Abstract
Computerised cognitive behavioural therapy (CCBT) has been shown to be an efficacious treatment for depression. A recent meta-analysis of 9 studies showed a large mean effect size superiority over control group (effect size=0.86, number needed to treat=2), good adherence (69%) and benefits were evident at follow-up at a median of 26 weeks. In contrast, REEACT, a major study which compared usual general practitioner (GP) care versus usual GP care plus access to 1 of 2 pioneering CCBT courses detected no differences between the groups. We present the results and discuss possible explanations for these findings. In all 3 groups, usual care was extensive (9 visits in 12 months, 80% on medication, 8–23% getting psychological sessions). Adherence to CCBT courses was very poor (17%). Perhaps the surfeit of services meant there was no need for CCBT. Perhaps neither of the 2 CCBT courses encouraged adherence. What is certain is that this study did not test the potential of these CCBT courses to produce change in patients with depression presenting in primary care.
Background
Cognitive behaviour therapy (CBT) has a robust evidence base, and is recommended as the first-line psychotherapy for anxiety and depressive disorders.1–3 However, many people who could potentially benefit from CBT have limited access to qualified clinicians, because of long waitlists and the direct and out of pocket costs of face-to-face treatment.4 The content of CBT is relatively standard, so it has been possible to produce manuals describing the process of CBT for patients and clinicians.1 5 Computers can deliver manualised information. This raised the possibility that a computerised version of a CBT manual (CCBT) could reduce the aforementioned barriers to care.
Waller and Gilbody6 conducted an early systematic review of CCBT and expressed concern: “Studies…show clinical efficacy for treating anxiety and depression, but have not focused on barriers to uptake. Potential barriers include adverse consequences, accessibility and acceptability” (p. 705). They concluded that CCBT programmes had no significant clinical effect at follow-up. There has been significant growth in the development and evaluation of CCBT programmes in the past 6 years, most positive, but a recent large study in primary care—the Randomised Evaluation of the Effectiveness and Acceptability of Computerised Therapy trial (the REEACT trial)7—attributed no benefit from CCBT when added to usual care. The purpose of this paper is to respond to the REEACT trial with reference to the most recent meta-analyses of CCBT in people likely to meet criteria for major depressive disorder.
Methods
We searched for meta-analyses published since the Waller and Gilbody6 review until December 2015 that addressed the use of CCBT in major depressive disorder. We then compared those findings with that of the REEACT trial.7
Results
We found four meta-analyses of people with major depressive disorder that followed the Waller and Gilbody review.
Andrews et al8 reported on six studies of CCBT for people who met diagnostic criteria for a depressive disorder. CCBT was superior over controls (usually wait list; effect size (ES)=0.78) and significant improvement was evident at a median of 9 weeks follow-up. Median adherence was 73%, and 85% of patients were satisfied with their treatment. The authors concluded that CCBT is efficacious, acceptable and practical healthcare.
So et al9 analysed 14 CCBT studies of depressive disorders or depressive symptoms. Five had no therapist support, nine did; six were compared with treatment as usual (TAU), eight to wait list controls. Compared with TAU and waitlist controls, CCBT had a mean ES=0.23 and ES=0.63, respectively. Median adherence was 73%. There was no significant clinical effect at 6-month follow-up.
Arnberg et al10 listed five studies of supported CCBT for people with mild or moderate depressive disorder. The mean effect size superiority over the waitlist control groups was 0.83. Data on adherence and long-term outcome were not reported.
Hedman et al11 identified 20 randomised controlled trials of CCBT for depressive disorder or depressive symptoms with varying levels of clinical support. The mean pre-post change in depressive symptoms in the intervention group was ES=0.94, symptom change in the control groups was not reported. The authors concluded that CCBT for depression met the American Psychiatric Association criteria for a well-established treatment.
We reanalysed the nine studies of participants likely to meet criteria for major depressive disorder listed by Hedman et al11 that compared guided CCBT with wait list controls. As can be seen in table 1, these nine studies included 1282 patients in either guided CCBT or control groups; the unweighted mean effect size superiority of the intervention over control groups was ES=0.86; a median adherence in the intervention group of 69%; and the median follow-up was 26 weeks (range 4–78 weeks) at which time significant benefit was still evident.
Table 1.
