Abstract
A 45-year-old male patient with clinically suspected schizophrenia was referred for an MRI brain to look for organicity. An incidental lesion was noted on the right side of the tubercinerium with suspicious findings of osteolipoma. T1 and T2 weighted sequences showed a hyper-intense lesion suggestive of fatty intensity or hemorrhage. A homogenous blooming artefact was seen on gradient imaging suggestive of a calcific/hemorrhagic element. The referring clinician was conveyed the findings asking about the need for further imaging by CT. The patient was started on antipsychotics for schizophrenia. One week later, a CT head was obtained, which showed a fatty density lesion with a smooth, peripheral rim of hyperdensity. The HU value matched rim calcification suggesting radiological diagnosis of osteolipoma. The patient was kept under close observation and no specific therapy was guided to this lesion. The patient was responding well to pharmacotherapy (in terms of control of symptoms) confirming osteolipoma as an incidental finding. This case report establishes the role of adequate imaging in subtle brain lesions which may mimic primary lesion-producing neurological symptoms. The importance of clinical judgment and follow-up in guiding suitable therapy is also highlighted.
Keywords: Osteolipoma, Tubercinerium, Mammillary body, CT, MRI, Incidental finding
Introduction
Intracranial lipomas are rare, benign masses accounting for less than 1% of all intracranial tumors. Rarely, intracranial lipomas may demonstrate osseous transformation or metaplasia. Nevertheless, the incidence remains undetermined [1]. The peculiar architectural arrangement of a central core of mature adipose tissue and a peripheral rim of bone helps distinguish these ossified masses from other lipomas [2]. They are consistently found between corpora mammillaria and the pituitary stalk and demonstrate marked consistency in their size. Histologically, they are displaced elements of mesenchyme encompassing walls of the cricopharyngeal duct. They are usually incidental findings in patients presenting with other ailments and show classical imaging findings in cross-sectional studies. Both CT and MRI are crucial to demonstrate central fatty and peripheral calcific components as approximately half of these lesions contain a bony spherule with central marrow space. This is an important differentiating feature of intracranial lipomas and is uncommonly seen in cases of peripheral lipomas. Another critical feature demonstrated on imaging (mostly on CT) is the pattern of calcification as extra-cranial lipomas show amorphous, punctate calcification rather than peripheral, rim-like calcification. Intracranial osteolipomas are rare and seldom reported so limited literature is available [2].
These lesions are important to identify as they are often asymptomatic and inadvertent removal will lead to nonresolution of symptoms. Adequate preoperative workup should be accomplished whenever there is suspicion of osteolipomas in initial imaging to guide the suitable therapy [2].
Case report
A 45-year-old male, a suspected case of schizophrenia was referred for an MRI brain. The patient had complaints of sleeplessness, auditory hallucinations, the delusion of persecution, and emotional liability for 2 months which are classical symptoms of schizophrenia, however, clinicians were doubtful and wanted to exclude organic brain lesions. Family history and history of trauma to head was nil. The Lab reports show mild microcytic hypochromic anemia (possibly due to poor nutrition).
The patient underwent an MRI initially which revealed an intra-axial lesion on the right side of tubercinerium with suspicious findings of osteolipoma. The need for further imaging with CT is conveyed to the clinician, meanwhile, the patient was initiated on drug therapy for schizophrenia. One week later, a CT head was obtained which supported the findings of osteolipoma depicting the fatty lesion with an incomplete, thin rim of hyperdensity, HU matching for calcification.
The patient continued medical treatment with a good response, which suggested osteolipoma was an incidental lesion, that mimicked a primary brain lesion.
Imaging findings
MRI brain findings
-
•
T1 sagittal images show a well-defined hyper-intense lesion of approximate size 4.7 × 4.9 mm tubercinereum anterior to the right maxillary body.
-
•
T2 and FLAIR axial images show similar hyper-intense lesions suggestive of fatty lesions or subacute hemorrhage.
-
•
The lesion shows a central signal drop on 3D T1 fat sat images confirming the central fat-containing lesion.
-
•
On gradient recalled echo (GRE) peripheral blooming artefact was seen suggestive of either calcification or hemorrhage.
-
•
No evidence of diffusion-weighted imaging (DWI) restriction was seen.
