Abstract
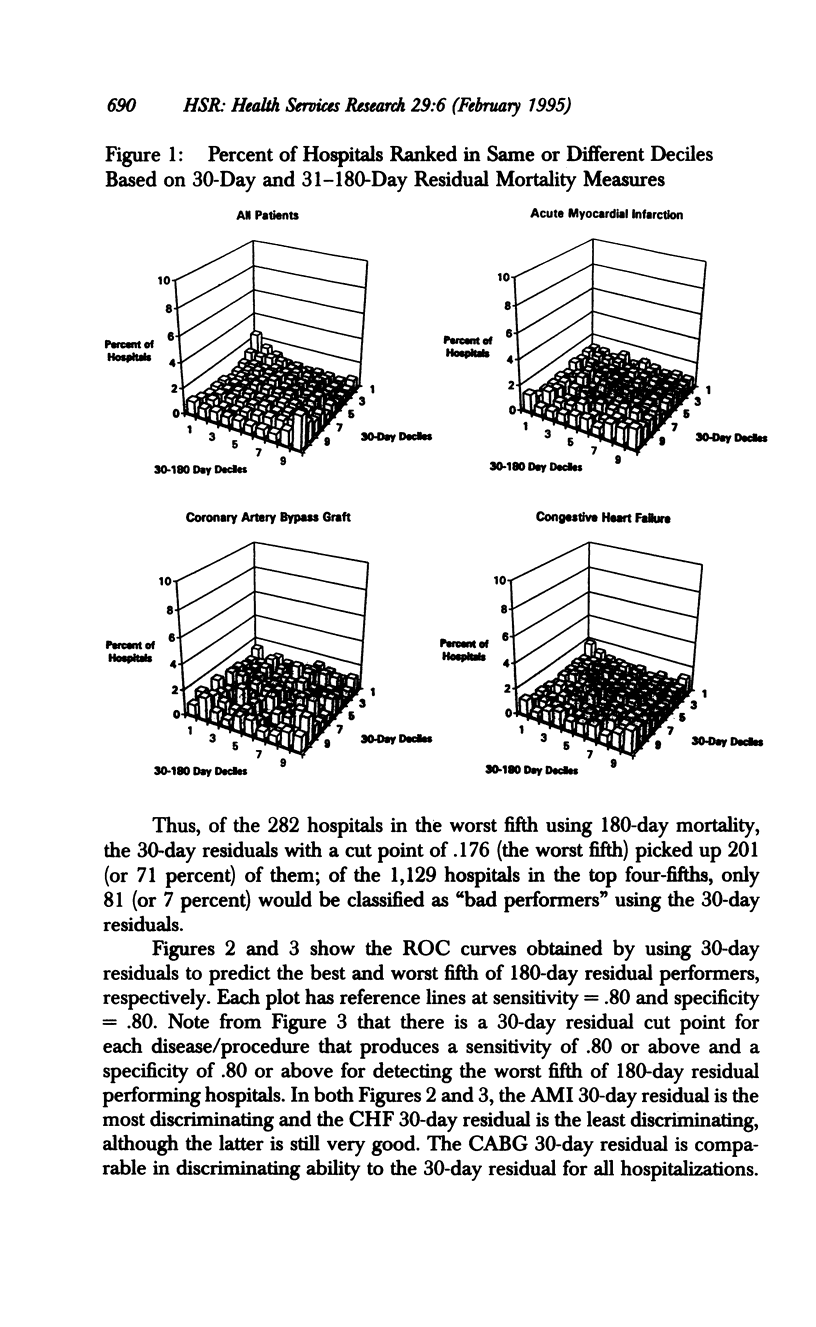
OBJECTIVE. We compare 30-day and 180-day postadmission hospital mortality rates for all Medicare patients and those in three categories of cardiac care: coronary artery bypass graft surgery, acute myocardial infarction, and congestive heart failure. DATA SOURCES/COLLECTION. Health Care Financing Administration (HCFA) hospital mortality data for FY 1989. STUDY DESIGN. Using hospital level public use files of actual and predicted mortality at 30 and 180 days, we constructed residual mortality measures for each hospital. We ranked hospitals and used receiver operating characteristic (ROC) curves to compare 0-30, 31-180, and 0-180-day postadmission mortality. PRINCIPAL FINDINGS. For the admissions we studied, we found a broad range of hospital performance when we ranked hospitals using the 30-day data; some hospitals had much lower than predicted 30-day mortality rates, while others had much higher than predicted mortality rates. Data from the time period 31-180 days postadmission yield results that corroborate the 0-30 day postadmission data. Moreover, we found evidence that hospital performance on one condition is related to performance on the other conditions, but that the correlation is much weaker in the 31-180-day interval than in the 0-30-day period. Using ROC curves, we found that the 30-day data discriminated the top and bottom fifths of the 180-day data extremely well, especially for AMI outcomes. CONCLUSIONS. Using data on cumulative hospital mortality from 180 days postadmission does not yield a different perspective from using data from 30 days postadmission for the conditions we studied.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Garnick D. W., Hendricks A. M., Comstock C. B. Measuring quality of care: fundamental information from administrative datasets. Int J Qual Health Care. 1994 Jun;6(2):163–177. doi: 10.1093/intqhc/6.2.163. [DOI] [PubMed] [Google Scholar]
- Hanley J. A., McNeil B. J. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982 Apr;143(1):29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- Luft H. S., Hunt S. S. Evaluating individual hospital quality through outcome statistics. JAMA. 1986 May 23;255(20):2780–2784. [PubMed] [Google Scholar]
- Rich M. W., Freedland K. E. Effect of DRGs on three-month readmission rate of geriatric patients with congestive heart failure. Am J Public Health. 1988 Jun;78(6):680–682. doi: 10.2105/ajph.78.6.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley G., Lubitz J. Outcomes of surgery among the Medicare aged: surgical volume and mortality. Health Care Financ Rev. 1985 Fall;7(1):37–47. [PMC free article] [PubMed] [Google Scholar]
- Romano P. S. Can administrative data be used to compare the quality of health care? Med Care Rev. 1993 Winter;50(4):451–477. doi: 10.1177/002570879305000404. [DOI] [PubMed] [Google Scholar]
- Roos L. L., Roos N. P., Sharp S. M. Monitoring adverse outcomes of surgery using administrative data. Health Care Financ Rev. 1987 Dec;Spec No:5–16. [PMC free article] [PubMed] [Google Scholar]
- Wennberg J. E., Roos N., Sola L., Schori A., Jaffe R. Use of claims data systems to evaluate health care outcomes. Mortality and reoperation following prostatectomy. JAMA. 1987 Feb 20;257(7):933–936. [PubMed] [Google Scholar]


