Abstract
AIM
To evaluate the effect of symmetrical arc incision correcting corneal astigmatism in femtosecond laser-assisted phacoemulsification (FLACS).
METHODS
This study enrolled patients with cataract combined with regular corneal astigmatism of >0.75 D, who underwent FLACS. Symmetrical arc incision was set at 8 mm diameter and 85% depth. The follow-up time was 3-24mo (4.92±3.49mo). Pentacam recorded the corneal astigmatism and higher-order aberration at pre-operation and post-operation. The changes in corneal astigmatism were analyzed by Alpins method. The correlation of astigmatism type, age, corneal horizontal diameter, corneal thickness, arc incision length, and correction index (CI) was analyzed, and the residual corneal astigmatism was compared with the residual whole eye astigmatism.
RESULTS
Totally 79 patients (102 eyes) were enrolled, 10 patients had corneal epithelial injury, 1 patient occurred corneal epithelial hyperplasia. The corneal astigmatism was 1.23±0.38 D pre-operation, and decreased to 0.76±0.39 D post-operation (t=10.146, P=0.000). Corneal high-order aberration was 0.17±0.08 µm pre-operation and 0.24±0.11 µm post-operation (t=-5.186, P=0.000). The residual corneal astigmatism and residual whole eye astigmatism were no significant difference (t=-0.347, P=0.729). Using Alpin's method, the following were determined: target-induced astigmatism (TIA) =1.23±0.38 D, surgery-induced astigmatism (SIA) =0.77±0.45 D, difference vector (DV)=0.77±0.39 D, and CI=0.54±0.28. Age, astigmatism size, corneal horizontal diameter, corneal thickness, and arc incision length were not correlated with CI. The CI for against the rule astigmatism (ATR) was better than that for with the rule astigmatism (WTR; P=0.001).
CONCLUSION
Femtosecond laser-assisted astigmatic keratotomy has better CI of ATR, but increase higher-order corneal aberration. CI is not ideal, it's not a perfect choice if we pursue ideal correction effect.
Keywords: femtosecond laser arc incision keratotomy, astigmatism, cataract, higher-order aberrations
INTRODUCTION
Refractive cataract surgery requires correcting myopia, hyperopia, astigmatism and presbyopia during the operation, in order to restore good vision for patients. Epidemiology studies have revealed that the proportion of cataract patients with corneal astigmatism of ≥1.0 D before surgery ranges within 34.0%-47.27%[1]. The existence of corneal astigmatism remains an obstacle to achieve excellent visual quality. Thus, it remains challenging for ophthalmologists to consider the treatment of corneal astigmatism before cataract surgery. In addition, the corneal astigmatism would affect the use of intraocular lenses (IOL) for presbyopia. Thus, some patients may not be able to take off their lenses after surgery. Although astigmatism combined with multifocal IOL can be used, clinical application of astigmatism multifocal IOL has high requirements, the operation is relatively complicated, and there is risk of IOL rotation postsurgery. Hence, identifying an effective and accurate method to correct the corneal astigmatism in cataract surgery has become a hot topic. At present, the methods for simultaneous astigmatism correction in cataract surgery include the implantation of toric IOL and arc incision on the steep axis of the cornea. Studies have revealed that toric IOL and arc incision are equally effective for correcting low and moderate astigmatism[2]–[3]. Recent years, femtosecond laser-assisted phacoemulsification (FLACS) has become increasingly popular. Compared to manual incision, incision made using femtosecond laser is more accurate and controllable. Therefore, the effect of femtosecond laser-assisted astigmatic keratotomy (FSAK) has gradually attracted attention. At present, arc incisions performed using a femtosecond laser can be classified into two types: penetrating femtosecond laser-assisted astigmatic keratotomy (pFSAK) and intrastromal FSAK (iFSAK). The present study evaluated the effect of symmetrical, double-arc and separate pFSAK with a consistent design.
SUBJECTS AND METHODS
Ethical Approval
The study design was a retrospective study set in Aier Eye Hospital affiliated Jinan University and was conducted in accordance with the ethical norms and standards in the Declaration of Helsinki and written informed consent was obtained from all subjects. The present study was approved by the Ethics Committee of Shenzhen Aier Eye Hospital Affiliated to Jinan University (No.2020-004-01).
