Abstract
Adults with intellectual and developmental disabilities frequently experience poor life outcomes, with individuals reporting lower levels of social support, relationships, gainful employment, and satisfaction in their quality of life. To ameliorate these outcomes, social skills and social communication interventions aligned with the needs of adults are warranted. This study examined the efficacy of Snack Talk, a supplemental naturalistic visual communication support, with five adults with intellectual and developmental disabilities. Snack Talk was implemented during the midday mealtime, with the goal of increasing conversation engagement. A withdrawal design across participants was used. Results demonstrated increases in conversation engagement and showed meaningful gains for participants in the intervention and postintervention phase compared to baseline.
Keywords: Intellectual and developmental disabilities, Social skills, Mealtimes, Communication
The prevalence of diagnoses of developmental disabilities (DD) in general, and autism spectrum disorder (ASD) diagnoses in particular, have increased dramatically in the last two decades (Baio et al., 2018; Boyle et al., 2011; Hill et al., 2014). Many of the individuals who have received these diagnoses are now approaching, or have entered, adulthood. Unfortunately, the adult service system is ill-prepared and underfunded (Gerhardt, 2009), often lacking resources and experienced staff (O'Keefe & Siebenaler, 2006). Thus, effective treatment and services for adults with DD and/or ASD1 continues to be needed.
Current literature indicates that outcomes for adults with disabilities, including ASD and DD, are generally poor for the majority of the surveyed individuals (Levy & Perry, 2011). That is, most individuals remain living at home, are often isolated, and rely on aging parents or other caregivers for daily care. Individuals with disabilities indicate they are often unable to access higher education, gain employment, or build successful friendships or romantic relationships with others (Bishop-Fitzpatrick et al., 2018; Grob et al., 2019; Howlin et al., 2013; Levy & Perry, 2011).
Social skills are necessary for these endeavors and are critically needed to independently navigate the social expectations of adult life. Further, social skills are prerequisites to other desired outcomes such as gainful employment, meaningful relationships, and community inclusion. Adults with disabilities may experience difficulties in social skills and although they may respond to bids for communication, their responses may be incomplete, brief, or acontextual, and therefore less successful (Hood et al., 2017). This may diminish an individual’s sense of community membership or sense of inclusion and belonging to a group of peers, ultimately affecting an individual’s overall quality of life (Schwartz, 2000; Schwartz & Kelly, 2021). Literature strongly suggests that social skills are essential for a successful and independent adult life and attention to social supports and outcomes is warranted (Gresham & Elliott, 2014). Yet there is a paucity of evidence-based social communication supports for adults with ASD and/or DD designed to meet the needs of the adult population and their specific contexts of social life. Although in recent decades gains have been made towards identifying effective social communication supports, most social skills research has been conducted with children (Grob et al., 2019; Walton & Ingersoll, 2013). Therefore it is unclear if interventions that have demonstrated effectiveness in younger populations are effective for adult populations with disabilities.
Applied Behavior Analysis across the Lifespan
Much of the research that does include this population is rooted in the field of applied behavior analysis (ABA; Baer et al., 1968; Cooper et al., 2020). Interventions based on ABA have shown medium to large effects (Eldevik et al., 2009; Reichow & Wolery, 2009) and are considered the gold standard intervention for individuals with ASD. ABA encompasses numerous different evidence-based practices to address interfering behavior and teach new skills. These practices can easily be adapted to meet the needs of each learner, ensuring intervention is matched to the appropriate age and level of skill and overall development. This inherent flexibility allows interventions to grow with learners across the lifespan. Research has demonstrated the effectiveness of ABA-based interventions with children with ASD and/or I/DD (e.g., Haymes et al., 2015; Machalicek et al., 2021; Neidert et al., 2010), but limited research exists demonstrating the effects of ABA with the adult population.
The Association of Professional Behavior Analysts (APBA), an organization whose mission is to promote and advance the science of ABA, recommends ABA for adults in their practice guidelines (APBA, 2019). Yet, as a result of lack of evidence demonstrating the effectiveness of ABA for adults, insurance coverage for ABA services for this population often falls outside of age limits (Autism Speaks, 2020). In order to demonstrate the effectiveness of ABA with adults with ASD and DD across the lifespan, additional research is needed.
Social Skills Interventions for Adults with DD
Social skills and social communication supports have been examined extensively in research grounded in ABA (e.g., Hughes et al., 2011; Krantz & McClannahan, 1998; Murdock & Hobbs, 2011; Steinbrenner et al., 2020; Walton & Ingersoll, 2013; Wong et al., 2015), yet few studies have included adults with ASD or other DD as the primary participants (Aguirre et al., 2015). In addition, most published studies have not included naturalistic settings and natural conversation partners (Aguirre et al., 2015; Haring et al., 1986; but see Nuernberger et al., 2013, for an exception).
Mealtimes present a potentially opportune time to address social communication skills through intervention. As a routine, mealtimes provide opportunities for individuals to develop and engage in social communication skills (Massey, 2004) and build connections and community membership within their social groups. This natural structure allows for opportunities to embed social skills instruction (Snow & Beals, 2006). One intervention that has shown promising effects in supporting social communication for younger populations with DD and/or ASD during mealtimes is Snack Talk (Bateman et al., 2022).
Snack Talk
Snack Talk (Gauvreau, 2017) is a visually based naturalistic instructional protocol built on the evidence-based practice of using visual supports (Steinbrenner et al., 2020) to increase social communication during mealtimes. Snack Talk is a low-cost and low-resource intervention that has been evaluated with younger individuals with DD (Bateman et al., 2022). Snack Talk involves a training package that incorporates visual supports, modeling, prompting, and reinforcement (explained further below). Participants are first interviewed to identify high-interest and preferred topics. The Snack Talk visual supports include a textual prompt (e.g., “Where do you like to travel?”) with 9–12 pictures representing previously identified possible responses from participant interviews. The supports are also aligned with current communication goals for the participants and can be used as a supplement to augmentative and alternative communication supports (AAC). This study sought to conduct a systematic replication, examining the effects of implementation of Snack Talk in an adult academy setting with adults with ASD and DD, compared to previous iterations of the Snack Talk intervention which was evaluated with younger populations (see Bateman et al., 2022, for a further discussion of studies). We sought to investigate the following questions: (1) Does the use of the Snack Talk intervention result in increased conversation engagement for adults with ASD and DD during mealtimes? (2) Does the effects of implementation of the Snack Talk intervention maintain following the initial intervention? and (3) What is the social validity of Snack Talk for participants and staff members at an adult academy serving adults with ASD and DD?
Method
Participants
Five adults with ASD and other DD were recruited from a day program at an adult academy for individuals with disabilities in a mid-Atlantic state. This adult day academy provided behavioral services and support to focus on promoting learning, personal growth, individual choice, and meaningful engagement. Further, each participant received individualized programming and intervention developed by a board certified behavior analyst, and implemented by behavioral technicians and staff in the adult day academy. Participants recruited in this study demonstrated challenges in the skillset of social skills. Social engagement was a target goal for these individuals, as identified by participants, participants’ families, as well as adult academy staff. These individuals expressed a desire to attend events in the community (such as lunch and dinner meet ups). Some participants recruited did not demonstrate the skills necessary to appropriately engage and attend these community events, as they engaged in high rates of interfering behavior. Some participants did currently attend these types of events in the community, but struggled to meaningfully engage with their peers.
Adults with disabilities in this study attended this academy 5 days a week from morning until early evening, for a total of 8 hr a day. The inclusion criteria for participants in this study were (1) a medical diagnosis of DD; (2) a chronological age between 18 and 60; (3) eligibility for adult services at the adult academy; (4) identified challenges in social communication; and (5) demonstration of intraverbal control and intraverbal-tact control. Demographic information pertaining to age, eligibility, and repertoires of skills were collected via staff and interventionist report.
