Abstract
A 23 year old young lady was admitted for Ayurveda treatments of her refractive error coupled with migraine. She was put on Shadbindu Taila Nasya, 24 drops in both her nostrils immediately the next day. Within 6 h of performing Nasya, the patient started developing pyrexia which was initially of low grade, and later, within 6 h, went on to high-grade. Nasya was suspended, and rescue Ayurveda medicines were started but had no improvement. The patient later self-medicated an antipyretic drug, and with a single dose, the high-grade pyrexia came down to normal. Naranjo adverse drug reaction probability scale recording gave a score of six, which shows that the AE could be probably due to Nasya with Shadbindu Taila. This case report adds evidence to the medical database of under-reported/poorly reported adverse effects (AE) cases of Nasya therapy. It shows that Nasya is not a 100 % complication and adverse effect free treatment, but rather has to be done with extreme caution. This case report highlights that effective Ayurveda principle based preparatory treatments are also to be done before initiating Nasya to minimize the chances of adverse effects. This case report also suggests practicing a test dose of Nasya, before initiating a high dose, so as to detect adverse events and prevent severe complications.
Keywords: Adverse effect, Ayurveda, Nasya, Migraine, Pyrexia, Refractive error, Shadbindu Taila
1. Introduction
Nasya is one among the Panchakarma (∼five purificatory treatments), with special importance in diseases of Shalakya Tantra (∼one of the eight branches of Ayurveda that deal with diseases of eyes, ear, nose, throat, and head). Nasya is one of the common modalities of treatment adopted for refractive error [1] and migraine [2]. Migraine is usually associated with refractive error [3]. Shadbindu Taila and Anu Taila are the drugs that are used commonly in clinical practice for Nasya in the above conditions. Till date any detailed published literature on the complication of Nasya is not available in the medical database, except that of Krishna Kumar V et al., who had reported an event of a short-lasting unilateral neuralgiform headache attack with conjunctival injection and tearing (SUNCT) following Virechanika Nasya in Ménière's disease [4]. Hence, it is believed to be safe and without adverse effects (AE) and complications. We demonstrate the AE of Nasya with Shadbindu Taila in a patient of refractive error coupled with migraine. This case report has been written in accordance with the CARE guidelines [5].
1.1. Case presentation
A 23-year-old young lady was admitted for Ayurveda treatments on account of her refractive error coupled with migraine for 6 years. She was using spectacles and her best corrected visual acuity was 6/6 (RE) and 6/6 (LE) [Snellen's chart]. Complaints initially started with migraine at the age of 13 years, and later from 17 years of age, she noticed defective vision in her both eyes. She consulted an ophthalmologist when she was of 19 years and was put on spectacles. Migraine headache was severe, pulsating in nature, and concentrated on the frontal and temporal region. It did not have any typical periodicity. She had associated heaviness of head just before initiation of the migraine. Her menstrual cycle was regular with normal bleeding, and was on Thyroxine 75 mcg since her 13th year of age. She had come here for Ayurveda treatment of refractive error and migraine.
1.2. On examination
On the day of admission, she was afebrile (98.6 °F); BMI was 16.9 kg/m2 (was underweight); appetite, bowel, bladder, and sleep were normal. Unaided visual acuity was 6/24 (Snellen's Chart) in both eyes. Headache was present without any PNS tenderness.
After analyzing the symptoms in accordance with Ayurveda, the disease was diagnosed as shirashula added on with its complication of involvement of eyes. Since there was no laterality in headache or any definitive period in recurrence, ardhavabhedaka was excluded. The presence of heaviness of the head (moordhno guru) just before initiation of headache, showed the involvement of kapha. Presence of severe, pulsating type of headache concentrated over the frontal and temporal area (nistudyate bhrisham shankhau … bhruvormadhyam lalatam cha … sphuratyati), involvement of eye as a complication (atrivruddhastu … nayanam va vinashayet – here it manifested as timira (refractive error)) showed the predominance of vata [6]. [Uttara Sthana; shirorogavijnaneeyam adhyayam: Chapter 23 verse 1–11]. Hence, the disease could be diagnosed as vata-pradhana-kapha-anubandha shirashula, and is a sadhyavyadhi (treatable disease).
