Abstract
This study aimed to determine the optimal location of the iliac cortical window (ICW) for the direct reduction of acetabular dome impactions using a reference bony landmark.
Methods
In the first part of the study, computed tomography scans of 10 normal acetabula, the femoral head weight bearing area, were projected through the superior iliac cortical surface perpendicular to the plane of the true pelvis to show the area that corresponds to the acetabular dome. A line connecting each pair of anterior inferior iliac spines (AIIS) was drawn then reflected in the superior surface of the acetabulum and a reference point (RP) was marked on the line halfway between the AIIS and the pelvic brim. A 12-point 1-cm interval grid with horizontal and vertical axes labeled A, B, C and 1 to 4, respectively, overlying the acetabular surface projection was created to identify the location of the acetabular dome. In the second part of the study, the 12-point grid was marked on eight fresh cadavers (16 acetabula) and the same acetabular dome reference point was identified. K-wires were drilled into the acetabula using a parallel drill guide at each of the twelve grid points. An arthrotomy was carried out and the locations of the K-wires which penetrated the acetabular dome were recorded.
Results
The average distance from the AIIS to the medial pelvic brim in the CT scans and cadaveric study were 47.7 and 45.9 mm, respectively. The K-wires at grid points B2 and C1 had a 100% correlation to the dome area. The A2, B1, and C2 grid points had a correlation with the dome area of >80%. The remaining grid points had joint penetrations ranging from 6.25% to 62.5%.
Conclusion
The proposed RP, which can be easily identified intraoperatively, and the area 1 cm2 around the RP (except in the posterior direction) can be used as reliable reference landmarks and for identification of the location of the ICW for the reduction of an acetabular dome impaction.
Keywords: Iliac cortical window, Dome impaction, Acetabular fracture, Reduction
1. Introduction
The incidence of acetabular fractures in the elderly is rising, often resulting from low-energy trauma such as a fall from standing height onto the greater trochanter and is often associated with osteoporosis.1,2 The majority of fracture patterns in this age group involve predominantly either the anterior column or the anterior column with posterior hemitransverse, and are associated with both anterior and posterior column injuries.3,4 The injuries often result in the involvement of the anterior column with medial displacement of the femoral head, causing medial displacement of the quadrilateral surface and superomedial acetabular dome impaction. Failure to anatomically reduce dome impactions, described by Anglen et al. as the “Gull wing sign”, leads to very poor radiographic and clinical outcomes.5 Various surgical techniques to reduce dome impactions have been described.6
Anatomical reduction and stable fixation of acetabular dome impaction results in early mobilization and provides good clinical outcomes. Most acetabular dome injuries require surgical fixation using anterior approaches. The classic ilioinguinal approach developed by Letournel and Judet7,8 has been used as the main surgical approach for open reduction and internal fixation of acetabulum fractures with excellent results. Cole and Bolhofner9 described the use of a modified Stoppa limited intrapelvic approach for the treatment of acetabulum fractures that involve the anterior column which has become increasingly popular among surgeons.10 Both the ilioinguinal approach and the modified Stoppa intrapelvic approach are currently used to treat these difficult fractures with the reduction done through the quadrilateral fragment or the anterior column fracture.11,12 The major limitations of these approaches are the inability to directly visualize the joint or articular surface and that the reduction of the dome fragment while the quadrilateral fragment or anterior column is displaced is challenging. Moreover, when the displaced impacted superior dome is not connected to the primary fracture fragment, reduction through the fracture is usually not possible. Keel et al.13,14 described the pararectus approach to reduce the anterior column and quadrilateral plate. With that approach, the dome impaction fragment is reduced through a small window on the pelvic brim using a periosteal elevator and is filled with allograft. A supra-acetabular screw is inserted to support the reduction of the dome fragment. For cases where the dome impaction fragment is not accessible through the fracture, Scolaro and Routt15 proposed an alternative technique involving opening an independent iliac cortical window (ICW). The cortical window is made superior to the acetabular dome impaction, and a spike pusher or bone tamp is used to reduce the impacted articular fragment. To the best of our knowledge, the location of this ICW has not been described in the literature. Our study aimed to determine the optimal location of the ICW for the reduction of acetabular dome impactions using an intraoperative reference bony landmark.
