Abstract
Background
Ossicles of avulsed fractures of the lateral malleolus can result in pain or chronic ankle instability. The purpose of this study was to evaluate and compare the arthroscopic double-row fixation procedure with anatomic ankle lateral ligaments reconstruction for the treatment of ankle lateral ligaments injury with os subfibulare.
Methods
This retrospective study included 38 patients with ankle lateral ligaments injury with concomitant os subfibulare who were treated between July 2016 and November 2021. The patients were divided into a double-row fixation group (n = 19) and an ankle lateral ligaments reconstruction group (n = 19). The Karlsson and Peterson Scoring System for Ankle Function (KAFS), American Orthopedic Foot and Ankle Society (AOFAS) score, Tegner score, visual analog scale (VAS), and anterior drawer test (ADT) were obtained preoperatively and at the last post-operative follow-up. Magnetic resonance imaging (MRI) was also performed at the last post-operative follow-up.
Results
The KAFS, AOFAS, VAS, and Tegner scores increased significantly after the surgery. Furthermore, the pre- and post-operative functional scores were comparable between the two groups. The ADT was negative in all participants post-operatively. There were no significant differences between the double-row fixation and ligaments reconstruction groups regarding the proportions of patients who achieved a minimally clinically important difference (MCID) in KAFS, AOFAS, and Tegner scores. There was no significant difference in T2 mapping values for the tibial and talar side post-operatively between the two groups. Moreover, there were no significant differences in functional scores post-operatively between bony fusion and non-fusion patients in the double fixation group.
Conclusion
The double-row fixation procedure provided similar satisfactory clinical outcomes when compared with lateral ligaments reconstruction for the treatment of ankle lateral ligaments injury with os subfibulare over a short follow-up duration.
Keywords: Ankle lateral ligaments, Double-row fixation, Injury, Reconstruction, Os subfibulare
1. Introduction
Os subfibulare is defined as an ossicle around the tip of the lateral malleolus of the ankle.1 A previous report stated that 0.2–6.6% of the population have ossicles in the lateral malleolus.2 Two etiologies describe the origin of subfibular ossicles, including the accessory ossification center that remains separate from the lateral malleolus3,4 and non-united avulsion fractures following an ankle sprain.5,6 Patients with subfibular ossicles can be symptomatic or asymptomatic; asymptomatic ossicles may become symptomatic due to ankle sprain or overuse. If conservative treatments fail, surgery should then be considered. For small ossicles less than 10 mm in diameter, ossicle resection combined with the modified Broström operation is widely used.7,8 However, for cases with ossicles larger than 10 mm, the protocols for surgical treatment remain controversial and clinical outcomes are uncertain.4,9 There is increasing interest in the use of arthroscopy as it presents several advantages: less invasive, clearer visualization, less post-operative pain, lower rate of complications, and accelerated healing post-operatively.10, 11, 12, 13 Previous studies have indicated that the resection of ossicles and anatomical reconstruction of the lateral ligaments achieve satisfactory clinical results for the treatment of chronic ankle instability with large os subfibulare.14,15 On the other hand, arthroscopic double-row fixation technology has been used in patients with acute bony Bankart lesions and avulsion fractures of the great tuberosity; the outcomes of this technique have been confirmed via biomechanical and clinical studies.16, 17, 18, 19 Double-row fixation technique could improve the initial repair strength and provide superior interface contact.17 Moreover, in treatment of ankle lateral ligaments injury with ossicles larger than 10 mm, the potential advantage of double-row fixation technique was allowing re-fixation of the lateral ligament in situ, which overcomes the difficulty in repairing the ligaments with large gap after removal of the os subfibulare. Therefore, we hypothesized that this technique would also yield satisfactory clinical outcomes for the treatment of os subfibulare-associated ankle sprain.
The purpose of this study was to evaluate and compare the arthroscopic double-row fixation procedure with anatomical ankle lateral ligaments reconstruction for the treatment of ankle lateral ligaments injury with os subfibulare. We hypothesized that the double-row fixation procedure would provide similar clinical and imaging outcomes when compared with the lateral ligaments reconstruction for the treatment of ankle lateral ligaments injury with os subfibulare.
2. Materials and methods
2.1. Participant selection criteria
Between July 2016 and November 2021, we recruited a total of 38 patients for this retrospective cohort study. All the patients were consecutive cases. The research was conducted in accordance with a protocol approved by the Research Ethics Committee in our hospital. All participants were diagnosed with ankle lateral ligaments injury with a concomitant os subfibulare.
The inclusion criteria were as follows: 1) a history of ankle sprain with persistent symptoms such as giving way, pain, or swelling; 2) lateral ankle ligaments injury ((including anterior talofibular ligament (ATFL) and/or calcaneofibular ligament (CFL)) with os subfibulare larger than 10 mm, as determined by history, physical examination, X ray, MRI, and arthroscopy evaluation, and 3) a willingness to undergo surgery.