To differentiate the calcification from hemorrhage, a CT head was obtained 1 week later which showed-
-
•
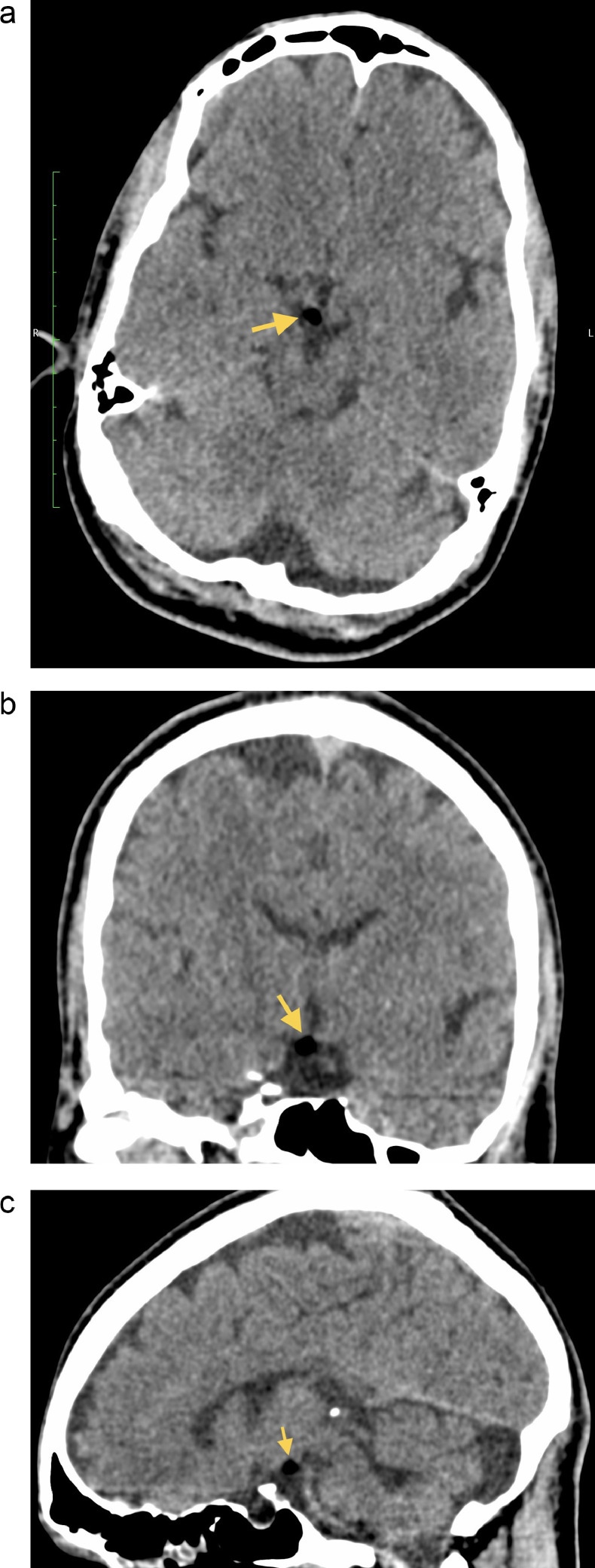
Brain windows (axial, coronal and sagittal sections) show a predominant fatty lesion with HU values ranging from -120 to -60.
