Highlights
-
•
SFTSV can be transmitted via oral and ocular routes.
-
•
Mucous membrane is involved in the transmission of SFTSV.
-
•
Blood is the the risk factor for SFTS person-to-person transmission.
Keywords: SFTSV, Nosocomial infection, Person-to-person transmission, Fecal-oral, Fecal-ocular
Abstract
Background
Severe fever with thrombocytopenia syndrome virus (SFTSV) is a tick-borne bunyavirus that could cause a severe hemorrhagic fever termed SFTS with a high fatality rate of up to 30%. Importantly, SFTSV is frequently transmitted from person-to-person and patients’ blood or excreta are considered as the risk factors for transmission of SFTSV. However, the mechanism of person-to-person transmission of SFTSV is still elusive.
Methods
In this study, wild-type (WT) C57BL/6 J mice and a lethal SFTSV mouse model IFNAR−/− A129 mice were utilized to evaluate whether SFTSV could be transmitted via oral or ocular routes. C57BL/6 J mice were inoculated with cell-cultured SFTSV via oral and ocular inoculation. IFNAR−/− A129 mice were inoculated with cell-cultured SFTSV or SFTSV infected mouse acute sera via oral and ocular inoculation.
Results
We found that SFTSV antibody positive rates in C57BL/6 J mice were 70% (7/10) and 30% (3/10) in the oral inoculation group and ocular inoculation group, respectively on day 21 post SFTSV inoculation. The mortality rates of IFNAR−/− mice with oral and ocular inoculation of cell-cultured SFTSV were 100% and 83.33% (5/6), respectively on day 6 post inoculation. The mortality rates of IFNAR−/− mice with oral and ocular inoculation of SFTSV infected mouse acute serum were 100% and 66.67% (4/6), respectively on day 9 post inoculation.
Conclusions
Together, our results show that SFTSV can be transmitted effectively through oral and ocular membrane, suggesting exposure to SFTS positive excreta may be a high-risk factor of nosocomial transmission of SFTSV in hospitals and/or families. Family members and healthcare workers should be protected properly during taking care of SFTS patients to prevent SFTSV nosocomial infection.
1. Introduction
Severe fever with thrombocytopenia syndrome virus (SFTSV) is a negative-strand enveloped RNA virus with virion diameters ranging from 80 to 120 nm, classified under the genus Bandavirus, family Phenuiviridae, order Bunyavirales[1,2]. Typically, SFTSV infection could cause a severe hemorrhagic fever, termed SFTS, with the case fatality rate (CFR) up to 30% [2], [3], [4]. The primary symptoms in SFTS patients include fever, thrombocytopenia, and leukocytopenia[2]. Reported SFTS cases are increasing yearly and the SFTSV epidemic area is expanding worldwide[5,6]. Since 2009, SFTS has been reported in China, South Korea, Japan, and most recently in Vietnam, Thailand, and Pakistan [2,[5], [6], [7], [8], [9]]. Importantly, the World Health Organization (WHO) has declared SFTS as prioritized diseases in 2018. However, no specific vaccines or effective drug are approved for SFTSV prevention or treatments.
Bunyavirus SFTSV virion comprises tripartite RNA genome, designated as the large (L), medium (M), and small (S) RNA segments, respectively, while those RNA genomes contains a pseudo-circular structure owing to the terminal nucleotides of those RNA genomes being partially complementary. Of note, L and M segments are encoded in a negative-sense orientation, while the S segment is encoded in an ambisense manner. Briefly, the L segment encodes the RNA-dependent RNA polymerase involved in the viral RNA replication and mRNA synthesis. The M segment encodes a glycoprotein involved in the entry and assembly of virions. The S segment encodes a non-structural protein in a sense orientation and the nucleocapsid protein in a negative-sense orientation, involved in the virulence, and viral RNA replication and assembly of virions respectively.
