Abstract
Despite increasing prevalence and huge personal and societal burden, psychiatric diseases still lack treatments which can control symptoms for a large fraction of patients. Increasing insight into the neurobiology underlying these diseases has demonstrated wide-ranging aberrant activity and functioning in multiple brain circuits and networks. Together with varied presentation and symptoms, this makes one-size-fits-all treatment a challenge. There has been a resurgence of interest in the use of neurostimulation as a treatment for psychiatric diseases. Initial studies using continuous open-loop stimulation, in which clinicians adjusted stimulation parameters during patient visits, showed promise but also mixed results. Given the periodic nature and fluctuations of symptoms often observed in psychiatric illnesses, the use of device-driven closed-loop stimulation may provide more effective therapy. The use of a biomarker, which is correlated with specific symptoms, to deliver stimulation only during symptomatic periods allows for the personalized therapy needed for such heterogeneous disorders. Here, we provide the reader with background motivating the use of closed-loop neurostimulation for the treatment of psychiatric disorders. We review foundational studies of open- and closed-loop neurostimulation for neuropsychiatric indications, focusing on deep brain stimulation, and discuss key considerations when designing and implementing closed-loop neurostimulation.
Subject terms: Biomarkers, Translational research
Introduction
Psychiatric diseases have been notoriously difficult to treat, partly because of their heterogeneous presentations and constellations of symptoms. A growing body of research has shown alterations in functional activity in a variety of brain regions and across networks, often associated with specific manifestations of disorders or symptoms. This aberrant activity often normalizes with successful treatment or symptom reduction. Therefore, a rational treatment design approach could utilize this neural activity to both target therapy and assess the effects of treatment. This approach is particularly promising for neurostimulation therapies.
Neurostimulation refers to a collection of techniques which apply electrical, electromagnetic, or ultrasound energy to the nervous system with the intention of modulating activity. Modalities of stimulation can be non-invasive or invasive, and include transcranial electrical stimulation (tES), transcranial magnetic stimulation (TMS), transcranial focused ultrasound (tFUS), spinal cord stimulation (SCS), vagus nerve stimulation (VNS), and deep brain stimulation (DBS). Stimulation can be implemented using an open-loop or closed-loop approach. Open-loop stimulation is delivered continuously or with a fixed duty cycle; stimulation parameters are held constant in between device programming sessions. With closed-loop stimulation, a biomarker of neural activity, symptoms, or side effects is monitored and used to trigger treatment when that signal indicates that the target clinical state is detected. In this review, we focus on closed-loop DBS controlled by a neural activity biomarker; however, considerations for closed-loop stimulation can be applied to many of these stimulation modalities and can utilize biomarkers relying on physiological activity other than neural signatures. Foundational studies which demonstrated therapeutic efficacy of neurostimulation did so using open-loop techniques, where stimulation parameters were fixed in between clinician/researcher programming sessions and stimulation was either delivered continuously or with a predefined schedule, independent of neural activity, disease state, or symptom status. However, many psychiatric diseases manifest with varying temporal profiles of symptoms, some of which are highly episodic. In these cases, matching therapy to the time course of symptoms may result in better symptom control with fewer side effects. Furthermore, stimulation may be more effective when delivered during particular states. Our interest in closed-loop approaches is motivated by their promise to make possible treatment that is state targeted, matched to symptom time-course.
In an engineering control system, one set of algorithms is focused on monitoring the neural activity underlying disease symptoms, defined as the biomarker decoder, and another set of algorithms is focused on enacting the logic, defined as the biomarker actuator, that guides when, where, and how stimulation is delivered as a function of the biomarker. We adopt a broad definition of closed-loop neurostimulation - stimulation in which the timing and/or parameters of stimulation are algorithmically determined by the stimulation device based on a biomarker. Throughout the following sections, we seek to provide the reader with a framework for developing and implementing closed-loop stimulation for the treatment of psychiatric diseases. We start by reviewing the neurobiological basis for psychiatric disorders for which closed-loop DBS strategies have been designed and/or implemented: mood and anxiety spectrum disorders and obsessive-compulsive disorder (OCD). We next discuss the heterogeneity of psychiatric disease presentation and varying temporal dynamics of symptoms, both important for how closed-loop stimulation is designed at the individual and population levels. Following is an overview of the most common modalities of neurostimulation and promising results from DBS studies treating Major Depressive Disorder (MDD) and OCD with open-loop stimulation. We continue with a discussion of considerations and requirements for implementing closed-loop stimulation, along with a review of closed-loop studies in neurological disorders (where this approach has been more widely tested) and the pioneering closed-loop studies in MDD. The last section of this review discusses current challenges faced when implementing closed-loop neurostimulation. Throughout, we move beyond defining optimal circumstances and discuss closed-loop neuromodulation in the context of real-world limitations while also providing forward looking perspective on open questions, key challenges, and promising research directions.
Neurobiological basis for mood and anxiety spectrum disorders and OCD
There is a growing body of animal and human literature implicating a wide variety of neural circuit dysfunction in mood and anxiety spectrum disorders, including within the default mode network (DMN), salience network, reward network, and stress/threat network [1, 2]. Many of these studies use magnetic resonance imaging (MRI) and function MRI (fMRI), and are often underpowered to appropriately capture reproducible interindividual differences between brain structure or function and psychiatric symptomatology [3], which may explain some of the heterogeneity in results reported to date. However, some consistency in implicated regions has also emerged. The DMN, which primarily consists of areas in medial prefrontal cortices (mPFC), posterior cingulate cortex, and angular gyrus, is activated when individuals are not engaged in task or goal-directed behavior [4, 5], and has been implicated in episodic memory, self-referential processes, and rumination [6–8]. fMRI studies of patients with MDD have consistently shown hyperactivation within the DMN [9–11], with successful treatment associated with a reduction in this hyperactivity [12–15].
The salience network includes the anterior cingulate cortex (ACC), the anterior insula, amygdala, ventral striatum, hypothalamus, and thalamus [16, 17]. Studies of salience network connectivity in individuals with anxiety disorders have produced varied results, with increased connectivity observed in post-traumatic stress disorder (PTSD), particularly between the insula and the amygdala [18, 19], decreased connectivity in patients with generalized anxiety disorder (GAD), with anxiety symptoms being negatively correlated with amygdala-dorsolateral prefrontal cortex (dlPFC) coupling [20], and both increased and decreased connectivity reported in patients with social anxiety disorder [21–23]. A meta-analysis of resting-state fMRI data in patients with MDD revealed hypoconnectivity within the salience network [24]. A possible explanation for these varied results is that the salience network does not simply encode overall arousal or anxiety, but rather processes salience of interoceptive or external stimuli and coordinates the response of arousal, attentional, motor, and cognitive control systems, and that the regulation of these processes becomes dysfunctional in mood and anxiety spectrum disorders [1, 25].
The reward circuit has primary nodes in the ventral tegmental area and nucleus accumbens (NAc) (also referred to as the ventral striatum), and includes mPFC, amygdala, and hippocampus. Patients with MDD have consistently been observed to have hypoactivation in the reward circuit [26], and decreased connectivity within the left ventral striatum is associated with greater severity of depressive symptoms [27, 28]. It is hypothesized that deficits within this circuitry underlie symptoms of anhedonia. For example, patients with MDD display attenuated responses to unexpected reward in the left NAc and bilateral caudate [29]. Hypoactivation within the ventral striatum during reward anticipation is correlated with the severity of anhedonia in patients with MDD and activity normalized following treatment with an SSRI [30].
Negatively valanced stimuli and various stressors lead to activation of a network of regions that constitute the stress/threat network which includes the amygdala, hippocampus, ACC, insula, and mPFC [31]. Patients with mood and anxiety spectrum disorders display hyperactivity within the amygdala in response to sad/negative appearing faces and hypoactivation in response to happy/positive faces [32–34]. Further, patients with GAD display deficits in behavioral tasks that require spontaneous regulation of emotional conflict, and this deficit is associated with a failure to engage the pregenual anterior cingulate in ways that would inhibit activation of the amygdala [35]. The development of these stress and threat related neural circuits may contribute to risk of developing mood and anxiety disorders, as adolescents with a family history of depression display increased threat-related activation of the amygdala and decreased activation of the dlPFC compared to adolescents without this history [36–38].
OCD is characterized by intrusive thoughts and repetitive behaviors that are present in 1–2% of the general population. There is a greater degree of consensus regarding the neural circuitry underlying OCD compared to other psychiatric disorders. The dominant model for OCD involves hyperactivation of a recurrent set of circuits connecting the cerebral cortex to the basal ganglia, which can be described as cortico-striato-thalamo-cortical (CSTC) loops [39]. In particular, the ACC and OFC, in addition to their downstream targets in the caudate, are abnormally active at rest and have elevated activity during OCD provocation, which resolves with successful pharmacological or behavioral therapy [40].
Presentation of psychiatric diseases
Heterogeneous syndromes with constellations of symptoms
The complexity of psychiatric presentations has proven to be a substantial obstacle for studying and treating these disorders. Psychiatric disorders are not discrete entities, rather they are heterogenous syndromes that vary widely in etiology and pathophysiology, even within a specific diagnosis. There is growing recognition that the current Diagnostic and Statistical Manual of Mental Disorders (DSM) classification system does not capture the immense heterogeneity of symptomology nor reflect our growing understanding of the relationship between neurobiology and psychiatric illness [41, 42]. For example, using the DSM-V diagnostic criteria, MDD can be diagnosed using over 200 unique combinations of symptoms [43]. The breadth of this diversity was demonstrated in a survey of over 1500 individuals with MDD that found these patients met the diagnostic criteria in 170 different ways [44].
The Research Domain Criteria (RDoC) project developed by the National Institute of Mental Health was launched to facilitate continued research and understanding of psychiatric disorders unencumbered by traditional diagnoses and without siloing of discrete disorders [45]. The primary focus of RDoC is on identifying neural circuitry responsible for mental and behavioral functions of the brain. Shared circuitry across some disorders suggests that similar targets and methods may be viable across broad neuropsychiatric conditions while tailoring biomarker design.
Temporal dynamics of symptoms
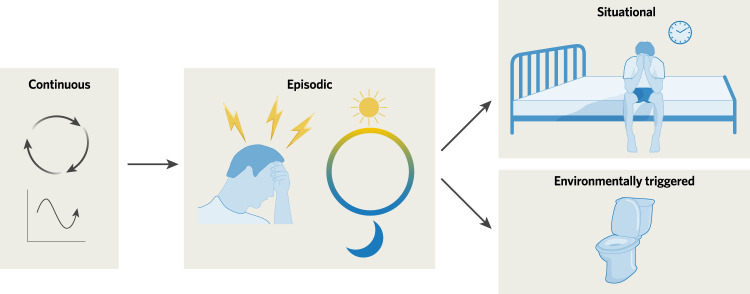
Symptoms of psychiatric diseases may be continuous or episodic, with some episodic symptoms related to situational (e.g. phobias) or environmental (e.g. patients with contamination OCD who must complete particular rituals after entering a bathroom) triggers (Fig. 1). Continuous symptoms may always be present, but typically vary in intensity and severity over a range of timescales. An episode of depression may last from weeks to years [46, 47]; however, individual symptoms (i.e. low mood, anhedonia, fatigue, cognitive symptoms, suicidal ideation, and anxiety) often fluctuate over the course of the day. Indeed, individuals with depression display greater variability in mood throughout the day compared to healthy controls [48]. Further, analyses from the Sequenced Treatment Alternative to Relieve Depression (STAR-D) Study revealed that approximately one quarter of individuals with depression experience diurnal variation in mood, with 31.9% of those experiencing morning worsening, 19.5% afternoon worsening, and 48.6% evening worsening [49]. Suicidality also displays predictable temporal variation; suicides are more likely to occur in the beginning of the week (peaking on Monday) and in the late morning/early afternoon, findings that have been replicated across decades and in numerous populations [50, 51].
Fig. 1. Symptoms of psychiatric diseases can be continuous or episodic.
Continuous symptoms often exhibit fluctuations in severity, while episodic symptoms may be associated with specific times, situations, or environments.
Episodic symptoms, including those that are environmentally triggered or situational, vary in their presence and severity. Panic attacks are discrete, time-limited surges of intense fear and anxiety that typically last minutes, which can be spontaneous or triggered by specific situations. The frequency of panic attacks varies widely, with some individuals reporting short periods of frequent attacks (e.g. daily), others reporting longer periods of 1–2 attacks per week, and others still reporting very infrequent attacks (e.g. several per year) [52–54]. Individuals with OCD experience symptoms such as anxiety, panic, disgust, or dissociation when confronted with situations that trigger their obsessions or compulsions; obsessions and compulsions themselves can be situationally triggered symptoms [54]. Interestingly, OCD symptoms may also have a diurnal component, with some patients experiencing peak symptoms around mid-day [55].
The temporal dynamics of psychiatric symptoms speaks for rationally-designed closed-loop neurostimulation treatments. Closed-loop systems could deliver treatment only when symptoms are present or when symptoms reach a certain severity. It may even be possible to deliver treatment preemptively before symptoms emerge.