The choice of treatment for heaviness of head (shirogaurava), headache (shiroruk), removal of any kapha involvement in shiras (shleshma hara), bringing clarity to sense organs (indriyabodhana), was to administer virechana nasya [6]. [Chikitsa Sthana; jvarachikitsita adhyayam: Chapter 01 verse 125-6] Since the disease had predominance of vata, snigdha nasya was to be done [6]. [Uttara Sthana; shirorogapratishedham adhyayam: Chapter 24 verse 4] Hence, snigdha nasya with virechana property having specific action on shiras and netra (eyes), here Shadbindu Taila, was selected. It was greeshma ritu (∼summer) and her bala (∼physical strength) was madhyama. She was of vata-pitta prakriti, and with madhyama satva.
1.3. Treatments adopted
As soon as the patient was admitted on 25.03.2023, she was advised to refrain from the asta-mahadosha-kara bhava to prevent complications arising out from the panchakarma treatments [7]. [Siddhi Sthana; Uttaravasti Siddhi adhyayam: Chapter 12 verse 11-2] The very next day the following treatments were administered to the patient: (a) Marsha nasya with Shadbindu Taila 24 drops in each nostril two times daily; (b)Mukha abhyanga (∼Oil massage of face) with Asanavilwadi Taila; (c)Dhoomapana (∼inhalation of medicated smoke) with Kaishora Guggulu Varti; and (d) Thalam (∼local poultice on vertex of head) with Rasnadi Choorna mixed with Asanavilwadi Taila. [See supplementary file 1 for the standard operating procedures (SOP) followed]. Orally Pathya Shadanga Kwatha 60 ml bid before food, Ksheera Bala Taila (14 Avarti) 10 drops with kwatha, Ashta Churna 1 tsp with Mahatraiphala Ghrita along with the first morsel of food in the morning and two tablets of Saptamrita Lauha at bedtime after food. References of these medicines have been given in supplementary file 2.
1.4. Timeline of clinical observations
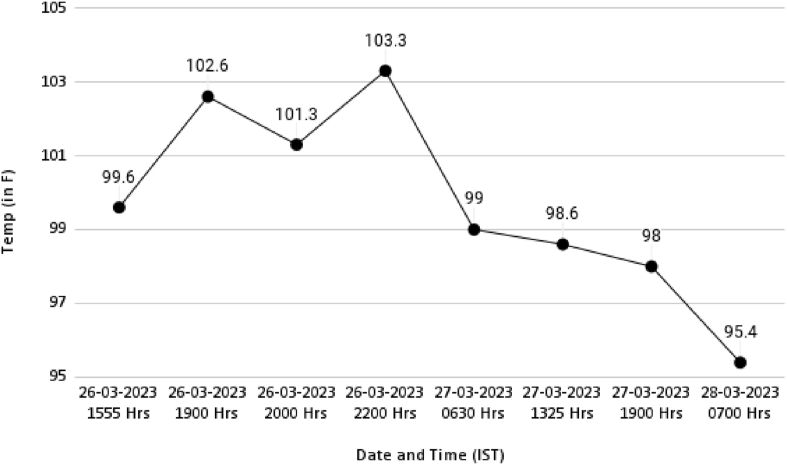
Within 6 h of the first dose of nasya therapy in the morning, the patient started developing pyrexia. Initially, the pyrexia was low-grade. Then as time progressed, it started to increase in intensity finally reaching high grade fever at 2200 h on 26.03.2023 (See Fig. 1). There was associated myalgia, heaviness of the head and body, but PNS tenderness was negative. Rhinorrhoea, sneezing, nasal obstruction, and rashes on the face, and body were absent. There were no bleeding abnormalities. Her appetite was poor.
Fig. 1.
Shows the plotting of temperature versus date and time chart, where date with time is on X-Axis and temperature is on Y-Axis.