SFTSV is a tick-borne virus, and Haemaphysalis longicornis and Ixodes sinensis ticks have been laboratory confirmed as vectors of SFTSV [10,11]. Haemaphysalis longicornis has been spread from Asia to Oceania including Australia and New Zealand hundred years ago and recently to the United States [12,13], indicating that SFTSV may not be only limited to Asia. Importantly, elderly people are prone to SFTSV with high mortality [14], [15], [16]. Like other reported bunyavirus [17,18], SFTS has been documented frequently person-to-person transmission within family and hospital [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32]. Exposure to SFTSV patients’ blood or excreta are the risk factors for SFTS person-to-person transmission [33], while multiple studies indicate that mucosal transmission is important for infection of different viruses[34,35]. Hence, we suspected that person-to-person transmission of SFTSV could be mediated via the mouth or eyelid membranes. In our study, we aim to investigate the routines of person-to-person transmission of SFTSV using mouse infection models.
2. Materials and methods
2.1. Mouse experiments
SFTSV strain JS2014–06 (GenBank: KY362339) was cultured in Vero cells and the frozen virus stock with 2 × 105 plaque-forming unit (PFU)/mL was used in animal experiments. Wild type (WT) C57BL/6 J mice were randomly divided into 6 groups: PBS oral inoculation group (10 mice), inactivated SFTSV oral inoculation group (5 mice), SFTSV oral inoculation group (5 mice), PBS ocular inoculation group (10 mice), inactivated SFTSV ocular inoculation group (5 mice), and SFTSV ocular inoculation group (5 mice). For 50% lethal doses (LD50) calculation, IFNAR−/− A129 mice were challenged with different doses of SFTSV intraperitoneally to monitor the mouse survival rates and to determine the LD50. IFNAR−/− A129 mice were randomly divided into 8 groups (6 mice per groups): PBS oral inoculation group, SFTSV oral inoculation group, PBS ocular inoculation group, and SFTSV ocular inoculation group, as well as mock-serum oral inoculation group, SFTSV-serum oral inoculation group, mock-serum ocular inoculation group, and SFTSV-serum ocular inoculation group.
2.2. Quantitative real-time PCR and enzyme-linked immunosorbent assay (ELISA)
Blood RNA was isolated with TRIzol Reagent (Servicebio, Wuhan, China) and transcribed into cDNA with cDNA Synthesis Kit (Servicebio). Real-time quantitative PCR (RT-qPCR) assays were performed using a ChamQ Universal SYBR qPCR Master Mix (Vazyme, Nanjing, China). The S segment of SFTSV was amplified by RT-PCR (forward primer: 5′ GGGTCCCTGAAGGAGTTGTAAA 3′; reverse primer: 5′ TGCCTTCACCAAGACTATCAATG 3′) [10]. Data were normalized to the β-actin level. Anti-SFTSV total antibodies (IgM and IgG) were tested with a commercial double-antigen sandwich ELISA Kit (Xinlianxin Biotech, Jiangsu, China). The sensitivity and specificity of the kit were 91.7% and 100%, respectively [36].
3. Results
Oral and ocular transmission of SFTSV
To investigate whether SFTSV could be transmitted through mouth and eyelid membranes, C57BL/6 J mice were inoculated with SFTSV via oral inoculation and ocular inoculation, respectively. Heat-inactivated SFTSV and PBS were used as negative controls. Then, to detect whether those mice were infected with SFTSV successfully, blood samples were collected from those mice on day 3, 10, and 21 post infection (DPI). SFTSV RNA and SFTSV antibodies were then detected by RT-PCR and ELISA, respectively. Interestingly, we observed that, on DPI 3, 1 mouse in the oral SFTSV inoculation group were tested RT-PCR positive to SFTSV (Table 1). Importantly, WT C57BL/6 J mice are highly resistant to SFTSV infections [37,38], which could explain the low positive rate of SFTSV RNA detection. Moreover, we found that, on DPI 21, SFTSV antibody positive rates were 70% (7/10) and 30% (3/10) in the oral inoculation group and ocular inoculation group, respectively (Table 1), indicating SFTSV was effectively transmitted to mice through oral and ocular inoculation routes.
Table 1.