Summary statistics of nine studies comparing guided computerised cognitive behavioural therapy for major depression with wait list controls
| n | ES superiority (Intervention) | Adherent (intervention) (%) | Follow-up length (weeks) | |
|---|---|---|---|---|
| Andersson et al19 | 117 | 0.98 | 65 | 26 |
| Berger et al20 | 51 | 1.10 | 56 | 26 |
| Kessler et al21 | 297 | 0.81 | 52 | 16 |
| Meyer et al22 | 396 | 0.65 | 50 | 26 |
| Perini et al23 | 48 | 0.65 | 74 | – |
| Ruwaard et al24 | 54 | 0.70 | 92 | 78 |
| Titov et al25 | 104 | 1.31 | 89 | 16 |
| Vernmark et al26 | 58 | 0.96 | 93 | 26 |
| Warmerden et al27 | 175 | 0.54 | 69 | 4 |
| Mean ES | 0.86 |
ES, effect size.
One of the authors of the present clinical review (GA) is also an author of two of the nine studies presented in table 1. Having declared this conflict of interest we conclude, on the basis of these nine studies, exactly as we did in 2010, that CCBT—with a number needed to treat of 2, benefits evident at 26 weeks follow-up, and high levels of adherence—is efficacious, acceptable and practical healthcare for major depressive disorder. The recently published REEACT trial produced a different result that could potentially challenge this conclusion.
REEACT trial design: Gilbody et al7 conducted the REEACT trial from 2008 to 2015. It is an important study of people with major depression, recruited from primary care practices in England, followed for 2 years, that compared the outcomes of three groups receiving usual general practitioner (GP) care, with two of the groups receiving usual GP care plus access to one of two pioneering efficacious CCBT programmes. GPs knew which patients were in the trial and that the effect of their ‘usual care’ would be measured.
REEACT trial interventions: The first CCBT programme, Beating the Blues, is an eight lesson course designed for primary care.12 The second, MoodGYM, is a six lesson course designed for use without supervision.13 During the REEACT trial, the organisers attempted a median of 13 contacts with people allocated to the CCBT groups to encourage adherence.
REEACT trial results: Adherence was much lower than expected. In the Beating the Blues group, 17% of patients did not start (n=35/210) and only 18% (n=31/175) of those who did start completed all sessions. In the MoodGYM group, 23% (n=56/242) did not start and only 16% (n=29/186) of those who did start completed all sessions. Patients allocated to usual GP care alone had no stated completion requirements.
REEACT trial conclusions: REEACT showed significant reductions in depressive symptoms in all three groups. Half the people no longer met criteria for depression at 4 months, and there was no evidence of overall differences in depression reduction between groups at any time point. The study's authors conclude: “Our main finding is therefore that while CCBT has been shown to be efficacious in developer led trials, it was not effective in usual NHS care settings. The main reason for this was low adherence and engagement with treatment, rather than lack of efficacy” (p. 11).
Commentary on REEACT trial: This study was large and from an experienced group of researchers. The age, characteristics and severity of depression in the participants were as expected in primary care patients. Given previous meta-analytic reviews show that CCBT is efficacious for major depression, the findings of Gilbody et al7 are surprising. They occasioned 17 media headlines in the first week. For example, ‘Questions raised over effectiveness of online CBT for treating depression’ wrote the Guardian cautiously on 11 November 2015 (http://www.theguardian.com/society/2015/nov/11/online-cognitive-behavioural-therapy-questions-effectiveness-treating-depression); but ‘Computerized CBT Not Effective for Depression’ was the usual headline, this one from PsychCentral on 13 November 2015 (http://psychcentral.com/news/2015/11/13/computerized-cbt-not-effective-for-depression/94788.html).
We agree with Gilbody et al7 that the level and type of service provision given to patients as part of usual care, and patients’ adherence (or lack thereof) to CCBT, underlie the REEACT findings. We suggest that because of these two factors, their findings are not indicative of the utility of CCBT for treating major depression.
First, ‘usual GP care’ in this trial was considerable and this did not differ by group allocation (table 9 in Gilbody et al7). Patients in all three groups attended their general practice an average of nine times in the first 12 months; 80% were on medication; and between 8% and 23% got additional psychological services. Although the type of psychological therapy was not reported in the paper, participants who got extra psychological services likely received CBT as part of the Increasing Access to Psychological Services (IAPT) initiative. Clearly patients in this study were fortunate. This level of service provision is not indicative of usual care in developed nations.14 15 For instance, only about one in five Australian adults who receive help for depression in primary care receive ‘minimally adequate treatment’.14 All in the REEACT study would have received much more than minimally adequate treatment. Cuijpers et al16 show that the cumulative effect of multiple treatments for depression is small. It is therefore likely that the unusually high level of service provision in the REEACT trial meant that it was not possible to demonstrate the additional benefit of CCBT from usual care, particularly given that 19% of the usual care group also accessed other CCBT programmes.