1.5. Therapeutic interventions
As soon as she started developing fever, all her treatments and internal medicines prescribed were suspended and therapeutic interventions were started as shown in Table 1. She was advised to have only Ganji (∼rice gruel). Despite initiating these medications, her pyrexia did not come down (See Fig. 1). On the same day (26.03.2023), by about 2230 h, the patient self-medicated a single dose of an antipyretic medicine (Paracetamol), after which her temperature started coming down to normal the next day (27.03.2023) by 1325 h. Myalgia and the heaviness of head and body were reduced but were present, and hence the same medicines, as in Table 1 were continued, and all other treatments were stopped. Her temperature became totally normal by evening of 27.03.2023. On 28.03.2023, the temperature went to subnormal state of 95.4 °F and Vettumaran Gulika 1 BID was replaced with Ayush 64 Tablets 2 BID. As the patient was willing to continue her treatments for refractive error and migraine, its further management was reinstated.
Table 1.
Showing the timeline of medical management of adverse drug reactions (ADR) and its effect.
| Date and Event | Clinical status | Medicines given | Remarks |
|---|---|---|---|
| 26.03.2023 | Patient developed pyrexia post nasya. Patient developed myalgia, heaviness of head and body and poor appetite. | AmruthotharamKwatha (AK) 60 ml BID, Vettumaran Gulika (VG) 1 nos BID, Thalam with RasnadiChurna and JambeeraSwarasa (∼juice of lemon) (RJT) | All treatments and previous internal medicines were suspended. No reduction in pyrexia even after administration of 120 ml of AK, 2 VG, and RJT by 10 p.m. Patient self-medicated Paracetamol. |
| 27.03.2023 | Temperature, myalgia, heaviness of head and body reduced. Temperature came to normal by 13.25 h and continued to be normal. Appetite improved, but was not good, bowels were not good. | AmruthotharamKwatha (AK) 60 ml QID, Vettumaran Gulika (VG) 1 nos BID, Thalam with RasnadiChurna and JambeeraSwarasa (∼juice of lemon) (RJT) | AK was increased to QID and rest was continued as on 26.03.2023. |
| 28.03.2023 | Temperature came subnormal by 07.00 h. No myalgia, and heaviness of head. Good appetite and bowels were clear. | AmruthotharamKwatha (AK) 60 ml QID, Ayush-64 2nos BID | VG was replaced with Ayush 64. AK was continued. Dhoomapana with KaishoraGugguluVarti two times was continued. Other Eye related treatments like Anjana, Padabhyanga, and Kabala was initiated. |
2. Discussion
The case report demonstrates that nasya procedure is not a 100 % complication and adverse-effect free procedure. It should always be done with extreme caution. It can be noted that during admission the koshta (∼gastrointestinal tract system complex) of the patient was good (as she was afebrile) Dosha analysis showed the predominance of vata, associated with kapha (shiras being the kapha sthana, vata being the vitiated dosha), prakriti was vata-pitta predominant. The least matra (∼dose) for doing marsha nasya is six bindu (∼3 ml) [6]. [Sutra Sthana; Nasyavidhi: Chapter 20 verse 10–11] One bindu is equal to 0.5 ml [8] and one drop from a dropper bottle is 0.05 ml [9]. Hence, here 1.2 ml (24 × 0.05 ml) was dropped into each nostril, which is still less than the least dosage.
Two times nasya is mentioned in conditions where vata gets vitiated in shiras [6].[Sutra Sthana; Nasyavidhi: Chapter 20 verse 15–16] Here, vata kopa in shiras and eyes was the hypothesized pathophysiology for refractive error and migraine. Tagara (Valeriana wallichii DC.), Shatahva (Anethum sowa Roxb.), Rasna (Alpinia galanga Swartz), Vidanga (Embelia ribes Burm. f.), Shunthi (Zingiber officinale Roscoe.), and Saindhava Lavana (Rock salt) present in Shadbindu Taila reduces kapha. The sesame oil base pacifies vata. Based on the description of the efficacy of the medicine available in Ayurveda literature, it has a specific target action towards the head and pathologies of sense organs, and hence was selected for nasya [10]. Shadbindu Taila [Batch No: 43-ATA-LDB-595 Exp date: 03/25] was procured from Indian Medicines Pharmaceutical Corporation Limited (IMPCL), a central public sector enterprise ISO 9001-2015 GMP certified company. Using other medicines of the same batch did not report any complications to date, and hence the possibility of having a batch defect is ruled out. Rasnadi Churna and Asana vilwadi Taila again reduce vata-kapha due to the properties of the ingredients. Dhoomapana (∼inhalation of medicated smoke) has a special affinity for vata-kapha diseases of the shiras and indriya [6]. [Sutra Sthana; Dhumapanavidhi: Chapter 21 verse 01]Evaluating the ingredients of Kaishora Guggulu it can be said that it is teekshna (∼potent), ushna (∼hot in nature), rakta prasadaka (∼satiating rakta) and kapha shamana (∼reduces kapha).