The exclusion criteria were as follows: 1) a history of ipsilateral lower extremity surgery or ankle fracture; 2) deformity around the ankle joint (flat foot, high arch, varus heel, or inverting tibial plateau); 3) simultaneous surgery for ankle osteoarthritis or anatomic deformity; 4) patients with a peroneal tendon tear or dislocation, and 5) aged younger than 16 years or older than 60 years.
Participants were divided into two groups. Group A received arthroscopic double-row fixation of the os subfibulare. Group B received open anatomic reconstruction using an auto or allo-semitendinosus tendon.20 All surgical procedures were performed by a senior surgeon qualified in sports medicine.
2.2. Surgical technique
After providing signed and informed consent, all the participants underwent arthroscopic evaluation. Under general anesthesia, the individual was placed in the supine position with the knee flexed on a custom-made triangular pillow. A pneumatic tourniquet was applied to the thigh. After the standard anterior medial and lateral portals were created, we performed the arthroscopic evaluation of the ankle joint and addressed the intra-articular pathologies. The synovial tissue was resected with a 2.7 mm shaver and the os subfibulare was identified; all of the subfibluare were in the joint, these were often located anterior to the tip of the lateral malleolus. Subsequently, the double-row fixation or ankle lateral ligaments reconstruction procedure was performed depending on the willingness of the participant (see Fig. 1).
Fig. 1.
Diagram to illustrate the technique of double-row fixation.
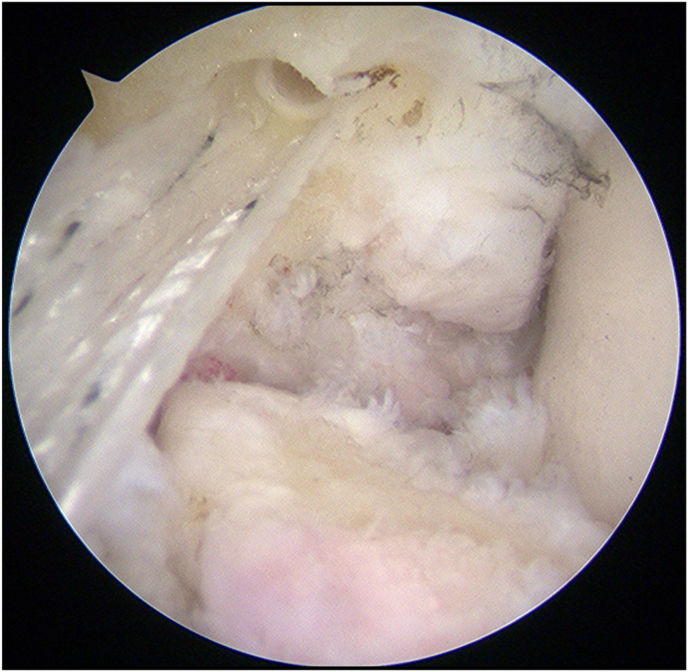
2.3. Double-row fixation procedure (Fig. 1)
Hard bone was removed, and the bone surface was freshen with a 2.7 mm burr and a suture tape (FiberTape, Arthrex Inc., FL, USA) was passed into the eyelet of a 2.9 mm knotless anchor (PushLock, Arthrex Inc., FL, USA). The anchor was inserted into the medial edge of the fibular fracture surface which was parallel to the shaft of the fibula (Fig. 2). Using a suture hook, both ends of the suture tape were passed separately through the soft tissue anterior and posterior to the CFL, between the space of the ATFL and CFL, as well as the CFL and posterior talofibular ligament (PTFL) (Fig. 3). The two ends of the suture tape were then passed through the eyelet of a 4.75 mm knotless anchor (SwiveLock, Arthrex Inc., FL, USA). After adjusting the tension of the suture tape, the 4.75 mm knotless anchor was inserted into the lateral side of the lateral malleolus to fix the two ends of the tape with the ankle in a neutral dorsiflexion and lightly everted position (Fig. 4). After confirming that the fixation was satisfactory, the portals were closed.
Fig. 2.
A suture tape (FiberTape, Arthrex Inc., FL, USA) was passed into the eyelet of a 2.9 mm knotless anchor (pushlock, Arthrex Inc., FL, USA). The anchor was inserted into the medial edge of the fibular fracture surface, which was parallel to the shaft of the fibula.
Fig. 3.
Both ends of the suture tape were pass through the soft tissue inside the os subfibulare with a suture hook. A: One end of the suture tape was passed through the space between anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL); B: Another end of the suture tape was passed through the space between CFL and posterior talofibular ligament (PTFL).
Fig. 4.
