Abstract
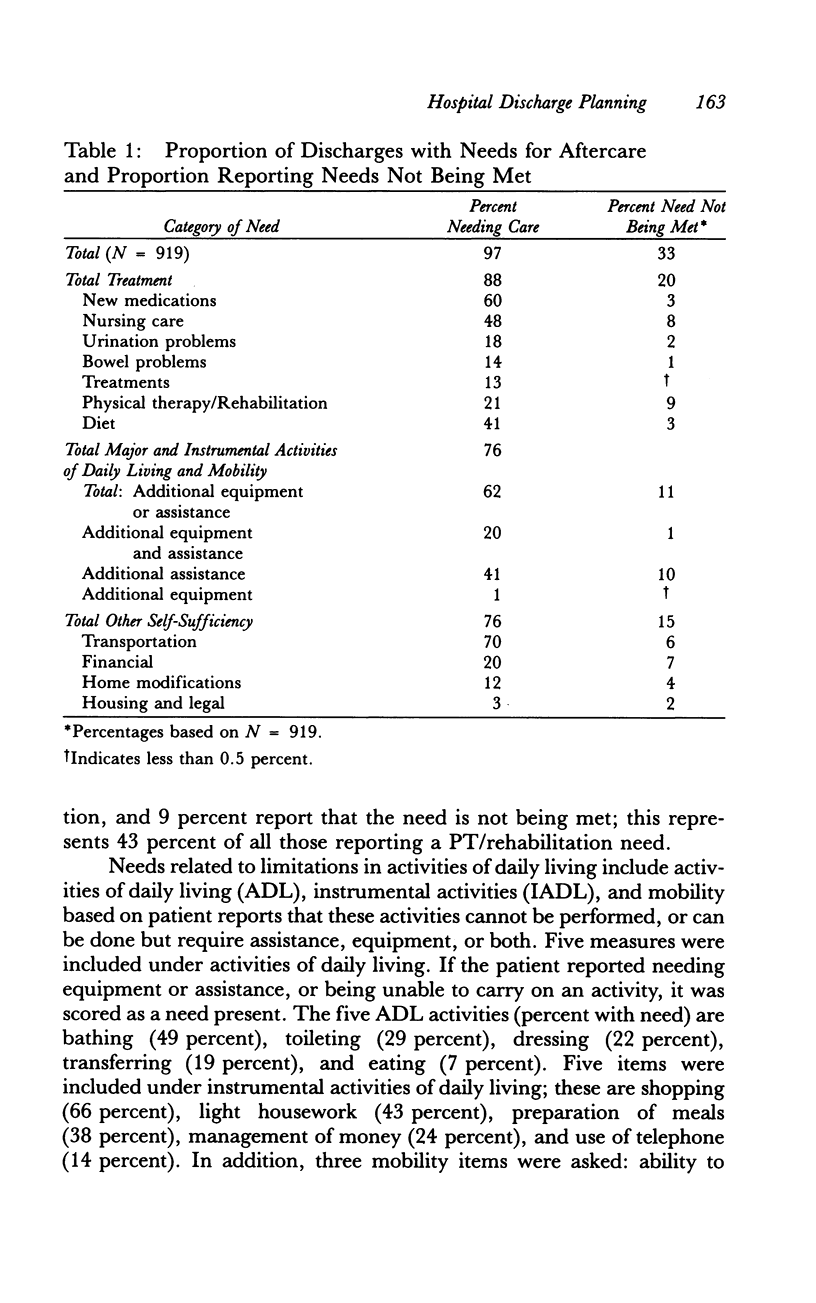
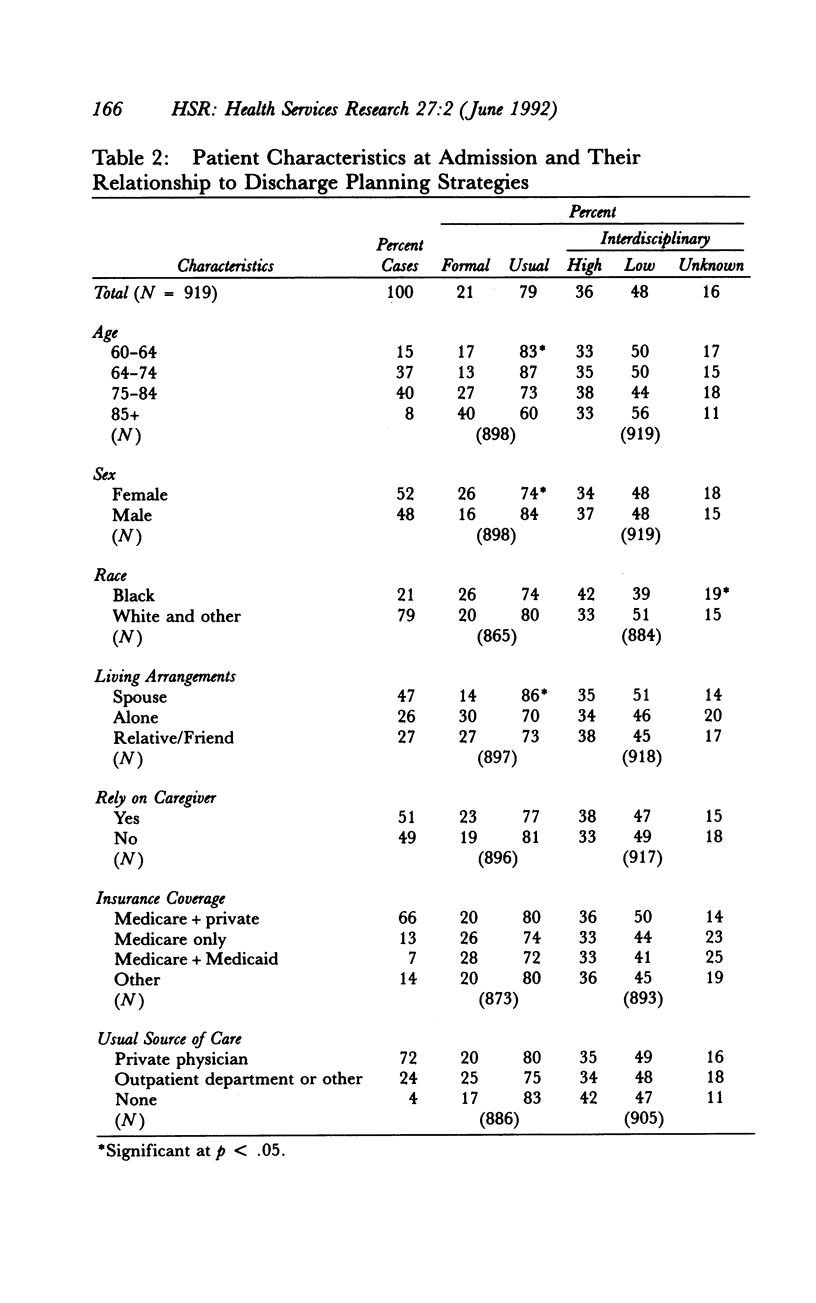
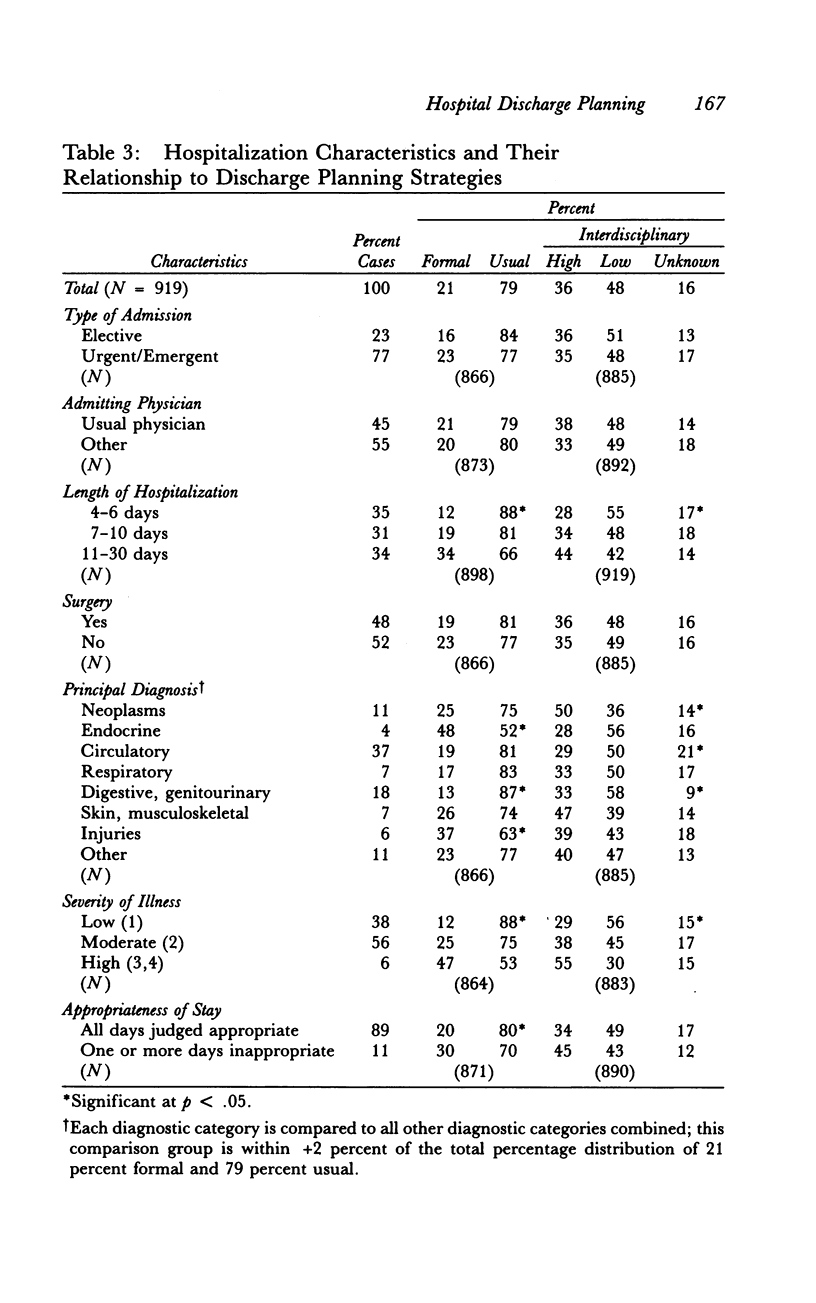
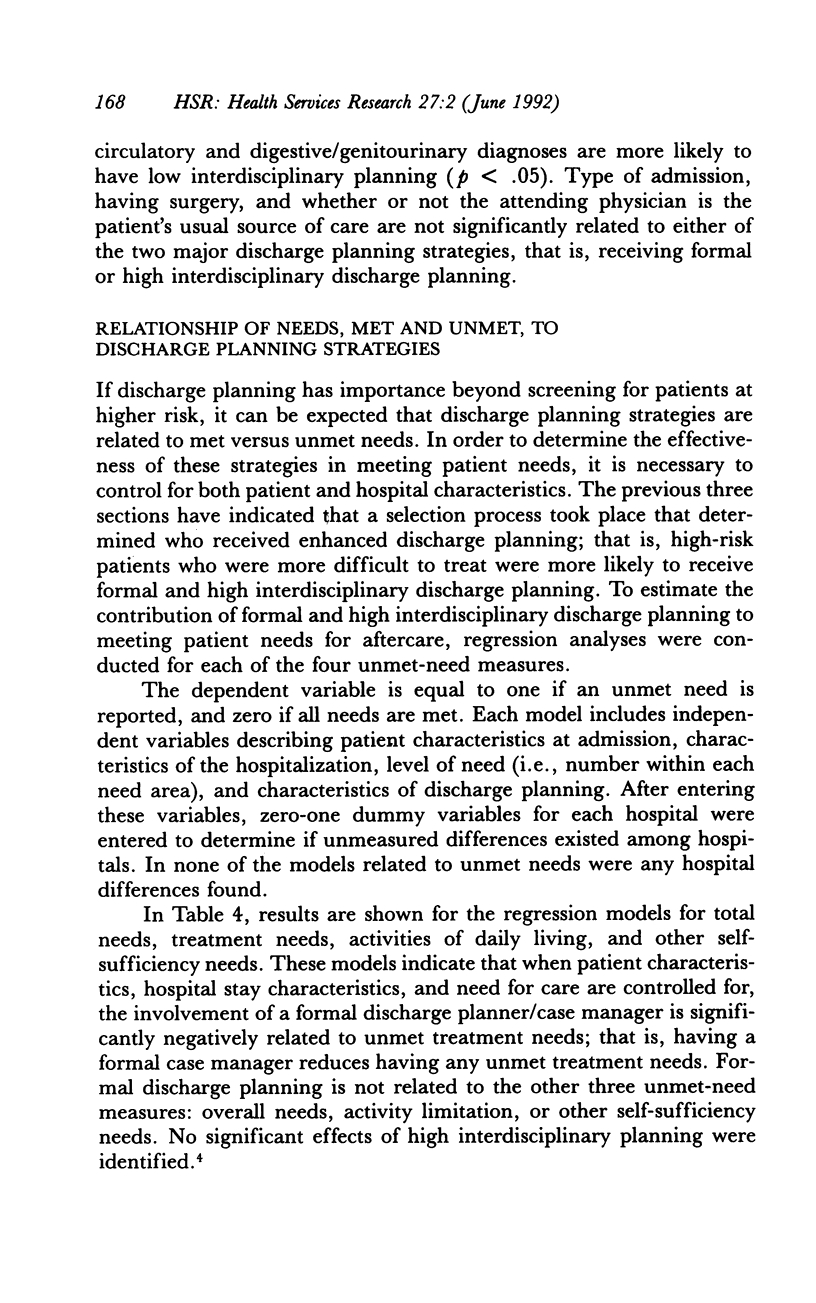
This study examines the contribution of hospital discharge planning in meeting the needs of patients for care after their return home. A random sample of 919 admissions (age 60 and over) to five hospitals was studied to obtain information on characteristics of discharge planning during the patients' hospital stay. Specifically, information was obtained on the involvement of a designated professional for managing and coordinating the discharge plan, and the extent to which the planning was interdisciplinary. Patient interviews conducted two weeks after discharge provided information on needs for care related to: (1) treatment, (2) activity limitations, and (3) other self-sufficiency limitations. Patients were asked about their need for care in these three areas and about whether or not these needs were being met. Overall, 