Internally, Pathya Shadanga Kwatha was given which has efficacy in diseases of shiras and eyes, as per Ayurveda literature. Ksheera Bala Taila (14 Avarti) was added to reduce the vata-pitta. Ashta Churna along with Mahatriphala Ghrita was given to increase the appetite, as per the classical literature and to get target-oriented action on the eyes. Saptamruta Lauha, again is a target-oriented drug for netra roga (∼eye diseases) [11]. Hence, all the medicines, in spite of good choices for the condition, resulted in high-grade pyrexia.
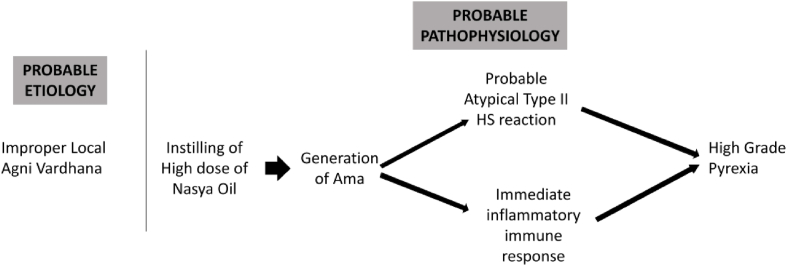
Naranjo adverse drug reaction probability scale [12] showed a score of six which gives a probable association of Nasya with Shadbindu Taila in generation of the AE. The high-grade pyrexia subsided with a single dose of antipyretic medicine and with the withdrawal of nasya therapy, thus ruling out the possibility of an iatrogenic infection. Since, there was no sinus tenderness, the possibility of sinusitis has been ruled out. Hence, this AE could be probably a hypersensitivity reaction. Type I hypersensitivity reaction has been ruled out as there was no cardio-vascular involvement. Type III hypersensitivity has been ruled out, as there was no chronic infection to bring persistent antigen nor there was any autoimmune history. Type IV hypersensitivity reaction is also ruled out, as it is a delayed reaction, while in this case, the reaction was immediate. Probably an atypical Type II reaction may have occurred without any bleeding disorder or rash. Hence, the active ingredients in the oil used for nasya may have induced an atypical Type II hypersensitivity reaction and/or immediate inflammatory immune response resulting in high grade pyrexia (See Fig. 2) [13]. Following could be the probable reasons for the generation of this response.
-
1.
Enough preparatory procedures before nasya were not performed. Localized agni vardhana and reduction of kapha, should have been performed. Even though Shadbindu Taila is a kapha shodhana medicine (by means of the properties of its drugs), which gives the effects of shiro virechana, the oil, and its ingredients by its nature would have contributed to the generation of hypersensitivity. Here, a special point to be highlighted is the principle of ‘Brumhyamstu mrudu langhayet.’ (∼do mild langhana before initiating brumhana therapy) [6]. [Sutra Sthana; Dvividhopakramaniya: Chapter 14 verse 15-6] Hence, before initiating nasya therapy, some form of rookshana therapy should have been performed to remove kapha, and to increase localized agni so as to negate the possible AE. Previous studies show that intra-nasal drug route medication transfers the medications across the blood brain barrier (BBB) [4]. As localized agni vardhana was not initiated, the active ingredients in the nasya oil may have crossed the BBB, resulting in the generation of ama (∼immune complexes), which would have triggered the atypical Type II HS reaction to result in high grade pyrexia (Fig. 2).
-
2.