After the tension of the suture tape was adjusted, the 4.5 mm knotless anchor were inserted into the lateral side of the lateral malleolus to fix the 2 ends of the tape with the ankle in a neutral dorsiflexion and lightly everted position.
2.4. Ligaments reconstruction procedure
A longitudinal skin incision was made from the tip of the distal fibula to the talar insertion of the ATFL. The anterior edge of the distal fibula and the os subfibulare was then exposed and the avulsion fragment was excised. As all the fragments were larger than 10 mm, directly repair the lateral ligament repair was very difficult because of the high tension, ligaments reconstruction was chosen. Two oblique 3.5 mm tunnels were created in the fibula beginning 7 and 13 mm proximal to the tip of the fibula, respectively. An additional two 3.5-mm converging tunnels were created at the talar insertion of the ATFL. The tubercle of the calcaneus was exposed and a 7 mm tunnel was made at the insertion of the CFL on the calcaneus.
A semitendinosus autograft or allograft (Osteolink Biomaterial Inc. Hubei, China) that was 20 cm in length was then applied. Both ends of the graft were braided with No.2 non-absorbable sutures (Ethibond, Ethicon, Inc., OH, USA). One end of the graft was pulled into the tunnel of the calcaneus and fixed with a 7 mm bioabsorbable screw (Bio Intrafix, DePuy Synthes Inc., MA, USA). The other end of the graft was passed beneath the peroneal tendons, and then pulled into the inferior tunnel in the fibula in an anteroposterior direction. The graft was then routed back through the superior tunnel in the fibula. Next, the graft was pulled into the tunnels in the talus. After the tension of the graft was adjusted, the free end of the graft was sutured to the tendon itself with the ankle in a neutral dorsiflexion and lightly everted position. Finally, the capsule was re-sutured and the incision was closed.20
2.5. Rehabilitation
Following surgery, the ankle was immobilized in a slightly everted position with a short leg cast. The cast was removed two weeks post-operatively. After the cast was removed, passive dorsiflexion and plantar flexion were permitted. Partial weight-bearing was started four weeks later. All patients were followed up for a minimum of 6 months after surgery.
2.6. Outcome measures
The Karlsson and Peterson Scoring System for Ankle Function (KAFS),21 visual analog scale (AOFAS) score,22 Tegner score,23 Visual analog scale (VAS), and anterior drawer test (ADT) were evaluated pre-operatively and at the last post-operative follow-up.
The primary outcome was the KAFS at the last post-operative follow-up. The secondary outcomes included the AOFAS, Tegner score, VAS, and ADT.
2.7. MRI evaluation
MRI evaluations were performed at the last post-operative follow-up. The MRI evaluation included two aims. The first aim was to evaluate the bone union after the operation. The second aim was to evaluation the T2 mapping values postoperation.
All MRI examinations were performed on a 3T scanner (Magnetom Verio, Siemens Healthcare, Erlangen, Germany) with a gradient strength of 45 mT/m using an 8-channel phased-array coil. All participants were scanned after at least 30 min of rest to ensure that the ankle cartilage was in a stable resting condition during image acquisition.
For the biochemical evaluation of cartilage, multi-echo spin-echo technique (T2-mapping) images were acquired in the sagittal section plane for ankles. The parameters were as follows: TR/TE: 1220/13.8, 27.6, 41.4, 55.2, 69.0 ms; field-of-view: 160 × 160 mm; matrix: 384 × 384; matrix phase: 100%; pixel size: 0.4 × 0.4 × 2.0 mm; slice thickness: 2 mm; number of excitations: 2; flip angle: 180°; bandwidth: 228 Hz/pixel; Scan time: 8:22 min. T2 relaxation times were measured from T2-mapping images which were obtained using a pixel-wise, mono-exponential non-negative least squares (NNLS) fit analysis.24
2.8. Statistical analysis
Due to the skewed distributions and the heterogeneity of variance between groups, data are presented as medians and ranges and were analyzed by non-parametric tests. The within-group differences in ankle scores from pre-to post-surgery were analyzed with Wilcoxon's signed-rank test. Gender differences were analyzed with Pearson's Chi-square test. To compare the differences in ankle scores before and after surgery between the two surgical groups, we used the Mann-Whitney U test. To compare the T2 mapping values between the three groups, we used the Kruskal-Wallis test. All statistical analyses were performed with IBM SPSS 19.0 (Armonk, New York, USA). Differences were considered statistically significant when p < 0.05. Post-hoc analysis was performed to calculate the statistical power. As the calculated effect size was 0.9, the sample size was 19 in each group, and the α level was 0.05; the calculated power was 0.86. The minimum clinically important difference (MCID) was calculated using a distribution-based method based on patient-reported outcome measures (PROMs) for the study population.25 Moreover, the percentage of PROMs that reached the MCID was calculated.