Brandon was a 25-year-old man diagnosed with ASD, anxiety, obsessive-compulsive disorder, and attention-deficit/hyperactivity disorder. Results of his Vineland-II placed his expressive language skills at 2 years, 4 months; receptive language skills at 2 years, 2 months; and interpersonal skills at 2 years of age. Brandon primarily communicated vocally using rote 3 to 5 word utterances. Adult academy staff described Brandon’s communication, identifying he spoke quickly, presented with poor articulation, and engaged in high-frequency vocal perseveration. Other than greeting others, pragmatic language was not observed. Brandon had not been observed independently initiating interactions with peers.
Alexander was a 40-year-old man diagnosed with Fragile X, anxiety, and impulse-control disorder. Results of his most recent Vineland-II placed his expressive language skills at 4 years, 5 months; receptive language skills at 18 years; and interpersonal skills at 4 years, 7 months. Alexander, a vocal communicator, used short phrases and gestures to communicate his needs. Adult academy staff described Alexander's communication, indicating that he demonstrated poor articulation, stuttering, and very low voice volume, making him difficult to understand; however, he frequently initiated greetings toward staff members by reaching out to shake their hand. Beyond this initial exchange, Alexander was not observed to engage in a conversation with more than one or two exchanges, and although he was observed to be interested in peers (i.e., watching them), he did not independently initiate an interaction with them.
Mason was a 25-year-old man diagnosed with ASD. Results of his most recent Vineland-II placed his expressive language skills at 6 years, 4 months; receptive language skills at 7 years, 6 months; and interpersonal skills at 2 years, 4 months. Mason was a vocal communicator who had been observed to communicate using short sentences and rote phrases. Adult academy staff described Mason’s communication, identifying that he engaged in high rates of vocal stereotypy in the form of scripting from cartoons and movies, which was difficult to interrupt or shift in topic. Conversation partners often had to repeat questions before he answered. Following a very quick answer, he would return to scripting. Mason had not been observed asking others questions about themselves or their interests, nor had he been observed to independently initiate interactions with peers.
Felicity was a 23-year-old woman diagnosed with ASD and anxiety. Results of her most recent Vineland-II placed her expressive language skills at 22+ years; receptive language skills at 6 years, 6 months, and interpersonal skills at 3 years, 7 months. Felicity could make requests and ask using full sentences. Adult academy staff described Felicity’s communication, indicating she commonly spoke to both peers and staff members, generally by asking questions related to topics of interest to her. She primarily directed most communication towards staff members, frequently requiring prompting to initiate to peers. Felicity was also observed to perseverate on topics and ask the same questions repeatedly.
Tim was a 35-year-old man diagnosed with moderate-intellectual disability, bipolar disorder, and obsessive-compulsive disorder. Results of his Vineland-II placed his expressive language skills at 7 years, 7 months; receptive language skills at 4 years, 7 months, and interpersonal skills at 8 years, 7 months. Tim, a vocal communicator, was able to use and understand full sentences, however he demonstrated deficits in pragmatic language. Adult academy staff described Tim’s communication, indicating that Tim often spoke to staff members about topics of interest to him, but failed to reliably respond to questions or statements. Tim would perseverate on a single topic for extended periods of time and it was difficult for staff to change the topic. In addition, Tim was not observed to ask questions about any topic and was not observed to independently initiate interactions with peers.
Interventionists
To assess the efficacy of Snack Talk, the intervention was implemented by the first and second authors. At the time of the study, the first author was a board certified behavior analyst with a doctoral designation (BCBA-D), held a doctoral degree in special education, and had 12 years of experience working with individuals with ASD and other DD in school settings. The second author was a doctoral student who worked with the first author as a research assistant. At the time of the study, the second author held a master’s degree in special education and had 8 years of experience working with individuals with DD in school and clinic settings.
Experimental Design
The current study employed a variation of a withdrawal design (Gast & Ledford, 2014), in which participants moved through baseline and intervention phases concurrently. Because intervention was simultaneously provided to all participants during mealtime as a naturalistic intervention package, it was not feasible to make individual programming decisions regarding phase changes. Baseline and intervention phases were alternated, meeting What Works Clearinghouse (Kratochwill et al., 2013) methodology criteria for single-case research design. Data from a total of two baseline conditions, two intervention conditions, and postintervention maintenance probes were collected for each participant.
Setting and Materials
Experimental sessions occurred in a conference room at an adult academy program for adults diagnosed with DD. As a whole, the program had 15 adults and 5 staff members. Five adults participated in the study and sat at one large table during lunchtime. Sessions across all phases occurred daily for the entire duration of the 30-min lunch block unless there was a planned disruption in the adult academy schedule (e.g., a field trip was planned or it was a holiday) over a period of 3 months. During all sessions, the participants, and two members of the research team were present. This allowed for a 1:2.5 staff-to-participant ratio. Intervention was implemented during the adults’ typical lunchtime routine. Adults not participating in the intervention were in another room having lunch with staff members.
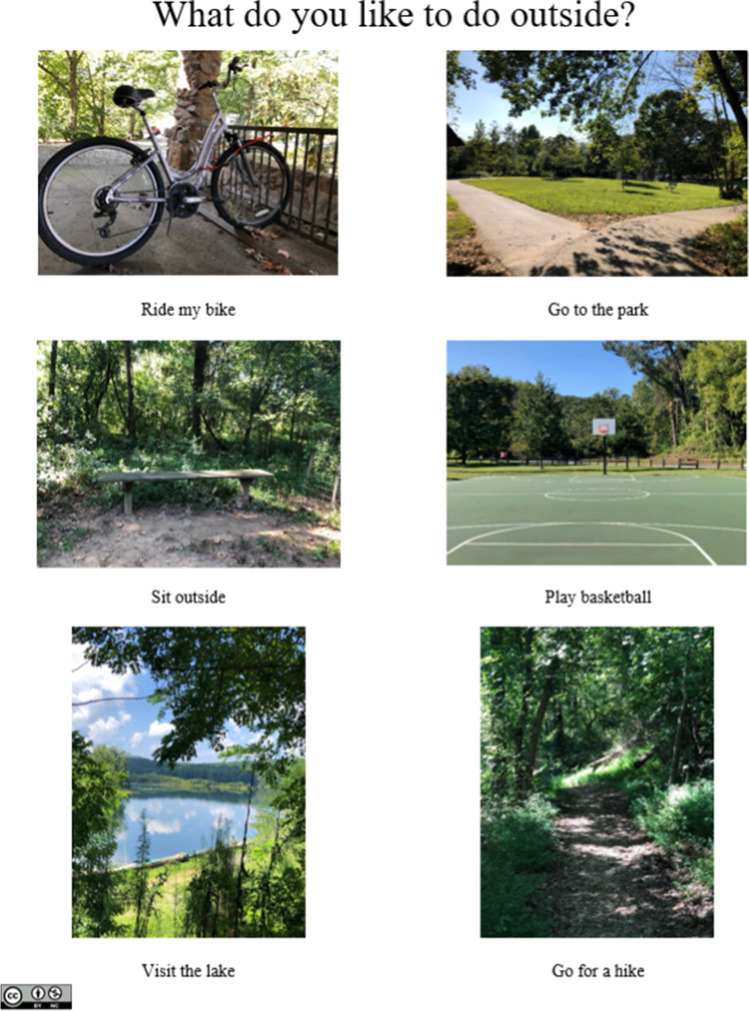
Snack Talk visual supports served as the primary intervention tool in this study (see Fig. 1). Prior to development of the Snack Talk supports, adult academy staff and adult participants interviewed participants to identify each individual’s interests. In these separate interviews, the research team asked staff and adult participants what kind of activities the participants liked to engage in at the adult academy, as well as what their individual interests were such as preferred topics of conversation, movies, activities to do at home, places to eat, and travel. These interviews ensured incorporation of family and cultural norms into the development of intervention, as cultural considerations and values were often reflected in each participant’s interests. Then, Snack Talk supports were created by the interventionists on the research team (i.e., the first and second authors). Snack Talk supports were 8½ by 11-in laminated sheets of paper that included a question related to the identified topic (e.g., “Where do you like to visit?”) and 9–12 pictures with text representing possible answers. Possible answers included individual interests identified in brief interviews with participants to ensure participants were motivated to communicate with their peers with Snack Talk supports. Both text and pictures were included in these supports to ensure all participants could access intervention regardless of their ability to read text. Each sheet included preferred answers from several participants to promote engagement by more than one participant at a time. These supports were made using Microsoft Word and pictures identified through the Google Images service. In addition to Snack Talks supports, a video camera and tripod were used to video record sessions in order to collect implementation data, and a laptop was utilized to code and analyze the data.