Study Design and Patients
The descriptive study enrolled patients who underwent femtosecond laser cataract surgery combined with arc incision to correct the corneal astigmatism from January 2020 to August 2022. Inclusive criteria: the Pentacam imaging revealed that the front astigmatism in the 4-mm area of the cornea was >0.75 D, which was a regular astigmatism, and symmetric double arc corneal incision was performed to correct the corneal astigmatism, the follow-up time reached or exceeded 3mo. Exclusion criteria: 1) patients with corneal scars, corneal degeneration, corneal dystrophy, a history of corneal surgery, severe dry eye, or glaucoma; 2) patients who received single-arc incision to correct the corneal astigmatism. In addition, preoperative visual acuity examination, slit lamp examination, intraocular pressure examination, fundus examination, IOL power measurement, corneal topography, and corneal endothelium were performed. The routine follow-up time is: 1wk, 1, 3, 6, 12, and 24mo, but some patients failed to meet this requirement. The observation time of the cases included in this study is at least 3mo. During the follow-up visit , all patients underwent visual acuity, optometry, intraocular pressure, slit lamp and Pentacam imaging to measure the corneal topography.
Procedure for FLACS Combined with FSAK
All surgeries were performed by the same experienced surgeon using the LenSx femtosecond laser system (Version 2.31; Alcon, USA), and the Centurion (Alcon, USA) or Infiniti (Alcon, USA) phacoemulsification machine. Before surgery, all eyes received 0.3% levofloxacin and pranoprofen eye drops for four times a day, for three days. On the day of surgery, tropicamide eye drops were given to fully dilate the pupils and proparacaine hydrochloride was used for topical anesthesia. Patients were placed in supine, eyelid opener was placed. The general main incision position was set to 130-160 (adjusted according to the patient's astigmatism correction design), with three planes and a size of 2.6 mm; the arc incision was symmetrical double arc with 85% depth. Next, the incision length and position were entered. According to the corneal curvature, the appropriate patient interface (PI) was chosen, and the patients were instructed and guided to complete the docking and suction procedures. Real-time optical coherence tomography (OCT) was used to verify and confirm the parameters, and a laser was emitted to complete the operation. Afterwards, the patient underwent phacoemulsification. Subsequently, a disinfection towel was placed, and 5% povidone iodine was applied on the conjunctival sac for 30s. The Sima' instrument (one of the utility patents of the authors) was used to open the primary incision. Then, the anterior chamber was filled with viscoelastic, a secondary incision was performed using a 15 corneal puncture knife at the 2:30 o'clock position, the anterior capsule was taken out using capsulorhexis forceps and was separated with water, the nucleus was removed by phacoemulsification, suction was performed on the cortex, the corneal arc incision was separated after filling the viscoelastic and washed, the IOL was implanted in the capsular bag, the viscoelastic was removed, and the corneal incision was sealed with water. Tobramycin dexamethasone eye ointment was applied to the conjunctival sac to cover the eyes. The occurrence of intraoperative and postoperative complications was recorded.
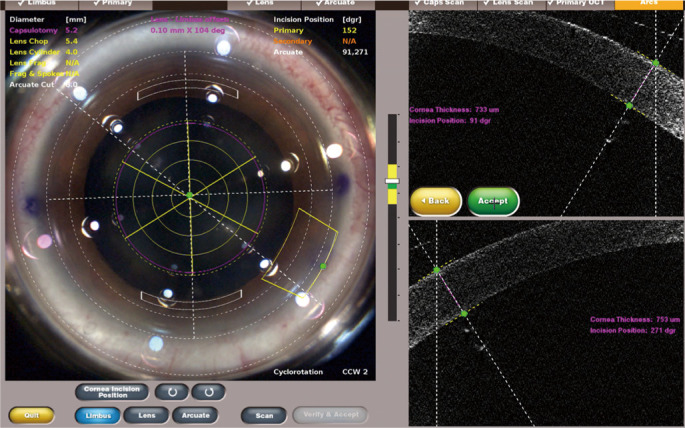
pFSAK Design
The target correction amount of corneal astigmatism before the operation was entered into the online calculator (http://www.lricalculator.com), according to the front surface astigmatism value of the central 4 mm area in the Pentacam imaging, and the nomogram algorithm was selected. Surgery-induced astigmatism (SIA) was the centroid value calculated by the surgeon's personalized femtosecond laser incision in the past. Then, 0.3 was entered. If the position of the arc-shaped incision needs to be repeated using the primary incisions, the position of the primary incision was appropriately adjusted. The calculation method used for the conversion arc with a diameter of 8.0 mm was, as follows: multiply the calculated value by 8/10. Before the operation, the patient was instructed to sit in front of the slit lamp with the head vertically aligned, and the corneal limbus was marked at the 0°, 180°, and primary incision position using a sterile marker pen. Parameter settings for the femtosecond laser machine: Laser energy was 3.0 µJ, side cut angle was 90°, spot separation was 4 µm, laser separation was 5 µm. The incision depth was set to 85%, and the arc diameter was set to 8.0 mm. An example of the pFSAK is presented in Figure 1.