Working towards closed-loop stimulation for neuropsychiatric diseases
Application of electrical current to the brain is not a modern invention. Use of electrical energy to relieve pain can be traced back to the ancient Romans in 15 A.D. [56]. Penfield used electric stimulation to map eloquent cortex and to localize epileptogenic areas in the 1950s [57]. The first spinal cord stimulator for pain relief was implanted in 1967 [58], and stimulation to mimic a ‘virtual lesion’ for Parkinson’s Disease was conceptualized and tested in the 1960s and 70 s. The FDA has approved several stimulation techniques and targets, including a handful for psychiatric indications over the past decade (Table 1).
Table 1.
Neurostimulation modalities.
| Modality | Description | FDA Approval Status |
|---|---|---|
| Non-Invasive | ||
| Transcranial Electrical Stimulation (tES) | Electrical current applied via electrodes on the scalp to elicit subthreshold modulation of brain activity. Waveforms include direct current (tDCS), alternating current (tACS), random noise (tRNS), and slow oscillatory direct current (soTDCS). | Not FDA approved or cleared |
| Transcranial Magnetic Stimulation (TMS) | A changing magnetic field is applied to the brain via a coil placed against the scalp; through electromagnetic induction, an electric current is elicited in targeted brain regions. Approaches include single and paired pulse TMS to elicit action potentials, and repetitive TMS to modulate excitability. |
- 2008: Cleared for MDD - 2013: Approved for treatment of pain from migraine with aura - 2017: Approved for migraine headache with aura - 2017: Approved for OCD - 2020: Cleared as aid for smoking cessation - 2021: Cleared for anxious depression |
| Non-Invasive Vagus Nerve Stimulation (VNS) |
A hand-held device applies mild electrical stimulation to the vagus nerve through the neck. (Transcutaneous auricular VNS, stimulation of the auricular branch of the vagus nerve that innervates the human ear, is being studied but is not FDA cleared) |
- 2017: Cleared for treatment of cluster headaches |
| Transcranial Focused Ultrasound (tFUS) | Short bursts of low intensity ultrasound are delivered from the scalp to modulate activity of deep structures with high spatial resolution. |
- 2016: Approved for ET - 2018: Approved for tremor dominant PD - 2021: Approved for treatment of patients with advanced PD suffering with mobility, rigidity, or dyskinesia |
| Invasive | ||
| Spinal Cord Stimulation (SCS) | Electrical stimulation is delivered to the epidural space. An implantable pulse generator (IPG) is implanted in the abdomen or buttocks. |
- 1989: Approved to treat chronic pain from nerve damage in the trunk, arms, or legs - 2015: Approved high frequency SCS - 2016: Approved burst SCS - 2022: Approved closed-loop SCS - 2022: Approved to treat multi-site pain |
| Implantable Vagus Nerve Stimulation (VNS) | Electrical stimulation is delivered to the Vagus Afferent Network, which includes brainstem, subcortical, and cortical structures [199]. An IPG is implanted in the chest and electrodes are wrapped around the cervical vagus nerve. |
- 1997: Approved for epilepsy in adolescents and adults (>12 years) [200] - 2005: Approved for difficult-to-treat depression - 2017: Approved for epilepsy in pediatrics (≥4 years) |
| Deep Brain Stimulation (DBS) | Electrical stimulation is delivered to the brain through strip or depth electrodes. An IPG is implanted in the chest or cranially. |
- 1997: Approved DBS in VIM for essential tremor and severe tremor in PD - 2002: Approved DBS in STN or GPi in advanced PD - 2003: HDE for DBS for dystonia - 2009: HDE for DBS for OCD - 2013: Approved RNS for medically refractory epilepsy - 2016: Approved DBS in PD patients diagnosed for at least four years who experience troublesome “off” periods or dyskinesia - 2018: Approved DBS for focal epilepsy - 2020: Approved DBS in VIM for ET |
FDA food and drug administration, MDD major depressive disorder, OCD obsessive compulsive disorder, ET essential tremor, IPG implantable pulse generator, PD Parkinson’s disease, VIM ventral intermediate nucleus of the thalamus, STN subthalamic nucleus, GPi internal segment of the globus pallidus, HDE humanitarian device exemption, RNS responsive neurostimulation system.
The therapeutic potential of a stimulation modality is typically first demonstrated using open-loop approaches, in which the timing of stimulation administration is predefined and fixed – stimulation can be on continuously or it can be intermittent (delivered with a set duty cycle). Therapy is delivered independent of symptom status with stimulation parameters that are static between programming sessions. In many cases, stimulation parameters for open-loop stimulation must be refined based on patient feedback and side effects and are updated by clinicians or researchers during programming visits. In this way, the clinician or researcher is ‘closing the loop’. However, throughout this review, we refer to closed-loop stimulation to mean algorithmically controlled stimulation by the device. Closed-loop paradigms are typically investigated to improve outcomes through better control of symptoms, decreased side-effects, or other improvement to patient experience (e.g. fewer surgeries for battery replacement). A biomarker, or biological marker, indicative of a particular state or symptom status is identified. Here, we discuss neural activity biomarkers. The biomarker is monitored by the device, and based on the programmed biomarker actuator, delivers stimulation or adjusts stimulation parameters. There are multiple subtypes of closed-loop stimulation with increasing sophistication. Responsive stimulation is triggered when a monitored biomarker achieves programmed detection criteria, typically a threshold; stimulation parameters are the same each time stimulation is triggered. In adaptive stimulation, the biomarker is continuously monitored, and stimulation parameters can dynamically change in response to shifting biomarker activity, according to a programmed biomarker actuator with multiple fix points or automated continuous adjustment.
Promising open-loop DBS results for MDD and OCD
Treatment resistant depression (TRD) does not have a universally accepted definition, but typically refers to failure to respond to antidepressant treatment given at a sufficient dose and duration. Comprehensive review of DBS targets for MDD is available [59], and we here highlight some key findings. The subgenual cingulate (SGC), which overlaps with Brodmann Area 25 and the subcallosal cingulate gyrus, was identified as a target for DBS for TRD based upon early imaging findings that this region is overactive when depressive symptoms are worse. Numerous open-label studies have demonstrated the safety and preliminary efficacy of SGC DBS [60–64]. However, a large (n = 90), prospective, randomized, sham-controlled multisite trial found no significant differences in depression relief between active and sham groups (20% vs 17%, respectively) at a predefined 6-month endpoint [65]. These disappointing results led investigators to consider if other factors such as sub-optimal placement of electrodes may be contributing to variable outcomes. Indeed, modeling of white matter connections using diffusion tensor imaging in 16 patients receiving SGC DBS showed that all responders shared bilateral pathways of activation to medial frontal cortex, rostral and dorsal cingulate cortex, and subcortical nuclei; these connections were not consistently found in non-responders [66]. Notably, a DBS study prospectively targeting these circuits found that after one year of DBS stimulation, 9 of 11 patients were responders and six were in remission [67]. Interestingly, open-label, long-term follow-up of 77 of 90 patients from the multi-site SGC DBS trial showed increasing response over time, with response rates of 29%, 53%, and 49% after 12, 18, and 24 months of stimulation, respectively, and remission in 14%, 18%, and 26% of patients, respectively [65]. Additional studies have also demonstrated enduring positive effects of SGC DBS, with an average response rate of 64.3% after 3–6 years in one study [62], and response rates at or above 50% and remission rates at or above 30% through years 2–8 of the follow-up period in another study [68].
Investigators began considering ventral capsule/ventral striatum (VC/VS) as a target for DBS in TRD based upon the observation that DBS at this target significantly reduced depressive symptoms in patients with OCD. Here, we define the VC/VS region to include the NAc, the more posterior bed nucleus of the stria terminalis, and overlying white matter tracts in the ventral anterior limb of the internal capsule (ALIC). Malone, et al. [69] trialed VC/VS DBS for primary refractory MDD, observing response rates of ~50% at 12 months. Subsequently, the first randomized clinical trial of VC/VS DBS for MDD did not find a significant difference between active and control group response rates [70]. However, a later trial incorporating a longer open-label optimization timeframe (up to 52 weeks vs up to 4 weeks used in [70]) followed by a randomized, blinded crossover discontinuation period detected a larger efficacy signal [71]. A report of 3 individuals with TRD showed rapid improvements in clinical ratings of depression when NAc DBS was turned on and increase in symptoms back to baseline (pre-treatment) levels when the stimulation was turned off [72]. In a study of 10 patients with TRD, half the participants achieved a 50% reduction in Hamilton Depression Rating Scale scores after 12 months of NAc DBS [73]. Long-term follow-up has demonstrated responder status maintained to 4 years after NAc DBS initiation [74].
The medial forebrain bundle (MFB), which includes dopaminergic neurons projecting from the VTA to NA, was chosen as a target for MDD because of its presumed role in reward processing [75]. The initial open-label pilot met its study endpoint with 6 of 7 participants responding to MFB DBS (>50% decrease in Montgomery-Asberg Depression Rating Scale [MADRS] score) [76]. Most patients were still responders, and some had reached remission at the 12-month follow-up [77]. Two randomized control trials have been conducted targeting MFB. One trial enrolled 16 patients and demonstrated relatively fast benefit of DBS, averaging within a week [78]. All patients responded at some point in the trial, and at 12 months, 50% of patients were considered to be in remission. However, after the 8-week blinded phase, the response rate with active or sham could not be differentiated due in part to sustained responses that seemed to last through the discontinuation phase. The other study is ongoing, but preliminary results from the first 4 patients indicate that three have responded so far with promising results [79]. Given the rapid response of MFB DBS, it is an interesting candidate for use in closed-loop therapies even though it remains understudied.
Approximately 10% of patients with OCD will have severe symptoms that do not respond to pharmacotherapy or cognitive therapies. Initially, DBS for OCD was targeted to the ALIC, which includes fibers connecting the PFC to the thalamus and basal ganglia. This initial DBS target was based on existing capsulotomy targets (about midway up the ALIC). The deepest electrode contacts were often placed within the VS/NAc region in front of the anterior commissure [80]. The target region gradually migrated back, closer to the junction of the VC and anterior commissure, with corresponding improvements in efficiency and lower required stimulation current [81]. This evolution had led to the target region being referred to as both ALIC (where it started) and VC/VS (where it is now). In 2009 the FDA granted Humanitarian Device Exemption for ALIC DBS for OCD. To date there has been strong evidence supporting DBS for treatment-resistant OCD [82].
The bed nucleus of the stria terminalis (BNST) is a component of the extended amygdala complex that resides posterior to the anterior commissure and the VS, situated beneath the VC. BNST DBS in OCD led to an initial 67% response rate and 83% response rate at last follow-up [83]. This was the first study to use an open-label optimization period in which a psychiatrist changed settings over the course of several months prior to the randomized double-blind crossover, and the excellent trial outcome was attributed to this novel trial design. While the BNST is thought to have an important role in anxiety and stress, it is also situated within cortico-basal ganglia-limbic fibers within the VC that broadly influence a larger network. Therefore, it is unclear whether therapeutic benefit stems from stimulation at a specific anatomical region such as the ventral striatum, BNST, or a larger white matter network that happens to reside close to one of these structures.
The subthalamic nucleus (STN) is a critical component of the basal ganglia implicated in OCD. It is organized along an axis in which prefrontal/medial forebundle inputs target more anteriomedial STN while sensory-motor systems connect dorsolaterally. The anteriomedial STN has been utilized as a DBS target based upon evidence from patients with co-morbid OCD who were treated using DBS for their movement disorders. These observations subsequently motivated randomized sham-controlled trials verifying the efficacy of this region as an OCD DBS target [84].
More recently, a connectomic model has been proposed that a central ALIC white matter pathway is the optimal target of DBS for OCD [85, 86]. This target is part of the hyper-direct pathway connecting the dorsal ACC and PFC to the anteriomedial STN. This model suggests that effective neuromodulation for OCD may be possible at various nodes within this circuit including at the VC/VS, BNST, and STN. Additional work has used tractography to look at connections between major DBS targets for OCD (ALIC, VS, medial STN, a midbrain target), finding numerous similar connections but some unique connections [87]. Ongoing and future work using non-invasive imaging may provide more insight into likelihood of response to therapy based on functional or anatomical data [67, 88].
Biomarkers
Biomarkers, such as measures of neural activity or state measured using iEEG, often serve as the control signal for closed-loop stimulation. Numerous other recording modalities, which may not be compatible with long-term closed-loop stimulation because of acquisition constraints, can provide valuable insight into neural processing and promising biomarkers. We focus on neurophysiological correlates and symptom tracking as biomarkers, but neurochemical monitoring of ions has also been suggested for controlling closed-loop stimulation (see [89] for a review).
Known regions of perturbed activity or circuit dysfunction (see section “Neurobiological Basis for Mood and Anxiety Spectrum Disorders and OCD”) can be a good starting point for biomarker discovery. However, this process is often constrained by real-world limitations, including temporally and spatially sparse data. While some neurological symptoms, mostly in the motor domain, can be continuously monitored, most psychiatric symptoms cannot be measured in this way. Rather, there are discrete measurement timepoints which, together with spatially and/or temporally limited biological process measurements, are used to calculate biomarkers. These discrete measurements often involve patient self-report or assessment completion.