Fig. 1.
Visual communication support example. Note. Example of visual communication support used during mealtimes. Copyright 2020 by Author under a Creative Commons Attribution-Noncommercial 4.0 International License (CC BY-NC). Publicly available at (Open Science Framework blinded for review)
Dependent Variable Definitions and Measurement
The dependent variable was conversation engagement between and among participants and implementers. Conversation engagement was defined as verbal or nonverbal communicative acts by participants towards a peer, adult academy staff member, or intervention implementer. Conversation engagement included communicative acts that were initiations and responses, to include the reciprocal nature of conversation. Staff members and implementers were included in this definition because the participants were adults, and therefore age-peers of the staff members and implementers. An initiation was defined as a participant verbally or nonverbally initiating a communicative interaction that was not in response to a peer’s or implementer's prior statement. Initiations could be based on Snack Talk cards or relevant topics (e.g., the weather or lunch) but initiations that were perseverative speech or not directed towards a peer or implementer were not counted unless the participant directly engaged a peer or adult in the process. For example, a participant commenting on the weather to a staff member would be coded as a verbal initiation, but a general comment regarding the weather made to the entire room without a bid for attention to someone would not be coded as conversation engagement. Responses were defined as verbal or nonverbal communicative acts in response to a peer’s or implementers’ verbal or nonverbal initiation. Overall, vocal utterances were considered verbal communicative acts while directed gestures such as pointing were considered nonverbal communicative acts. If a participant was unresponsive to a communication bid from a peer or implementer within 5 s of the original communication bid, this was indicated as a “nonresponse” on the data coding sheet and a least-to-most prompting protocol was implemented (see below). Conversational engagement was measured by collapsing initiations and responses into one broad code of “communicative acts” due to the range of communication skills demonstrated across participants. Further, we collapsed verbal and nonverbal modes into one category as participants frequently used both modalities simultaneously. If both modalities were used, it was recorded as a single instance of a communicative act. This allowed the data collected to represent the nonverbal and developing social communication abilities for this group of adults.
The first 10 min of each 30-min mealtime were video recorded, and coders subsequently observed the video and manually recorded conversation engagement. Because social conversation often does not include a defined beginning and end, 10-s partial interval recording was used, in which coders scored conversation engagement if the target behavior occurred at any point during a given interval. Although this coding procedure risks overestimating target behavior occurrence (Ledford & Gast, 2018), it can estimate conversation engagement while accounting for the natural lulls and breaks in conversation, as shown with previous social communication interventions (e.g., Hochman et al., 2015).
Procedures
All baseline and intervention sessions occurred during the first 10 min of lunchtime. A video camera with audio capabilities was set up in the corner of the room for all conditions. Video recording began as soon as all participants were present at the table for mealtime (unless they were absent from the academy that day). To accommodate the natural variation in the lunchtime routine, coding continued if an adult consumer left the table, with the resulting intervals coded as nonengagement.
Baseline
Baseline sessions were “business as usual,” because mealtime was a pre-established and familiar routine at the adult academy. Study implementers and participants sat and ate lunch at the table. During this condition, Snack Talk supports were not available, and any adult academy staff members that were present were directed to interact with participants as they typically would.
Intervention
During intervention sessions, implementers supported adult participants in a 1:2 or 1:3 ratio. Implementers rotated supporting adult participants daily throughout the entirety of intervention and postintervention generalization phases. Implementers positioned Snack Talk supports on the table where they were visually and physically accessible for the adult participants. Several Snack Talk cards were made available to all participants to decrease the likelihood of participants becoming familiar and/or memorizing a single discriminative stimulus. Next, the implementers started intervention by initiating a group model of conversation engagement by holding up a Snack Talk card making a statement of preference related to the picture (for example, “What did you do this weekend? I went to the movies! What did you do?”). The implementer then paused 5–10 s to provide each of the adult participants an opportunity to respond. If participants did not engage in conversation independently within this time frame, the implementers used two-step least-to-most prompting (verbal only and a combination of gestural and verbal) as needed with each of the participants the implementer was supporting. First, the implementers directly asked the adult participant the topic question printed on the Snack Talk support card. If a target response did not occur, the implementers next used a combined gestural and verbal prompt, which consisted of pointing at the Snack Talk card while verbally prompting the participant to ask a peer the question on the Snack Talk card (“You can ask Felicity what she likes to do for fun.”) Implementers alternated prompting as needed between participants to ensure all study participants had equal opportunities to engage in conversation. Instances of conversation engagement were immediately reinforced by providing positive social praise (e.g., “Awesome job telling me you like to visit the movies!”). Praise was provided following each instance of conversation engagement, regardless of prompting level. Following the group model and individual engagement with each adult participant, implementers provided individual support using the identified prompt procedures to participants to engage in conversation engagement using the Snack Talk cards. This modeling procedure was implemented with adult participants daily during intervention phases of intervention.
Because the intervention was implemented during lunch, natural lulls in conversation were anticipated. A natural lull in conversation was defined as a period of 10–15 s where there was no occurrence of verbal or nonverbal social interaction. This length of a pause in our operational definition of a lull in conversation was used to allow enough time for adult consumers to have an adequate opportunity to engage with their peers before implementation of prompting procedures. When these pauses occurred, implementers used the described least-to-most prompting hierarchy to facilitate social conversations between the participants for the duration of the mealtime. Initiations towards peers, staff members, and implementers were verbally reinforced through delivery of social praise and engagement in naturalistic conversational turns. Intervention procedures remained consistent throughout all intervention conditions.
Postintervention Maintenance Phase
Given the applied nature of this research, participants were integrated back into the classroom with all peers during mealtimes at the end of the final intervention phase. Study participants sat at different tables with different peers who did not participate in intervention. Maintenance probes were conducted every 2 weeks for 6 weeks, for a total of three data collection probes. Due to restrictions related to video consent for other adult academy attendees, and limited resources and personnel within the adult academy, study participants returned to the original intervention setting for these probes. Snack Talk supports were implemented during these probes, and implementers continued to prompt and reinforce as they had in the intervention phase.
Procedural Fidelity
Implementers completed a self-report procedural fidelity checklist in every session in each condition. In addition, procedural fidelity was coded from video recordings by primary and secondary coders (see IOA), using the same procedural checklist. The checklist consisted of six steps: (1) Place Snack Talk on the table during mealtimes; (2) model by making an on-topic comment and showing the Snack Talk card to the participants seated at the table; (3) If participants respond, reinforce these interactions with social praise and other reinforcement systems if appropriate; (4) If participants do not respond, begin least-to-most prompting and continue the prompting hierarchy until the target response occurs; (5) provide reinforcement when conversation engagement occurs: and (6) as natural lull in conversation occurs, reinstate prompting hierarchy. Self-report and fidelity coding from video recordings were collected across baseline, intervention, and maintenance conditions. The data showed that 0% of treatment components were implemented in baseline and 100% were implemented in intervention and maintenance conditions.
