemic in Greece. AIMS Public Health, 9(1), 94–105. 10.3934/publichealth.2022008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumner, R. , & Kinsella, E. (2021). Grace under pressure: Resilience, burnout, and wellbeing in frontline Workers in the United Kingdom and Republic of Ireland during the SARS‐CoV‐2 pandemic. Frontiers in Psychology, 11, 1–18. 10.3389/fpsyg.2020.576229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabakakis, C. , McAllister, M. , Bradshaw, J. , & To, Q. G. (2019). Psychological resilience in New Zealand registered nurses: The role of workplace characteristics. Journal Nursing Management, 27, 1351–1358. 10.1111/jonm.12815 [DOI] [PubMed] [Google Scholar]
- Tan, B. , Kanneganti, A. , Lim, L. , Tan, M. , Chua, Y. X. , Tan, L. , Sia, C. H. , Denning, M. , Goh, E. T. , Purkayastha, S. , Kinross, J. , Sim, K. , Chan, Y. H. , & Ooi, S. B. S. (2020). Burnout and associated factors among health Care Workers in Singapore during the COVID‐19 pandemic. Journal of the American Medical Director Association., 21(12), 1751–1758e. 10.1016/j.jamda.2020.09.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The King's Fund . (2022). NHS staffing shortages. www.kingsfund.org.uk/sites/default/files/2022‐11/NHS_staffing_shortages_final_web%20%282%29.pdf
- Tipa, R. O. , Tudose, C. , & Pucarea, V. (2019). Measuring burnout among psychiatric residents using the Oldenburg burnout inventory (OBI) instrument. Journal of Medicine and Life, 12(4), 354–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ture, A. , & Akkoc, I. (2021). The mediating role of social support in the effect of perceived organizational support and psychological empowerment on career satisfaction in nurses. Perspectives in Psychiatric Care, 56(4), 985–998. 10.1111/ppc.12562 [DOI] [PubMed] [Google Scholar]
- Turner, S. (2015). Resilience of nurses in the face of disaster. Disaster Medicine and Public Health Preparedness, 9(6), 1–4. 10.1017/dmp.2015.70 [DOI] [PubMed] [Google Scholar]
- UK Government . (2022). COVID‐19 and Occupational Impacts. https://www.gov.uk/government/publications/covid‐19‐and‐occupational‐impacts/covid‐19‐and‐occupational‐impacts
- Wang, Q. , & Wang, C. (2020). Reducing turnover intention: Perceived organizational support for frontline employees. Frontiers of Business Research in China, 14, 6. 10.1186/s11782-020-00074-6 [DOI] [Google Scholar]
- WHO . (2021a). Health systems resilience during COVID‐19: Lessons for building back better. https://apps.who.int/iris/rest/bitstreams/1390564/retrieve [PubMed]
- WHO . (2021b). The impact of COVID‐19 on health and care workers: a closer look at deaths. https://apps.who.int/iris/handle/10665/345300
- Windle, G. , Bennett, K. M. , & Noyes, J. A. (2011). Methodological review of resilience measurement scales. Health and Quality of Life Outcomes, 9(8), 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. , Guan, C. , Jiang, J. , Zhu, C. , & Hu, X. (2022). Mediating effect of resilience on the relationship between perceived social support and burnout among Chinese palliative nurses. Journal of Clinical Nursing, 32(13–14), 3887–3897. 10.1111/jocn.16532 [DOI] [PubMed] [Google Scholar]
- Zhang, Y. , Jiang, J. , Ni, P. , Li, H. , Li, C. , Zhou, Q. , Ou, Z. , Guo, Y. , & Cao, J. (2021). Association between resilience and burnout of front‐line nurses at the peak of the COVID‐19 pandemic: Positive and negative affect as mediators in Wuhan. International Journal of Mental Health Nursing, 30, 939–954. 10.1111/inm.12847 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