2. Materials and methods
This two-part study consisted of simulation using tomography (CT) followed by a cadaveric study. The study protocol was reviewed, and approved by the Institutional Review Board, IRB REC No.58-252-11-1(6).
Our proposed “Reference Point” (RP) identifying the location of the ICW was determined by drawing an imaginary line connecting the two anteroinferior iliac spines (AIIS) and reflecting it on the superior cortical surface of the acetabulum. The midpoint between the cortical surface of the AIIS and the medial part of the pelvic brim was marked as the RP (Fig. 1).
Fig. 1.
An imaginary line (thick dash line) connecting both AIISs was drawn and reflected (thin dash line) on the superior cortical surface of the pelvis. The Reference Point (RP, x) was marked at the midpoint from AIIS to the medial pelvic brim.
The objective of the first part of the study was to identify the iliac cortical surface that covers the acetabular dome. The image reconstructions (MIMICS and Imageware software) from 10 CT scans of intact cadavers with no history of trauma were used to simulate the pilot experiment. A line connecting both AIIS was created then reflected on the superior cortical surface of the acetabulum. An RP was marked as previous described. A 12-point 1-cm grid was created with the horizontal axis lines labeled as A, B, and C and the vertical axis lines labeled as 1, 2, 3, and 4. The grid point B2 was placed over the RP, overlying the superior cortical surface of the acetabulum (Fig. 2A). Image reconstruction software retrieved the data of the femoral head corresponding to the acetabular socket as a sphere and projected this area superiorly through the iliac cortical surface above the acetabulum perpendicular to the plane of the true pelvis. This area represented the acetabular dome lying underneath (Fig. 2B). The overlapping area between the grid and the area corresponding to the femoral head projection was recorded (Fig. 2C).
Fig. 2.
Demonstration of the method to locate the bony landmark in relation to the femoral head
a) A 12-point grid with 1 cm spacing was drawn across the iliac cortical surface to locate the B2 at the RP
b) The image reconstruction software projected the femoral head upward perpendicular to the plane of the true pelvis on the iliac cortical surface
c) The overlap area of the grid and the femoral head projection represents the area that overlays the femoral head.
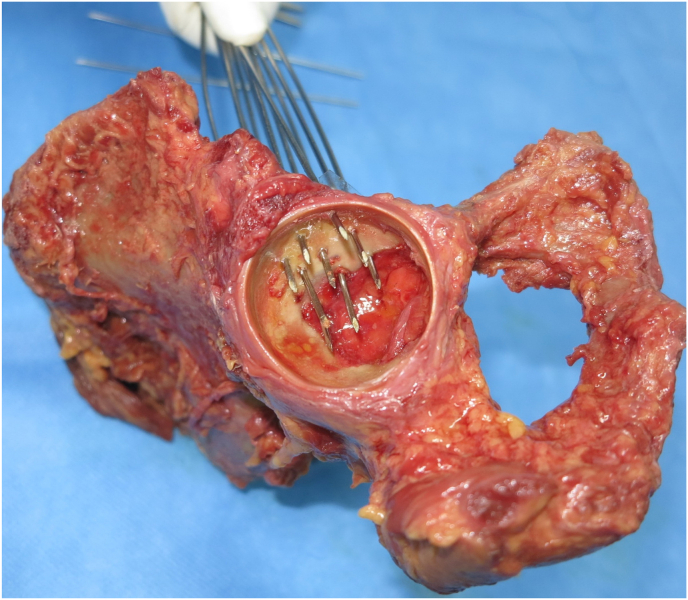
In the second part of the study, eight fresh cadavers (16 acetabula) with no history of trauma were dissected using an ilioinguinal approach to expose the superior cortical surface of the acetabulum. The RP and the grid were marked on the superior cortical surface as previously described. The first Kirchner wire was drilled through the RP perpendicular to the plane of the true pelvis (Fig. 3A and B) and additional wires were drilled through the remaining points of the grid marked as in the image reconstruction study using a parallel drill guide with the first wire as a reference (Fig. 3C). After all twelve wires had been drilled, arthrotomies and removal of the femoral head were accomplished. The location of the K wires that penetrated into the joint was recorded (Fig. 4). The data from both the first and second parts of the study was used to map the area corresponding to the acetabular dome underneath.