Interobserver Agreement
Interobserver agreement (IOA) was measured independently by members of the research team. The second author was the primary data collector and a special education graduate student served as a secondary coder. The second author trained the second coder on behavioral definitions and measurement procedures during data collection sessions not included in IOA calculations. Training continued until 90% agreement on IOA coding procedures was reached in three consecutive sessions. Interval-by-interval IOA (Cooper et al., 2020) was collected between 29% and 33% of sessions in all study conditions across all participants via video recorded sessions. IOA is reported in Table 1.
Table 1.
Interobserver agreement
| Participants | Baseline 1 (range) | Intervention 1 (range) | Baseline 2 (range) | Intervention 2 (range) | Maintenance |
|---|---|---|---|---|---|
| Brandon | 97% | 94% (92–96) | 99% (98–100) | 99% (97-100) | 92% |
| Alexander | 96% (95–97) | 90% (92–98) | 94% (88–100) | 100% | 100% |
| Mason | 99% (97–100) | 100% | 98% (95–100) | 100% | 100% |
| Felicity | 98% (96–100) | 92% (88–96) | 98% (95–100) | 100% | 96% |
| Tim | 89% (80–98) | 85% | 98% (96–100) | 100% | 100% |
Note. Percentage and range of interobserver agreement for each condition is reported for each participant
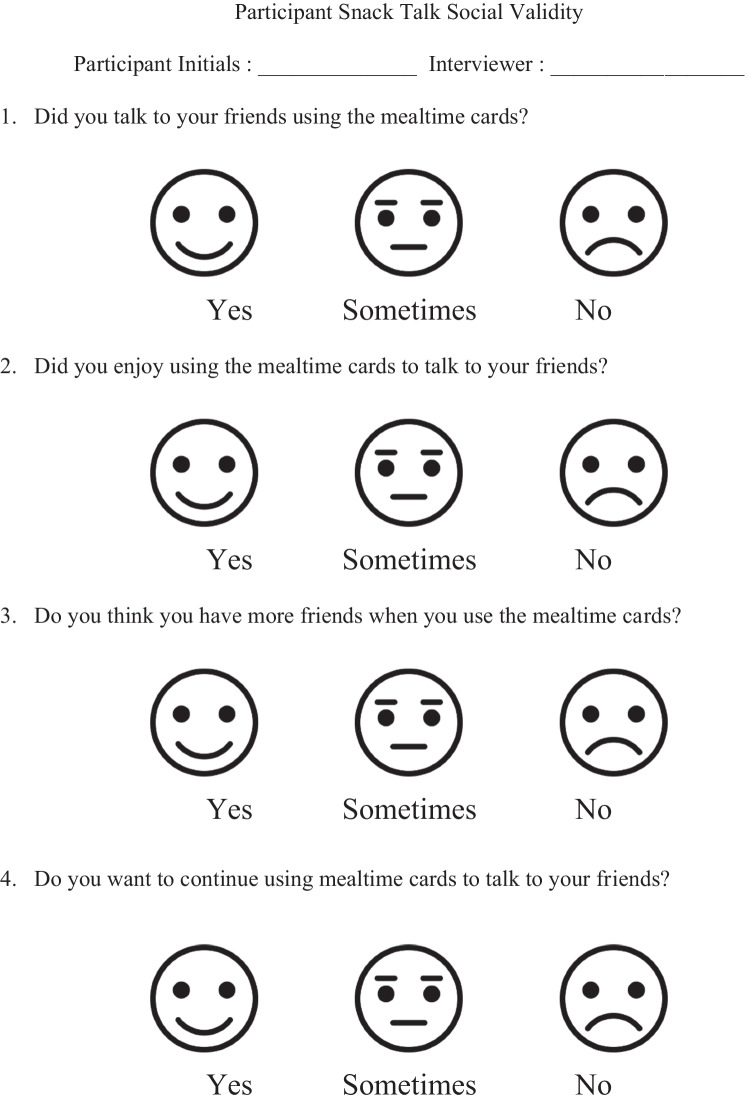
Social Validity
In order to evaluate perceptions and acceptability of Snack Talk, social validity data were collected from both participants and academy staff members. To identify perceptions of intervention from participants, a four-question survey was administered upon completion of this study. This survey was four questions long and included a Likert-scale with three possible answers. A visual representation of possible responses, ensuring participants were able to respond independently, was included in this survey for participants (see Fig. 2).
Fig. 2.
Participant social validity rating scale
To identify perceptions of intervention from academy staff members, anonymous, self-report, surveys were collected (see Table 2). These surveys were distributed to the lead of the adult day academy by members by the research team. Then, surveys were distributed among staff members. Once complete, surveys were returned to the lead of the adult day academy and then given back to the research team. Identifying information was not included in social validity surveys. This survey was eight questions long and included a Likert-scale with five possible answers. An opportunity to provide open-ended feedback was included.
Table 2.
Social validity questions and results: Staff
| Social validity questions | Average rating |
|---|---|
| 1. To what extent do you feel this intervention seemed effective in increasing communication (teachers or peers) during mealtimes? | 4.5 |
| 2. To what extent do you feel this intervention seemed effective in increasing engagement during mealtimes? | 4.75 |
| 3. To what extent do you feel this intervention seemed effective in increasing consumer’s repertoire of conversational topics during mealtimes? | 4.75 |
| 4. To what extent do you feel this intervention seemed effective in decreasing consumer engagement in challenging behavior? | 3.5 |
| 5. To what extent do you feel that this intervention seemed effective in increasing confidence in teachers to support consumers during mealtimes? | 3.25 |
| 6. To what extent do you feel that this intervention seemed effective in increasing interactions among consumers and staff outside mealtimes? | 3.25 |
| 7. To what extent do you feel that this intervention seemed effective in increasing friendships among consumers? | 2.75 |
| 8. To what extent do you feel that this intervention seemed effective in increasing community membership (feeling of group belonging) among consumers? | 2.75 |
Note. The scale was 1 = very ineffective to 5 = very effective.
Effect Size Estimation
In addition to visual analysis, the percentage of nonoverlapping (PND; Scruggs et al., 1987) was used to analyze the effects of intervention. To calculate this, we calculated the proportion of data points in intervention conditions that exceeded the highest data point in the baseline conditions. We followed Scruggs et al. 's (1987) recommendation that interventions with no clear differences have a PND less than 50, moderately effective interventions have a PND between 50 and 70, and the most effective interventions have a PND greater than 70.
Results
Conversation Engagement
In comparison to baseline, implementation of the Snack Talk intervention resulted in increased conversation engagement across all participants (see Figs. 3, 4, 5, 6 and 7).
Fig. 3.
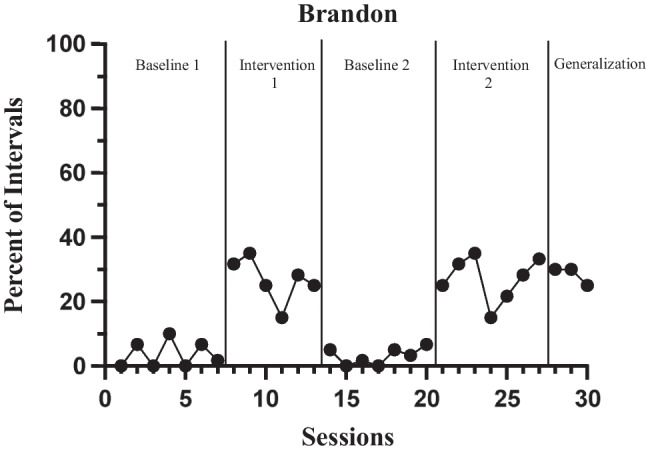
Percent of intervals Brandon engaged in conversation
Fig. 4.