A wealth of studies has looked at neurophysiological differences in patient populations vs. healthy controls or between clinical indications. For example, functional connectivity assessed using EEG showed increased theta and alpha functional connectivity in patients with MDD compared to healthy controls, with some of these connections being positively correlated with depression severity across the study sample [90]. Intracranial recordings conducted in patients receiving DBS demonstrated an alpha peak in BNST of patients with MDD but not those with OCD; this alpha power was positively correlated with state depression severity [91]. This is consistent with prior non-invasive electrophysiology studies establishing increased alpha activity as a hallmark of the depressive state [92, 93]. However, these studies do not assess any temporal relationship between symptom fluctuation and neurophysiology, thereby limiting their direct applicability as a control signal for closed-loop stimulation. A handful of studies have looked at neurophysiology that is temporally correlated with psychiatric symptoms. One study found that 10 and 15 min of iEEG gamma activity recorded from the amygdala of one patient with MDD was sufficient to detect a high symptom severity state, as determined from patient self-report metrics [94]. Delta power recorded from VC/VS in one OCD patient demonstrated strong negative correlation with self-reported symptoms; 2 min of iEEG data were used for each symptom report, with a total of 41 symptom ratings over a continuous 3-day at-home recording period [95]. Chronic VC/VS recordings in another OCD patient demonstrated right and left hemisphere alpha power suppression when OCD symptoms were lower [96]. A study in 11 patients with OCD demonstrated that neurophysiological correlates of symptom states are highly patient-specific [97]. Most neural signatures for psychiatric illnesses that have been identified to date are correlative, rather than causal, markers.
Distinct from biomarkers with tight temporal correlation to symptom fluctuation are physiological markers of disease state or treatment efficacy over time. Such information may be particularly important when clinical effects of DBS are delayed or accumulate. While currently available closed-loop devices do not use these types of biomarkers, future devices and more advanced algorithms may be able to incorporate such information. Additionally, while preferable to implement stimulation that does not result in any stimulation induced side-effects, this may not always be possible. In such cases, a biomarker for the side-effect can be used to further refine therapy delivery. Some devices can implement AND/OR logic between multiple detectors, allowing for more nuanced stimulation delivery incorporating the status of multiple different biomarkers.
Biomarker discovery is ongoing and will continue to be refined. Open questions and challenges include understanding if personalized biomarkers are required or if some neurophysiological correlates are conserved across patients. Additionally, more sophisticated measures of symptoms may be needed. Even in cases when neurophysiological markers are correlated with symptom fluctuation, the timescale of measured symptoms may not match the timescale of feedback needed to control stimulation.
Designing closed-loop neurostimulation
There are several fundamental questions to consider when designing closed-loop therapy: (1) What is the characteristic time scale of the biological process that is being tracked by the neural biomarker? (2) How responsive is the neural biomarker to changes in its correlate? (3) How quickly does stimulation modulate symptoms? (4) How does stimulation modulate the neural biomarker?
The time scale of the biological process of interest must be considered when determining the data to use for biomarker calculation and what computations are appropriate. For symptoms with fast time scales (periodic symptoms, those with rapid onset and offset), short snapshots of neural data temporally coincident with onset of symptoms may be effective for determining biomarkers. For symptoms which fluctuate more slowly, taking longer periods of neural data for biomarker calculation may facilitate averaging out variability unrelated to the symptom of interest.
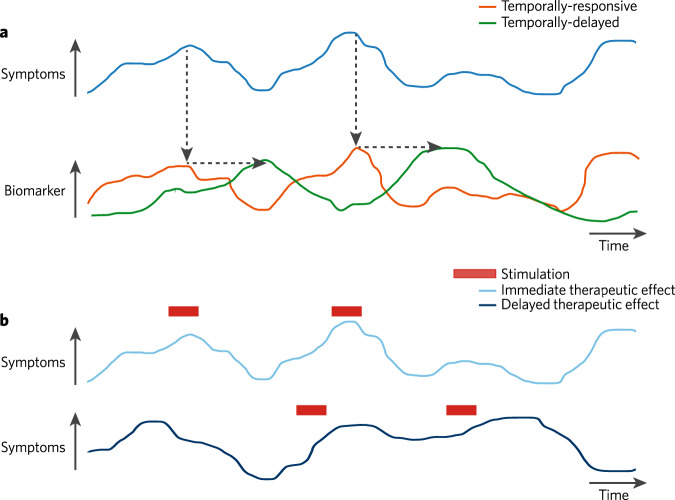
A related but distinct consideration is how rapidly neural biomarker activity adjusts when there is reduction or resolution of the symptom (Fig. 2a). A mismatch in temporal coupling between the neural biomarker and symptoms may lead to re-triggering of responsive stimulation unnecessarily and can preclude adaptive stimulation approaches. If these dynamics are well understood they can be accounted for in programming stimulation algorithms, device capability permitting.
Fig. 2. Considerations of temporal dynamics when designing closed-loop neurostimulation.
a As symptoms (blue) fluctuate, corresponding changes in the biomarker may be temporally-responsive (orange) or temporally-delayed (green). These relationships affect how the biomarker should be used to trigger stimulation. b Symptoms may reduce quickly in response to stimulation (top), or the therapeutic effect may be delayed or require more cumulative stimulation (bottom).
How quickly stimulation affects symptoms is typically determined empirically. Stimulation can lead to improvement of symptoms with delays ranging from seconds to weeks (Fig. 2b). The shorter end of this scale may depend on increase, decreases, synchronization, or desynchronization of local or network activity. In contrast, longer therapeutic wash-in may depend on plasticity as the mechanism of action.
How stimulation modulates the neural biomarker is often an afterthought, but this process can influence how stimulation should be administered longitudinally. Neural biomarkers more closely related to the physiological underpinning of a symptom or behavior are more likely to be directly influenced by stimulation that is effective at modulating the symptom or behavior. Biomarkers which are more removed correlates of a symptom may exhibit modulation on a time-scale that is not matched to the stimulation time course which may lead to unnecessary stimulations occurring when the target state arises. In cases when stimulation does not lead to timely modulation of neural biomarker activity, the design of closed-loop algorithms can be adjusted to pace the delivery of stimulation accordingly. Our understanding of the mechanism of action of DBS is incomplete. There are multiple explanations, including: inhibition of local neuronal firing (inhibition hypothesis), akin to a functional ablation, through depolarization block, inactivation of voltage-gated currents, and activation of inhibitory afferents; excitation of local neuronal elements (excitation hypothesis) that spreads through the network through spikes induced in the axon as well as antidromic propagation; and disruption of abnormal information flow (disruption hypothesis) across multiple brain areas [see [98, 99] for more detailed reviews]. There is also evidence that DBS acts through multifactorial mechanisms, with some immediate neuromodulatory effects as well as synaptic plasticity and long-term neuronal reorganization [100]. Adjusting stimulation parameters, such as frequency, produce fundamentally different network responses, likely with differing underlying mechanisms of action [101]. When measured at the level of extracellular electrophysiology and behavior, the mechanism of action of DBS likely depends upon cellular composition of the particular brain region being targeted, with considerations for the relative innervation by excitatory and inhibitory pathways.
Preliminary evidence from closed-loop neurostimulation studies
We next discuss studies of closed-loop neuromodulation in neuropsychiatric disorders. Learnings from closed-loop stimulation in chronic pain, movement disorders, epilepsy, and Tourette Syndrome can be applied to other neuropsychiatric indications. Some closed-loop devices are highly tailored to specific indications, such as SCS for pain relief (discussed more below). Other devices such as those using iEEG to deliver intracortical stimulation, while initially designed for one indication, can more readily be used for other indications. At present, there are two main companies which manufacture fully implanted devices capable of closed-loop intracranial stimulation. Neuropace manufactures the RNS System, a cranially-contained implant which includes an implantable neurostimulator (INS) and two leads. iEEG from bipolar channels is continuously processed by programmed detectors which utilize calculations optimized for the detection of seizure activity, including line-length, half-wave, and area under the curve [102]. If criteria for detection are met, bursts of stimulation are delivered using programmed stimulation parameters. Medtronic manufactures a selection of implantable closed-loop neurostimulation devices. Its Activa PC + S (primary cell battery) and Summit RC + S (rechargeable battery) [103] devices, previously available for investigational use, each contain two leads and an INS typically implanted in the chest. On-device processing first utilizes FFT to calculate spectral power with defined frequency cutoffs from select iEEG channels. These neural features are then used to determine state using linear discriminant analysis. Stimulation is delivered depending upon the determined state; this can be implemented with predefined stimulation parameters or in an adaptive mode. Medtronic’s commercially-available Percept PC device [104] (building on predecessor Activa PC + S technology) [105] also contains closed-loop capabilities, although these are currently only available for investigational use in the US market. Other closed-loop neurostimulation devices are under development and being tested [106].
As discussed below, subcortical brain regions often serve as therapeutic stimulation sites. However, cortical targets are often used for sensing biomarker activity and show improved decoding compared to subcortical sites in some indications. Cortical channels may also be less susceptible to certain types of artifacts, which can make closed-loop control more challenging [107].
Chronic pain
The most widely used neurostimulation modality for pain treatment is SCS, with some devices capable of closed-loop stimulation. Stimulation electrodes placed within the epidural space may shift with changes in body-position, thereby affecting the intensity of stimulation reaching nerves [108]. An initial closed-loop system using the RestoreSensor (Medtronic, Minneapolis, MN, USA) incorporated an accelerometer to measure body position and provide direct feedback for adjusting stimulation intensity; patients reported improved pain relief and greater convenience with the closed-loop mode compared to manually programmed adjustments [109]. Newer closed-loop SCS systems, such as the Evoke System (Saluda Medical, Bloomington, MN, USA), have incorporated real-time monitoring of spinal cord electrophysiology as a control signal biomarker. Multicenter, randomized control trial studies with intention-to-treat analyses of such closed-loop systems have been highly positive, revealing an overall improvement in pain relief and comfort without a worsening safety profile, as compared to open-loop systems [110, 111]. Recent work also shown promise in using cortical signals, particularly from OFC, to decode chronic pain intensity [112], paving the way for closed-loop stimulation controlled by neural biomarkers.
Movement disorders
Closed-loop DBS has been shown to be effective for treating symptoms of PD and essential tremor (ET). Unilateral closed-loop DBS in subthalamic nucleus (STN), controlled by beta activity in the same region, was superior to continuous or random intermittent stimulation (both forms of open-loop stimulation) for controlling motor symptoms in PD (contralateral hemibody Unified Parkinson’s Disease Rating Scale [UPDRS] motor scores), while delivering approximately 50% less total stimulation [113]; this study tested conditions for approximately 10 min, in a non-ambulatory setup utilizing leads connected to external equipment for processing and stimulation. A case-study in one PD patient extended these findings to ambulatory, freely moving test conditions [114]. A follow-up study to [113] assessed bilateral closed-loop stimulation in the STN in ambulatory conditions, with independent sense and stimulation control in each hemisphere; closed-loop stimulation led to a 43% reduction in blinded UPDRS scores relative to no stimulation (continuous stimulation was not tested) [115]. Furthermore, closed-loop DBS avoided speech impairment side-effects compared to continuous stimulation [116].
The preceding studies tested stimulation shortly following electrode implantation, a period susceptible to the ‘stun effect’, during which symptoms may be reduced independent of stimulation. To overcome this limitation [117], tested right-sided closed-loop DBS in a patient who had been implanted with bilateral STN electrodes for 14 years, showing better symptom control with closed-loop compared to continuous DBS. Additional studies, looking at stimulation over longer time periods, in the context of medication, or with multiple thresholds also support the efficacy of closed-loop stimulation [118–120].
Beta activity in the STN is the most commonly used biomarker for closed-loop DBS in PD. However, beta power may be attenuated with motor movements and is more susceptible to stimulation artifact contamination because the biomarker is recorded from the same region that is being stimulated. Using an alternative biomarker, closed-loop stimulation controlled by gyroscope signals from a wearable watch decreased tremor with stimulation on only 51.5% of the time [121]. Narrowband gamma activity recorded from motor cortex, a biomarker of dyskinesia, was also successful in controlling ipsilateral STN closed-loop stimulation, with maintained therapeutic efficacy and energy savings of 38–45% compared to continuous stimulation [122]. More recently, subcortical beta activity and cortical gamma activity were each used during naturalistic at-home closed-loop DBS to dynamically change stimulation amplitude based on the neural features reflecting motor fluctuations [123].
For the treatment of patients with ET, proof-of-concept testing demonstrated that surface electromyographic (EMG) activity of a patient’s tremulous forearm could inform timing of DBS in the ventral intermediate nucleus of the thalamus (VIM) [124]. Other closed-loop stimulation for ET has been controlled using EMG activity recorded from the biceps brachii muscle [125], an inertial sensor attached to the patients’ tremulous limb [126], and using neural activity detected from the M1 hand motor region [127].
Epilepsy
Real-time cortical stimulation for the abortion of seizures has long been observed and leveraged for intracranial cortical mapping applications [57, 128, 129]. Closed-loop stimulation for epilepsy was initially tested and found potentially beneficial in patients with subacute intracranial electrodes [130, 131]. Through a series of initial clinical trials, the chronically implanted RNS system provided improvement in the frequency of seizures compared to sham stimulation, including in a multicenter, double-blinded randomized control trial [132, 133], and in long-term follow up [134–136]. Although initially conceptualized to serve as a closed-loop abortive therapy, assessments of long-term efficacy have revealed a progressive reduction in the frequency of seizures over years with stimulation therapy [134–136].