Numbers of wild type C57BL/6 J mice with SFTSV RNA and anti-SFTSV antibodies in inoculation experiments.
| Inoculation type | N | RNA-positive on DPI 3 | RNA-positive on DPI 10 or 21 | Antibodies-positive on DPI 21 |
|---|---|---|---|---|
| Virus treatment | ||||
| Oral inoculation | 10 | 1 | 0 | 7 |
| Ocular inoculation | 10 | 0 | 0 | 3 |
| Inactivated virus control | ||||
| Oral inoculation | 5 | 0 | 0 | 0 |
| Ocular inoculation | 5 | 0 | 0 | 0 |
| PBS control | ||||
| Oral inoculation | 5 | 0 | 0 | 0 |
| Ocular inoculation | 5 | 0 | 0 | 0 |
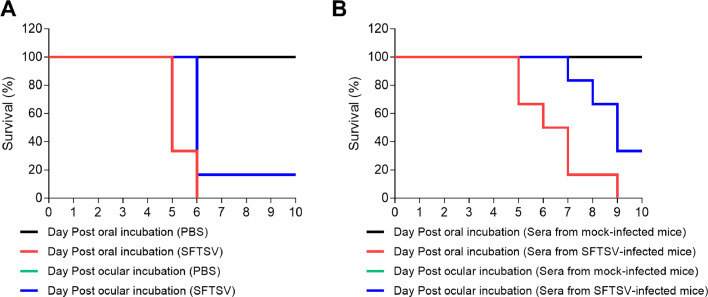
Due to the wild type mice are resistance to SFTSV infection, we further challenged type I interferon receptor knockout (IFNAR−/− A129) mice, a lethal SFTSV mouse model, with SFTSV through oral or ocular inoculation [39]. Interestingly, we found that the mortality rates of IFNAR−/− mice with oral and ocular inoculation of SFTSV were 100% and 83.33%, respectively on 6 DPI (Fig. 1A). To further investigate whether the SFTSV infected mouse acute serum could also be transmitted through oral and ocular membrane routes in IFNAR−/− A129 mice, acute sera were isolated from blood of IFNAR−/−mice, which was collected from the medial canthus after anesthesia 4 days after the mice were infected with 10 LD50 of SFTSV intraperitoneally. Then, IFNAR−/− A129 mice were challenged with the acute sera of SFTSV-infected mice or the sera of PBS-mock infected mice through oral and ocular membrane inoculation. Consistent with the result above, the mortality rates of IFNAR−/− mice with oral and ocular inoculation of SFTSV serum were 100% and 66.67%, respectively on 9 DPI (Fig. 1B). Together, our data demonstrated that SFTSV could be transmitted via oral and ocular routes in mice.
Fig. 1.
IFNAR−/− mice were challenged with cell-cultivated SFTSV (A) or sera of SFTSV- infected mice (B) via oral or ocular innoculation (6 mice per groups). Survival of mice was monitored up to 7 days. Kaplan–Meier survival curves were obtained using GraphPad. SFTSV, Severe fever with thrombocytopenia syndrome virus. Color version of figure is available online.
4. Discussion
SFTS is a tick-borne hemorrhagic fever disease which is frequently transmitted from person to person or from animals to humans. However, the mechanism of SFTSV transmission between persons or between humans and animals were not clear. Our results showed that through ocular oral and ocular inoculation, wild type mice that are resistance to SFTSV infection could develop antibody to SFTSV, suggesting wild type mice can be infected through oral and ocular membrane; in a lethal mouse model, most IFNAR−/− mice eventually died when exposing to SFTSV through oral or ocular routes, further confirming that mice are infected through oral and ocular membranes.
Most index patients in SFTSV cluster infection died in the early phase of SFTS and exhibited hemorrhagic symptoms [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], indicating that viral load may be associated with the occurrence of SFTSV cluster infection. An epidemiological investigation based on 2096 SFTS patients showed that CFR of SFTS was associated with the viral load [3]. SFTSV could be detected in patients’ excreta like blood, urine, and fecal specimens [40]. Of those reported secondary SFTS patients, most individuals had SFTS patients’ blood-contacting history directly or indirectly[19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], suggesting that SFTS transmission may be mediated via blood contact. However, few secondary cases had an entry wound when contacting the blood of SFTS patients. Patients’ excreta might only play a role as contaminated material to spread SFTSV from SFTS patients to naïve individuals in reported cluster infection. Importantly, SFTSV RNA was also detected in serum, eye swab, and oral swabs in SFTSV-infected animals [41,42]. In addition, our studies showed that oral incubation could be more effectively to promote the transmission of SFTSV than ocular incubation. The precise mechanisms by which SFTSV interacts with ocular or oral mucous membrane remain largely elusive. Further study is necessary to assess the potential SFTSV entry receptor in ocular or oral mucous membranes.
