The predominant challenge in the management of substance use disorders (SUD) lies in the frequent recurrence of use (relapse) and patient departure from treatment programs (dropout). These situations, more the rule than the exception, have been traditionally examined through comprehensive assessments of various factors we believe contribute to relapse, such as the severity of addiction, demographic elements, and life history [1]. Such factors are often assessed at treatment entry with structured interviews that are dependent on the patient’s retrospective self-reporting of a highly complex health condition.
Recent studies have shown potential in digital phenotyping individuals with SUD by leveraging Artificial Intelligence (AI) to predict treatment outcomes from social media posts alongside standard clinical records and structured interviews [2]. The study utilized a modern deep learning-based AI model, known as Bidirectional Encoder Representations from Transformers (BERT), to create a contextual “digital phenotype” from patients’ English Facebook posts prior to their intake into community-based SUD treatment programs. In this context, a digital phenotype refers to a quantitative characterization of an individual’s digital behavior, particularly their language use on social media platforms. This digital phenotype was then used to predict future SUD treatment outcomes, offering a novel approach to assessing the risk of adverse treatment outcomes (Fig. 1A).
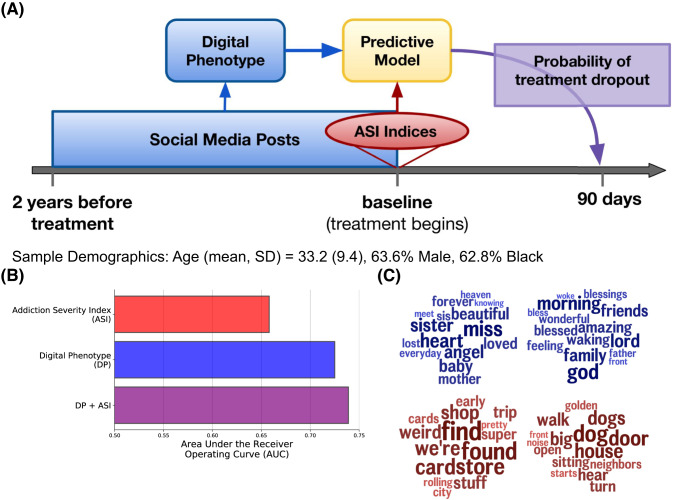
Fig. 1. Study design, Sample Demographics, and Results.
A Study design: language collected two years prior to starting treatment and surveys collected at intake are used to forecast the probability of each participant dropping out of treatment at 90 days. B Out of sample classification accuracy: predicting treatment dropout at 90 days. C Language most associated with treatment retention (blue) and treatment dropout (red).
We compared the predictive power of this social media language-based digital phenotype with that of the Addiction Severity Index [3], a widely used structured interview, to predict 90-day SUD treatment outcomes (a three-way classification task: abstinence, relapse, and dropout). Results showed that the digital phenotype outperformed the traditional interview method (AUC 0.725 vs. 0.658; Fig. 1B), via an out-of-sample cross-validation setup. This suggests that the digital phenotype, derived from patients’ social media language, could be a powerful tool for identifying patients at high risk for dropout at the beginning of treatment engagement.
Linguistic features from the digital phenotype indicated distinctive correlational patterns for those who remained in treatment versus dropped out (Fig. 1C) [4]. Those who stayed in treatment used more positive language with increased discussion of religion and family, both markers of social relationships. Discontinuing treatment was associated with diverse discussions of daily life, such as shopping and news, and more past-focused language, which can be associated with emotional distress [5].
In conclusion, this study represents a significant step forward in our understanding of how AI and social media can be used to improve outcomes for patients with SUD. Digital phenotypes, alongside traditional intake measures and other digital data sources, like electronic health records [6], could lead to quicker interventions and more efficient and accessible SUD assessments and treatments, ultimately reducing the cost of healthcare in this process. Future work would need to develop and validate a similar model for populations from different cultures, across languages, and over time. As we continue to explore the potential of AI and social media in neuropsychopharmacology, we must also navigate the ethical considerations and strive to ensure that these tools are used responsibly and effectively to improve patient outcomes.
Author contributions
SG and BC wrote the manuscript and prepared the figures.
Funding
This study was funded by the Intramural Research Program of the National Institutes of Health (NIH), National Institute on Drug Abuse (NIDA; ZIA DA000628).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McCaul ME, Svikis DS, Moore RD. Predictors of outpatient treatment retention: patient versus substance use characteristics. Drug Alcohol Depend. 2001;62:9–17. doi: 10.1016/S0376-8716(00)00155-1. [DOI] [PubMed] [Google Scholar]
- 2.Curtis, B, Giorgi, S, Ungar, L, Vu, H, Yaden, D, Liu, T, et al. AI-based analysis of social media language predicts addiction treatment dropout at 90 days. Neuropsychopharmacology. 2023. 10.1038/s41386-023-01585-5. [DOI] [PMC free article] [PubMed]
- 3.McLellan, AT, Alterman, AI, Metzger, DS, Grissom, GR, Woody, GE, Luborsky, L, et al. (1997). Similarity of outcome predictors across opiate, cocaine, and alcohol treatments: role of treatment services. In GA Marlatt & GR VandenBos (Eds.), Addictive behaviors: Readings on etiology, prevention, and treatment (pp. 718–58). (Reprinted from the “Journal of Consulting and Clinical Psychology,” 62, 1994, pp. 1141–1158) American Psychological Association. 10.1037/10248-028 [DOI] [PubMed]
- 4.Liu T, Giorgi S, Yadeta K, Schwartz HA, Ungar LH, Curtis B. Linguistic predictors from Facebook postings of substance use disorder treatment retention versus discontinuation. Am J Drug Alcohol Abus. 2022;48:573–85. doi: 10.1080/00952990.2022.2091450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shipp AJ, Aeon B. Temporal focus: thinking about the past, present, and future. Curr Opin Psychol. 2019;26:37–43. doi: 10.1016/j.copsyc.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Gianfrancesco MA, Tamang S, Yazdany J, Schmajuk G. Potential biases in machine learning algorithms using electronic health record data. JAMA Intern Med. 2018;178:1544–7. doi: 10.1001/jamainternmed.2018.3763. [DOI] [PMC free article] [PubMed] [Google Scholar]