3. Results
Demographic data for the participants are shown in Table 1. There were no significant differences between the double-row fixation and ligaments reconstruction groups in terms of age, sex, height, weight, body mass index (BMI), time from injury to surgery, and mean follow-up time.
Table 1.
Participant demographic data.
| Demographic Data | Double-row fixation | Ligaments reconstruction | P value |
|---|---|---|---|
| Subjects (n) | 19 | 19 | |
| Sex male/female (n) | 11/8 | 15/4 | 0.163 |
| Age (years) | 33(18, 47) | 30(19, 43) | 1.000 |
| Height (mm) | 173(155, 186) | 175(160, 187) | 0.661 |
| Weight (kg) | 70(49, 110) | 75(49, 103) | 0.672 |
| BMI | 23.4(20.1, 32.1) | 25(18, 29.8) | 0.672 |
| Time since injury (months) | 36(1, 120) | 26(23, 72) | 0.815 |
| Mean follow-up time (months) | 23(6, 46) | 26(23, 72) | 0.064 |
| Concomitant intra-articular lesions (no. (%)) | |||
| Osteochondral defect rowhead | 11(57.9%) | 9(50%) | 0.516 |
| Anterior impingement rowhead | 4(21.1%) | 2(10.5%) | 0.374 |
| Loose body rowhead | 3(15.8%) | 1(5.3%) | 0.290 |
| Sinus Tarsi Syndrome rowhead | 3(15.8%) | 1(5.3%) | 0.290 |
BMI: Body Mass Index.
The KAFS, AOFAS, VAS, and Tegner scores were significantly increased after surgery (Fig. 5) in the double-row fixation and ligaments reconstruction groups. Moreover, comparable improvements of functional scores after surgery were found between the two groups (Table 2). The anterior drawer test was negative for all participants following surgery. There were also no significant differences between the double-row fixation and ligaments reconstruction groups regarding the proportion of patients who achieved the minimally clinically important difference (MCID) in all scores (KAFS 94.7% versus 100%; AOFAS 89.5% versus 100%; Tegner 68.4% versus 52.6%, respectively).
Fig. 5.
Scores before and after the operation. The KAFS, AOFAS, VAS, and Tegner scores were significantly increased after surgery in the double-row fixation and ligaments reconstruction groups. AOFAS: American Orthopedic Foot and Ankle Society Score KAFS: Karlsson and Peterson Scoring System for Ankle Function VAS: Visual analog scale.
Table 2.
Scores between groups Median (min, max).
| Group | AOFAS |
KAFS |
Tegner |
VAS |
|---|---|---|---|---|
| Improvement△ (Postop-preop) | Improvement△ (Postop-preop) | Improvement△ (Postop-preop) | Improvement△ (Preop-postop) | |
| Double-row fixation | 17(0, 83) | 38(-5, 80) | 2(0, 6) | 1(0, 7) |
| Ligaments reconstruction | 16(6, 49) | 25(10, 40) | 2(0, 5) | 3(0, 7) |
| P value | 0.919 | 0.145 | 0.376 | 0.137 |
△: difference between preoperative and postoperative value.
AOFAS: American Orthopedic Foot and Ankle Society Score.
KAFS: Karlsson and Peterson Scoring System for Ankle Function.
VAS: Visual analog scale.
Eleven patients in the double-row fixation group and 19 patients in the ligaments reconstruction group were evaluated by MRI during their last post-operative follow-up. The T2 mapping values in double-row fixation and ligaments reconstruction groups are shown in Table 3. There were no significant differences in the T2 mapping values on the tibial and talar side after surgery when compared between the double-row fixation and the reconstruction groups.
Table 3.
Values of T2 Mapping between groups. Median (min, max).
| Group | Subjects n | Tibial side | Talar side |
|---|---|---|---|
| Double-row fixation | 11 | 35.3(26.2,44.3) ∗ | 36.2(25.3,38.6) ∗ |
| Ligaments reconstruction | 19 | 35.1(29.3,46.5) ∗ | 35.3(28.3,46.2) ∗ |
| P value | 0.780 | 0.620 |
In the double-row fixation group, 7 individuals showed bony fusion and 4 showed non-fusion. There were no significant differences in functional scores after surgery when compared between bony fusion and non-fusion individuals (Table 4).
Table 4.
Scores between fusion and non-fusion in double-row fixation groups.
| Phase | AOFAS |
KAFS |
Tegner |
VAS |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fusion | Non-fusion | P value | Fusion | Non-fusion | P value | Fusion | Non-fusion | P value | Fusion | Non-fusion | P value | |
| Pre-operation | 85 (7, 100) | 83(10, 97) | 0.849 | 65 (5, 95) | 70 (30, 95) | 0.775 | 6 (0, 7) | 2 (1, 4) | 0.068 | 1 (0, 4) | 1 (0, 4) | 0.770 |
| Post-operation | 100 (90, 100) | 96(79, 100) | 0.229 | 97 (85, 100) | 92.5 (70, 100) | 0.788 | 6(6, 7) | 5 (2, 7) | 0.684 | 0 (0, 1) | 0 (0, 1) | 0.673 |
| P value | 0.027 | 0.068 | 0.018 | 0.197 | 0.180 | 0.109 | 0.038 | 0.180 | ||||
Median (min, max).