-
•
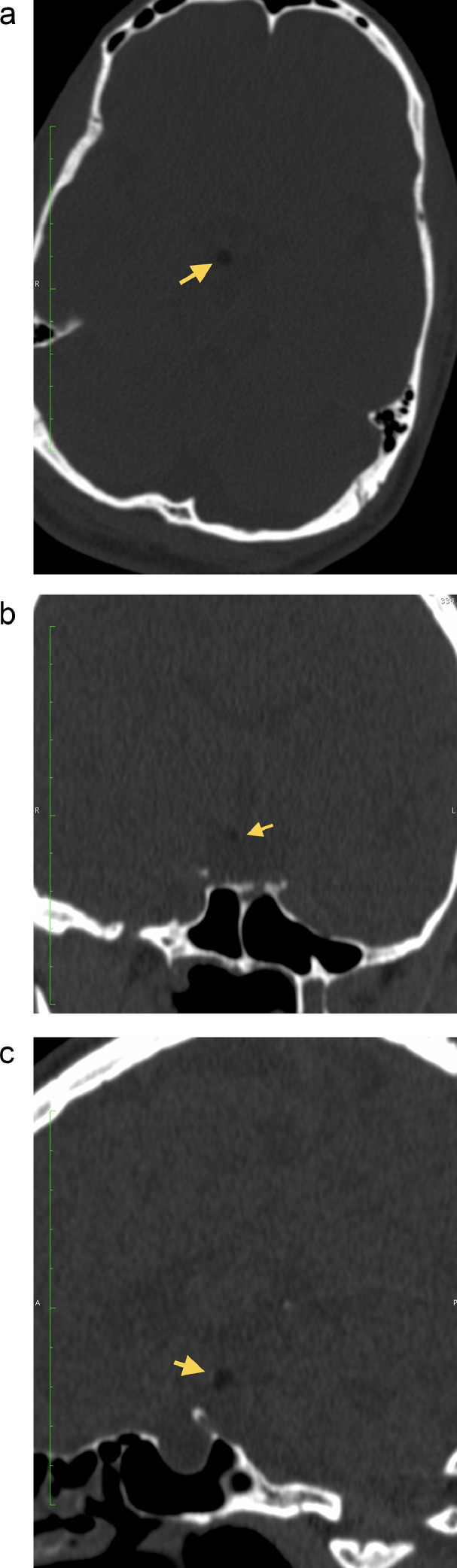
Bony Window (axial, coronal and sagittal sections) demonstrate a thin, incomplete rim of calcification with HU ranging from 70 to 111.
-
•
These findings strongly suggested the diagnosis of osteolipoma. The treating physician believed that the presence of intracranial osteolipoma was purely incidental and kept the patient under observation while continuing drug therapy for schizophrenia. On follow up patient responded well in terms of control of symptoms. This improvement in the patient's clinical condition established osteolipoma as an incidental lesion not contributing to the patient's symptoms. See Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7.
Fig. 1.
T1 sag image shows a small, rounded, well defined hyperintense lesion involving tubercinerium.
Fig. 2.
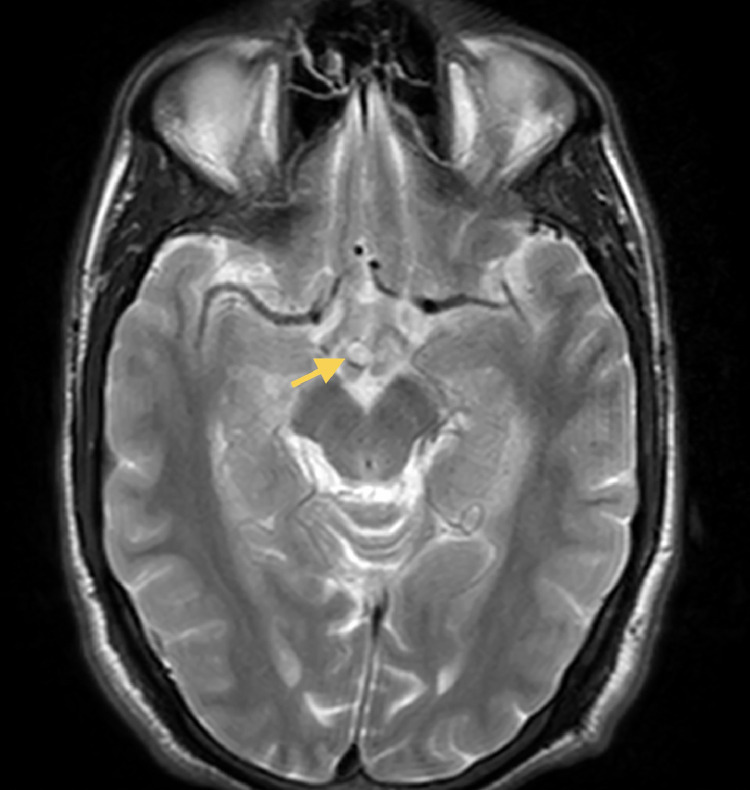
T2 axial image shows a relatively well-defined hyperintense lesion in the tubercinerium anterior to the right mammillary body.
Fig. 3.