97 percent reported one or more needs for care and 33 percent reported that at least one of these needs was not being met. Findings show that the involvement of a discharge planning case manager is related to a significant reduction in unmet treatment needs, but not to reductions in activity limitation, other self-sufficiency needs, or overall needs. No significant effects of interdisciplinary planning were identified. These findings suggest that treatment-related benefits result when a case manager has specific responsibility for the discharge planning of elderly patients returning home after hospitalization. These results provide insights into what is being achieved through current discharge planning practices. The meeting of specific patient needs through enhanced discharge planning may save future costs by reducing the rates of complications and hospital readmissions in an era of prospective payment, thus potentially offsetting the increased costs involved in planning and coordinating postdischarge care for older adults.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brook R. H., Lohr K. N. Monitoring quality of care in the Medicare program. Two proposed systems. JAMA. 1987 Dec 4;258(21):3138–3141. [PubMed] [Google Scholar]
- Gertman P. M., Restuccia J. D. The appropriateness evaluation protocol: a technique for assessing unnecessary days of hospital care. Med Care. 1981 Aug;19(8):855–871. [PubMed] [Google Scholar]
- Hedrick S. C., Inui T. S. The effectiveness and cost of home care: an information synthesis. Health Serv Res. 1986 Feb;20(6 Pt 2):851–880. [PMC free article] [PubMed] [Google Scholar]
- Horn S. D., Sharkey P. D., Bertram D. A. Measuring severity of illness: homogeneous case mix groups. Med Care. 1983 Jan;21(1):14–30. doi: 10.1097/00005650-198301000-00002. [DOI] [PubMed] [Google Scholar]
- Jones E. W., Densen P. M., Brown S. D. Posthospital needs of elderly people at home: findings from an eight-month follow-up study. Health Serv Res. 1989 Dec;24(5):643–664. [PMC free article] [PubMed] [Google Scholar]
- Kosecoff J., Kahn K. L., Rogers W. H., Reinisch E. J., Sherwood M. J., Rubenstein L. V., Draper D., Roth C. P., Chew C., Brook R. H. Prospective payment system and impairment at discharge. The 'quicker-and-sicker' story revisited. JAMA. 1990 Oct 17;264(15):1980–1983. [PubMed] [Google Scholar]
- Lowe J. I., Herranen M. Understanding teamwork: another look at the concepts. Soc Work Health Care. 1981 Winter;7(2):1–11. doi: 10.1300/j010v07n02_01. [DOI] [PubMed] [Google Scholar]
- Reichelt P. A., Newcomb J. Organizational factors in discharge planning. J Nurs Adm. 1980 Dec;10(12):36–42. [PubMed] [Google Scholar]
- Shine M. S. Discharge planning for the elderly patient in the acute care setting. Nurs Clin North Am. 1983 Jun;18(2):403–410. [PubMed] [Google Scholar]
- Wilson P. A. Expanding the role of social workers in coordination of health services. Health Soc Work. 1981 Feb;6(1):57–64. doi: 10.1093/hsw/6.1.57. [DOI] [PubMed] [Google Scholar]