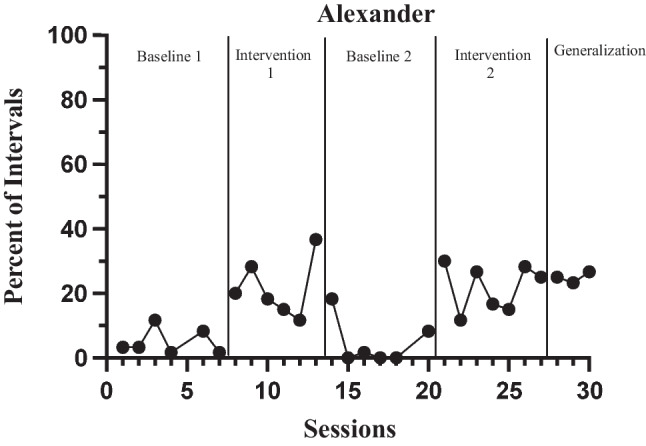
Percent of intervals Alexander engaged in conversation
Fig. 5.
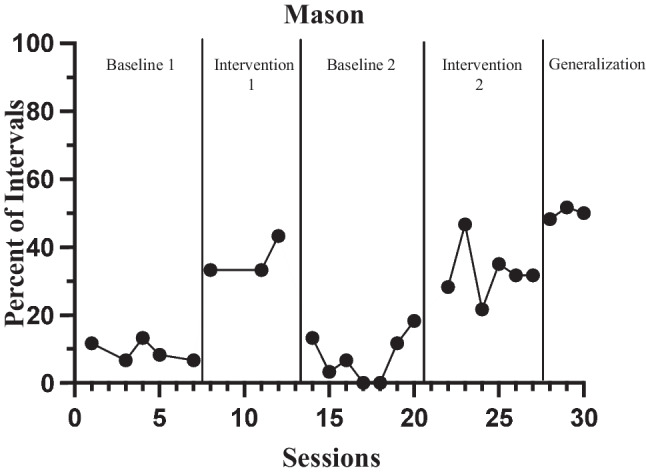
Percent of intervals Mason engaged in conversation
Fig. 6.
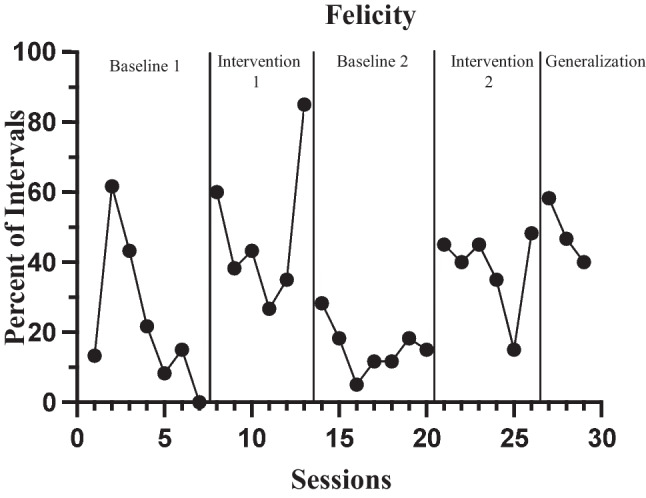
Percent of intervals Felicity engaged in conversation
Fig. 7.
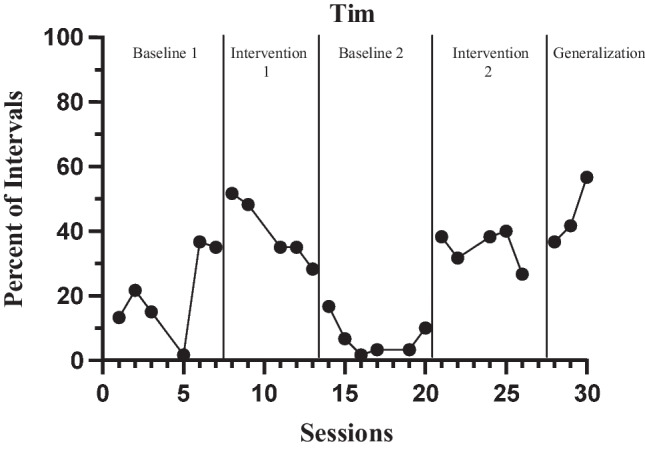
Percent of intervals Tim engaged in conversation
Brandon engaged in low levels of conversation with teachers and peers during baseline phases, ranging from 0% to 10% of intervals (M = 3.3%, SD = 3.3%; see Fig. 3). When the intervention was implemented, Brandon showed an immediate increase in conversation engagement, ranging from 15% to 35% of intervals (M = 26.2%, SD = 6.3). There was no overlap between baseline and intervention sessions, with levels of conversation engagement consistently higher in the intervention phases. PND was calculated and = 100%. During the maintenance phase, Brandon continued to show relatively stable and high levels of conversation engagement (range: 25%–30%, M = 28.3%, SD = 2.9%).
Alexander engaged in low levels of conversation with teachers and peers during baseline phases, ranging from 0% to 18% of intervals (M = 4.9%, SD = 5.7%; see Fig. 4). When the intervention was implemented, Alexander showed an immediate increase in the percentage of intervals with conversation engagement, ranging from 12% to 37% of intervals (M = 21.8%, SD = 7.9%). Although overlap occurred between baseline and intervention sessions (six sessions), overall levels of conversation engagement were consistently higher during intervention. PND was calculated and = 54%. During the maintenance phase, Alexander continued to show stable, high levels of engagement in conversation (range: 23%–27% of intervals, M = 25%, SD = 1.7%).
Mason engaged in low levels of conversation with teachers and peers during baseline phases, ranging from 0% to 18% of intervals (M = 8.3%, SD = 5.6%; see Fig. 5). When the intervention was implemented, Mason showed an immediate increase in the percentage of intervals with conversation engagement, ranging from 22% to 47% of intervals (M = 33.9%, SD = 7.5%). Although there was a slight upward trend towards the end of Mason’s second intervention phase, the overall results show no overlap between baseline and intervention sessions and the immediate change in behavior that was evident when the first intervention phase was introduced and withdrawn. PND was calculated and = 100%. During the maintenance phase, Mason continued to show stable and high levels of conversation engagement (range: 48%–52% of intervals, M = 50%, SD = 1.7%).
Felicity engaged in inconsistent and variable levels of conversation engagement with teachers and peers during baseline phases, ranging from 0% to 62% of intervals (M = 19.4%, SD = 16.1%; see Fig. 6). When the intervention was implemented, Felicity showed an immediate increase in the percentage of intervals with conversation engagement, ranging from 15% to 85% of intervals (M = 43.1%, SD = 17.3%). Elevated levels of conversation engagement were evident in both intervention phases compared to baseline. However, Felicity’s data showed considerable variability within phases, as well as overlap between baseline and intervention (six sessions). PND was calculated and = 54%. During the maintenance phase, Felicity showed stable and high levels of conversation engagement (range: 40%–46% of intervals, M = 48.3%, SD = 9.3%).
Tim engaged in low levels of conversation with teachers and peers during baseline phases, ranging from 2% to 37% of intervals (M = 13.8%, SD = 12.2%; see Fig. 7). When the intervention was implemented, Tim showed an immediate increase in conversation engagement, ranging from 27% to 52% of intervals (M = 37.3%, SD = 8.0%). Overall, higher levels of conversation engagement were seen in intervention phases compared with baseline. However, Tim’s data showed considerable variability within phases, as well as overlap (five sessions) between baseline and intervention. PND was calculated and = 50%. Further, Tim showed an increasing trend in conversation engagement during the maintenance phase (range: 37%–57% of intervals, M = 45%, SD = 10.4%). The strength of functional control shown in Tim’s data is somewhat limited by undesirable trends in the first baseline and intervention phases. However, the consistently high levels of conversation engagement during the second intervention and maintenance phase suggest that the intervention was ultimately effective.
Social Validity
Social validity results from participants suggested that all participants reported that they enjoyed using Snack Talk (see Table 3). All participants responded “Yes” to all questions. In addition, participants indicated increased friendships when using these supports and wanted to continue using Snack Talk supports following completion of this intervention.
Table 3.