Figure 1. An example of correcting corneal astigmatism with symmetrical arc incision in femtosecond laser-assisted cataract surgery.
Vector Analysis of Corneal Astigmatic Changes
The corneal astigmatism correction effect was analyzed using Alpin's method[4] at three months post-operation. Then, the online calculation was performed (ASSORT group analysis calculator website: https://www.isrs.org/resources/assort-group-analysis-calculator)[5]. The three basic vectors in Alpin's method: 1) Target-induced astigmatism (TIA), defined as the astigmatism change that the surgery was intended to induce. The target astigmatism for the present study was 0. Therefore, the size of the TIA was equal to the preoperative corneal astigmatism. 2) SIA, defined as the astigmatism actually caused by surgery. 3) Difference vector (DV) refers to the difference (including the size and direction) between TIA and SIA. Since the target astigmatism is 0, the DV size is usually equal to the postoperative corneal astigmatism. Other parameters calculated from the three basic parameters: 1) error angle (AE), namely, the vector difference between SIA and TIA, that is, the difference in direction and magnitude between the actual result and expected result (AE=0 indicates that there is no dislocation). A positive AE indicates that the axis of the SIA moves counterclockwise relative to the TIA, and a negative AE indicates that the axis of the SIA moves clockwise relative to the TIA. 2) Correction index (CI), 3) adjustment coefficient (CA), the ratio of SIA to TIA (the ideal value is 1; CI>1 indicates overcorrection, CI<1 indicates insufficient correction). CA is defined as the ratio of TIA to SIA, which is the reciprocal of CI. CA can be used to provide guidance for future operations. Both CI and CA are ratios, and the geometric average needs to be calculated. 4) Index of success (IOS), the ratio of DV to TIA, indicating the success of the astigmatism correction. The smaller the value, the smaller the difference between the surgical results and target.
Statistical Analysis
SPSS 26.0 was used for the statistical analysis. Numerical data was expressed as mean±standard deviation (SD), and percentage data was expressed in percentage. The corneal astigmatism at pre-operation and three months post-operation were compared by paired sample t-test. The magnitudes of residual astigmatism in the whole eye and cornea after the operation were compared using independent sample t-test. The relationship between CI and age, corneal horizontal meridian, central corneal thickness, and preoperative astigmatism degree was determined using linear correlation. Spearman grade correlation was used to determine the relationship between arc incision length and CI. Variance analysis was used to compare CI among the different types of astigmatism, and the Bonferroni method was used for pair comparisons after the variance analysis. P-value of <0.05 was considered statistically significant.
RESULTS
A total of 79 patients (102 eyes) were included for the present study. No corneal penetration during the operation, 10 patients had slight corneal epithelial injury when the arc incision was separated, this maybe caused by the incorrect eye position during operation, and the deviation of the cutting position during making arc incision by laser, which leads to some difficulties in separation and epithelial injury. One day after operation, corneal epithelial defects near the arc incision appeared in 4 eyes, patients had some foreign body sensation and recovered after a few days. Two weeks after operation, corneal epithelial hyperplasia occurred in one patient, which disappeared after being dropped by corticosteroid, consider that this maybe related to incomplete washing after incision separation. No patient was infected.
Astigmatic Change
Table 1 presents the basic data of the patients. The corneal topography revealed that the corneal astigmatism decreased from 1.23±0.38 D before the operation to 0.76±0.39 D at three months after the operation (t=10.146, P=0.000). The higher-order corneal aberration increased from 0.17±0.08 um before the operation to 0.24±0.11 µm after the operation (t=-5.186, P=0.000). However, there was no significant difference between the postoperative corneal astigmatism and residual astigmatism of the whole eye (t=-0.347, P=0.729), indicating that there was consistency between the residual corneal astigmatism and residual astigmatism, in terms of evaluating the correction effect of the FSAK.