Fig. 3.
a) Plastic bone model illustrates where the first K wire was drilled at the RP perpendicular to the plane of the true pelvis b) The first K wire was drilled at the RP via the ilioinguinal approach c) The rest of the K wires were drilled on the grid points using a parallel drill guide.
Fig. 4.
The K wires from the RP and the grid which penetrated into the joint.
3. Results
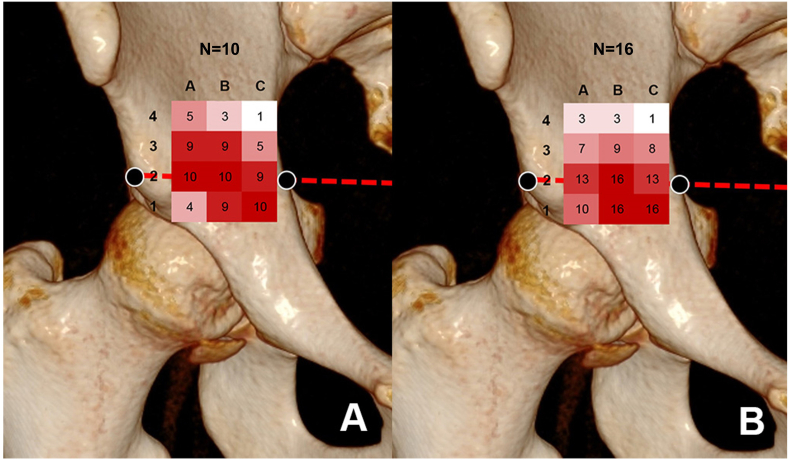
There were 5 males and 5 females in the CT data group and 4 males and 4 females in the cadaveric group, with an average age of 47.4 years and an average height of 171.5 cm in males and 157.6 cm in females. The average distance from AIIS to the medial pelvic brim in the CT data and the cadaveric study was 47.7 and 45.9 mm, respectively. From the CT image reconstruction study, 100% of the points A2, B2, and C1 were in the area of the femoral head projection. Of the femoral head projection of the points B1, C2, A3, and B3, 90% were in that area. Of the remaining five points, 10%–50% were in the projected area (Table 1) (Fig. 5).
Table 1.
Demonstration of the reference point in relation to the femoral head area.
| CT reconstruction study (N = 10) |
Cadaveric study (N = 16) |
|||||
|---|---|---|---|---|---|---|
| Grid | A | B | C | A | B | C |
| 4 | 5 (50%) | 3 (30%) | 1 (10%) | 3 (18.8%) | 3 (18.8%) | 1 (6.3%) |
| 3 | 9 (90%) | 9 (90%) | 5 (50%) | 7 (43.8%) | 9 (56.3%) | 8 (50%) |
| 2 | 10 (100%) | 10 (100%) | 9 (90%) | 13 (81.2%) | 16 (100%) | 13 (81.3%) |
| 1 | 4 (40%) | 9 (90%) | 10 (100%) | 10 (62.5%) | 16 (100%) | 16 (100%) |
Fig. 5.
Demonstration of the reference point in relation to the femoral head area.
a) The number and opacity of the red color in the grids represented the femoral head projection of the dome in the CT scan
b) The number and opacity of the red color in the grids represented the K wires which penetrate into the hip joint.
In the cadaveric dissection, the K-wires at B2, B1, and C1 had 100% joint penetration and the K-wires at A2 and C2 had 81.25% joint penetration. The joint penetration of the rest of the K-wires ranged from 6.25% to 62.5%. The arthrotomy found that all the K-wires penetrated into the joint at the superomedial dome area.
Analysis of the data from both parts of the study found that the grid points B2 and C1 had a 100% correlation to the dome area and the A2, C2, and B1 grid points had a correlation with the dome area of more than 80% (Table 1) (Fig. 5).