AOFAS: American Orthopedic Foot and Ankle Society Score.
KAFS: Karlsson and Peterson Scoring System for Ankle Function.
VAS: Visual analog scale.
4. Discussion
The most important finding of the present study was that the double-row fixation procedure provided similarly satisfactory clinical outcomes when compared with lateral ligaments reconstruction for the treatment of ankle lateral ligaments injury with os subfibulare.
Lateral ankle sprain is very common and results in significant functional disability. A previous study indicated that the incidence rate of ankle sprains is 2.15 per 1000 person-years in the general population and 9.35 per 1000 person-years in elite athletes.26 Most of these injuries involve the lateral ligaments and more than 30% of these patients experience persistent symptoms and chronic instability. Chronic ankle instability may be influenced by several factors, including mechanical and functional factors. Previous studies indicate that 20–40% of patients with mechanical instability require surgical treatment.27,28
Numerous surgical techniques have been introduced to treat chronic lateral ankle instability, including non-anatomical reconstruction, anatomical repair, and anatomical reconstruction. Although non-anatomical reconstruction techniques have resulted in a high degree of patient satisfaction, these repairs are prone to numerous post-operative complications.29 Conversely, anatomical repair has been widely used with few complications, although it is not suitable for patients with ATFL or CFL deficiencies. More recently, anatomical reconstruction has been introduced to anatomically recreate the stability of the ankle joint. Excellent results have been reported following anatomical open or arthroscopic reconstruction.20,29,30
A previous study indicated that the presence of a distal fibula avulsion fracture is associated with an increased risk of recurrent sprain.6 In terms of symptomatic os subfibulare, if conservative treatment fails, then surgery should be considered. A systematic review found that satisfactory postoperative outcomes can be reliably expected following surgical treatment.1 For small ossicles, resection of the ossicle and repair of the ankle lateral ligaments can achieve excellent outcomes.3,7,8,31,32 However, in patients with large os subfibulare, it is difficult to repair the ligaments in situ after the os subfibulare has been removed.33 Therefore, ligaments reconstruction15 or refixation34 of the ossicle may be needed.
Previous studies have confirmed the advantages of double-row fixation technology for the treatment of shoulder avulsion fractures. Biomechanical research has found that the double-row fixation technique can provide higher contact pressure, thus resulting in superior stability and reduced displacement when compared with the single-row repair technique for the treatment of avulsion fracture.16,17 In addition, clinical research has shown that the double-row suture anchor fixation technique can provide satisfactory clinical results for the treatment of avulsion fracture in the shoulder.18,19
In the current clinical research, both surgical techniques have shown similar satisfactory clinical outcomes for the treatment of ankle lateral ligaments injury with os subfibulare. We believe that the arthroscopic double-row fixation procedure has numerous advantages; it is less invasive, less costly, involves a shorter operation time, is associated with fewer complications from donations, involves less pain, and avoids allograft rejection. Moreover, in treatment of ankle lateral ligaments injury with ossicles larger than 10 mm, the potential advantage of double-row fixation technique was allowing re-fixation of the lateral ligament in situ, which overcomes the difficulty in repairing the ligaments with large gap after removal of the os subfibulare.
In terms of MRI, previous studies have shown that a higher T2 value is associated with an irregular collagen arrangement and an increased water content in the cartilage matrix,35 thus indicating potential cartilage degeneration in these areas. Moreover, Tao et al.24 found that cartilage degeneration cannot be completely reversed even after the ankle lateral ligaments had been repaired in patients with chronic ankle instability. One potential reason may be that anatomical repair cannot completely restore the native hind foot contact mechanics. Therefore, the altered contact mechanics might continue to contribute to the progression of cartilage degeneration in the ankle joint.36 Another potential reason is that early and persistent synovial changes after injury could result in progressive gross and histological cartilage damage, even in a mechanically stable joint.37 In our study, there was no significant difference in T2 values of the tibial and talar cartilage when compared between the ligaments reconstruction and double-row fixation groups. As participant demographics between the surgical groups were comparable, we considered that both techniques contributed similar roles in helping to restore normal movement and preventing the further degradation of cartilage after the surgery. In the double-fixation group, no significant differences in functional scores after surgery when compared between bony fusion and non-fusion individuals. We believe that the purpose of the surgery is to re-position the os subfibulare to the distal fibula, which could restore the tension of lateral collateral ligament and maintain joint stability. Therefore, on-fusion patients could achieved satisfactory clinical outcomes. However, the small sample size limits the accuracy of the results. A large sample size study maybe need in the future.