Table 1. Patient demographics and biometric parameters.
| Parameters | Mean±SD (range) |
| Age | 59.48±12.09 (24-81) |
| Female | 66 (64.71%) |
| Right eye | 46 (45.10%) |
| Follow-up time (3- <6mo) | 52 (50.98%) |
| Follow-up time (6- <12mo) | 30 (29.41%) |
| Follow-up time (12-24mo) | 20 (19.61%) |
| With the rule astigmatism | 64 (62.74%) |
| Aginst the rule astigmatism | 33 (32.35%) |
| Oblique astigmatism | 5 (4.90%) |
| Central corneal thickness, µm | 547.41±30.39 (468-618) |
| Periph cornea thickness, µm | 639.50±43.67 (491-751) |
| Corneal horizontal diameter, µm | 11.40±0.42 (10.3-12.2) |
| Preoperative corneal astigmatism, D | 1.23±0.38 (0.76-2.9) |
| Postoperative corneal astigmatism, D | 0.76±0.39 (0.11-2.09) |
| Postoperative refractive astigmatism, D | 0.73±0.55 (0-2.62) |
| Preoperative corneal higher-order aberrations, µm | 0.17±0.08 (0.05-0.44) |
| Postoperative corneal higher-order aberrations, µm | 0.24±0.11 (0.09-0.66) |
| Arc incision length | 36.07±9.39 (20-60) |
D: Diopter; SD: Standard deviation.
The astigmatism of 102 eyes exceeded 0.75 D at pre-operation, while the astigmatism of 57 eyes was less than 0.75 D at three months post-operation. If the corneal astigmatism was below 0.75 D, a success rate of 55.88% (57/102) was used as the criterion for success. According to the expert consensus for the application of multifocal IOL in China (2019)[6], a post-operative astigmatism ≤1.0 D is an indication for implantation of multifocal IOL. According to this, the success rate is 78.43% (80/102). That is, 78.43% of cataract patients with low and moderate corneal astigmatism can be converted into suitable people who can be implanted with multifocal IOL.
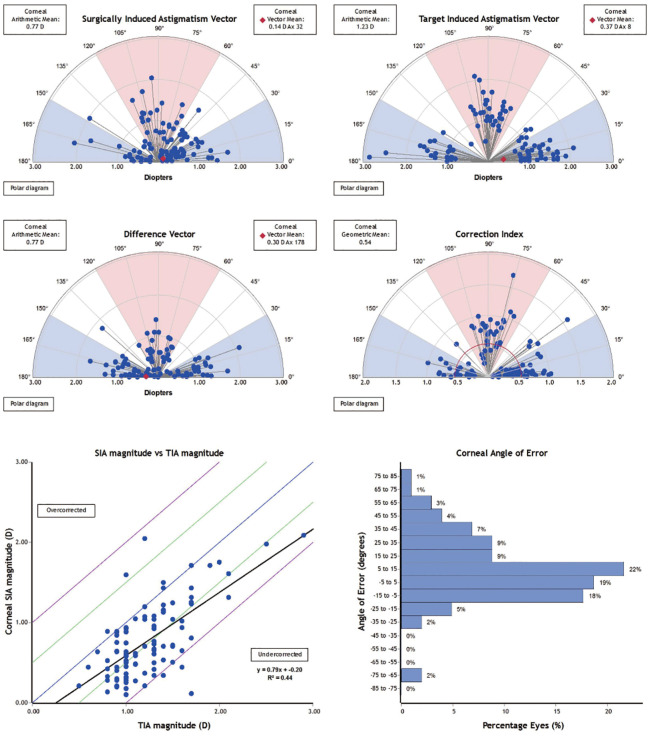
Vector Analysis of Astigmatism
The analysis results using Alpin's method is presented in Table 2 and Figure 2. TIA was 1.23±0.38 D, SIA was 0.77±0.45 D, DV was 0.77±0.39 D, and CI was 0.54±0.28, showing insufficient correction. CA is the reciprocal of CI. Hence, CA=1.64. IOS was 0.77±0.38, which indicates under corrected. AE was 8.52±18.09: 60 eyes (60/102, 59%) had an AE of ≤15° and two eyes had an AE of 0°, with a positive value for 68 eyes (counterclockwise dislocation) and a negative value for 32 eyes (clockwise dislocation).
Table 2. Vector analysis outcome using Alpins methods.
| Parameters | Mean | SD | Range |
| TIA | 1.23 | 0.38 | 0.76, 2.9 |
| SIA | 0.77 | 0.45 | 0.11, 2.09 |
| DV | 0.77 | 0.39 | 0, 1.10 |
| AE | 8.52 | 18.09 | -23.62, 67.65 |
| CI | 0.54a | 0.28 | 0.07, 1.71 |
| IOS | 0.66 | 0.34 | 0, 1.56 |
TIA: Target induced astigmatism; SIA: Surgically induced astigmatism; DV: Difference vector; AE: Angle of Errior; CI: Correction index; IOS: Index of Success; SD: Standrad deviation. aGeometric mean.