4. Discussion
Anatomic reduction and stable fixation is the goal of operative fixation for displaced acetabular fractures because it has been shown to improve function and to decrease the rate of posttraumatic osteoarthritis.16 Acetabular dome impactions are still challenging to manage and are associated with poor outcomes. Obtaining anatomical reduction can be difficult, and the results of surgical fixation are unpredictable. Due to the uncertain success with anatomical reduction, total hip replacement has been suggested as a treatment option in elderly patients with acetabular fractures with severe articular involvement.17
Various techniques have been proposed to surgically address these acetabular dome impaction in elderly patients. Laflamme et al.11 demonstrated a technique utilizing the anterior intrapelvic approach (AIP) to obtain direct reduction of the impacted fragments through the fracture by mobilizing the quadrilateral fragment in 9 patients. With that technique, voids were filled with grafts or bone substitute, and fixed with 3.5 mm cortical screws in the subchondral bone directly over the Gull fragment. The overall conversion rate to total hip replacement (THR) was 33%, and the average Harris Hip Score was 81. Archdeacon et al.18 used the AIP approach to access the impacted subchondral bone through the anterior column fracture line or with an osteotomy of the anterior column in 26 patients with a mean age of 74 years. The reduced dome fragment was stabilized with a medial to lateral buttress screw to prevent subsequent displacement, and an infrapectineal plate was used to buttress the quadrilateral plate. The follow-up radiographs at 12 months were graded as excellent or good in 69% of cases according to the Matta criteria, and the average modified Merle d'Aubigné score for clinical outcomes was excellent, very good, or good in 80%. Both techniques rely on the reduction of the displaced femoral head to its anatomical position by traction and reduction of the anterior column or the main articular fragment, followed by the reduction of the impacted articular fragment through the fracture gap using the reduced femoral head as a template. These techniques can have some limitations. For example, access to the dome impaction via the fracture displacement may be impossible in some cases due to an incomplete fracture or a fracture pattern which does not provide adequate visualization of the depressed fragment, or if the impacted fragment is not connected to the main fracture line. Second, in some cases the reduction of some osteoarticular fragments and the maintenance of the reduction is not possible. Additionally, it is often not possible to achieve containment of void fillers without the reduction of the displaced column or quadrilateral plate.
Keel et al.13,14 described a method for treating acetabular fractures using the pararectus approach to reduce the anterior column and quadrilateral plate. With that method, the dome impaction fragment is reduced through an isolated window on the pelvic brim. Sclolaro et al.15 recommend a technique for the reduction of osteoarticular dome impaction through an ICW from the lateral window of the ilioinguinal approach. This technique can be used when the area of impaction cannot be reduced through fracture displacement and is done after reduction of other components of the fracture. Both of these techniques use the opening of the iliac cortical window to reduce the dome impaction from the cephalad direction and use the reduced femoral head as a template. Identification of the location of the ICW using intraoperative fluoroscopy and direct opening according to the image, as has been done in many types of intraarticular fractures, e.g., tibial plateau depression fractures, may look simple. However, the anatomy of the acetabulum is complex and the surgeon has to plan in three dimensions. The AP x-ray only identifies the location of the fracture in the sagittal plane; however, the location in the coronal and transverse planes have to be correctly identified as well. We propose creating a simple anatomical landmark by first drawing a line for the axis of the pelvis using both AIIS and reflecting on the cortical surface over the acetabulum. Secondly, we identified the AIIS as the lateral landmark and the pelvic brim on this line as the medial landmark and found the midpoint, described as the RP. Thirdly, the plane of the true pelvis can then be used to set the direction of the software image projection of the dome on the iliac cortical surface and of the K wires which penetrate the joint. This provides guidelines in all three planes for the reduction of the articular impaction. In the majority of cases, the area of articular dome impaction is anteromedial. The fragment may be either free-floating hinged on the lateral articular surface.6 Careful evaluation of preoperative radiographs and CT scans must be done to determine the location and displacement of the articular dome impactions.
Our study found the location of the RP (B2) is simple to identify and should be an appropriate initial point of reference. The cortical surface area at the RP (B2) and 1-cm anteromedial to the RP (C1) accurately identified the dome projection and resulted in correct joint penetration in 100% of the cases. The points 1-cm anterior (B1), 1-cm lateral (C2) and 1 cm medial (A2) to the RP also had a high percentage within the dome projection and had a joint penetration of 80–90%. The area 1-cm posterior, posteromedial, and posterolateral to the RP had an accuracy of the dome projection and joint penetration of 50–70%, while 2-cm posterior to this area had a low accuracy of 7–30%. This means that the 1-cm area around the RP, except in the posterior direction, corresponds to the dome of the acetabulum with 80–100% accuracy. Using the RP combined with careful preoperative planning and intraoperative imaging, can help the surgeon accurately locate the cortical window for the reduction of an osteoarticular dome impaction. After opening the ICW at the desired location, a bone impactor, or pusher should be positioned perpendicular to the plane of the true pelvis in order to create a direct impaction of the displaced fragment. This should be confirmed under intraoperative imaging for the most accuracy and the quality of reduction.