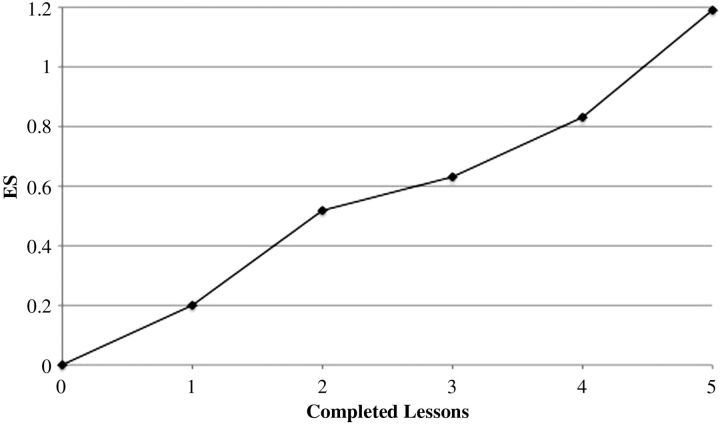
Second, engagement of participants with the CCBT programmes in the REEACT trial was very poor. Contrary to the REEACT study, we have shown that patients who are prescribed CCBT by their GP show significant clinical improvement. Approximately half of the patients who adhere to treatment recover,17 18 and importantly, half of patients who drop out sustain a 0.50 SD benefit.17 Moreover, a minimal level of support (median=1 contact) resulted in adherence of 55%, considerably greater than reported in the REEACT trial that attempted 13 contacts. Furthermore, there was a strong dose–response relationship between the number of completed CCBT sessions and the reduction in the distress associated with depression (see figure 1).17 It seems that the failure to engage REEACT patients in the CCBT programmes may have further obscured the clinical benefit associated with these programmes and could be explained by patient disengagement following a surfeit of usual care services.
Figure 1.
Effect size reductions in the Kessler Psychological Distress Scale (K10) by the number of lessons completed (n=426).14
Footnotes
Contributors: GA, MJH and JMN each contributed to the substantive content of this manuscript.
Funding: JMN was supported by a National Health and Medical Research Council (NHMRC) Early Career Fellowship (1037787).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Andrews G, Dean K, Genderson M, et al. Management of mental disorders. 5th edn. Sydney: Amazon.com, 2014. [Google Scholar]
- 2.National Institute for Health and Clinical Excellence. Depression: management of depression in primary and secondary care. London, UK: National Institute for Health and Clinical Excellence, 2009. [Google Scholar]
- 3.Barlow DH, Farchione TJ, Fairholme CP, et al. Unified protocol for transdiagnostic treatment of emotional disorders: therapist guide (treatments that work). New York: Oxford University Press, 2011. [Google Scholar]
- 4.Anderson R, Wong N, Newby JM, et al. The non-medical out of pocket costs to attend a free anxiety disorders treatment clinic in Australia. Aust Psychiatry Published Online First: 3 Nov 2015 doi:10.1177/1039856215613004 10.1177/1039856215613004 [DOI] [PubMed] [Google Scholar]
- 5.Andrews G, Creamer M, Crino R, et al. The treatment of anxiety disorders: clinician guides and patient manuals. Cambridge, UK: Cambridge University Press, 2003. [Google Scholar]
- 6.Waller R, Gilbody S. Barriers to the uptake of computerized cognitive behavioural therapy: a systematic review of the quantitative and qualitative evidence. Psychol Med 2009;39:705–12. 10.1017/S0033291708004224 [DOI] [PubMed] [Google Scholar]
- 7.Gilbody S, Littlewood E, Hewitt C, et al., REEACT Team. Computerised cognitive behaviour therapy (cCBT) as treatment for depression in primary care (REEACT trial): large scale pragmatic randomised controlled trial. BMJ 2015;351:h5627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andrews G, Cuijpers P, Craske MG, et al. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS ONE 2010;5:e13196. 10.1371/journal.pone.0013196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.So M, Yamaguchi S, Hashimoto S, et al. Is computerised CBT really helpful for adult depression? A meta-analytic re-evaluation of CCBT for adult depression in terms of clinical implementation and methodological validity. BMC Psychiatry 2013;13:113. 10.1186/1471-244X-13-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arnberg FK, Linton SJ, Hultcrantz M, et al. Internet-delivered psychological treatments for mood and anxiety disorders: a systematic review of their efficacy, safety and cost-effectiveness. PLoS ONE 2014;9:e98118. 10.1371/journal.pone.0098118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hedman E, Ljotsson B, Lindefors N. Cognitive behavior therapy via the internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Expert Rev Pharmacoecon Outcomes Res 2012;12:745–64. 10.1586/erp.12.67 [DOI] [PubMed] [Google Scholar]