Figure 2. Astigmatism vector correction effect after operation (≥3mo).
Analysis of Influencing Factors of Correction Effect
The linear correlation analysis results revealed that there was no linear relationship between CI and age, corneal horizontal diameter, corneal thickness (central and periph) and preoperative astigmatism size. The arc incision length was correlated with CI based on the Spearman grade. However, the results revealed no correlations. The comparison results for the CI of different types of astigmatism are presented in Table 3. CI was against the rule astigmatism (ATR)>with the rule astigmatism (WTR)>oblique astigmatism (OBL), and the CI of ATR was obviously better than that of WTR (t=-3.574, P=0.001).
Table 3. Comparison of CI of different types of astigmatism.
| Types | WTR | ATR | OBL | Bonferroni comparisons | ||
| Total (n=102) | 64 | 33 | 5 | WTR vs ATR | WTR vs OBL | ATR vs OBL |
| Mean±SD | 0.47±0.28 | 0.68±0.28 | 0.57±0.31 | P=0.001 | P=0.461 | P=0.396 |
| Homogeneity of variance | F=3.744, P=0.03 | - | - | - | ||
WTR: With the rule astigmatism; ATR: Against the rule astigmatism; OBL: Oblique astigmatism; SD: Standard deviation.
DISCUSSION
There are three methods to correct astigmatism on the cornea during cataract surgery: main corneal incision on steep axis, limbal relaxing incision, and corneal keratotomy. The principle of these three methods is same. Furthermore, these all adopt a symmetrical- or single-arc incision, and cuts the cornea with a certain thickness and length at the steep meridian to flatten the steep meridian, and make the flat meridian steep. Although arc incisions assisted by the corneal depth control knife and astigmatism cup can be manually performed, the arc incision technique still needs nearly perfect surgical skills, and the accuracy and predictability are lower than that for FSAK[7]. FLACS is a novel option for arc incision. FSAK has the advantages of precise angle, depth and position, and this is programmed and standardized. Furthermore, this can theoretically improve the predictability. Previous studies have reported that the long-term effect of FSAK is stable and ideal[8]–[10]. Mayer et al[11] reported that the micro-serrated incision performed using the femtosecond laser led to higher apoptosis, when compared to manually performed incisions, and this upregulated the scar healing reaction, indicating that FSAK may be more effective in flattening the cornea.
The iFSAK performed for the corneal stroma does not penetrate the Bowman's layer. Theoretically, compared to pFSAK, the absence of an open wound can prevent infection, relieve postoperative pain, and prevent poor wound healing and epithelial hyperplasia[12]. However, all patients in the present study had a smooth operation, and there was no corneal incision penetration under the guidance of real-time OCT. The SIMA instrument was used for the incision separation, and no obvious corneal epithelial injury was observed. Upon washing incision, only one corneal epithelial hyperplasia and no infection was observed at post-operation, indicating that pFSAK is convenient and safe.
The reason why we choose symmetrical double incision instead of single incision is because we observe that symmetrical double incision is better than single incision through clinical observation, and Stanojcic et al's[13] research results also confirm this point.
The present study revealed that the corneal astigmatism decreased from 1.23±0.31 D at pre-operation to 0.76±0.39 D post-pFSAK operation. Furthermore, the astigmatism correction was effective, which is consistent with previous reports[14]–[20]. The CI reported by those studies ranged within 0.53-0.89, while the CI in the present study was 0.54, which was generally consistent, but a little low. The following factors were considered: 1) Moon et al[16] designed a symmetrical double-arc iFSAK using the Catalys femtosecond laser platform (USA), and the CI was 0.64, which was higher than that for pFSAK with the LenSx femtosecond laser platform. That is, different femtosecond laser platforms may influence the CI. 2) Visco et al[19] designed a depth of arc incision of 90%, which was higher than 85%. That is, the deeper the incision, the greater the correction effect. 3) Chen et al[18] reported that the Verion digital navigation system can more accurately locate the axial position of the astigmatism, and that the CI value was 0.89. In the present study, the patient's sitting position was marked on the horizontal axis, and the main incision was performed using a slit lamp. Hence, there may be some errors with the manual marking. 4) The research conducted by Noh et al[20] lengthened the arc length by 30% after calculating this based on the nomogram, thereby obtaining a CI of 0.71, which was higher than that in the present study. 5) In order to realize the symmetrical double-arc incision, the position of the primary incision needs to be changed sometimes, which may become a situation where the doctor is not comfortable to operate, resulting in the change of personalized surgical astigmatism, and in turn, leading to differences in SIA and TIA. 6) Zhang et al[21] reported that the lower CI value in Chinese people was probably because the corneal diameter of Chinese people is smaller than that of Europeans and Americans, and that the incision would relatively be closer to the limbus, reducing the effect of correcting the astigmatism. Therefore, it was speculated that the incision-to-limbus distance might affect the efficacy of the FSAK. The present study revealed that the correction effect of WTR was worse than that of ATR. The reason for this may be because the vertical cornea diameter was smaller, and the incision-to-limbus distance was closer to the limbus. Our study showed FSAK has the best correction effect on ATR, which may indicate that the distance between the arc incision and the limbus of cornea is the factor affecting CI. 7) This study, WTR patients accounted for a large proportion (64/102), and the lower CI for WTR was another the reason.