In addition to direct brain stimulation, closed-loop VNS has been used as adjunctive therapy for refractory epilepsy. In 2015, the AspireSR M106 generator (LivaNova, London, UK) was released with cardiac-based seizure detection. In this closed-loop system, heart rate serves as the control signal, with the device delivering stimulation when a rapid increase in heart rate (presumably associated with seizures) is detected [137]. Closed-loop VNS has been demonstrated through prospective, multicenter clinical trials and retrospective chart studies to yield a moderate improvement in seizure frequency [137–141]; however, due to the limitations of being unable to perform a double-blind crossover, it remains an open question which factors most contribute to the improvement.
Tourette syndrome
Tourette Syndrome is characterized by paroxysmal motor or vocal tics and neuropsychiatric symptoms [142]. A first proof-of-concept case study of closed-loop stimulation for Tourette Syndrome utilized bilateral RNS System devices with leads in the centromedian-parafascicular (Cm-Pf) region of the thalamus [143]. Closed-loop stimulation was implemented using spectral power in the 5–15 Hz range (found to yield the best sensitivity for tics). Closed-loop stimulation was superior at symptom control compared to scheduled intermittent stimulation, with 64% vs. 53% improvement compared to pre-implant, respectively, on the Modified Rush Tic Rating Scale and 48% vs. 33% improvement, respectively, on the Yale Global Tic Severity Scale which reflects chronic clinical outcome. Another study with four individuals first determined optimal personalized settings of Cm-Pf stimulation using continuous, open-loop stimulation. Those stimulation parameters were then delivered using closed-loop stimulation, with equivalent success as open-loop stimulation in symptom reduction [144].
MDD
As of this writing, there have been few studies investigating closed-loop neurostimulation for the treatment of MDD. This likely stems from uncertainty on what biologic processes to focus on for development of biomarkers. There are currently at least three active trials of closed-loop stimulation for the treatment of MDD in the United States, two using combined EEG-rTMS (NCT04142320 and NCT03421808) and one using iEEG-DBS (NCT04004169). One of the EEG-rTMS trials aims to test whether synchronizing the delivery of rTMS with an individual’s frontal alpha rhythm will lead to improved treatment outcomes [145].
The trial of closed-loop DBS is investigating whether iEEG can be used to identify personalized neural biomarkers of depression and whether those biomarkers can be used to drive a safe and therapeutic closed-loop DBS system [146]. This trial includes a 10-day exploratory stage where iEEG electrodes (10 electrodes, each with 16 contacts) are implanted with distal contacts in the OFC, amygdala, hippocampus, VC/VS, and SGC bilaterally for the purpose of personalized biomarker identification and personalized stimulation target selection. If the patient demonstrates a positive response to stimulation in at least one of these contacts, an RNS System device is implanted in the most promising regions for stimulation and biomarker detection and patients undergo ongoing evaluation as the stimulation parameters and biomarker are optimized. Thus far, preliminary results from closed-loop DBS treatment of a single patient have been published. This patient, a 36-year-old woman, with severe TRD unresponsive to multiple antidepressant combinations and electroconvulsive therapy, demonstrated a robust response to stimulation of the VC/VS triggered by gamma activity within the amygdala [94].
Other studies have used neurophysiology to inform DBS using approaches other than closed-loop stimulation. A personalized medicine platform was developed in which an individual’s brain network is characterized in relation to their depressive phenotype and response to stimulation [147]. Intracranial electrophysiology can then be used to inform stimulation parameters that may be most effective for targeting these networks [148]. A transdiagnostic framework has also been described, in which functional domains are identified and targeted for treatment, cutting across traditional DSM-V diagnoses [149]. The goal of this framework is to address diagnostic overlap and heterogeneity within a single disorder. Identification of brain networks related to these transdiagnostic behavior and categories can then be targeted directly using DBS; indeed, closed-loop stimulation targeting one construct of this framework, cognitive control, improved performance on a conflict task during lapses in cognitive control [150].
Models of the therapeutic effects of closed-loop neurostimulation
In an ideal closed-loop model, a biomarker decoder infers symptom state and the biomarker actuator specifies stimulation strategy based on the biomarker. Closed-loop therapies are built on the assumption that symptom states fluctuate over time and that the fluctuations may be controlled acutely through timely delivery of stimulation or adjustment of stimulation parameters. One paradigm assume that the biomarker is an indication of current symptom state and that stimulation is delivered exclusively during the symptomatic state. We might expect that this cadence of state-dependent stimulation would be accompanied by problematic chronic fluctuation of symptoms. It would seem to require significant increases in symptoms to occur that would trigger stimulation that lowers symptoms. However, this has not been observed in real-world experience with closed-loop therapy. Instead, studies carried out to date suggest that treatment leads to sustained reduction in symptoms over the course of multiple closed-loop stimulation events delivered chronically [94, 136]. While future studies may indeed demonstrate up-and-down fluctuations in symptoms associated with closed-loop therapy, there are several possible explanations for why this does not occur.
First, we consider the possibility that the biomarker could be an indicator that an increase in clinical symptoms will soon occur rather than an indicator of current state. Currently, biomarkers are largely designed to reflect the onset and occurrence of the symptomatic state; and while there is ongoing work to design predictive biomarkers of future symptom state [151–153], these methods have not yet been incorporated into practice. Therefore, if the biomarker fluctuates concurrently with symptom state, then the actuator will deliver therapy during this inferred state and with the expectation that the patient will be driven out of the state. In this scenario, we would expect to see a change or worsening in symptoms before therapeutic stimulation is delivered or adjusted. Alternatively, if the biomarker is predictive of an upcoming symptom state, then the actuator will deliver or adjust therapy before entering the symptomatic state and with the expectation that the patient will be prevented from entering the state entirely. While fluctuation in symptom state would not be observed in this scenario, we would still expect to see fluctuation in the predictive biomarker. Indeed, this latter phenomenon of biomarker fluctuation distinct from fluctuations in symptom state has been observed and reported extensively in studies of closed-loop stimulation for epilepsy [154, 155]. Confirmatory studies to assess the veracity of the anticipatory mechanism of biomarker-triggered therapy in mood disorders is a key focus for future work.
A second potential explanation is that the effects of individual or multiple stimulations may have therapeutic effects that persist independently of fluctuations in the biomarker. The effects of stimulation on ongoing biomarker and symptom dynamics are poorly understood. Under the current model, we expect that therapeutic stimulation triggered by the biomarker would drive patients out of the symptomatic state. For a static closed-loop approach, in which stimulation is triggered based on the temporal dynamics of the biomarker, stimulation may attenuate the biomarker acutely, and therapy will continue ad infinitum based on the dynamics of the biomarker and be associated with significant symptom variability. However, sustained improvement without symptom fluctuation could occur if stimulation has two effects, one that is associated with relatively brief improvement that is linked to the biomarker and another that is associated with mechanisms linked to longer-lasting improvement that are not reflected in the biomarker, potentially associated with single stimulations or cumulative effects of multiple stimulations. Fluctuations in brain processes that are associated with symptom worsening and brief improvement could continue and trigger stimulations but might not be perceived clinically as they are overshadowed by the sustained symptom reduction occurring due to the other more sustained mechanisms.
A related third possibility is that repeated stimulation during the symptom state leads to plasticity that gradually conditions the brain to avoid entering the target clinical state entirely and decouples the biomarker from clinical state [156]. Stimulation over multiple closed-loop triggers could induce circuit plasticity [157–159] and reinforce brain states that protect the participant from symptom recurrence. Might changes in brain network connectivity sustain therapeutic benefit of closed-loop stimulation? A concrete answer to this question remains elusive, but we consider two possibilities. In one, we might observe change in brain network connectivity that is temporally correlated with a reduction in the occurrence of the symptom state and with a corresponding reduction in the occurrence of the biomarker signature of the target symptom state. A reduced biomarker occurrence rate would yield less frequent or no therapeutic stimulation. In this case, one would expect to see a decrease in the frequency of target state identifications by the biomarker and corresponding decrease in number of stimulations over time. Another possibility is that change in brain network connectivity uncouples the variability in symptom state from variation in the biomarker. Fluctuations in brain activity associated with the biomarker continue to trigger stimulation, but these fluctuations that are no longer tightly linked to symptom state, could play a role in maintaining therapeutic brain circuit changes chronically. Indeed, an open question is whether further stimulation is needed to maintain reorganized connectivity associated with therapeutic effects once the patient is in remission. In other words, should the biomarker actuator employ a rule for stimulation delivery that has a non-linear dependence on the relationship between the biomarker and symptoms? A stimulation strategy that is more flexible than threshold-based or linear-based dependence on the biomarker could potentially help maintain the therapeutic effect of closed-loop stimulation during periods of low symptom occurrence in the optimal way with the least intensity of intervention. Lastly, we consider the possibility that in some cases the best biomarker identifiable correlates poorly with symptom state. In such cases we would expect that fluctuations in the biomarker will trigger therapy but that the patient would receive stimulation across the complete spectrum of symptom states. If enough stimulation is delivered during states with significant symptoms, then the patient might still experience therapeutic benefit. However, this explanation assumes that the same type of stimulation delivered outside of symptom states has a neutral or favorable therapeutic effect on symptoms. An important question for future work is whether stimulation delivered in this manner is sufficient for preventing symptoms from emerging and maintaining therapeutic benefit.
Current challenges for closed-loop neurostimulation
Reliability and validity of psychiatric diagnoses and rating scales
Consistent diagnosis of disorders and assessment of psychiatric symptoms are critical for the success of closed-loop neurostimulation. Inaccurate diagnosis may lead to tracking of less relevant symptoms or attempts to determine a biomarker from the incorrect brain regions. If comorbid conditions are not diagnosed, multiple neurobiological circuits may contribute to what is perceived or tracked as a single symptom. Accordingly, a selected neural biomarker would only relate to part of the biological contribution to that symptom, thereby leading to poor relationship between symptoms and closed-loop stimulation. Broadly, rather than treating a diagnosed condition (which contains heterogeneous circuit dysregulation and resulting behavioral manifestations), utilizing the RDoC framework and targeting phenotypic clusters may provide more benefit for a particular functional deficit [160]. With regard to symptoms, the timeframe captured by standard severity or symptom assessments is often incompatible with requirements for neural biomarker discovery. For example, information regarding appetite or sleep function (measures that fluctuate on a slow time scale) do not directly aid in determining temporally-linked neural biomarkers.
Questions of noise, validity, and reliability in psychiatric ratings apply to both clinician-rated measures and patient self-reports. While clinician-rated scales are often considered the gold standard for assessment of depression symptoms, there are concerns that one of the most commonly used scales, the Hamilton Depression Rating Scale, may be psychometrically and conceptually flawed [161] and has limited sensitivity to change in depression severity [162]. Another commonly used scale, the Montgomery-Asberg Depression Scale, was originally published with an inter-rater reliability of 0.9 [162] but inter-rater reliability has also been measured at 0.57–0.76 [163]; some postulate that lower reliability may stem from lack of a structured interview. Many newer scales are still validated against older scales. In the case of self-report, scores from one individual may exhibit drift over time that is not actually related to change in symptoms. For example, ratings on a visual analog scale (VAS) of depression severity may show a general upward or downward trend because of an individual’s framing of what no symptoms (score of 0) should feel like vs what worse symptoms (score of 10) should feel like. It is particularly challenging to modify or correct these measures, as they are by definition a report from the patient related to their perception. While it remains to be seen if transfer learning can be applied to biomarkers of psychiatric symptoms, variability across participants in how they self-rate symptoms could complicate such attempts.
Concordance between clinician-rated scales and patient self-report also varies. A meta-analysis of studies which each included both forms of assessment, typically with different measures used between clinician ratings and self-report, found a significant difference in ratings of improvement in individuals with depression following psychotherapy [164]. Another study using both clinician-administered and self-report versions of the same scales (Inventory of Depressive Symptomatology, 16- and 30-items) with identical questions similarly found significant differences in scores, although they agreed for ~90% of patients in determining treatment response or remission to standard pharmaceutical treatment [165]. Given the shortcomings of all approaches of symptom assessment, a combination of multiple surveys [166] and approaches may provide a more comprehensive view of symptoms in order to determine highly correlated neural biomarkers.
Optimizing stimulation parameters
Stimulation parameters have typically been tested by ordered adjustment guided by expert opinion [167, 168] and updated through time-intensive trial-and-error testing. Such approaches are particularly onerous when response to DBS is delayed from parameter adjustment. Optimal settings for adaptive stimulation, in which stimulation parameters (e.g. contacts, amplitude, frequency, pulsewidth) are dynamically modulated based on the neural biomarker are even more challenging to elucidate. A number of approaches have been used to improve objective stimulation parameter selection. Machine learning of prospective fMRI data in patients receiving DBS for PD has identified brain activity patterns associated with clinical benefit and predicted optimal DBS settings [169]. Software algorithms can be used to optimize stimulation parameters to target a specific neuroanatomical target [170, 171]. Intracranial electrophysiology has also been used to facilitate determination of individually optimized DBS stimulation parameters using an inverse solution approach [148]. Continued improvement in rapid and objective stimulation parameter selection will be critical as the parameter space for stimulation grows with increasing number of implanted regions and greater device capability.