Secondly, a test dose of the drug was not given. A test dose shall always reduce the possibility of an AE or a severe and systemic complication, even if the patient is prone to HS reaction. Hence, it is recommended that a test dose in the form of 2 drops (0.1 ml) or 4 drops (0.2 ml) of medicine may be initially instilled to confirm the absence of HS reaction, as a part of safer practice. Later, higher doses of medicine may be instilled, as per the condition of the patient. This may prove beneficial for the health and time of the patient.
Fig. 2.
Showing the probable etiology and pathophysiology of generation of high-grade pyrexia.
We hypothesize that this sudden pathophysiology shown in Table 1 was the reason for the non-response of the medicines. High grade pyrexia had come down to normal due to the antipyretic property of Paracetamol. But the presence of ama was evident from the presence of myalgia and heaviness of head and body, for which the same medicines were continued for achieving ama-pachana. When the temperature of the body became subnormal, it was inferred that ama-pachana had occurred, and to remove any sesha dosha (remnant dosha) in the koshta, Ayush 64 was administered. Ayush 64, a drug developed by Central Council for Research in Ayurvedic Sciences (CCRAS), has Kiratatikta (Picrorhiza kurroa Royle ex. Benth), Katurohini (Swertia chirata Pexbex. Karst), and Saptaparna (Alstonia scholaris R. Br.), and Kuberaksha (Caesalpinia crista L.) as its ingredients. This ingredient helps in preventing vishama jvara by removing the sesha dosha, and thus stopping the occurrence of dhatu leenagata avastha (doshas infusing in dhatus) [14].
We did not perform any blood analysis as the pyrexia dropped to normal, the very next day of taking a single dose of antipyretic. Hence, analysis of total count and differential count remains as a limitation of this case report.
3. Conclusion
Nasya is not a 100 % complication and AE free treatment. This case report highlights possibility of high-grade pyrexia as an uncommon adverse event following nasya therapy. AEs like high-grade pyrexia is possible if nasya is administered without proper preparatory treatments. There are possibilities of complications like infections, depending upon the immune status of the patient. This case also highlights the need for proper Ayurveda principles based examination to evaluate the status of agni and koshta, keep all the rescue medications ready for managing possible AE (as highlighted by Charaka in Upakalpaniyam Chapter of Sutra Sthana) [15], and need for integrated management during non-response to Ayurveda medicines. This case also highlights the need to having a test dose of a lesser amount of medicine, to check AE possibilities, even in patients in whom the proper preparatory treatments are completed. We also suggest documentation and publication of such cases of AE so that the scientific community can take necessary steps for its prevention.
3.1. Patient perspective
The patient said that she thought, Ayurveda treatments and nasya were safe and without complications. She felt a a bit anxious and tensed as her fever rose, despite the medicines given, and hence consumed paracetamol. She thought that this might trigger her headache but surprisingly, it did not. As the fever subsided, she was willing to continue Ayurveda treatments further for her migraine and refractive error.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Contribution
PB: Conceptualization; Visualization, Writing Original Draft, ES: Visualization, Review and Editing, LR: Visualization, Review and Editing.
Declaration of Generative AI and AI-assisted technologies in the writing process
The authors declare that no generative AI and AI-assisted technologies have been used in the writing process.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
We thank the Director General, CCRAS-New Delhi, Deputy Director General, CCRAS-New Delhi, and Assistant Director in Charge, CCRAS-Thiruvananthapuram for their constant motivation in doing research in Ayurveda.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jaim.2023.100812.
Appendix A. Supplementary data
The following are the Supplementary data to this article.