The present study innovatively compared postoperative corneal astigmatism with residual astigmatism of the whole eye, and the results revealed that these are consistent, indicating that residual corneal astigmatism is the main source of the whole eye astigmatism after FSAK, and that the intraocular astigmatism can be neglected. If toric IOLs can be designed as the control group to compare the astigmatism correction effect, it would be feasible to use residual whole-eye astigmatism.
Furthermore, the present results revealed that the higher-order corneal aberration increased after FSAK, which is consistent with the research results reported by Pohlmann et al[22]. The existence of higher-order corneal aberration would reduce the visual quality, attracting the attention of clinicians. Afterwards, objective visual quality analyzers, such as iTrace, Sirus and OPD, should be used to analyze the higher-order corneal aberration.
CA is the adjustment coefficient. This is the reciprocal of CI, and can guide the follow-up surgery. The CA in the present study was 1.85. This means that if the TIA needs to be corrected for 1 D, the operation should be designed based on 1.85 D. However, the surgery cannot be completely carried out according to this design before further research. Furthermore, it would be feasible to appropriately increase the arc length, in order to improve the CI, as reported by Noh et al[20]. Baharozian et al[17] innovatively designed the incision length of WTR, OBL and ATR with a 9 mm corneal diameter, according to the nomogram calculation, and the CI reached 0.53, 0.95 and 1.01, respectively. This design was based on the research, which revealed that the correction effect of FSAK is ATR>OBL>WTR[16]–[19]. The present results revealed that the CI for ATR, OBL and WTR was 0.75, 0.64 and 0.54, respectively, which is similar to the report of a previous research. However, merely WTR and ATR had statistically significant differences (P=0.001). Furthermore, the CI for WTR was low, considering that the cornea is a transverse ellipse, and the vertical diameter was smaller than the horizontal. According to the 8/10 design, the incision would be closer to the cornea periphery. This suggests that when designing an arc incision with regular astigmatism in the future, it is advisable to set the incision closer to the center of the cornea, in order to improve the CI. However, the prospective 5-year follow-up results reported by Chan et al[10] revealed that the WTR tends to be corrected with age, which is correlated to the conversion of corneal astigmatism to ATR with age. Some studies have also revealed that the correction of low-grade WTR cannot improve the visual quality of patients[23]. Therefore, various aspects needs to be considered when designing the TIA of WTR.
The results of the present study revealed that there was no linear relationship between CI and age, preoperative corneal astigmatism size, corneal thickness (central and periph), corneal horizontal diameter, and arc incision length. However, previous studies have reported different results. For example, for the relationship between age and CI, some studies reported that the CI for older patients was better than that for younger patients[24]. Furthermore, in the study conducted by Moon et al[16], the Catalys platform was used to perform the iFSAK, and it was observed that the CI was negatively correlated with age. The author in that study suggested that the arc length should be appropriately increased for older patients. For the relationship between preoperative corneal astigmatism size and CI, Noh et al[20] reported that the CI was higher in ≤1.5 D, when compared to >1.5 D. In the present study, the preoperative corneal astigmatism ranged within 0.8-2.1 D, and the astigmatism of most patients belonged to low and moderate astigmatism. However, the linear correlation regression analysis revealed that there was no linear relationship. That is, the degree of astigmatism did not affect the correction effect, which is consistent with the report of Moon et al[16]. These research reports were inconsistent due to the following: retrospective design, small sample size, short follow-up time, different femtosecond laser platforms, different devices for measuring the corneal astigmatism before the operation, and different algorithms for designing the incision. This indicates that there is no definite conclusion on the correction effect of FSAK. Although the present study was also a retrospective study, there was a lack of strict control. Thus, it may be difficult to prevent some bias factors in the evaluation of the results. In the future, patients with higher CI who should undergo a personalized FSAK based on the type of astigmatism, corneal biomechanics, etc.