5. Limitations
The present study had some limitations that need to be considered. One limitation was the potential for recall bias and selective bias due to the retrospective nature of this study. In the future, a prospective, randomized and controlled study will help resolve this. The second limitation was that we only considered a relatively short follow-up time. A longer period of follow-up will help characterize long-term outcomes. The third limitation was that not all patients in the double-row fixation group received an MRI evaluation.
6. Conclusion
The double-row fixation procedure provided similarly satisfactory clinical outcomes when compared with lateral ligaments reconstruction for the treatment of ankle lateral ligaments injury with os subfibulare, over a short follow-up period.
Acknowledgment
This work was supported by a grant awarded to Ying-Hui Hua from the National Natural Science Foundation of China (NSFC81871823) and Hong-Yun Li from the National Key Research and Development Program of China (2019YFF030170, 2020YFC20070405).
The first and the second authors contribute equally to this work.
Ethical approval for this study was obtained from the Ethics Committee of Huashan Hospital (2020–1123).
References
- 1.Schlickewei C., Krähenbühl N., Rolvien T., et al. Surgical outcome of avulsion fractures of the distal fibula: a systematic literature review. Arch Orthop Trauma Surg. 2023;143(3):1275–1291. doi: 10.1007/s00402-021-04256-6. https://doi:10.1007/s00402-021-04256-6 [DOI] [PubMed] [Google Scholar]
- 2.Keles-Celik N, Kose O, Sekerci R, Aytac G, Turan A, Güler F. Accessory ossicles of the foot and ankle: disorders and a review of the literature. Cureus. 2017; 29 (11): e1881. https://doi: 10.7759/cureus.1881. [DOI] [PMC free article] [PubMed]
- 3.Kim W.J., Lee H.S., Moon S.I., et al. Presence of subfibular ossicle does not affect the outcome of arthroscopic modified Brostrom procedure for chronic lateral ankle instability. Arthroscopy. 2019;35(3):953–960. doi: 10.1016/j.arthro.2018.10.148. https://doi: 10.1016/j.arthro.2018.10.148 [DOI] [PubMed] [Google Scholar]
- 4.El Ashry S.R., El Gamal T.A., Platt S.R. Atypical chronic ankle instability in a pediatric population secondary to distal fibula avulsion fracture nonunion. J Foot Ankle Surg. 2017;56(1):148–152. doi: 10.1053/j.jfas.2016.04.018. https://doi: 10.1053/j.jfas.2016.04.018 [DOI] [PubMed] [Google Scholar]
- 5.Haraguchi N., Toga H., Shiba N., Kato F. Avulsion fracture of the lateral ankle ligament complex in severe inversion injury: incidence and clinical outcome. Am J Sports Med. 2007;35(7):1144–1152. doi: 10.1177/0363546507299531. https://doi: 10.1177/0363546507299531 [DOI] [PubMed] [Google Scholar]
- 6.Yamaguchi S., Akagi R., Kimura S., et al. Avulsion fracture of the distal fibula is associated with recurrent sprain after ankle sprain in children. Knee Surg Sports Traumatol Arthrosc. 2019;27(9):2774–2780. doi: 10.1007/s00167-018-5055-7. https://doi: 10.1007/s00167-018-5055-7 [DOI] [PubMed] [Google Scholar]
- 7.Kubo M., Yasui Y., Sasahara J., Miki S., Kawano H., Miyamoto W. Simultaneous ossicle resection and lateral ligament repair give excellent clinical results with an early return to physical activity in pediatric and adolescent patients with chronic lateral ankle instability and os subfibulare. Knee Surg Sports Traumatol Arthrosc. 2020;28(1):298–304. doi: 10.1007/s00167-019-05718-6. https://doi: 10.1007/s00167-019-05718-6 [DOI] [PubMed] [Google Scholar]
- 8.Park C.H., Park J. Effect of modified Broström procedure with periosteal fap augmentation after subfibular ossicle excision on ankle stability. Foot Ankle Int. 2019;40(6):656–660. doi: 10.1177/1071100719837230. https://doi: 10.1177/1071100719837230 [DOI] [PubMed] [Google Scholar]
- 9.Han S.H., Choi W.J., Kim S., Kim S.J., Lee J.W. Ossicles associated with chronic pain around the malleoli of the ankle. J Bone Joint Surg Br. 2008;90(8):1049–1054. doi: 10.1302/0301-620X.90B8.20331. https://doi: 10.1302/0301-620X.90B8.20331 [DOI] [PubMed] [Google Scholar]