References
- 1.Gupta D.P., Rajagopala M., Dhiman K.S. A clinical study on Akshitarpana and combination of Akshitarpana with Nasya therapy in Timira with special reference to myopia. Ayu. 2010 Oct;31(4):473–477. doi: 10.4103/0974-8520.82045. PMID: 22048542; PMCID: PMC3202262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soman A., Venkatram S., Chikkanna U., Ramakrishna K.K., Bhargav H., Mailankody P., et al. Ayurveda for management of migraine: a narrative review of clinical evidence. J Family Med Prim Care. 2022 Aug;11(8):4228–4235. doi: 10.4103/jfmpc.jfmpc_2109_21. Epub 2022 Aug 30. PMID: 36352975; PMCID: PMC9638656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gunes A., Demirci S., Tok L., Tok O., Koyuncuoglu H., Yurekli V.A. Refractive errors in patients with migraine headache. Semin Ophthalmol. 2016;31(5):492–494. doi: 10.3109/08820538.2014.962177. Epub 2014 Nov 20. PMID: 25412330. [DOI] [PubMed] [Google Scholar]
- 4.Krishna Kumar V., Nair P.P., Sree Deepthi G.N., Pradeep Kumar P.P. A case report on probable short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing following vairechanika nasya in Ménière's disease. J Ayurveda Integr Med. 2022 Apr-Jun;13(2) doi: 10.1016/j.jaim.2021.10.004. Epub 2021 Dec 27. PMID: 34969589; PMCID: PMC8728096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riley D.S., Barber M.S., Kienle G.S., Aronson J.K., von Schoen-Angerer T., Tugwell P., et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017 Sep;89:218–235. doi: 10.1016/j.jclinepi.2017.04.026. Epub 2017 May 18. PMID: 28529185. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Ayurveda and Integrative Medicine (I-AIM) 2010. Astanga Hrudayam E-book. e-hrudayam - Institute of ayurveda and integrative medicine (I-AIM)http://vedotpatti.in/samhita/Vag/ehrudayam/?mod=read Available from. [Google Scholar]
- 7.National Institute of Indian Medical Heritage . Central Council for Research in Ayurvedic Sciences (CCRAS). 2010; 2010. Caraka Samhita E-book.http://niimh.nic.in/ebooks/ecaraka/ Available at: [Google Scholar]
- 8.Radhika C., Kumar G.V., Mihirjan K. A randomized controlled clinical trial to assess the efficacy of Nasya in reducing the signs and symptoms of cervical spondylosis. Ayu. 2012 Jan;33(1):73–77. doi: 10.4103/0974-8520.100316. PMID: 23049188; PMCID: PMC3456869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moore D.B., Beck J., Kryscio R.J. An objective assessment of the variability in number of drops per bottle of glaucoma medication. BMC Ophthalmol. 2017 May 22;17(1):78. doi: 10.1186/s12886-017-0473-8. PMID: 28532424; PMCID: PMC5441018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shailajan S., Menon S.N., Tiwari B.R., Singh A.S. Standardization of Shadbindu Taila: an ayurvedic oil based medicine. Ayu. 2013 Jan;34(1):103–107. doi: 10.4103/0974-8520.115442. PMID: 24049414; PMCID: PMC3764865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bansal C. Comparative study on the effect of Saptamrita Lauha and Yoga therapy in myopia. Ayu. 2014 Jan;35(1):22–27. doi: 10.4103/0974-8520.141904. PMID: 25364195; PMCID: PMC4213962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Naranjo C.A., Busto U., Sellers E.M., Sandor P., Ruiz I., Roberts E.A., et al. A method for estimating the probability of adverse drug reactions. Clin Pharacol Ther. 1981;30:239–245. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 13.Justiz Vaillant A.A., Vashisht R., Zito P.M. StatPearls Publishing; 2023 Jan. Immediate hypersensitivity reactions. [Updated 2023 Mar 7]. In: StatPearls [Internet]. Treasure Island (FL)https://www.ncbi.nlm.nih.gov/books/NBK513315 Available from. [PubMed] [Google Scholar]
- 14.Gundeti M.S., Bhurke L.W., Mundada P.S., Murudkar S., Surve A., Sharma R., et al. AYUSH 64, a polyherbal Ayurvedic formulation in Influenza-like illness - results of a pilot study. J Ayurveda Integr Med. 2022 Jan-Mar;13(1) doi: 10.1016/j.jaim.2020.05.010. Epub 2020 May 14. PMID: 33446377; PMCID: PMC8718941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shrivastav V.K., Srivastava A., Deole Y.S. In: Charak Samhita New edition. Mangalasseri P., Deole Y.S., Basisht G., editors. Jamnagar:CSRTSDC; 2020. Upakalpaniya Adhyaya; p. 17.https://www.carakasamhitaonline.com/index.php?title=Upakalpaniya_Adhyaya&oldid=42733 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.