Our study clearly showed that SFTSV could be transmitted via oral or ocular membranes. Considering most secondary SFTS patients having exposure history to the index patients’ blood or excreta and the results of our experiments, we concluded that person-to-person transmission of SFTSV may be via oral or ocular routes through the mucous membranes. To avoid nosocomial transmission, better management of SFTSV patients’ excreta is necessary and healthcare workers and family members should wear adequate personal protective equipment when contacting SFTS patients.
Declaration of competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
This study was supported by the National Natural Science Funds of China (81971939 and 31570167) and the Fundamental Research Funds for the Central Universities (2042021kf0046). The funders had no role in the study design, data collection and analysis, decision to publish, or the preparation of the manuscript.
Ethics statement
Animal study was approved by the ethics committees of Wuhan University (2019YF2013). Experiments with SFTSV were performed and approved in a biosafety laboratory at Wuhan University.
Contributor Information
Xiao-Ying Lei, Email: leixy@sdu.edu.cn.
Xue-Jie Yu, Email: yuxuejie@whu.edu.cn.
References
- 1.Kuhn J.H., Adkins S., Alioto D., et al. 2020 taxonomic update for phylum Negarnaviricota (Riboviria: orthornavirae), including the large orders Bunyavirales and Mononegavirales. Arch. Virol. 2020;165(12):3023–3072. doi: 10.1007/s00705-020-04731-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yu X.J., Liang M.F., Zhang S.Y., et al. Fever with thrombocytopenia associated with a novel bunyavirus in China. N. Engl. J. Med. 2011;364(16):1523–1532. doi: 10.1056/NEJMoa1010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li H., Lu Q.B., Xing B., et al. Epidemiological and clinical features of laboratory-diagnosed severe fever with thrombocytopenia syndrome in China, 2011-17: a prospective observational study. Lancet Infect. Dis. 2018;18(10):1127–1137. doi: 10.1016/S1473-3099(18)30293-7. [DOI] [PubMed] [Google Scholar]
- 4.Yu X.J. Risk factors for death in severe fever with thrombocytopenia syndrome. Lancet Infect. Dis. 2018;18(10):1056–1057. doi: 10.1016/S1473-3099(18)30312-8. [DOI] [PubMed] [Google Scholar]
- 5.Tran X.C., Yun Y., Van An L., et al. Endemic severe fever with thrombocytopenia syndrome, Vietnam. Emerging Infect. Dis. 2019;25(5):1029–1031. doi: 10.3201/eid2505.181463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ongkittikul S., Watanawong R., Rompho P. Severe Fever with Thrombocytopenia Syndrome Virus: the First Case Report in Thailand. BKK Med. J. 2020;16(2):204. 2020. [Google Scholar]
- 7.Kim K.H., Yi J., Kim G., et al. Severe fever with thrombocytopenia syndrome, South Korea, 2012. Emerging Infect. Dis. 2013;19(11):1892–1894. doi: 10.3201/eid1911.130792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Takahashi T., Maeda K., Suzuki T., et al. The first identification and retrospective study of Severe Fever with Thrombocytopenia Syndrome in Japan. J. Infect. Dis. 2014;209(6):816–827. doi: 10.1093/infdis/jit603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zohaib A., Zhang J., Saqib M., et al. Serologic evidence of severe fever with thrombocytopenia syndrome virus and related viruses in Pakistan. Emerg. Infect. Dis. 2020;26(7):1513–1516. doi: 10.3201/eid2607.190611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luo L.M., Zhao L., Wen H.L., et al. Haemaphysalis longicornis Ticks as Reservoir and Vector of Severe Fever with Thrombocytopenia Syndrome Virus in China. Emerg. Infect. Dis. 2015;21(10):1770–1776. doi: 10.3201/eid2110.150126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hu Y.Y., Zhuang L., Liu K., et al. Role of three tick species in the maintenance and transmission of Severe Fever with Thrombocytopenia Syndrome Virus. PLoS Negl. Trop. Dis. 2020;14(6) doi: 10.1371/journal.pntd.0008368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hutcheson H.J., Dergousoff S.J., LR Lindsay. Haemaphysalis longicornis: a tick of considerable veterinary importance, now established in North America. Can. Vet. J. 2019;60(1):27–28. [PMC free article] [PubMed] [Google Scholar]