In conclusion, although the present study demonstrated that pFSAK based on the nomogram algorithm is safe and has a better correction effect for ATR, but this would increase the higher-order corneal aberration. Age, astigmatism size, corneal horizontal diameter, corneal thickness and arc incision length had no influence on the CI. The CI is not ideal. At present it's not a good choice if we pursue the ideal correction effect, especially in the era of refractive cataract surgery with higher requirements. There need to conduct further in-depth, studies for the different femtosecond laser platforms used for pFSAK or iFSAK.
Acknowledgments
We sincerely thank Dr. Liu Dongcheng, Department of Science and Education, Shenzhen Aier Eye Hospital, affiliated to Jinan University, for his guidance on the paper writing. Thanks Mr. Chen Qingshan, Department of Epidemiology, Jinan University, for his guidance on statistical methods. Thanks Dr. He Jieqiong, Dr. Lu Yijie and Dr. Liu Ying for their assistance.
Authors' contributions: Study concept and design (Sima J, Cao JG, Li L); collection,management,analysis and interpretation of data (Hu ZX, Ke Y, Zhang YY, Guo QT, He YP, Liao HX, Tan X); preparation,review,or approval of the manuscript (Hu ZX, Li L, Qin B, Sima J). All authors read and approved the final manuscript.
Foundations: Supported by the Natural Science Foundation of Guangdong Province, China (No.2022A1515010742); Hunan Provincial Natural Science Foundation of China (No.2021JJ30045); the Science Research Grant of Aier Eye Hospital Group (No.AF2102D5; No.AF2201D06; No.AF2201D05).
Conflicts of Interest: Hu ZX, None; Sima J, None; Cao JG, None; Ke Y, None; Zhang YY, None; Guo QT, None; He YP, None; Liao HX, None; Tan X, None; Qin B, None; Li L, None.
REFERENCES
- 1.Anderson DF, Dhariwal M, Bouchet C, et al. Global prevalence and economic and humanistic burden of astigmatism in cataract patients: a systematic literature review. Clin Ophthalmol. 2018;12:439–452. doi: 10.2147/OPTH.S146829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwon HJ, Lee H, Lee JA, et al. Astigmatic correction of simultaneous femtosecond laser-assisted cataract surgery (FLACS) with intrastromal arcuate keratotomy (ISAK) versus Toric intraocular Lens Impantation with conventional phacoemulsification. BMC Ophthalmol. 2021;21(1):298. doi: 10.1186/s12886-021-02059-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yoo A, Yun S, Kim JY, Kim MJ, Tchah H. Femtosecond laser-assisted arcuate keratotomy versus toric IOL implantation for correcting astigmatism. J Refract Surg. 2015;31(9):574–578. doi: 10.3928/1081597X-20150820-01. [DOI] [PubMed] [Google Scholar]
- 4.Reinstein DZ, Archer TJ, Randleman JB. JRS standard for reporting astigmatism outcomes of refractive surgery. J Refract Surg. 2014;30(10):654–659. doi: 10.3928/1081597X-20140903-01. [DOI] [PubMed] [Google Scholar]
- 5.ASSORT group analysis calculator. 2019. https://www.isrs.org/resources/assort-group-analysis-calculator. [DOI] [PubMed]
- 6.Cataract and Intraocular Lens Group, Ophthalmology Branch of Chinese Medical Association. Expert consensus on clinical application of multifocal intraocular lens in China (2019) Chinese Journal of Ophthalmology. 2019;55(7):491–494. [Google Scholar]
- 7.Sorkin N, Mimouni M, Santaella G, et al. Comparison of manual and femtosecond astigmatic keratotomy in the treatment of postkeratoplasty astigmatism. Acta Ophthalmol. 2021;99(5):e747–e752. doi: 10.1111/aos.14653. [DOI] [PubMed] [Google Scholar]
- 8.Chan TCY, Ng ALK, Cheng GPM, Wang Z, Woo VCP, Jhanji V. Corneal astigmatism and aberrations after combined femtosecond-assisted phacoemulsification and arcuate keratotomy: two-year results. Am J Ophthalmol. 2016;170:83–90. doi: 10.1016/j.ajo.2016.07.022. [DOI] [PubMed] [Google Scholar]