Social validity questions and results: Participants
| Social validity questions | Respondent percentages | ||
|---|---|---|---|
| Yes | Sometimes | No | |
| 1. Did you talk to your friends using the mealtime cards? | 100% | 0% | 0% |
| 2. Did you enjoy using the mealtime cards to talk to your friends? | 100% | 0% | 0% |
| 3. Do you think you have more friends when you use the mealtime cards? | 100% | 0% | 0% |
| 4. Do you want to continue using the mealtime cards to talk to your friends? | 100% | 0% | 0% |
Note. Percentages reported includes responses from all (5) participants
Social validity results suggested that all academy staff members found intervention to be moderately effective in increasing engagement in social conversation for adults diagnosed with ASD and DD (see Table 2). Feedback collected from the open-ended question included in the social validity questionnaire indicated that staff felt that implementation of Snack Talk played a role in increased social relationships with peers during mealtimes. In addition, anecdotal feedback from staff members identified the necessity of continued implementation outside of the intervention setting to ensure generalization.
Discussion
This study sought to examine the effects of implementation of Snack Talk with five adults diagnosed with DD and or/ ASD. Results indicated increased engagement in conversation for participants during intervention and maintenance phases, demonstrating moderate effect upon visual analysis of intervention. The level of behavior change shown during intervention phases was different for each participant, comparable to each participant’s learning history and current levels of support and communication development. The goal of this intervention was to increase engagement in reciprocal conversation with staff and peers.
In this study, participants had a wide range of language abilities, demonstrating the potential versatility of this intervention to support a diverse range of individuals. Participants who communicated using multiword, complex sentences were able to engage with peers who used one- to two-word phrases to communicate. This intervention serves as a vehicle to foster social communication, providing a context for community membership. Although an abundance of literature exists identifying meaningful outcomes of visual supports in early childhood and early intervention settings (e.g., Watson & DiCarlo, 2016; Zimmerman et al., 2017), this study extends this literature to the adult population of individuals diagnosed with ASD and other DD.
Social validity findings were mixed. Although the staff at the adult day support center rated the intervention as very effective in increasing the conversation engagement of adults with DD and/or ASD during mealtimes, their ratings of their confidence in implementing the intervention were lower. This may be due to their inconsistent exposure to intervention implementation, because researchers acted as implementers for the duration of the study with indirect involvement from center staff. We hypothesize it may also be due to the perceived lack of importance of the lunchtime routine. If staff members view this time as noninstructional, there may be more reluctance to implement an intervention during this time, lowering perceptions of intervention feasibility.
Social validity results from the staff and consumers also indicated differing assessments of intervention efficacy in increasing a sense of community membership and strengthening friendship ties with adult participants rating the intervention as more effective in increasing friendships and community membership. Exploring the differences in definitions of friendship and community membership between individuals who staff adult support centers and the adults themselves is important when considering the intended goals of this intervention and its perceived efficacy. Results from the differing perspectives within the social validity surveys tentatively suggest that there may be a mismatch in definitions and the goal of friendship supports between the individuals who staff adult centers and the adults that attend them.
In addition, future research could extend this research to incorporate additional social skills related to social communication within the Snack Talk intervention protocol. Further, as reciprocal conversation engagement occurs consistently among participants, additional target skills can be targeted focusing on the social nuances of communication. This includes more formal, targeted instruction around turn taking in conversations, as well as timing and pacing and conversation elaboration.
Limited research exists identifying the effectiveness of ABA in adolescent and adult populations, as much of research funding targeting ASD is focused on early intervention. As a result, additional research examining the effects of ABA across the lifespan is needed. This study identifies the effectiveness of strategies and practices used in ABA in the adult population, demonstrating that individuals in this age group continue to learn and gain skills well into adulthood. In particular, findings from the current study contribute to literature on the use of ABA to increase communication and social and skills development in several ways. First, this study included adults with ASD and other DD, a group historically underresearched and underserved (Aguirre et al., 2015), as its participants. Participant and social validity outcomes suggest that Snack Talk is an effective intervention for supporting the conversation engagement and communication skill development of adults with DD. Second, Snack Talk uses a combination of research-based practices including modeling, use of visual supports, prompting, and reinforcement. This aligns with existing research suggesting that these practices are often effective in supporting communication and social skills development for not only children with ASD and DD, but also adults (Bates, 1980; Kleitsch et al., 1983; Lalli et al., 1991; Nuernberger et al., 2013). Finally, this study demonstrates the potential for embedding communication and social skills instruction within naturalistic contexts in adult service centers.
Limitations
This study has several limitations. First, implementation of the Snack Talk intervention occurred in a group format and participants moved through intervention conditions together. This approach was necessary because of the nature of the Snack Talk intervention, but limitations are present. This group format of implementation of intervention presents threats to internal validity, including each participant’s learning history. Further, it is possible that as intervention progressed, historical threats affected internal validity of intervention and ultimately created confounding variables to intervention. Future research should address historical threats to internal validity by exploring alternative research designs that account for the components of this intervention.
In addition to threats to internal validity, the prescribed phase changes through intervention conditions did not allow for participants to choose if they would like to use Snack Talk cards during mealtimes during intervention. Future research should incorporate choice of intervention, ensuring participants have autonomy over their own treatment and intervention.
Overall, a functional relation was demonstrated in this experiment, in that the level of conversation engagement was consistently higher during intervention compared to baseline for all five participants. However, greater variability and overlap between phases was observed for Felicity than the other participants. This variability could be attributed to frequent changes in medication and irregular attendance. Nevertheless, the effectiveness of the intervention is supported by the downward trend evident in both baseline phases, and the fact that consistently high levels of conversation engagement were seen for Felicity only when the intervention was in place. The higher data points in baseline indicate that Felicity may have had greater conversation engagement skills in her repertoire compared to the other participants prior to the intervention. Implementation of Snack Talk intervention may have resulted in Felicity engaging in conversation more consistently, however, issues pertaining to the appropriate levels of reciprocal conversation are present. In other words, as Felicity engaged in higher rates of conversation engagement, the question of what the ideal rate of reciprocal conversation arises. Future research should explore the appropriate levels of conversation engagement, tempering criteria for this skillset to ensure conversations are not one sided and include opportunities for both conversation partners to engage equally in conversation.
The data trends in the first two phases for Tim (initial baseline and first intervention) were less than optimal, because they were in the opposite direction of anticipated behavior change. However, such limitations are ultimately inevitable when phase change decisions must be made simultaneously for a group of participants. These undesirable trends were not seen in the latter phases for Tim, nor for the other participants.
The intervention required sustained involvement from implementers and staff. Intervention implementers implemented modeling, prompting, and social praise for both conversation initiations and bids throughout the intervention and postintervention generalization phases. Implementation of these additional behavioral strategies are expected when teaching new skills. Yet, the addition of these procedures could have confounded results, as it is possible the effects of intervention could have resulted from additional implementation of these behavioral strategies. However, this was anticipated as the focus of this study was on teaching procedures and initial phases of intervention using Snack Talk. Further, because participants may have had a lengthy reinforcement history contributing to social isolation, it was not expected that shifts in social communication would occur rapidly. It was also not anticipated that the participants would achieve complete independence in using Snack Talk within the relatively short time span of the current study. Therefore, this study did not include a formalized fading protocol to eliminate the role of staff. Least-to-most prompting was used to fade staff and implementers as the primary conversation partner, but future studies should examine procedures to fade other aspects of staff support, including reminders to use the Snack Talk supports and reinforcing individual conversational turns.
Because this intervention was inclusive of individuals with a wide range communication skill sets, conversation engagement data was collected as one single code and specific responses or topographies were not collected. Further, data specifically identifying instances of verbal or nonverbal conversation engagement were not disaggregated. In addition, data on initiations and responses, whether verbal or nonverbal, were also not collected. Future research should examine these behaviors separately to explore the effects of this intervention on the nuances of conversation engagement.