Chronic stability of biomarkers
Real-world application of therapeutic closed-loop neurostimulation requires continuous, precise, and reliable tracking of symptom-relevant neural biomarkers over long periods of time. A critical step in therapy optimization involves manually tuning the biomarker detection algorithm on a device. This calibration should occur during a biomarker discovery phase in which a definitive statistical decoder of the neural activity patterns related to symptoms is found, ideally before starting stimulation treatment. Indeed, sustained performance of closed-loop therapy relies on a temporally stable biomarker model – comprised of a biomarker decoder that maps brain activity patterns to symptoms and a biomarker actuator that maps observed neural biomarker intensity to stimulation delivery. Conventional design of closed-loop stimulation devices assumes that effective therapy attenuates, but does not impact, the relationship of the biomarker to the target clinical state [172–176]. Yet, it is possible over the course of chronic therapy that changes in brain or behavior alter the optimal neural biomarker [177]. To be clear, a change in the intensity of the biomarker does not necessarily indicate instability of the biomarker. Rather, gradual disruption of the mapping amongst biomarkers, symptoms, and stimulation could lead to misguided or mistimed therapy delivery and reduced efficacy and/or increased adverse effects.
Instability in the biomarker model could manifest at the level of the biomarker decoder or actuator. Conceptually, a biomarker decoder learns rules that govern how variability in symptom state is linked to variability in brain activity, and current approaches assume that these rules are static over time. If the rules learned by the decoder were to change, then the decoder’s ability to reliably predict symptom state may also degrade. A change in the decoder’s learning rule could stem from either a shift in behaviors and symptoms or a shift in brain physiology. Behaviorally, the phenotype of the patient’s disease-relevant symptom state or the way the patient codifies and quantifies their self-reported symptoms may change [178–182]. Neural encoding of new symptom phenotypes or of new subjective experiences reported by the patient may be linked to brain activity patterns distinct from those linked to the original symptoms and require refinement of the biomarker decoder. Physiologically, a shift in brain activity dynamics or in brain network plasticity might also drive instability of the biomarker. Specifically, the brain activity patterns that encode symptom states might gradually change, potentially due to reorganization of the brain network driven by neurodevelopment [183, 184], naturalistic fluctuation in symptoms [185, 186], changes in medication, or the emergence of new neuropsychiatric conditions [177]. Chronic stimulation therapy may also modify the brain’s encoding of symptoms by altering the excitability of neuronal populations [187–189] or by reorganizing connectivity between brain regions [157–159]. Altered brain activity patterns underlying symptom state would also impact the rules guiding stimulation delivery via the biomarker actuator. Indeed, algorithms driving the biomarker actuator could also suffer from instability. Stimulation parameters that optimally control the biomarker could shift over the course of therapy [190] and require periodic re-calibration. Change in this mapping could stem from waning effectiveness of the stimulation parameters or due to the aforementioned shift in the brain activity patterns that comprise the biomarker. Stimulation parameters that best control biomarkers of one brain region or of one signal pattern may not be optimal for others [191]. Therefore, routine quality assessment of the biomarker model is critical for long term reliability of closed-loop therapy.
Considerations for patient selection
DBS has proven to be generally safe and well tolerated, with retrospective analyses showing that surgical implantation carries an approximately 1% risk of intracranial hemorrhage, 2–3% risk of infection, and greater risk for more minor complications such as skin erosion [192–194]. Treatment with neurostimulation can cause side effects that impact speech, gait/motor control, cognition, and psychiatric symptoms [195]. Given this risk profile and the investment associated with DBS, careful consideration must be given to patient selection. Sufficient dose and duration of established therapies should have been trialed before implantation with DBS is considered. This results in only the most severe and refractory cases becoming candidates for DBS, which from a scientific standpoint limits our understanding of the efficacy of DBS in less severe manifestations of disease. Prospective DBS recipients should be no contraindications for surgery, which include consideration of cardiovascular health, anticoagulant use, and allergies to device components. History of seizures should be carefully assessed, as electrical stimulation may increase the risk of seizure (although the RNS System is an FDA-approved treatment for epilepsy). Patients should be capable of operating the peripheral equipment required for device charging and data upload, and capable of numerous clinic or researcher visits for device programming. We have found that caregiver or family support is critical not only for post-operative recovery but also throughout periods of therapy optimization. While less quantifiable, patients should have appropriate expectations for DBS, both in terms of the therapeutic efficacy and the time course of potential benefit. Some stimulation targets may not be well suited for intermittent, closed-loop stimulation if patients can notice when stimulation is turning on or off; in such cases, continuous stimulation may be preferable despite the lost advantages of closed-loop delivery.
Our group also considers other factors during patient selection to improve likelihood of successfully identifying a biomarker for closed-loop DBS. First, patients must display a significant degree of symptom variability. This is important because fluctuations in symptoms are necessary in order to identify biomarkers related to those symptoms (i.e. if a patient reports constant symptom severity, it will not be possible to link that symptom to neural activity). We typically look for a range of at least 25 points on a 0–100 VAS and verbal report that symptom severity can vary. We also favor patients that have had at least a partial response to other neurostimulation treatments such as electroconvulsive therapy (ECT) or rTMS; these treatments may have been abandoned due to intolerability of side effects or because responses were not sustained. Lastly, we carry out ‘mock’ testing sessions for a number of reasons: so that the patient can get a sense of what the experience will be like to aid in their deciding whether to participate; we can assess whether the patient can provide reliable data needed to assess treatment outcome and for biomarker development; and so that we can determine if the patient can tolerate the study procedures which include long, intensive periods of observation and the completion of repeated assessments.
Future research directions
Closed-loop methods have the potential to advance neurostimulation by identifying and detecting biomarkers that are relevant to an individual’s specific disorder manifestation and administering stimulation in a tailored manner. With the opportunity to provide feedback, the scope of tunable parameters exponentially increases from the open-loop approach. Considerable work remains to understand how best to optimize a complex control system that is dynamic over acute and chronic time scales and has multidimensional outputs. To this end, ongoing efforts include understanding how biomarker-triggered stimulation affects network and therapeutic responses. Although the current standard in the field is to obtain self-reported measures and clinician-rated scales, such ratings are confounded by potential temporal misalignment with the acquired neural data and survey fatigue [196]. To improve the utility of characterizations of patient symptom state, which is necessary for biomarker and stimulation response determination, future efforts need to expand the arsenal of validated measures, likely utilizing artificial intelligence combined with wearable sensors, video, and/or language processing [197, 198]. Finally, prospective efforts are required not only to compare closed-loop therapy with sham stimulation, but also to compare it to open-loop, intermittent, non-biomarker driven responses to fully determine whether there are benefits of the closed-loop technology that justify the significant procedures, time, and resources required to identify robust biomarkers of target symptom state.
Acknowledgements
The authors thank members of the Departments of Psychiatry and Behavioral Sciences, Neurology, and Neurological Surgery at the University of California, San Francisco for thoughtful discussion related to the present and future of therapeutic neurostimulation.
Author contributions
KKS, JLC, ANK, JMF, AML, EFC, and ADK made substantial contributions to the conception or design of the work. KKS, JLC, ANK, JMF, AML and ADK drafted the work or revised it critically for important intellectual content. KKS, JLC, ANK, JMF, AML, EFC, and ADK approved the final version to be published. EFC and ADK agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This work was supported by the Ray and Dagmar Dolby Family Fund through the Department of Psychiatry at UCSF. JLC is funded by R25MH060482. JMF is funded by the Doris Duke Charitable Foundation (grant #2021090).
Competing interests
ADK Grant Support: Janssen Pharmaceuticals, Axsome Pharmaceutics, Attune, Harmony, Neurocrine Biosciences, Reveal Biosensors; Consulting; Axsome Therapeutics, Big Health, Eisai, Evecxia, Harmony Biosciences, Idorsia, Janssen Pharmaceuticals, Jazz Pharmaceuticals, Millenium Pharmaceuticals, Merck, Neurocrine Biosciences, Neurawell Therapeutics, Otsuka Pharmaceuticals, Sage, Takeda, Angelini, Genentech. JLC served as a consultant for OptionsMD. The other authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Williams LM. Precision psychiatry: a neural circuit taxonomy for depression and anxiety. Lancet Psychiatry. 2016;3:472–80. doi: 10.1016/S2215-0366(15)00579-9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spellman T, Liston C. Toward circuit mechanisms of pathophysiology in depression. Am J Psychiatry. 2020;177:381–90. doi: 10.1176/appi.ajp.2020.20030280.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marek S, Tervo-Clemmens B, Calabro FJ, Montez DF, Kay BP, Hatoum AS, et al. Reproducible brain-wide association studies require thousands of individuals. Nature. 2022;603:654–60. doi: 10.1038/s41586-022-04492-9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fox MD, Snyder AZ, Vincent JL, Corbetta M, Essen DCV, Raichle ME. The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc Natl Acad Sci. 2005;102:9673–8. doi: 10.1073/pnas.0504136102.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raichle ME, Snyder AZ. A default mode of brain function: a brief history of an evolving idea. NeuroImage. 2007;37:1083–90. doi: 10.1016/j.neuroimage.2007.02.041.. [DOI] [PubMed] [Google Scholar]
- 6.Davey CG, Pujol J, Harrison BJ. Mapping the self in the brain’s default mode network. NeuroImage. 2016;132:390–7. doi: 10.1016/j.neuroimage.2016.02.022.. [DOI] [PubMed] [Google Scholar]
- 7.Whitfield-Gabrieli S, Moran JM, Nieto-Castañón A, Triantafyllou C, Saxe R, Gabrieli JDE. Associations and dissociations between default and self-reference networks in the human brain. NeuroImage. 2011;55:225–32. doi: 10.1016/j.neuroimage.2010.11.048.. [DOI] [PubMed] [Google Scholar]