- 13.Raghavan R.K., Barker S.C., Cobos M.E., et al. Potential spatial distribution of the newly introduced long-horned tick, haemaphysalis longicornis in North America. Sci. Rep. 2019;9(1):498. doi: 10.1038/s41598-018-37205-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akbar A.N., DW Gilroy. Aging immunity may exacerbate COVID-19. Science. 2020;369(6501):256–257. doi: 10.1126/science.abb0762. [DOI] [PubMed] [Google Scholar]
- 15.Chen Y., Klein S.L., Garibaldi B.T., et al. Aging in COVID-19: vulnerability, immunity and intervention. Ageing. Res. Rev. 2021;65 doi: 10.1016/j.arr.2020.101205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ding S., Niu G., Xu X., et al. Age is a critical risk factor for severe fever with thrombocytopenia syndrome. PLoS ONE. 2014;9(11) doi: 10.1371/journal.pone.0111736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ergonul O., Celikbas A., Dokuzoguz B., et al. Characteristics of patients with Crimean-Congo hemorrhagic fever in a recent outbreak in Turkey and impact of oral ribavirin therapy. Clin. Infect. Dis. 2004;39(2):284–287. doi: 10.1086/422000. [DOI] [PubMed] [Google Scholar]
- 18.Martinez V.P., Di Paola N., DO Alonso, et al. Super-Spreaders" and Person-to-Person Transmission of Andes Virus in Argentina. N. Engl. J. Med. 2020;383(23):2230–2241. doi: 10.1056/NEJMoa2009040. [DOI] [PubMed] [Google Scholar]
- 19.Bao C.J., Guo X.L., Qi X., et al. A family cluster of infections by a newly recognized bunyavirus in eastern China, 2007: further evidence of person-to-person transmission. Clin. Infect. Dis. 2011;53(12):1208–1214. doi: 10.1093/cid/cir732. [DOI] [PubMed] [Google Scholar]
- 20.Chen H., Hu K., Zou J., et al. A cluster of cases of human-to-human transmission caused by severe fever with thrombocytopenia syndrome bunyavirus. Int. J. Infect. Dis. 2013;17(3):e206–e2e8. doi: 10.1016/j.ijid.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 21.Gong Z., Gu S., Zhang Y., et al. Probable aerosol transmission of severe fever with thrombocytopenia syndrome virus in southeastern China. Clin. Microbiol. Infect. 2015;21(12):1115–1120. doi: 10.1016/j.cmi.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 22.Huang D., Jiang Y., Liu X., et al. A cluster of symptomatic and asymptomatic infections of severe fever with thrombocytopenia syndrome caused by person-to-person transmission. Am. J. Trop. Med. Hyg. 2017;97(2):396–402. doi: 10.4269/ajtmh.17-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jiang X.L., Zhang S., Jiang M., et al. A cluster of person-to-person transmission cases caused by SFTS virus in Penglai, China. Clin. Microbiol. Infect. 2015;21(3):274–279. doi: 10.1016/j.cmi.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 24.Jung I.Y., Choi W., Kim J., et al. Nosocomial person-to-person transmission of severe fever with thrombocytopenia syndrome. Clin. Microbiol. Infect. 2019;25(5):633. doi: 10.1016/j.cmi.2019.01.006. e1- e4. [DOI] [PubMed] [Google Scholar]
- 25.Kim W.Y., Choi W., Park S.W., et al. Nosocomial transmission of severe fever with thrombocytopenia syndrome in Korea. Clin. Microbiol. Infect. 2015;60(11):1681–1683. doi: 10.1093/cid/civ128. [DOI] [PubMed] [Google Scholar]
- 26.Liu Y., Li Q., Hu W., et al. Person-to-person transmission of severe fever with thrombocytopenia syndrome virus. Vector Borne Zoonotic Dis. 2012;12(2):156–160. doi: 10.1089/vbz.2011.0758. [DOI] [PubMed] [Google Scholar]
- 27.Moon J., Lee H., Jeon J.H., et al. Aerosol transmission of severe fever with thrombocytopenia syndrome virus during resuscitation. Infect. Control Hosp. Epidemiol. 2018:1–4. doi: 10.1017/ice.2018.330. [DOI] [PubMed] [Google Scholar]