This study occurred during a naturally occurring activity in an applied setting. As a result, there are many confounding variables that may have affected conversation engagement that were not controlled for. For example, if an adult consumer, or multiple consumers, left the meal table during intervention, the frequency of opportunities were affected as fewer participants were at the table. Although this is a limitation in measurement procedures, we also view the naturalistic implementation of intervention in a setting like this one as a strength of this intervention.
Lastly, direct measurement of generalization to other peers and settings outside of intervention was not collected due to staffing and video consent constraints. This lack of generalization is reflected in social validity data collected from staff members. Future studies should include direct measures of generalization in order to capture a more comprehensive picture of the effects of the intervention beyond the training setting. Research focused on implementation of this intervention in community settings is recommended to inform future implementation.
Conclusion
As the number of adults with ASD and other DD continues to increase, targeted interventions aligned with the social nuances involved in navigating adulthood settings and relationships are needed. Snack Talk demonstrated the effectiveness of an easily adaptable ABA-based intervention designed to meet the individual communication and social needs of adults with ASD and other DD. Snack Talk supports are easily developed, and minimal training is needed for implementation, allowing for ease of application and high implementation fidelity. Social validity results indicate that the intervention is perceived as acceptable by service providers, but more important, it is also highly satisfactory to adults who experienced this intervention. These findings support the importance of skills that play a role in quality of life indicators for neurodiverse and neurotypical individuals. Participants liked this intervention and wanted to use it and were excited to engage with their peers during mealtimes with these supports.
Overall, results from the present study supply evidence that, despite numerous years of reinforcement of potentially isolating social communication behaviors, social communication skills for adults with ASD and other DD can be enhanced using ABA-based interventions. This study demonstrated that positive outcomes of implementation of good, evidence-based instruction are achievable throughout an individual's lifespan. These outcomes are especially important when put in the context of the lack of current funding mechanisms for intervention for adolescents and adults with ASD. This population is often denied access to meaningful intervention as a result of lack of funding (Gerhardt, 2009) due to a limited literature base that includes large randomized-control trial studies demonstrating the effectiveness of ABA for this population. This study demonstrates the effectiveness of intervention, highlighting positive outcomes of ABA across the lifespan.
With the support of individualized interventions that are aligned with the social expectations of adulthood settings, adults with ASD and other DD can experience an increase in engagement in sustained and meaningful conversations. This is critical because engagement in social communication during naturally occurring routines, such as mealtimes, fosters peer relationships and influences an individual’s ability to engage in the many social demands necessary to navigate adult life. Further, peer relationships and social networks play a large role in reducing feelings of isolation and increasing access to community networks. Providing individuals with the skills necessary to achieve these meaningful outcomes of life is a worthy objective and aligns with the goals of ABA to increase socially significant behaviors (Schwartz & Baer, 1991; Wolf, 1978).
Funding
This article was supported by the Supporting Transformative Autism Research (STAR) at the University of Virginia. Rose Nevill is an iTHRIV Scholar. The iTHRIV Scholars Program is supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Numbers UL1TR003015 and KL2TR003016
Data Availability
All data generated or analyzed during this study are included in this published article.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does contain a study with human or animal participants performed by the authors. This study was approved by IRB.
Informed Consent
This article does contain a study where informed consent was collected from participants.
Footnotes
The language used to describe individuals with disabilities is important. Many of us have been taught to use people-first language. Many autistic individuals prefer to use identity-first language. In our work, we use person-first language until an individual identifies the type of language they prefer.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Aguirre A, O’Neill J, Rehfeldt RA, Boyer V. Behavioral interventions for complex communication and social skills in adults with autism spectrum disorders. In: Tincani M, Bondy A, editors. Autism spectrum disorders in adolescents and adults: Evidence-based and promising interventions. Guilford Press; 2015. pp. 93–117. [Google Scholar]
- Association of Professional Behavior Analysts. (2019). Clarifications regarding applied behavior analysis treatment of autism spectrum disorder: practice guidelines for healthcare funders and managers (2nd ed.). Highlands Ranch, CO: Author. Retrieved from: https://www.apbahome.net/page/practiceguidelines
- Autism Speaks. (2020). State regulated health benefit plans. https://www.autismspeaks.org/state-regulated-health-benefit-plans. Accessed 22 Feb 2022.
- Baer, D. M., Wolf, M. M., & Risley, T. R. (1968). Some current dimensions of applied behavior analysis. Journal of Applied Behavior Analysis, 1(1), 91–97. 10.1901/jaba.1968.1-91 [DOI] [PMC free article] [PubMed]
- Baio, J., Wiggins, L., Christensen, D. L., Maenner, M. J., Daniels, J., Warren, Z., ... & Durkin, M. S. (2018). Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveillance Summaries, 67(6), 1–23. 10.15585/mmwr.ss6706a1 [DOI] [PMC free article] [PubMed]
- Bateman, K. J., Wilson, S. E., Gauvreau, A., Matthews, K., Gucwa, M., Therrien, W., Nevill, R., & Mazurek, M. (2022). Visual supports to increase conversation engagement for preschoolers with autism spectrum disorder during mealtimes: An initial investigation. Journal of Early Intervention. Advance online publication. 10.1177/10538151221111762
- Bates P. The effectiveness of interpersonal skills training on the social skill acquisition of moderately and mildly retarded adults. Journal of Applied Behavior Analysis. 1980;13(2):237–248. doi: 10.1901/jaba.1980.13-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Mazefsky CA, Eack SM. The combined impact of social support and perceived stress on quality of life in adults with autism spectrum disorder and without intellectual disability. Autism. 2018;22(6):703–711. doi: 10.1177/1362361317703090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, Visser S, Kogan MD. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics. 2011;127(6):1034–1042. doi: 10.1542/peds.2010-2989. [DOI] [PubMed] [Google Scholar]
- Cooper JO, Heron TE, Heward WL. Applied behavior analysis. 3. Pearson; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldevik S, Hastings RP, Hughes JC, Jahr E, Eikeseth S, Cross S. Meta-analysis of early intensive behavioral intervention for childrenwith autism. Journal of Clinical Child & Adolescent Psychology. 2009;38(3):439–450. doi: 10.1080/15374410902851739. [DOI] [PubMed] [Google Scholar]
- Gast, D. L., & Ledford, J. R. (2014). Applied research in education and behavioral sciences. In Single case research methodology (pp. 1–18). Routledge.