- 8.Sestieri C, Corbetta M, Romani GL, Shulman GL. Episodic memory retrieval, parietal cortex, and the default mode network: functional and topographic analyses. J Neurosci. 2011;31:4407–20. doi: 10.1523/jneurosci.3335-10.2011.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sheline YI, Barch DM, Price JL, Rundle MM, Vaishnavi SN, Snyder AZ, et al. The default mode network and self-referential processes in depression. Proc Natl Acad Sci. 2009;106:1942–7. doi: 10.1073/pnas.0812686106.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greicius MD, Flores BH, Menon V, Glover GH, Solvason HB, Kenna H, et al. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol Psychiatry. 2007;62:429–37. doi: 10.1016/j.biopsych.2006.09.020.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Milazzo A-C, Ng B, Jiang H, Shirer W, Varoquaux G, Poline JB, et al. Identification of mood-relevant brain connections using a continuous, subject-driven rumination paradigm. Cereb Cortex. 2016;26:933–42. doi: 10.1093/cercor/bhu255.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Posner J, Hellerstein DJ, Gat I, Mechling A, Klahr K, Wang Z, et al. Antidepressants normalize the default mode network in patients with dysthymia. JAMA Psychiatry. 2013;70:373–82. doi: 10.1001/jamapsychiatry.2013.455.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ven V, van de, Wingen M, Kuypers KPC, Ramaekers JG, Formisano E. Escitalopram decreases cross-regional functional connectivity within the default-mode network. PLoS ONE. 2013;8:e68355. doi: 10.1371/journal.pone.0068355.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liston C, Chen AC, Zebley BD, Drysdale AT, Gordon R, Leuchter B, et al. Default mode network mechanisms of transcranial magnetic stimulation in depression. Biol Psychiatry. 2014;76:517–26. doi: 10.1016/j.biopsych.2014.01.023.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Daws RE, Timmermann C, Giribaldi B, Sexton JD, Wall MB, Erritzoe D, et al. Increased global integration in the brain after psilocybin therapy for depression. Nat Med. 2022:1–8. 10.1038/s41591-022-01744-z. [DOI] [PubMed]
- 16.Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007;27:2349–56. doi: 10.1523/jneurosci.5587-06.2007.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seeley WW. The salience network: a neural system for perceiving and responding to homeostatic demands. J Neurosci. 2019:1138–17. 10.1523/jneurosci.1138-17.2019. [DOI] [PMC free article] [PubMed]
- 18.Rabinak CA, Angstadt M, Welsh RC, Kenndy AE, Lyubkin M, Martis B, et al. Altered amygdala resting-state functional connectivity in post-traumatic stress disorder. Front Psychiatry. 2011;2:62. doi: 10.3389/fpsyt.2011.00062.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sripada RK, King AP, Welsh RC, Garfinkel SN, Wang X, Sripada CS, et al. Neural dysregulation in posttraumatic stress disorder. Psychosom Med. 2012;74:904–11. doi: 10.1097/psy.0b013e318273bf33.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Etkin A, Prater KE, Schatzberg AF, Menon V, Greicius MD. Disrupted amygdalar subregion functional connectivity and evidence of a compensatory network in generalized anxiety disorder. Arch Gen Psychiatry. 2009;66:1361–72. doi: 10.1001/archgenpsychiatry.2009.104.. [DOI] [PubMed] [Google Scholar]
- 21.Pannekoek JN, Veer IM, van Tol M-J, van der Werff SJA, Demenescu LR, Aleman A, et al. Resting-state functional connectivity abnormalities in limbic and salience networks in social anxiety disorder without comorbidity. Eur Neuropsychopharmacol. 2013;23:186–95. doi: 10.1016/j.euroneuro.2012.04.018.. [DOI] [PubMed] [Google Scholar]
- 22.Prater KE, Hosanagar A, Klumpp H, Angstadt M, Phan KL. Aberrant amygdala–frontal cortex connectivity during perception of fearful faces and at rest in generalized social anxiety disorder. Depress. Anxiety. 2013;30:234–41. doi: 10.1002/da.22014.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peterson A, Thome J, Frewen P, Lanius RA. Resting-state neuroimaging studies: a new way of identifying differences and similarities among the anxiety disorders. Can J Psychiatry. 2013;59:294–300. doi: 10.1177/070674371405900602.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaiser RH, Andrews-Hanna JR, Wager TD, Pizzagalli DA. Large-scale network dysfunction in major depressive disorder: a meta-analysis of resting-state functional connectivity. JAMA Psychiatry. 2015;72:603–11. doi: 10.1001/jamapsychiatry.2015.0071.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Menon V, Uddin LQ. Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct. 2010;214:655–67. doi: 10.1007/s00429-010-0262-0.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nestler EJ, Carlezon WA. The mesolimbic dopamine reward circuit in depression. Biol Psychiatry. 2006;59:1151–9. doi: 10.1016/j.biopsych.2005.09.018.. [DOI] [PubMed] [Google Scholar]
- 27.Cheng W, Rolls ET, Qiu J, Liu W, Tang Y, Huang C-C, et al. Medial reward and lateral non-reward orbitofrontal cortex circuits change in opposite directions in depression. Brain. 2016;139:3296–309. doi: 10.1093/brain/aww255.. [DOI] [PubMed] [Google Scholar]
- 28.Satterthwaite TD, Kable JW, Vandekar L, Katchmar N, Bassett DS, Baldassano CF, et al. Common and dissociable dysfunction of the reward system in bipolar and unipolar depression. Neuropsychopharmacology. 2015;40:2258–68. doi: 10.1038/npp.2015.75.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pizzagalli DA, Holmes AJ, Dillon DG, Goetz EL, Birk JL, Bogdan R, et al. Reduced caudate and nucleus accumbens response to rewards in unmedicated individuals with major depressive disorder. Am J Psychiatry. 2009;166:702–10. doi: 10.1176/appi.ajp.2008.08081201.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stoy M, Schlagenhauf F, Sterzer P, Bermpohl F, Hägele C, Suchotzki K, et al. Hyporeactivity of ventral striatum towards incentive stimuli in unmedicated depressed patients normalizes after treatment with escitalopram. J Psychopharmacol. 2012;26:677–88. doi: 10.1177/0269881111416686.. [DOI] [PubMed] [Google Scholar]
- 31.Kober H, Barrett LF, Joseph J, Bliss-Moreau E, Lindquist K, Wager TD. Functional grouping and cortical–subcortical interactions in emotion: a meta-analysis of neuroimaging studies. NeuroImage. 2008;42:998–1031. doi: 10.1016/j.neuroimage.2008.03.059.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stuhrmann A, Suslow T, Dannlowski U. Facial emotion processing in major depression: a systematic review of neuroimaging findings. Biol Mood Anxiety Disord. 2011;1:10. doi: 10.1186/2045-5380-1-10.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Victor TA, Furey ML, Fromm SJ, Öhman A, Drevets WC. Relationship between amygdala responses to masked faces and mood state and treatment in major depressive disorder. Arch Gen Psychiatry. 2010;67:1128–38. doi: 10.1001/archgenpsychiatry.2010.144.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robinson OJ, Krimsky M, Lieberman L, Allen P, Vytal K, Grillon C. The dorsal medial prefrontal (anterior cingulate) cortex–amygdala aversive amplification circuit in unmedicated generalised and social anxiety disorders: an observational study. Lancet Psychiatry. 2014;1:294–302. doi: 10.1016/s2215-0366(14)70305-0.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Etkin A, Prater KE, Hoeft F, Menon V, Schatzberg AF. Failure of anterior cingulate activation and connectivity with the amygdala during implicit regulation of emotional processing in generalized anxiety disorder. Am J Psychiatry. 2010;167:545–54. doi: 10.1176/appi.ajp.2009.09070931.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mannie ZN, Taylor MJ, Harmer CJ, Cowen PJ, Norbury R. Frontolimbic responses to emotional faces in young people at familial risk of depression. J Affect Disord. 2011;130:127–32. doi: 10.1016/j.jad.2010.09.030.. [DOI] [PubMed] [Google Scholar]
- 37.Swartz JR, Williamson DE, Hariri AR. Developmental change in amygdala reactivity during adolescence: effects of family history of depression and stressful life events. Am J Psychiatry. 2015;172:276–83. doi: 10.1176/appi.ajp.2014.14020195.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kujawa A, Burkhouse KL. Vulnerability to depression in youth: advances from affective neuroscience. Biol Psychiatry: Cogn Neurosci Neuroimag. 2017;2:28–37. doi: 10.1016/j.bpsc.2016.09.006.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Graybiel AM, Rauch SL. Toward a neurobiology of obsessive-compulsive disorder. Neuron. 2000;28:343–7. doi: 10.1016/S0896-6273(00)00113-6.. [DOI] [PubMed] [Google Scholar]
- 40.Brennan BP, Rauch SL. Functional Neuroimaging Studies in Obsessive-Compulsive Disorder: Overview and Synthesis. In: Pittenger C, Pittenger C (eds) Obsessive-compulsive Disorder: Phenomenology, Pathophysiology, and Treatment. Oxford University Press. 2017.
- 41.Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 2013;11:126. doi: 10.1186/1741-7015-11-126.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cuthbert BN. Research Domain Criteria: toward future psychiatric nosologies. Dialog Clin Neurosci. 2015;17:89–97. doi: 10.31887/dcns.2015.17.1/bcuthbert.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Diagnostic and statistical manual of mental disorders: fifth edition. American Psychiatric Association. 2013.
- 44.Zimmerman M, Ellison W, Young D, Chelminski I, Dalrymple K. How many different ways do patients meet the diagnostic criteria for major depressive disorder? Compr Psychiatry. 2015;56:29–34. doi: 10.1016/j.comppsych.2014.09.007.. [DOI] [PubMed] [Google Scholar]
- 45.Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research Domain Criteria (RDoC): toward a new classification framework for research on mental disorders. AJP. 2010;167:748–51. doi: 10.1176/appi.ajp.2010.09091379.. [DOI] [PubMed] [Google Scholar]
- 46.Kendler KS, Walters EE, Kessler RC. The prediction of length of major depressive episodes: results from an epidemiological sample of female twins. Psychol Med. 1997;27:107–17. doi: 10.1017/s0033291796003893.. [DOI] [PubMed] [Google Scholar]
- 47.Gilmer WS, Trivedi MH, Rush AJ, Wisniewski SR, Luther J, Howland RH, et al. Factors associated with chronic depressive episodes: a preliminary report from the STAR-D project. Acta Psychiatr Scand. 2005;112:425–33. doi: 10.1111/j.1600-0447.2005.00633.x.. [DOI] [PubMed] [Google Scholar]
- 48.Hall DP, Sing HC, Romanoski AJ. Identification and characterization of greater mood variance in depression. Am J Psychiatry. 1991;148:1341–5. doi: 10.1176/ajp.148.10.1341.. [DOI] [PubMed] [Google Scholar]
- 49.Morris DW, Rush AJ, Jain S, Fava M, Wisniewski SR, Balasubramani GK, et al. Diurnal mood variation in outpatients with major depressive disorder: implications for DSM-V from an analysis of the sequenced treatment alternatives to relieve depression study data. J Clin Psychiatry. 2007;68:1339–47. doi: 10.4088/JCP.v68n0903. [DOI] [PubMed] [Google Scholar]
- 50.Maldonado G, Kraus JF. Variation in suicide occurrence by time of day, day of the week, month, and lunar phase. Suicide Life Threat Behav. 1991;21:174–87. doi: 10.1111/j.1943-278X.1991.tb00464.x. [DOI] [PubMed] [Google Scholar]
- 51.Galvão PVM, Silva HRSE, da Silva CMFP. Temporal distribution of suicide mortality: a systematic review. J Affect Disord. 2018;228:132–42. doi: 10.1016/j.jad.2017.12.008.. [DOI] [PubMed] [Google Scholar]
- 52.Margraf J, Taylor B, Ehlers A, Roth WT, Agras WS. Panic attacks in the natural environment. J Nerv Ment Dis. 1987;175:558–65. doi: 10.1097/00005053-198709000-00008.. [DOI] [PubMed] [Google Scholar]
- 53.Norton GR, Harrison B, Hauch J, Rhodes L. Characteristics of people with infrequent panic attacks. J Abnorm Psychol. 1985;94:216–21. doi: 10.1037//0021-843x.94.2.216.. [DOI] [PubMed] [Google Scholar]
- 54.American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders (5th edition).
- 55.Nota JA, Gibb BE, Coles ME. Obsessions and time of day: a self-monitoring study in individuals with obsessive-compulsive disorder. J Cogn Psychother. 2014;28:134–44. doi: 10.1891/0889-8391.28.2.134.. [DOI] [PubMed] [Google Scholar]
- 56.Lam CM, Latif U, Sack A, Govindan S, Sanderson M, Vu DT, et al. Advances in spinal cord stimulation. Bioengineering. 2023;10:185. doi: 10.3390/bioengineering10020185.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Penfield W, Jasper H. Epilepsy and the functional anatomy of the human brain. Little, Brown & Co., Oxford, England. 1954.