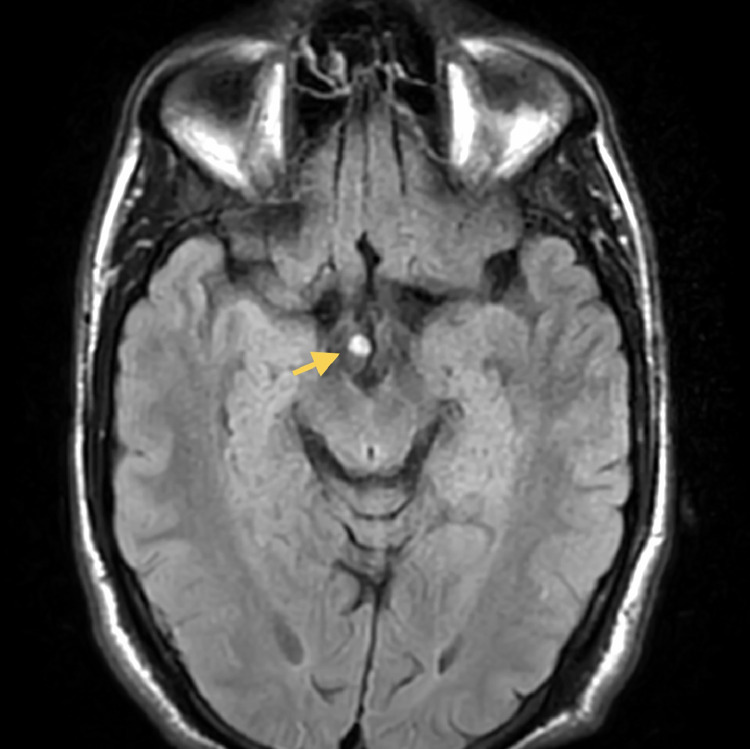
FLAIR axial image shows a hyperintense lesion in the tubercinerium anterior to the right mamillary body.
Fig. 4.
Axial gradient recalled echo image shows peripheral signal loss with blooming artefact in the lesion.
Fig. 5.
(A) 3D T1 axial sequence showing central suppression of signals. (B) 3D T1 coronal sequence showing central suppression of signals. (C) 3D T1 sagittal sequence showing central suppression of signals.
Fig. 6.
(A) Plain CT head axial section (brain window) shows a well-demarcated fatty intensity lesion in tubercinerium. (B) Plain CT head coronal section (brain window) shows a well-demarcated fatty intensity lesion (yellow arrow) in the tubercinerium. (C) Plain CT head sagittal section (brain window) shows a well-demarcated fatty intensity lesion (yellow arrow) in the tubercinerium.
Fig. 7.
(A) Plain CT head axial section (bone window) shows a well-demarcated fatty intensity lesion in the tubercinerium. (B) Plain CT head coronal section (bone window) shows a well-demarcated fatty intensity lesion (yellow arrow) in tubercinerium with a thin rim of calcification in the left superolateral aspect of the lesion. (HU ranging from 70-111). (C) Plain CT head sagittal section (bone window) shows a well-demarcated fatty intensity lesion (yellow arrow) in tubercinerium with a thin rim of calcification in the antero-superior aspect of the lesion (HU ranging from 70-111).
Discussion
OSTEOLIPOMA of tubercinerium are traditionally considered meningeal lipomas with remarkable consistency in their size and location, that is, found between corpora mammillaria and pituitary stalk (Supratentorial) [2]. These tumors are rare, benign intracranial lesions that are usually asymptomatic and have an indolent course [3]. These tumors are considered congenital malformations as they are neither hamartomas nor true neoplasms [4]. These intracranial lesions are seen in a suprasellar and interpeduncular cistern, close to the pituitary infundibulum, inferior surface of the hypothalamus, mammillary bodies and tubercinerium [5]. Extracranial location may include the submandibular region, tongue, subcutaneous region of the chest wall, and scapular and mandibular region. Cross-sectional imaging confirms the diagnosis by demonstrating typical imaging findings of central fatty and peripheral bony/calcific components.
CT/MRI by showing both fatty as well as bony/calcific component are invaluable for preoperative evaluation and excluding the other intracranial lesion related to neurological symptoms. T1 weighted sequence demonstrates hyperintense lesion with signal dropout on fat suppression sequences in central fat-containing areas is classical. GRE images show blooming artefact due to peripherally calcified rim. These lesions usually do not enhance on contrast-enhanced images which differentiates them from other tumors [5] such as teratomas and craniopharyngiomas. CT shows a rounded lesion containing fat and calcification. These lesions have a similar prognosis as a simple lipoma and asymptomatic cases do not require any treatment [5,6].