Our study has some limitations. First, it was conducted in intact cadavers with no fracture displacement. For this reason, we provisionally recommend reducing the main fracture column anatomically before trying to address the impacted dome fragment. Second, the location of the imaginary line connecting the two AIISs should be confirmed by fluoroscopy on the intact side. Additionally, the size of the instrument as well as the angular deviation of the instrument using on the bony surface could affect the location of the corresponding dome area. Prospective clinical studies with a higher power of evidence are needed to validate the outcomes of this study.
5. A clinical case
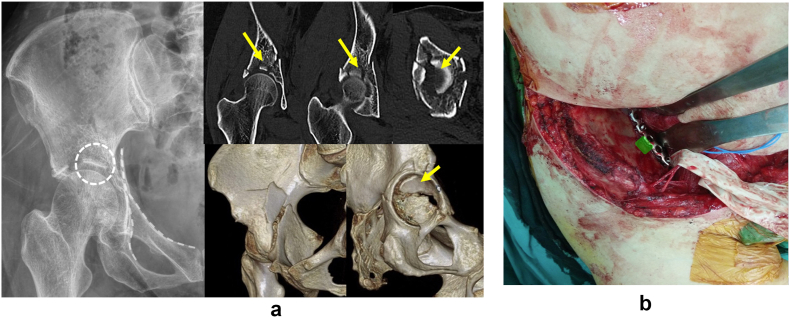
A 60-year-old female, with underlying osteoporosis, diabetes, hypertension, and breast cancer and who was currently receiving chemotherapy, sustained an anterior column and posterior hemitransverse fracture of her right acetabulum after falling from standing height. Preoperative radiographs and CT scans showed the femoral head had migrated superiorly with the displaced anterior column fracture and superomedial weight-bearing dome impaction (Fig. 6). She underwent operative fixation via an ilioinguinal approach. First the low anterior column fracture was reduced with a spike pusher and fixation was done with a pelvic reconstruction plate to buttress the fracture. After the reduction, the femoral head was pushed down to its anatomical position, but the articular impaction was still displaced superiorly. An iliac cortical window was identified using our RP superior to the joint impaction. The impacted fragment was tamped down with an impactor using the femoral head as a template under fluoroscopic monitoring. The bone graft was packed tightly into the defect. The patient was allowed to toe-touch weight bearing with a walker for 4 weeks, then partial weight bearing for 4 weeks. Full weight bearing was allowed at 8 weeks postoperatively. The follow-up radiographs at three years showed a congruent hip joint with no signs of osteoarthritic change (Fig. 7).
Fig. 6.
a) Preoperative radiographs and CT scans showed an anterior column posterior hemitransverse fracture with superomedial dome impaction (arrow). B) Intraoperative view of the location of the iliac cortical window (green area) from the lateral window of the ilioinguinal approach.
Fig. 7.
a) Fluoroscopic images demonstrating dome impaction reduction with impactor b) Follow-up radiographs at 3 years postoperatively showed a congruent hip joint with preserved joint space and no signs of posttraumatic arthritis.
6. Conclusions
Our proposed RP, which can be easily identified intraoperatively, can be used as a reliable intraoperative landmark to identify the location of the ICW for the reduction of acetabular dome impaction. We suggested that the 1-cm2 area around the RP, except in the posterior direction, corresponds to the dome of the acetabulum with 80–100% accuracy.
Ethical approval
This article does not contain any studies with human participants or animal performed by any of the authors. The study protocol was reviewed, and approved by the Institutional Review Board, IRB REC No.58-252-11-1(6).
Authors' contributions
R.J. conceived the experiments, R.J., C.J. and A.K. conducted the experiments, R.J., C.J. and T.A. analyzed the results and prepared the figures and manuscript. All authors reviewed the manuscript.
Funding
There was no funding received to assist with the preparation of this manuscript.