- 58.Shealy CN, Mortimer JT, Reswick JB. Electrical inhibition of pain by stimulation of the dorsal columns: preliminary clinical report. Anesth Analg. 1967;46:489–91. doi: 10.1213/00000539-196707000-00025. [DOI] [PubMed] [Google Scholar]
- 59.Drobisz D, Damborská A. Deep brain stimulation targets for treating depression. Behav Brain Res. 2019;359:266–73. doi: 10.1016/j.bbr.2018.11.004.. [DOI] [PubMed] [Google Scholar]
- 60.Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, et al. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45:651–60. doi: 10.1016/j.neuron.2005.02.014.. [DOI] [PubMed] [Google Scholar]
- 61.Lozano AM, Mayberg HS, Giacobbe P, Hamani C, Craddock RC, Kennedy SH. Subcallosal cingulate gyrus deep brain stimulation for treatment-resistant depression. Biol Psychiatry. 2008;64:461–7. doi: 10.1016/j.biopsych.2008.05.034.. [DOI] [PubMed] [Google Scholar]
- 62.Kennedy SH, Giacobbe P, Rizvi SJ, Placenza FM, Nishikawa Y, Mayberg HS, et al. Deep brain stimulation for treatment-resistant depression: follow-up after 3 to 6 years. AJP. 2011;168:502–10. doi: 10.1176/appi.ajp.2010.10081187.. [DOI] [PubMed] [Google Scholar]
- 63.Holtzheimer PE, Kelley ME, Gross RE, Filkowski MM, Garlow SJ, Barrocas A, et al. Subcallosal cingulate deep brain stimulation for treatment-resistant unipolar and bipolar depression. Arch Gen Psychiatry. 2012;69:150–8. doi: 10.1001/archgenpsychiatry.2011.1456.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lozano AM, Giacobbe P, Hamani C, Rizvi SJ, Kennedy SH, Kolivakis TT, et al. A multicenter pilot study of subcallosal cingulate area deep brain stimulation for treatment-resistant depression: clinical article. J Neurosurg. 2012;116:315–22. doi: 10.3171/2011.10.JNS102122.. [DOI] [PubMed] [Google Scholar]
- 65.Holtzheimer PE, Husain MM, Lisanby SH, Taylor SF, Whitworth LA, McClintock S, et al. Subcallosal cingulate deep brain stimulation for treatment-resistant depression: a multisite, randomised, sham-controlled trial. Lancet Psychiatry. 2017;4:839–49. doi: 10.1016/S2215-0366(17)30371-1.. [DOI] [PubMed] [Google Scholar]
- 66.Riva-Posse P, Choi KS, Holtzheimer PE, McIntyre CC, Gross RE, Chaturvedi A, et al. Defining critical white matter pathways mediating successful subcallosal cingulate deep brain stimulation for treatment-resistant depression. Biol Psychiatry. 2014;76:963–9. doi: 10.1016/j.biopsych.2014.03.029.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Riva-Posse P, Choi KS, Holtzheimer PE, Crowell AL, Garlow SJ, Rajendra JK, et al. A connectomic approach for subcallosal cingulate deep brain stimulation surgery: prospective targeting in treatment-resistant depression. Mol Psychiatry. 2018;23:843–9. doi: 10.1038/mp.2017.59.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Crowell AL, Riva-Posse P, Holtzheimer PE, Garlow SJ, Kelley ME, Gross RE, et al. Long-term outcomes of subcallosal cingulate deep brain stimulation for treatment-resistant depression. AJP. 2019;176:949–56. doi: 10.1176/appi.ajp.2019.18121427.. [DOI] [PubMed] [Google Scholar]
- 69.Malone DA, Dougherty DD, Rezai AR, Carpenter LL, Friehs GM, Eskandar EN, et al. Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Biol Psychiatry. 2009;65:267–75. doi: 10.1016/j.biopsych.2008.08.029.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dougherty DD, Rezai AR, Carpenter LL, Howland RH, Bhati MT, O’Reardon JP, et al. A randomized sham-controlled trial of deep brain stimulation of the ventral capsule/ventral striatum for chronic treatment-resistant depression. Biol Psychiatry. 2015;78:240–8. doi: 10.1016/j.biopsych.2014.11.023.. [DOI] [PubMed] [Google Scholar]
- 71.Bergfeld IO, Mantione M, Hoogendoorn MLC, Ruhé HG, Notten P, van Laarhoven J, et al. Deep brain stimulation of the ventral anterior limb of the internal capsule for treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry. 2016;73:456–64. doi: 10.1001/jamapsychiatry.2016.0152.. [DOI] [PubMed] [Google Scholar]
- 72.Schlaepfer TE, Cohen MX, Frick C, Kosel M, Brodesser D, Axmacher N, et al. Deep brain stimulation to reward circuitry alleviates anhedonia in refractory major depression. Neuropsychopharmacol. 2008;33:368–77. doi: 10.1038/sj.npp.1301408.. [DOI] [PubMed] [Google Scholar]
- 73.Bewernick BH, Hurlemann R, Matusch A, Kayser S, Grubert C, Hadrysiewicz B, et al. Nucleus accumbens deep brain stimulation decreases ratings of depression and anxiety in treatment-resistant depression. Biol Psychiatry. 2010;67:110–6. doi: 10.1016/j.biopsych.2009.09.013.. [DOI] [PubMed] [Google Scholar]
- 74.Bewernick BH, Kayser S, Sturm V, Schlaepfer TE. Long-term effects of nucleus accumbens deep brain stimulation in treatment-resistant depression: evidence for sustained efficacy. Neuropsychopharmacol. 2012;37:1975–85. doi: 10.1038/npp.2012.44.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fenoy AJ, Quevedo J, Soares JC. Deep brain stimulation of the “medial forebrain bundle”: a strategy to modulate the reward system and manage treatment-resistant depression. Mol Psychiatry. 2022;27:574–92. doi: 10.1038/s41380-021-01100-6.. [DOI] [PubMed] [Google Scholar]
- 76.Schlaepfer TE, Bewernick BH, Kayser S, Mädler B, Coenen VA. Rapid effects of deep brain stimulation for treatment-resistant major depression. Biol Psychiatry. 2013;73:1204–12. doi: 10.1016/j.biopsych.2013.01.034.. [DOI] [PubMed] [Google Scholar]
- 77.Bewernick BH, Kayser S, Gippert SM, Switala C, Coenen VA, Schlaepfer TE. Deep brain stimulation to the medial forebrain bundle for depression- long-term outcomes and a novel data analysis strategy. Brain Stimulation. 2017;10:664–71. doi: 10.1016/j.brs.2017.01.581.. [DOI] [PubMed] [Google Scholar]
- 78.Coenen VA, Bewernick BH, Kayser S, Kilian H, Boström J, Greschus S, et al. Superolateral medial forebrain bundle deep brain stimulation in major depression: a gateway trial. Neuropsychopharmacol. 2019;44:1224–32. doi: 10.1038/s41386-019-0369-9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fenoy AJ, Schulz P, Selvaraj S, Burrows C, Spiker D, Cao B, et al. Deep brain stimulation of the medial forebrain bundle: distinctive responses in resistant depression. J Affect Disord. 2016;203:143–51. doi: 10.1016/j.jad.2016.05.064.. [DOI] [PubMed] [Google Scholar]
- 80.Nuttin B, Cosyns P, Demeulemeester H, Gybels J, Meyerson B. Electrical stimulation in anterior limbs of internal capsules in patients with obsessive-compulsive disorder. Lancet. 1999;354:1526. doi: 10.1016/S0140-6736(99)02376-4.. [DOI] [PubMed] [Google Scholar]
- 81.Greenberg BD, Gabriels LA, Malone DA, Rezai AR, Friehs GM, Okun MS, et al. Deep brain stimulation of the ventral internal capsule/ventral striatum for obsessive-compulsive disorder: worldwide experience. Mol Psychiatry. 2010;15:64–79. doi: 10.1038/mp.2008.55.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gadot R, Najera R, Hirani S, Anand A, Storch E, Goodman WK, et al. Efficacy of deep brain stimulation for treatment-resistant obsessive-compulsive disorder: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2022;93:1166–73. doi: 10.1136/jnnp-2021-328738.. [DOI] [PubMed] [Google Scholar]
- 83.Luyten L, Hendrickx S, Raymaekers S, Gabriëls L, Nuttin B. Electrical stimulation in the bed nucleus of the stria terminalis alleviates severe obsessive-compulsive disorder. Mol Psychiatry. 2016;21:1272–80. doi: 10.1038/mp.2015.124.. [DOI] [PubMed] [Google Scholar]
- 84.Mallet L, Polosan M, Jaafari N, Baup N, Welter M-L, Fontaine D, et al. Subthalamic nucleus stimulation in severe obsessive–compulsive disorder. N. Engl J Med. 2008;359:2121–34. doi: 10.1056/NEJMoa0708514.. [DOI] [PubMed] [Google Scholar]
- 85.Li N, Baldermann JC, Kibleur A, Treu S, Akram H, Elias GJB, et al. A unified connectomic target for deep brain stimulation in obsessive-compulsive disorder. Nat Commun. 2020;11:3364. doi: 10.1038/s41467-020-16734-3.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Baldermann JC, Schüller T, Kohl S, Voon V, Li N, Hollunder B, et al. Connectomic deep brain stimulation for obsessive-compulsive disorder. Biol Psychiatry. 2021;90:678–88. doi: 10.1016/j.biopsych.2021.07.010.. [DOI] [PubMed] [Google Scholar]
- 87.Haber SN, Yendiki A, Jbabdi S. Four deep brain stimulation targets for obsessive-compulsive disorder: are they different? Biol Psychiatry. 2021;90:667–77. doi: 10.1016/j.biopsych.2020.06.031.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wang J, Shang R, He L, Zhou R, Chen Z, Ma Y, et al. Prediction of deep brain stimulation outcome in Parkinson’s disease with connectome based on hemispheric asymmetry. Front Neurosci. 2021;15:620750. doi: 10.3389/fnins.2021.620750.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mirza KB, Golden CT, Nikolic K, Toumazou C. Closed-loop implantable therapeutic neuromodulation systems based on neurochemical monitoring. Front Neurosci. 2019;13:808. doi: 10.3389/fnins.2019.00808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fingelkurts AA, Fingelkurts AA, Rytsälä H, Suominen K, Isometsä E, Kähkönen S. Impaired functional connectivity at EEG alpha and theta frequency bands in major depression. Hum Brain Mapp. 2007;28:247–61. doi: 10.1002/hbm.20275.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Neumann W-J, Huebl J, Brücke C, Gabriëls L, Bajbouj M, Merkl A, et al. Different patterns of local field potentials from limbic DBS targets in patients with major depressive and obsessive compulsive disorder. Mol Psychiatry. 2014;19:1186–92. doi: 10.1038/mp.2014.2.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pollock VE, Schneider LS. Quantitative, waking EEG research on depression. Biol Psychiatry. 1990;27:757–80. doi: 10.1016/0006-3223(90)90591-o.. [DOI] [PubMed] [Google Scholar]
- 93.Kemp AH, Griffiths K, Felmingham KL, Shankman SA, Drinkenburg W, Arns M, et al. Disorder specificity despite comorbidity: resting EEG alpha asymmetry in major depressive disorder and post-traumatic stress disorder. Biol Psychol. 2010;85:350–4. doi: 10.1016/j.biopsycho.2010.08.001.. [DOI] [PubMed] [Google Scholar]
- 94.Scangos KW, Khambhati AN, Daly PM, Makhoul GS, Sugrue LP, Zamanian H, et al. Closed-loop neuromodulation in an individual with treatment-resistant depression. Nat Med. 2021;27:1696–1700. doi: 10.1038/s41591-021-01480-w.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Provenza NR, Sheth SA, Dastin-van Rijn EM, Mathura RK, Ding Y, Vogt GS, et al. Long-term ecological assessment of intracranial electrophysiology synchronized to behavioral markers in obsessive-compulsive disorder. Nat Med. 2021;27:2154–64. doi: 10.1038/s41591-021-01550-z.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Vissani M, Nanda P, Bush A, Neudorfer C, Dougherty D, Richardson RM Toward Closed-Loop Intracranial Neurostimulation in Obsessive-Compulsive Disorder. Biol Psychiatry. 2022. 10.1016/j.biopsych.2022.07.003 [DOI] [PubMed]
- 97.Fridgeirsson EA, Bais MN, Eijsker N, Thomas RM, Smit DJA, Bergfeld IO, et al. Patient specific intracranial neural signatures of obsessions and compulsions in the ventral striatum. J Neural Eng. 2023. 10.1088/1741-2552/acbee1. [DOI] [PubMed]
- 98.Chiken S, Nambu A. Mechanism of deep brain stimulation. Neuroscientist. 2016;22:313–22. doi: 10.1177/1073858415581986.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.McIntyre CC, Savasta M, Kerkerian-Le Goff L, Vitek JL. Uncovering the mechanism(s) of action of deep brain stimulation: activation, inhibition, or both. Clin Neurophysiol. 2004;115:1239–48. doi: 10.1016/j.clinph.2003.12.024.. [DOI] [PubMed] [Google Scholar]
- 100.Ashkan K, Rogers P, Bergman H, Ughratdar I. Insights into the mechanisms of deep brain stimulation. Nat Rev Neurol. 2017;13:548–54. doi: 10.1038/nrneurol.2017.105.. [DOI] [PubMed] [Google Scholar]
- 101.Lozano AM, Lipsman N, Bergman H, Brown P, Chabardes S, Chang JW, et al. Deep brain stimulation: current challenges and future directions. Nat Rev Neurol. 2019;15:148–60. doi: 10.1038/s41582-018-0128-2.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sun FT, Morrell MJ. The RNS system: responsive cortical stimulation for the treatment of refractory partial epilepsy. Expert Rev Med Devices. 2014;11:563–72. doi: 10.1586/17434440.2014.947274.. [DOI] [PubMed] [Google Scholar]
- 103.Stanslaski S, Herron J, Chouinard T, Bourget D, Isaacson B, Kremen V, et al. A chronically implantable neural coprocessor for investigating the treatment of neurological disorders. IEEE Trans Biomed Circuits Syst. 2018;12:1230–45. doi: 10.1109/TBCAS.2018.2880148.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Waltz E. Green light for deep brain stimulator incorporating neurofeedback. Nat Biotechnol. 2020;38:1014–5. doi: 10.1038/s41587-020-0664-3.. [DOI] [PubMed] [Google Scholar]
- 105.Jimenez-Shahed J. Device profile of the percept PC deep brain stimulation system for the treatment of Parkinson’s disease and related disorders. Expert Rev Med Devices. 2021;18:319–32. doi: 10.1080/17434440.2021.1909471.. [DOI] [PubMed] [Google Scholar]