- 10.Lui T.H., Wan Y.T.O. Arthroscopic stabilization of unstable os subfibulare. Arthrosc Tech. 2019;8(9):e1007–e1012. doi: 10.1016/j.eats.2019.05.011. https://doi: 10.1016/j.eats.2019.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feng S.M., Sun Q.Q., Wang A.G., Zhang Z.Y., Hao L. Long-term functional outcomes of all-inside arthroscopic repair of anterior talofibular ligament avulsion fracture. Foot Ankle Surg. 2021;27(2):156–161. doi: 10.1016/j.fas.2020.03.007. https://doi: 10.1016/j.fas.2020.03.007 [DOI] [PubMed] [Google Scholar]
- 12.Li H., Hua Y., Li H., Ma K., Li S., Chen S. Activity level and function 2 years after anterior talofibular ligament repair: a comparison between arthroscopic repair and open repair procedures. Am J Sports Med. 2017;45(9):2044–2051. doi: 10.1177/0363546517698675. https://doi: 10.1177/0363546517698675 [DOI] [PubMed] [Google Scholar]
- 13.Matsui K., Takao M., Miyamoto W., Matsushita T. Early recovery after arthroscopic repair compared to open repair of the anterior talofibular ligament for lateral instability of the ankle. Arch Orthop Trauma Surg. 2016;136(1):93–100. doi: 10.1007/s00402-015-2342-3. https://doi: 10.1007/s00402-015-2342-3 [DOI] [PubMed] [Google Scholar]
- 14.Reiner M.M., Sharpe J.J. The role of the accessory malleolar ossicles and malleolar avulsion fractures in lateral ankle ligament reconstruction. Foot Ankle Spec. 2018;11(4):308–314. doi: 10.1177/1938640017729498. https://doi: 10.1177/1938640017729498 [DOI] [PubMed] [Google Scholar]
- 15.Cao Y., Xu Y., Huang Q., Xu Y., Hong Y., Xu X. Outcomes of ossicle resection and anatomic reconstruction of lateral ligaments for chronic ankle instability with large malleolar accessory ossicles. Foot Ankle Surg. 2021;27(7):736–741. doi: 10.1016/j.fas.2020.09.012. https://doi: 10.1016/j.fas.2020.09.012 [DOI] [PubMed] [Google Scholar]
- 16.Greenstein A.S., Chen R.E., Knapp E., et al. A biomechanical, cadaveric evaluation of single- versus double-row repair techniques on stability of bony Bankart lesions. Am J Sports Med. 2021;49(3):773–779. doi: 10.1177/0363546520985184. https://doi: 10.1177/0363546520985184 [DOI] [PubMed] [Google Scholar]
- 17.Lin C.L., Yeh M.L., Su F.C., et al. Different suture anchor fixation techniques affect contact properties in humeral greater tuberosity fracture: a biomechanical study. BMC Muscoskel Disord. 2019;20(1):26. doi: 10.1186/s12891-019-2412-8. https://doi: 10.1186/s12891-019-2412-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liao W., Zhang H., Li Z., Li J. Is arthroscopic technique superior to open reduction internal fixation in the treatment of isolated displaced greater tuberosity fractures? Clin Orthop Relat Res. 2016;474(5):1269–1279. doi: 10.1007/s11999-015-4663-5. https://doi: 10.1007/s11999-015-4663-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo S., Jiang C. "Double-Pulley" dual-row technique for arthroscopic fixation of large bony Bankart lesion: minimum 2-year follow-up with CT evaluation. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211029239. https://doi: 10.1177/23259671211029239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hua Y., Chen S., Jin Y., Zhang B., Li Y., Li H. Anatomical reconstruction of the lateral ligaments of the ankle with semitendinosus allograft. Int Orthop. 2012;36(10):2027–2031. doi: 10.1007/s00264-012-1577-7. https://doi: 10.1007/s00264-012-1577-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karlsson J., Eriksson B.I., Bergsten T., Rudholm O., Swärd L. Comparison of two anatomic reconstructions for chronic lateral instability of the ankle joint. Am J Sports Med. 1997;25(1):48–53. doi: 10.1177/036354659702500109. https://doi: 10.1177/036354659702500109 [DOI] [PubMed] [Google Scholar]
- 22.Guelfi M., Zamperetti M., Pantalone A., Usuelli F.G., Salini V., Oliva X.M. Open and arthroscopic lateral ligament repair for treatment of chronic ankle instability: a systematic review. Foot Ankle Surg. 2018;24(1):11–18. doi: 10.1016/j.fas.2016.05.315. https://doi: 10.1016/j.fas.2016.05.315 [DOI] [PubMed] [Google Scholar]