Availability of data and materials
Not applicable.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Mears D.C. Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg. 1999;7(2):128–141. doi: 10.5435/00124635-199903000-00006. Mar-Apr. [DOI] [PubMed] [Google Scholar]
- 2.Ferguson T.A., Patel R., Bhandari M., Matta J.M. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. Feb 2010;92(2):250–257. doi: 10.1302/0301-620X.92B2.22488. [DOI] [PubMed] [Google Scholar]
- 3.Carroll E.A., Huber F.G., Goldman A.T., et al. Treatment of acetabular fractures in an older population. J Orthop Trauma. Oct 2010;24(10):637–644. doi: 10.1097/BOT.0b013e3181ceb685. [DOI] [PubMed] [Google Scholar]
- 4.Rommens P.M., Schwab R., Handrich K., Arand C., Wagner D., Hofmann A. Open reduction and internal fixation of acetabular fractures in patients of old age. Int Orthop. Oct 2020;44(10):2123–2130. doi: 10.1007/s00264-020-04672-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anglen J.O., Burd T.A., Hendricks K.J., Harrison P. The "Gull Sign": a harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma. Oct 2003;17(9):625–634. doi: 10.1097/00005131-200310000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Kasha S., Yalamanchili R.K. Articular disimpaction in acetabular fractures. J Clin Orthop Trauma. 2020;11(6):1025–1030. doi: 10.1016/j.jcot.2020.09.018. Nov-Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. Sep 1980;(151):81–106. [PubMed] [Google Scholar]
- 8.Judet R., Judet J., Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. Dec 1964;46:1615–1646. [PubMed] [Google Scholar]
- 9.Cole J.D., Bolhofner B.R. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. Aug 1994;(305):112–123. [PubMed] [Google Scholar]
- 10.Sagi H.C., Afsari A., Dziadosz D. The anterior intra-pelvic (modified rives-stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. May 2010;24(5):263–270. doi: 10.1097/BOT.0b013e3181dd0b84. [DOI] [PubMed] [Google Scholar]
- 11.Laflamme G.Y., Hebert-Davies J. Direct reduction technique for superomedial dome impaction in geriatric acetabular fractures. J Orthop Trauma. Feb 2014;28(2):e39–e43. doi: 10.1097/BOT.0b013e318298ef0a. [DOI] [PubMed] [Google Scholar]
- 12.Collinge C.A., Lebus G.F. Techniques for reduction of the quadrilateral surface and dome impaction when using the anterior intrapelvic (modified Stoppa) approach. J Orthop Trauma. Feb 2015;29(Suppl 2):S20–S24. doi: 10.1097/BOT.0000000000000271. [DOI] [PubMed] [Google Scholar]
- 13.Keel M.J., Tomagra S., Bonel H.M., Siebenrock K.A., Bastian J.D. Clinical results of acetabular fracture management with the Pararectus approach. Injury. Dec 2014;45(12):1900–1907. doi: 10.1016/j.injury.2014.10.040. [DOI] [PubMed] [Google Scholar]
- 14.Keel M.J.B., Siebenrock K.A., Tannast M., Bastian J.D. The pararectus approach: a new concept. JBJS Essent Surg Tech. Sep 28 2018;8(3):e21. doi: 10.2106/JBJS.ST.17.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scolaro J.A., Routt M.L., Jr. Reduction of osteoarticular acetabular dome impaction through an independent iliac cortical window. Injury. Dec 2013;44(12):1959–1964. doi: 10.1016/j.injury.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 16.Bhandari M., Matta J., Ferguson T., Matthys G. Predictors of clinical and radiological outcome in patients with fractures of the acetabulum and concomitant posterior dislocation of the hip. J Bone Joint Surg Br. Dec 2006;88(12):1618–1624. doi: 10.1302/0301-620X.88B12.17309. [DOI] [PubMed] [Google Scholar]
- 17.Manson T.T. Open reduction and internal fixation plus total hip arthroplasty for the acute treatment of older patients with acetabular fracture: surgical techniques. Orthop Clin N Am. Jan 2020;51(1):13–26. doi: 10.1016/j.ocl.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 18.Archdeacon M.T., Kazemi N., Collinge C., Budde B., Schnell S. Treatment of protrusio fractures of the acetabulum in patients 70 years and older. J Orthop Trauma. May 2013;27(5):256–261. doi: 10.1097/BOT.0b013e318269126f. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.