Differential diagnoses include other fat-containing lesions such as simple lipoma, teratoma and dermoid. The lesion which contains bone includes dermoid and chondroid lipoma. Another lesion that constitutes an important differential in this region is craniopharyngioma [7]. Simple lipoma is characterized as a discrete, encapsulated, homogenous fatty mass with a similar signal intensity of the subcutaneous plane in all pulse sequences. Teratomas are heterogenous masses on imaging with bony, hair and sebaceous components. T1 and T2 weighted MRI show heterogeneous signals because of differing components. On CT Calcification is more solid and clump-like. These lesions usually enhance because of soft tissue components. Alfa fetoprotein (AFP) and carcino-embryogenic antigen (CEA) may be elevated in some cases. Dermoids are well-defined T1 hyper-intense, midline lesions with T2 variable signals, they do not enhance on contrast-enhanced scans [5]. CT shows mixed, fat-density lesions with no significant contrast enhancement. Craniopharyngiomas are mostly hyperintense on T2-weighted sequences with variable signals on T1-weighted sequences. Many of these lesions strongly enhance on contrast-enhanced scans. Chondroid lipoma show variable degree of T1 and T2 weighted signal intensity due to variable fat contents. Cartilaginous components show high signals on T2 fat sat images. Areas of calcification will show hypo-intensity in all sequences. CT shows fatty density lesion with internal areas of calcification of cartilaginous tissue. Fat may not be readily identifiable [7].
Other lesions such as tumor calcinosis, ossifying fibromyalgia, hemangioma, calcified bursa, and myosotis ossificans should also be considered for extracranial osteolipomas [8].
Conclusion
Intracranial osteolipomas are benign findings; however, a radiologist must be aware of typical location, size and imaging findings as these lesions form a close differential with other fat-containing intracranial neoplasms such as dermoid and teratomas, which require prompt treatment. These lesions impose a challenge in clinical diagnosis when present concurrently with other neurological/psychosomatic disorders. In these equivocal cases, it is difficult to evaluate whether this lesion is incidental or a primary source of the patient's symptoms. Inadvertent Surgical removal of this lesion may lead to an increased incidence of postsurgical complications as well as non-resolution of patients' symptoms. In these cases wait and wait-and-watch regimen with continued medical therapy of concurrent disease may prove beneficial to decide the correct therapy. This case highlights the importance of a combination of imaging to confirm the diagnosis as well as the critical role of follow-up in confirming the source of patients' symptoms and guiding the appropriate therapy.
Patient consent
The patient was informed and written consent for publication was obtained.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Nebi Y, Ozkan U, Nejmi K, Cahide Y, Omer E. Intracranial lipoma clinical study. J Clin Neurol Neurosurg. 2006;108(4):363–368. doi: 10.1016/j.clineuro.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Friede RL. Osteolipomas of the tuber cinereum. Arch Pathol Lab Med. 1977;101(7):369–372. [PubMed] [Google Scholar]
- 3.Kalakoti P, Osama A, Jamie A, Jacobsohn JA, Nanda A. Symptomatic osteolipoma of the tuber cinereum masquerading as calcified retroclival mass. J Clin Neurosci. 2015;22(6):1045–1051. doi: 10.1016/j.jocn.2014.11.038. [DOI] [PubMed] [Google Scholar]
- 4.Wittig H, Kasper U, Warich-Kirches M, Dietzmann K, Roessner A. Hypothalamic osteolipoma: a case report. Gen Diagn Pathol. 1997;142(5–6):361–364. [PubMed] [Google Scholar]
- 5.Gaillard F., Sharma R., Osteolipoma. Radiopedia.org. doi: 10.53347/rod-70454. [DOI]
- 6.Nishio J., Ideta S, Iwasaki H, Naito M. Scapular osteochondrolipoma: imaging features with pathological correlation. Oncol Lett. 2013;6:817–820. doi: 10.3892/ol.2013.1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skalski M., Gaillard F., Knipe H, et al. Chondroid lipoma. Radiopedia.org. doi: 10.53347/rlD-343134. [DOI]
- 8.Durmaz A, Fuat T, Bulent K, Mustafa G, Hakan B. Osteolipoma of the nasopharynx. J Craniofac Surg. 2007;18(5):1176–1179. doi: 10.1097/scs.0b013e31814b2b61. [DOI] [PubMed] [Google Scholar]