- 23.Tegner Y., Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 24.Tao H., Zhang Y., Hu Y., et al. Cartilage matrix changes in hindfoot joints in chronic ankle instability patients after anatomic repair using T2-mapping: initial experience with 3-year follow-up. J Magn Reson Imag. 2022;55(1):234–243. doi: 10.1002/jmri.27809. https://doi: 10.1002/jmri.27809 [DOI] [PubMed] [Google Scholar]
- 25.Sedaghat A.R. Understanding the minimal clinically important difference (MCID) of patient-reported outcome measures. Otolaryngol Head Neck Surg. 2019;161(4):551–560. doi: 10.1177/0194599819852604. https://doi: 10.1177/0194599819852604 [DOI] [PubMed] [Google Scholar]
- 26.Waterman B.R., Owens B.D., Davey S., Zacchilli M.A., Belmont P.J., Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279–2284. doi: 10.2106/JBJS.I.01537. https://doi: 10.2106/JBJS.I.01537 [DOI] [PubMed] [Google Scholar]
- 27.Hiller C.E., Nightingale E.J., Lin C.W., Coughlan G.F., Caulfield B., Delahunt E. Characteristics of people with recurrent ankle sprains: a systematic review with meta-analysis. Br J Sports Med. 2011;45(8):660–672. doi: 10.1136/bjsm.2010.077404. https://doi: 10.1136/bjsm.2010.077404 [DOI] [PubMed] [Google Scholar]
- 28.Karlsson J., Lansinger O. Chronic lateral instability of the ankle in athletes. Sports Med. 1993;16(5):355–365. doi: 10.2165/00007256-199316050-00006. https://doi: 10.2165/00007256-199316050-00006 [DOI] [PubMed] [Google Scholar]
- 29.Takao M., Oae K., Uchio Y., Ochi M., Yamamoto H. Anatomical reconstruction of the lateral ligaments of the ankle with a gracilis autograft: a new technique using an interference fit anchoring system. Am J Sports Med. 2005;33(6):814–823. doi: 10.1177/0363546504272688. https://doi: 10.1177/0363546504272688 [DOI] [PubMed] [Google Scholar]
- 30.Guillo S., Takao M., Calder J., et al. Arthroscopic anatomical reconstruction of the lateral ankle ligaments. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):998–1002. doi: 10.1007/s00167-015-3789-z. https://doi: 10.1007/s00167-015-3789-z [DOI] [PubMed] [Google Scholar]
- 31.Chun T.H., Park Y.S., Sung K.S. The effect of ossicle resection in the lateral ligament repair for treatment of chronic lateral ankle instability. Foot Ankle Int. 2013;34(8):1128–1133. doi: 10.1177/1071100713481457. https://doi: 10.1177/1071100713481457 [DOI] [PubMed] [Google Scholar]
- 32.Ahn H.W., Lee K.B. Comparison of the modified Broström procedure for chronic lateral ankle instability with and without subfibular ossicle. Am J Sports Med. 2016;44(12):3158–3164. doi: 10.1177/0363546516660069. https://doi: 10.1177/0363546516660069 [DOI] [PubMed] [Google Scholar]
- 33.Kim B.S., Choi W.J., Kim Y.S., Lee J.W. The effect of an ossicle of the lateral malleolus on ligament reconstruction of chronic lateral ankle instability. Foot Ankle Int. 2010;31(3):191–196. doi: 10.3113/FAI.2010.0191. https://doi: 10.3113/FAI.2010.0191 [DOI] [PubMed] [Google Scholar]
- 34.Diallo J., Wagener J., Schweizer C., Lang T.H., Ruiz R., Hintermann B. Intraoperative findings of lateral ligament avulsion fractures and outcome after refixation to the fibula. Foot Ankle Int. 2018;39(6):669–673. doi: 10.1177/1071100718760273. https://doi: 10.1177/1071100718760273 [DOI] [PubMed] [Google Scholar]
- 35.Mosher T.J., Dardzinski B.J. Cartilage MRI T2 relaxation time mapping: overview and applications. Semin Muscoskel Radiol. 2004;8(4):355–368. doi: 10.1055/s-2004-861764. https://doi: 10.1055/s-2004-861764 [DOI] [PubMed] [Google Scholar]
- 36.Prisk V.R., Imhauser C.W., O'Loughlin P.F., Kennedy J.G. Lateral ligament repair and reconstruction restore neither contact mechanics of the ankle joint nor motion patterns of the hindfoot. J Bone Joint Surg Am. 2010;92(14):2375–2386. doi: 10.2106/JBJS.I.00869. https://doi: 10.2106/JBJS.I.00869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huebner K.D., Shrive N.G., Frank C.B. New surgical model of post-traumatic osteoarthritis: isolated intra-articular bone injury in the rabbit. J Orthop Res. 2013;31(6):914–920. doi: 10.1002/jor.22284. https://doi: 10.1002/jor.22284 [DOI] [PubMed] [Google Scholar]