- 12.Proudfoot J, Goldberg DP, Mann A, et al. Computerised, interactive, multimedia cognitive behavioural therapy for anxiety and depression in general practice. Psychol Med 2003;33:217–27. 10.1017/S0033291702007225 [DOI] [PubMed] [Google Scholar]
- 13.Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: randomised controlled trial. BMJ 2004;328:265. 10.1136/bmj.37945.566632.EE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris MG, Hobbs MJ, Burgess PM, et al. Frequency and quality of mental health treatment for affective and anxiety disorders among Australian adults. Med J Aust 2015;202:185–9. 10.5694/mja14.00297 [DOI] [PubMed] [Google Scholar]
- 15.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: results from The National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:629–40. 10.1001/archpsyc.62.6.629 [DOI] [PubMed] [Google Scholar]
- 16.Cuijpers P, van Straten A, Hollon SD, et al. The contribution of active medication to combined treatments of psychotherapy and pharmacotherapy for adult depression: a meta-analysis. Acta Psychiatr Scand 2010;121:415–23. 10.1111/j.1600-0447.2009.01513.x [DOI] [PubMed] [Google Scholar]
- 17.Mewton L, Andrews G. Cognitive behavior therapy via the internet for depression: a useful strategy to reduce suicidal ideation. J Affect Disord 2015;170:78–84. 10.1016/j.jad.2014.08.038 [DOI] [PubMed] [Google Scholar]
- 18.Williams AD, Andrews G. The effectiveness of internet cognitive behavioral therapy (iCBT) for depression in primary care: a quality assurance study. PLoS ONE 2013;8:e57447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andersson G, Bergstrom J, Hollander F, et al. Internet-based self-help for depression: randomised controlled trial. Br J Psychiatry 2005;187:456–61. 10.1192/bjp.187.5.456 [DOI] [PubMed] [Google Scholar]
- 20.Berger T, Hammerli K, Guber N, et al. Internet-based treatment for depression: a randomized controlled trial comparing guided with unguided self-help. Cogn Behav Ther 2011;40:251–66. 10.1080/16506073.2011.616531 [DOI] [PubMed] [Google Scholar]
- 21.Kessler D, Lewis G, Kaur N, et al. Therapist-delivered internet psychotherapy for depression in primary care: a randomised controlled trial. Lancet 2009;374:628–34. 10.1016/S0140-6736(09)61257-5 [DOI] [PubMed] [Google Scholar]
- 22.Meyer B, Berger T, Casper F, et al. Effectiveness of a novel integrated online treatment for depression (Deprexis): randomized controlled trial. J Med Internet Res 2009;11:e15. 10.2196/jmir.1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perini S, Titov N, Andrews G. Clinician-assisted internet-based treatment is effective for depression: randomized controlled trial. Aust NZ J Psychiatry 2009;43:571–8. 10.1080/00048670902873722 [DOI] [PubMed] [Google Scholar]
- 24.Ruwaard J, Schrieken B, Schrijver M, et al. Standardized web-based cognitive behavioural therapy of mild to moderate depression: a randomized controlled trial with a long-term follow-up. Cogn Behav Ther 2009;38:206–21. 10.1080/16506070802408086 [DOI] [PubMed] [Google Scholar]
- 25.Titov N, Andrews G, Davies M, et al. Internet treatment for depression: a randomized controlled trial comparing clinician vs. technical assistance. PLoS ONE 2010;5:e10939. 10.1371/journal.pone.0010939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vernmark K, Lenndin J, Bjarehed J, et al. Internet administered guided self-help versus individualized email-therapy: a randomised trial of two version of CBT for major depression. Behav Res Ther 2010;48:368–76. 10.1016/j.brat.2010.01.005 [DOI] [PubMed] [Google Scholar]
- 27.Warmerden L, van Straten A, Twisk J, et al. Internet-based treatment for adults with depressive symptoms: randomized controlled trial. J Med Internet Res 2008;10:e44. 10.2196/jmir.1094 [DOI] [PMC free article] [PubMed] [Google Scholar]