- 9.Visco DM, Bedi R, Packer M. Femtosecond laser-assisted arcuate keratotomy at the time of cataract surgery for the management of preexisting astigmatism. J Cataract Refract Surg. 2019;45(12):1762–1769. doi: 10.1016/j.jcrs.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Chan TCY, Ng ALK, Wang Z, Chang JSM, Cheng GPM. Five-year changes in corneal astigmatism after combined femtosecond-assisted phacoemulsification and arcuate keratotomy. Am J Ophthalmol. 2020;217:232–239. doi: 10.1016/j.ajo.2020.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Mayer WJ, Klaproth OK, Hengerer FH, et al. In vitro immunohistochemical and morphological observations of penetrating corneal incisions created by a femtosecond laser used for assisted intraocular lens surgery. J Cataract Refract Surg. 2014;40(4):632–638. doi: 10.1016/j.jcrs.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 12.Chang JSM. Femtosecond laser-assisted astigmatic keratotomy: a review. Eye Vis (Lond) 2018;5:6. doi: 10.1186/s40662-018-0099-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stanojcic N, O'Brart D, Hull C, Wagh V, Azan E, Bhogal M, Robbie S, Li JP O. Corneal astigmatic outcomes after femtosecond laser-assisted cataract surgery combined with surface penetrating arcuate keratotomies. Int J Ophthalmol. 2023;16(7):1084–1092. doi: 10.18240/ijo.2023.07.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang J, Zhao JY, Xu J, Zhang JS. Evaluation of the effectiveness of combined femtosecond laser-assisted cataract surgery and femtosecond laser astigmatic keratotomy in improving post-operative visual outcomes. BMC Ophthalmol. 2018;18(1):161. doi: 10.1186/s12886-018-0823-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Day AC, Lau NM, Stevens JD. Nonpenetrating femtosecond laser intrastromal astigmatic keratotomy in eyes having cataract surgery. J Cataract Refract Surg. 2016;42(1):102–109. doi: 10.1016/j.jcrs.2015.07.045. [DOI] [PubMed] [Google Scholar]
- 16.Moon SY, Chung HS, Lee JH, Park SY, Lee H, Kim JY, Tchah H. Evaluation of astigmatic correction using vector analysis after combined femtosecond laser-assisted phacoemulsification and intrastromal arcuate keratotomy. J Ophthalmol. 2021;2021:2860840. doi: 10.1155/2021/2860840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baharozian CJ, Song C, Hatch KM, Talamo JH. A novel nomogram for the treatment of astigmatism with femtosecond-laser arcuate incisions at the time of cataract surgery. Clin Ophthalmol. 2017;11:1841–1848. doi: 10.2147/OPTH.S141255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen W, Zhou J, Du J, et al. The effect of femtosecond-assisted arcuate keratotomy on cataract patients with corneal astigmatism. Recent Advances in Ophthalmology. 2019;39(12):1137–1140. [Google Scholar]
- 19.Visco DM, Bedi R, Packer M. Femtosecond laser-assisted arcuate keratotomy at the time of cataract surgery for the management of preexisting astigmatism. J Cataract Refract Surg. 2019;45(12):1762–1769. doi: 10.1016/j.jcrs.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 20.Noh H, Yoo YS, Shin KY, et al. Comparison of penetrating femtosecond laser-assisted astigmatic keratotomy and toric intraocular lens implantation for correction of astigmatism in cataract surgery. Sci Rep. 2021;11(1):7340. doi: 10.1038/s41598-021-86763-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang F, Li SW, Huo DM, Li QM. Predictors of femtosecond laser-assisted arcuate keratotomy efficacy for astigmatism correction in cataract surgery. J Refract Surg. 2022;38(8):480–486. doi: 10.3928/1081597X-20220609-01. [DOI] [PubMed] [Google Scholar]
- 22.Pohlmann D, Pilger D, Bertelmann E, von Sonnleithner C. Corneal higher-order aberrations after cataract surgery: manual phacoemulsification versus femtosecond-laser assisted technique. Eur J Ophthalmol. 2021;31(6):2955–2961. doi: 10.1177/1120672121990611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tan QQ, Wen BW, Liao X, Tian J, Lin J, Lan CJ. Optical quality in low astigmatic eyes with or without cylindrical correction. Graefes Arch Clin Exp Ophthalmol. 2020;258(2):451–458. doi: 10.1007/s00417-019-04501-0. [DOI] [PubMed] [Google Scholar]
- 24.Byun YS, Kim S, Lazo MZ, et al. Astigmatic correction by intrastromal astigmatic keratotomy during femtosecond laser-assisted cataract surgery: factors in outcomes. J Cataract Refract Surg. 2018;44(2):202–208. doi: 10.1016/j.jcrs.2017.11.018. [DOI] [PubMed] [Google Scholar]