- Gauvreau AN. Using “Snack Talk” to support social communication in inclusive preschool classrooms. Young Exceptional Children. 2017;20(4):187–197. doi: 10.1177/1096250617725503. [DOI] [Google Scholar]
- Gerhardt PF. The current state of services for adults with autism. Advancing Futures for Adults with Autism Think Tank; 2009. [Google Scholar]
- Gresham FM, Elliott SN. Social skills assessment and training in emotional and behavioral disorders. In: Walker HM, Gresham FM, editors. Handbook of evidence-based practices for emotional and behavioral disorders: Applications in schools. Guilford Press; 2014. pp. 152–172. [Google Scholar]
- Grob CM, Lerman DC, Langlinais CA, Villante NK. Assessing and teaching job-related social skills to adults with autism spectrum disorder. Journal of Applied Behavior Analysis. 2019;52(1):150–172. doi: 10.1002/jaba.503. [DOI] [PubMed] [Google Scholar]
- Haring TG, Roger B, Lee M, Breen C, Gaylord-Ross R. Teaching social language to moderately handicapped students. Journal of Applied Behavior Analysis. 1986;19(2):159–171. doi: 10.1901/jaba.1986.19-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haymes LK, Storey K, Maldonado A, Post M, Montgomery J. Using applied behavior analysis and smart technology for meeting the health needs of individuals with intellectual disabilities. Developmental Neurorehabilitation. 2015;18(6):407–419. doi: 10.3109/17518423.2013.850750. [DOI] [PubMed] [Google Scholar]
- Hill AP, Zuckerman KE, Fombonne E. Epidemiology of autism spectrum disorders. In: Volkmar FR, Rogers SJ, Paul R, Pelphrey KA, editors. Handbook of autism and pervasive developmental disorders. 4. Wiley; 2014. pp. 57–96. [Google Scholar]
- Hochman JM, Carter EW, Bottema-Beutel K, Harvey MN, Gustafson JR. Efficacy of peer networks to increase social connections among high school students with and without autism spectrum disorder. Exceptional Children. 2015;82(1):96–116. doi: 10.1177/0014402915585482. [DOI] [Google Scholar]
- Hood SA, Luczynski KC, Mitteer DR. Toward meaningful outcomes in teaching conversation and greeting skills with individuals with autism spectrum disorder. Journal of Applied Behavior Analysis. 2017;50(3):459–486. doi: 10.1002/jaba.388. [DOI] [PubMed] [Google Scholar]
- Howlin P, Moss P, Savage S, Rutter M. Social outcomes in mid- to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(6):572–581. doi: 10.1016/j.jaac.2013.02.017. [DOI] [PubMed] [Google Scholar]
- Hughes C, Golas M, Cosgriff J, Brigham N, Edwards C, Cashen K. Effects of a social skills intervention among high school students with intellectual disabilities and autism and their general education peers. Research and Practice for Persons with Severe Disabilities. 2011;36(1–2):46–61. doi: 10.2511/rpsd.36.1-2.46. [DOI] [Google Scholar]
- Kleitsch EC, Whitman TL, Santos J. Increasing verbal interaction among elderly socially isolated mentally retarded adults: A group language training procedure. Journal of Applied Behavior Analysis. 1983;16(2):217–233. doi: 10.1901/jaba.1983.16-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krantz PJ, McClannahan LE. Social interaction skills for children with autism: A script-fading procedure for beginning readers. Journal of Applied Behavior Analysis. 1998;31(2):191–202. doi: 10.1901/jaba.1998.31-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kratochwill TR, Hitchcock JH, Horner RH, Levin JR, Odom SL, Rindskopf DM, Shadish WR. Single-case intervention research design standards. Remedial & Special Education. 2013;34(1):26–38. doi: 10.1177/0741932512452794. [DOI] [Google Scholar]
- Lalli JS, Pinter-Lalli E, Mace FC, Murphy DM. Training interactional behaviors of adults with developmental disabilities: A systematic replication and extension. Journal of Applied Behavior Analysis. 1991;24(1):167–174. doi: 10.1901/jaba.1991.24-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledford JR, Gast DL, editors. Single case research methodology: Applications in special education and behavioral sciences. Routledge; 2018. [Google Scholar]
- Levy A, Perry A. Outcomes in adolescents and adults with autism: A review of the literature. Research in Autism Spectrum Disorders. 2011;5(4):1271–1282. doi: 10.1016/j.rasd.2011.01.023. [DOI] [Google Scholar]
- Machalicek W, Douglas A, Drew C, Barton H, Erturk B, Brafford T. Applied behavior analysis and intellectual and developmental disabilities. In: Glidden LM, Abbeduto L, McIntyre LL, Tassé MJ, editors. APA handbook of intellectual and developmental disabilities: Clinical and educational implications: Prevention, intervention, and treatment. American Psychological Association; 2021. pp. 23–53. [Google Scholar]
- Massey SL. Teacher–child conversation in the preschool classroom. Early Childhood Education Journal. 2004;31(4):227–231. doi: 10.1177/1088357611405191. [DOI] [Google Scholar]
- Murdock LC, Hobbs JQ. Tell me what you did today: A visual cueing strategy for children with ASD. Focus on Autism & Other Developmental Disabilities. 2011;26(3):162–172. doi: 10.1177/1088357611405191. [DOI] [Google Scholar]
- Neidert PL, Dozier CL, Iwata BA, Hafen M. Behavior analysis in intellectual and developmental disabilities. Psychological Services. 2010;7(2):103. doi: 10.1037/a0018791. [DOI] [Google Scholar]
- Nuernberger JE, Ringdahl JE, Vargo KK, Crumpecker AC, Gunnarsson KF. Using a behavioral skills training package to teach conversation skills to young adults with autism spectrum disorders. Research in Autism Spectrum Disorders. 2013;7(2):411–417. doi: 10.1016/j.rasd.2012.09.004. [DOI] [Google Scholar]
- O'Keefe J, Siebenaler K. Adult day services: A key community service for older adults. Department of Health & Human Services; 2006. [Google Scholar]
- Reichow B, Wolery M. Comprehensive synthesisof early intensive behavioral interventions foryoung children with autism based on the UCLAyoung autism project model. Journal of Autismand Developmental Disorders. 2009;39(1):23–41. doi: 10.1007/s10803-008-0596-0. [DOI] [PubMed] [Google Scholar]
- Schwartz IS. Standing on the shoulders of giants: Looking ahead to facilitating membership and relationships for children with disabilities. Topics in Early Childhood Special Education. 2000;20:123–128. doi: 10.1177/027112140002000208. [DOI] [Google Scholar]
- Schwartz IS, Baer DM. Social validity assessments: Is current practice state of the art? Journal of Applied Behavior Analysis. 1991;24(2):189–204. doi: 10.1901/jaba.1991.24-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz IS, Kelly EM. Quality of life for people with disabilities: Why applied behavior analysts should consider this a primary dependent variable. Research & Practice for Persons with Severe Disabilities. 2021;46(3):159–172. doi: 10.1177/15407969211033629. [DOI] [Google Scholar]
- Scruggs TE, Mastropieri MA, Castro G. The quantitative synthesis of single-subject research: Methodology and validation. Remedial & Special Education. 1987;8:24–33. doi: 10.1177/074193258700800206. [DOI] [Google Scholar]
- Snow CE, Beals DE. Mealtime talk that supports literacy development. New Directions for Child & Adolescent Development. 2006;2006(111):51–66. doi: 10.1002/cd.155. [DOI] [PubMed] [Google Scholar]
- Steinbrenner JR, Hume K, Odom SL, Morin KL, Nowell SW, Tomaszewski B, Szendrey S, McIntyre NS, Yücesoy-Özkan S, Savage MN. Evidence-based practices for children, youth, and young adults with autism. University of North Carolina at Chapel Hill, Frank Porter Graham Child Development Institute, National Clearinghouse on Autism Evidence & Practice Review Team; 2020. [Google Scholar]
- Walton KM, Ingersoll BR. Improving social skills in adolescents and adults with autism and severe to profound intellectual disability: A review of the literature. Journal of Autism & Developmental Disorders. 2013;43(3):594–615. doi: 10.1007/s10803-012-1601-1. [DOI] [PubMed] [Google Scholar]
- Watson KJ, DiCarlo CF. Increasing completion of classroom routines through the use of picture activity schedules. Early Childhood Education Journal. 2016;44(2):89–96. doi: 10.1007/s10643-015-0697-2. [DOI] [Google Scholar]
- Wolf MM. Social validity: The case for subjective measurement or how applied behavior analysis is finding its heart. Journal of Applied Behavior Analysis. 1978;11(2):203–214. doi: 10.1901/jaba.1978.11-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong C, Odom SL, Hume KA, Cox AW, Fettig A, Kucharczyk S, Brock ME, Plavnick JB, Fleury VP, Schultz TR. Evidence-based practices for children, youth, and young adults with autism spectrum disorder: A comprehensive review. Journal of Autism & Developmental Disorders. 2015;45:1951–1966. doi: 10.1007/s10803-014-2351-z. [DOI] [PubMed] [Google Scholar]
- Zimmerman KN, Ledford JR, Barton EE. Using visual activity schedules for young children with challenging behavior. Journal of Early Intervention. 2017;39(4):339–358. doi: 10.1177/1053815117725693. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.