- 28.Wang Y., Deng B., Zhang J., et al. Person-to-person asymptomatic infection of severe fever with thrombocytopenia syndrome virus through blood contact. Intern. Med. 2014;53(8):903–906. doi: 10.2169/internalmedicine.53.1164. [DOI] [PubMed] [Google Scholar]
- 29.Yoo J.R., Choi J.H., Kim Y.R., et al. Occupational risk of severe fever with thrombocytopenia syndrome in healthcare workers. Open Forum Infect. Dis. 2019;6(5):ofz210. doi: 10.1093/ofid/ofz210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoo J.R., Lee K.H., ST Heo. Surveillance results for family members of patients with severe fever with thrombocytopenia syndrome. Zoonoses Public Health. 2018;65(8):903–907. doi: 10.1111/zph.12481. [DOI] [PubMed] [Google Scholar]
- 31.Zhu Y., Wu H., Gao J., et al. Two confirmed cases of severe fever with thrombocytopenia syndrome with pneumonia: implication for a family cluster in East China. BMC Infect. Dis. 2017;17(1):537. doi: 10.1186/s12879-017-2645-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gong L., Song D.D., Wu J.B., et al. Human-to-human transmissions of severe fever with thrombocytopenia syndrome virus in Anhui province, 2010-2017. Clin Microbiol. Infect. 2018;24(8):920–922. doi: 10.1016/j.cmi.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 33.Ye C., Qi R. Risk factors for person-to-person transmission of severe fever with thrombocytopenia syndrome. Infect. Control Hosp. Epidemiol. 2021;42(5):582–585. doi: 10.1017/ice.2020.1258. [DOI] [PubMed] [Google Scholar]
- 34.Newman C.M., Dudley D.M., Aliota M.T., et al. Oropharyngeal mucosal transmission of Zika virus in rhesus macaques. Nat. Commun. 2017;8(1):169. doi: 10.1038/s41467-017-00246-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garcia-Nicolas O., Braun R.O., Milona P., et al. Targeting of the nasal mucosa by japanese encephalitis virus for non-vector-borne transmission. J. Virol. 2018;92(24) doi: 10.1128/JVI.01091-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu J.-.W., Wen H.-.L., Fang L.-.Z, et al. Prevalence of SFTSV among Asian house shrews and rodents, China, January–August 2013. Emerg. Infect. Dis. 2014;20(12):2126. doi: 10.3201/eid2012.141013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Matsuno K., Orba Y., Maede-White K., et al. Animal Models of Emerging Tick-Borne Phleboviruses: determining Target Cells in a Lethal Model of SFTSV Infection. Front. Microbiol. 2017;8(104) doi: 10.3389/fmicb.2017.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jin C., Liang M., Ning J., et al. Pathogenesis of emerging severe fever with thrombocytopenia syndrome virus in C57/BL6 mouse model. Proc. Natl. Acad. Sci. U.S.A. 2012;109(25):10053–10058. doi: 10.1073/pnas.1120246109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu Y., Wu B., Paessler S., et al. The pathogenesis of severe fever with thrombocytopenia syndrome virus infection in alpha/beta interferon knockout mice: insights into the pathologic mechanisms of a new viral hemorrhagic fever. J. Virol. 2014;88(3):1781–1786. doi: 10.1128/JVI.02277-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang Y.Z., He Y.W., Dai Y.A., et al. Hemorrhagic fever caused by a novel Bunyavirus in China: pathogenesis and correlates of fatal outcome. Clin. Infect. Dis. 2012;54(4):527–533. doi: 10.1093/cid/cir804. [DOI] [PubMed] [Google Scholar]
- 41.Park S.C., Park J.Y., Choi J.Y., et al. Pathogenicity of severe fever with thrombocytopenia syndrome virus in mice regulated in type I interferon signaling: severe fever with thrombocytopenia and type I interferon. Lab. Anim. Res. 2020;36(38) doi: 10.1186/s42826-020-00070-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Park E.S., Shimojima M., Nagata N., et al. Severe Fever with Thrombocytopenia Syndrome Phlebovirus causes lethal viral hemorrhagic fever in cats. Sci. Rep. 2019;9(1):11990. doi: 10.1038/s41598-019-48317-8. [DOI] [PMC free article] [PubMed] [Google Scholar]