- 106.Arlotti M, Colombo M, Bonfanti A, Mandat T, Lanotte MM, Pirola E, et al. A new implantable closed-loop clinical neural interface: first application in Parkinson’s disease. Front Neurosci. 2021;15:763235. doi: 10.3389/fnins.2021.763235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ansó J, Benjaber M, Parks B, Parker S, Oehrn CR, Petrucci M, et al. Concurrent stimulation and sensing in bi-directional brain interfaces: a multi-site translational experience. J Neural Eng. 2022;19:026025. doi: 10.1088/1741-2552/ac59a3.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cameron T, Alo KM. Effects of posture on stimulation parameters in spinal cord stimulation. Neuromodulation: Technol Neural Interface. 1998;1:177–83. doi: 10.1111/j.1525-1403.1998.tb00014.x.. [DOI] [PubMed] [Google Scholar]
- 109.Schultz DM, Webster L, Kosek P, Dar U, Tan Y, Sun M. Sensor-driven position-adaptive spinal cord stimulation for chronic pain. Pain Physician. 2012;15:1–12. doi: 10.36076/ppj.2012/15/1. [DOI] [PubMed] [Google Scholar]
- 110.Mekhail N, Levy RM, Deer TR, Kapural L, Li S, Amirdelfan K, et al. Long-term safety and efficacy of closed-loop spinal cord stimulation to treat chronic back and leg pain (Evoke): a double-blind, randomised, controlled trial. Lancet Neurol. 2020;19:123–34. doi: 10.1016/S1474-4422(19)30414-4.. [DOI] [PubMed] [Google Scholar]
- 111.Mekhail N, Levy RM, Deer TR, Kapural L, Li S, Amirdelfan K, et al. Durability of clinical and quality-of-life outcomes of closed-loop spinal cord stimulation for chronic back and leg pain: a secondary analysis of the evoke randomized clinical trial. JAMA Neurol. 2022;79:251–60. doi: 10.1001/jamaneurol.2021.4998.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Shirvalkar P, Prosky J, Chin G, Ahmadipour P, Sani OG, Desai M, et al. First-in-human prediction of chronic pain state using intracranial neural biomarkers. Nat Neurosci. 2023:1–10. 10.1038/s41593-023-01338-z [DOI] [PMC free article] [PubMed]
- 113.Little S, Pogosyan A, Neal S, Zavala B, Zrinzo L, Hariz M, et al. Adaptive deep brain stimulation in advanced Parkinson disease. Ann Neurol. 2013;74:449–57. doi: 10.1002/ana.23951.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Rosa M, Arlotti M, Ardolino G, Cogiamanian F, Marceglia S, Di Fonzo A, et al. Adaptive deep brain stimulation in a freely moving parkinsonian patient. Mov Disord. 2015;30:1003–5. doi: 10.1002/mds.26241.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Little S, Beudel M, Zrinzo L, Foltynie T, Limousin P, Hariz M, et al. Bilateral adaptive deep brain stimulation is effective in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2016;87:717–21. doi: 10.1136/jnnp-2015-310972.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Little S, Tripoliti E, Beudel M, Pogosyan A, Cagnan H, Herz D, et al. Adaptive deep brain stimulation for Parkinson’s disease demonstrates reduced speech side effects compared to conventional stimulation in the acute setting. J Neurol Neurosurg Psychiatry. 2016;87:1388–9. doi: 10.1136/jnnp-2016-313518.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Piña-Fuentes D, Little S, Oterdoom M, Neal S, Pogosyan A, Tijssen MAJ, et al. Adaptive DBS in a Parkinson’s patient with chronically implanted DBS: a proof of principle. Mov Disord. 2017;32:1253–4. doi: 10.1002/mds.26959.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bocci T, Prenassi M, Arlotti M, Cogiamanian FM, Borellini L, Moro E, et al. Eight-hours conventional versus adaptive deep brain stimulation of the subthalamic nucleus in Parkinson’s disease. npj Parkinsons Dis. 2021;7:1–6. doi: 10.1038/s41531-021-00229-z.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Arlotti M, Marceglia S, Foffani G, Volkmann J, Lozano AM, Moro E, et al. Eight-hours adaptive deep brain stimulation in patients with Parkinson disease. Neurology. 2018;90:e971–e976. doi: 10.1212/WNL.0000000000005121.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Velisar A, Syrkin-Nikolau J, Blumenfeld Z, Trager MH, Afzal MF, Prabhakar V, et al. Dual threshold neural closed loop deep brain stimulation in Parkinson disease patients. Brain Stimulation: Basic Transl Clin Res Neuromodulation. 2019;12:868–76. doi: 10.1016/j.brs.2019.02.020.. [DOI] [PubMed] [Google Scholar]
- 121.Malekmohammadi M, Herron J, Velisar A, Blumenfeld Z, Trager MH, Chizeck HJ, et al. Kinematic adaptive deep brain stimulation for resting tremor in Parkinson’s disease. Mov Disord. 2016;31:426–8. doi: 10.1002/mds.26482.. [DOI] [PubMed] [Google Scholar]
- 122.Swann NC, de Hemptinne C, Thompson MC, Miocinovic S, Miller AM, Gilron R, et al. Adaptive deep brain stimulation for Parkinson’s disease using motor cortex sensing. J Neural Eng. 2018;15:046006. doi: 10.1088/1741-2552/aabc9b.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Gilron R, Little S, Perrone R, Wilt R, de Hemptinne C, Yaroshinsky MS, et al. Long-term wireless streaming of neural recordings for circuit discovery and adaptive stimulation in individuals with Parkinson’s disease. Nat Biotechnol. 2021;39:1078–85. doi: 10.1038/s41587-021-00897-5.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Graupe D, Basu I, Tuninetti D, Vannemreddy P, Slavin KV. Adaptively controlling deep brain stimulation in essential tremor patient via surface electromyography. Neurol Res. 2010;32:899–904. doi: 10.1179/016164110X12767786356354.. [DOI] [PubMed] [Google Scholar]
- 125.Yamamoto T, Katayama Y, Ushiba J, Yoshino H, Obuchi T, Kobayashi K, et al. On-demand control system for deep brain stimulation for treatment of intention tremor. Neuromodulation: Technol Neural Interface. 2013;16:230–5. doi: 10.1111/j.1525-1403.2012.00521.x.. [DOI] [PubMed] [Google Scholar]
- 126.Cagnan H, Pedrosa D, Little S, Pogosyan A, Cheeran B, Aziz T, et al. Stimulating at the right time: phase-specific deep brain stimulation. Brain. 2017;140:132–45. doi: 10.1093/brain/aww286.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Opri E, Cernera S, Molina R, Eisinger RS, Cagle JN, Almeida L, et al. Chronic embedded cortico-thalamic closed-loop deep brain stimulation for the treatment of essential tremor. Sci Transl Med. 2020;12:eaay7680. doi: 10.1126/scitranslmed.aay7680.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lesser RP, Kim SH, Beyderman L, Miglioretti DL, Webber WRS, Bare M, et al. Brief bursts of pulse stimulation terminate afterdischarges caused by cortical stimulation. Neurology. 1999;53:2073–2073. doi: 10.1212/WNL.53.9.2073.. [DOI] [PubMed] [Google Scholar]
- 129.Valentin A, Ughratdar I, Venkatachalam G, Williams R, Pina M, Lazaro M, et al. Sustained seizure control in a child with drug resistant epilepsy after subacute cortical electrical stimulation (SCES) Brain Stimul. 2016;9:307–9. doi: 10.1016/j.brs.2015.12.004.. [DOI] [PubMed] [Google Scholar]
- 130.Peters TE, Bhavaraju NC, Frei MG, Osorio I. Network system for automated seizure detection and contingent delivery of therapy. J Clin Neurophysiol. 2001;18:545–9. doi: 10.1097/00004691-200111000-00004.. [DOI] [PubMed] [Google Scholar]
- 131.Kossoff EH, Ritzl EK, Politsky JM, Murro AM, Smith JR, Duckrow RB, et al. Effect of an external responsive neurostimulator on seizures and electrographic discharges during subdural electrode monitoring. Epilepsia. 2004;45:1560–7. doi: 10.1111/j.0013-9580.2004.26104.x.. [DOI] [PubMed] [Google Scholar]
- 132.Morrell MJ. Responsive cortical stimulation for the treatment of medically intractable partial epilepsy. Neurology. 2011;77:1295–304. doi: 10.1212/WNL.0b013e3182302056.. [DOI] [PubMed] [Google Scholar]
- 133.Heck CN, King-Stephens D, Massey AD, Nair DR, Jobst BC, Barkley GL, et al. Two-year seizure reduction in adults with medically intractable partial onset epilepsy treated with responsive neurostimulation: final results of the RNS System Pivotal trial. Epilepsia. 2014;55:432–41. doi: 10.1111/epi.12534.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bergey GK, Morrell MJ, Mizrahi EM, Goldman A, King-Stephens D, Nair D, et al. Long-term treatment with responsive brain stimulation in adults with refractory partial seizures. Neurology. 2015;84:810–7. doi: 10.1212/WNL.0000000000001280.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Razavi B, Rao VR, Lin C, Bujarski KA, Patra SE, Burdette DE, et al. Real-world experience with direct brain-responsive neurostimulation for focal onset seizures. Epilepsia. 2020;61:1749–57. doi: 10.1111/epi.16593.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Nair DR, Laxer KD, Weber PB, Murro AM, Park YD, Barkley GL, et al. Nine-year prospective efficacy and safety of brain-responsive neurostimulation for focal epilepsy. Neurology. 2020;95:e1244–e1256. doi: 10.1212/WNL.0000000000010154.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.van Elmpt WJC, Nijsen TME, Griep PAM, Arends JBAM. A model of heart rate changes to detect seizures in severe epilepsy. Seizure. 2006;15:366–75. doi: 10.1016/j.seizure.2006.03.005.. [DOI] [PubMed] [Google Scholar]
- 138.Fisher RS, Afra P, Macken M, Minecan DN, Bagić A, Benbadis SR, et al. Automatic vagus nerve stimulation triggered by ictal tachycardia: clinical outcomes and device performance—The U.S. E-37 trial. Neuromodulation. 2016;19:188–95. doi: 10.1111/ner.12376.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Datta P, Galla KM, Sajja K, Wichman C, Wang H, Madhavan D. Vagus nerve stimulation with tachycardia detection provides additional seizure reduction compared to traditional vagus nerve stimulation. Epilepsy Behav. 2020;111:107280. doi: 10.1016/j.yebeh.2020.107280.. [DOI] [PubMed] [Google Scholar]
- 140.Hamilton P, Soryal I, Dhahri P, Wimalachandra W, Leat A, Hughes D, et al. Clinical outcomes of VNS therapy with AspireSR® (including cardiac-based seizure detection) at a large complex epilepsy and surgery centre. Seizure. 2018;58:120–6. doi: 10.1016/j.seizure.2018.03.022.. [DOI] [PubMed] [Google Scholar]
- 141.Winston GM, Guadix S, Lavieri MT, Uribe-Cardenas R, Kocharian G, Williams N, et al. Closed-loop vagal nerve stimulation for intractable epilepsy: a single-center experience. Seizure - Eur J Epilepsy. 2021;88:95–101. doi: 10.1016/j.seizure.2021.03.030.. [DOI] [PubMed] [Google Scholar]
- 142.Jankovic J, Kurlan R. Tourette syndrome: evolving concepts. Mov Disord. 2011;26:1149–56. doi: 10.1002/mds.23618.. [DOI] [PubMed] [Google Scholar]
- 143.Molina R, Okun MS, Shute JB, Opri E, Rossi PJ, Martinez-Ramirez D, et al. Report of a patient undergoing chronic responsive deep brain stimulation for Tourette syndrome: proof of concept. J Neurosurg. 2018;129:308–14. doi: 10.3171/2017.6.JNS17626.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Cagle JN, Okun MS, Cernera S, Eisinger RS, Opri E, Bowers D, et al. Embedded human closed-loop deep brain stimulation for tourette syndrome: a nonrandomized controlled trial. JAMA Neurol. 2022;79:1064–8. doi: 10.1001/jamaneurol.2022.2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Faller J, Doose J, Sun X, Mclntosh JR, Saber GT, Lin Y, et al. Daily prefrontal closed-loop repetitive transcranial magnetic stimulation (rTMS) produces progressive EEG quasi-alpha phase entrainment in depressed adults. Brain Stimulation. 2022;15:458–71. doi: 10.1016/j.brs.2022.02.008.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Scangos KW, Makhoul GS, Sugrue LP, Chang EF, Krystal AD. State-dependent responses to intracranial brain stimulation in a patient with depression. Nat Med. 2021;27:229–31. doi: 10.1038/s41591-020-01175-8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Allawala A, Bijanki KR, Goodman W, Cohn JF, Viswanathan A, Yoshor D, et al. A novel framework for network-targeted neuropsychiatric deep brain stimulation. Neurosurgery. 2021. 10.1093/neuros/nyab112. [DOI] [PMC free article] [PubMed]
- 148.Sheth SA, Bijanki KR, Metzger B, Allawala A, Pirtle V, Adkinson JA, et al. Deep brain stimulation for depression informed by intracranial recordings. Biol Psychiatry. 2022;92:246–51. doi: 10.1016/j.biopsych.2021.11.007.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Widge AS, Ellard KK, Paulk AC, Basu I, Yousefi A, Zorowitz S, et al. Treating refractory mental illness with closed-loop brain stimulation: progress towards a patient-specific transdiagnostic approach. Exp Neurol. 2017;287:461–72. doi: 10.1016/j.expneurol.2016.07.021.. [DOI] [PubMed] [Google Scholar]
- 150.Basu I, Yousefi A, Crocker B, Zelmann R, Paulk AC, Peled N, et al. Closed-loop enhancement and neural decoding of cognitive control in humans. Nat Biomed Eng. 2023;7:576–88. doi: 10.1038/s41551-021-00804-y.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Sani OG, Yang Y, Lee MB, Dawes HE, Chang EF, Shanechi MM. Mood variations decoded from multi-site intracranial human brain activity. Nat Biotechnol. 2018;36:954–61. doi: 10.1038/nbt.4200.. [DOI] [PubMed] [Google Scholar]
- 152.Sani OG, Abbaspourazad H, Wong YT, Pesaran B, Shanechi MM. Modeling behaviorally relevant neural dynamics enabled by preferential subspace identification. Nat Neurosci. 2021;24:140–9. doi: 10.1038/s41593-020-00733-0.. [DOI] [PubMed] [Google Scholar]
- 153.Yuxiao Y, Chang EF, Shanechi MM. Dynamic tracking of non-stationarity in human ECoG activity. Annu Int Conf IEEE Eng Med Biol Soc. 2017;2017:1660–3. doi: 10.1109/EMBC.2017.8037159.. [DOI] [PubMed] [Google Scholar]
- 154.Proix T, Truccolo W, Leguia MG, Tcheng TK, King-Stephens D, Rao VR, et al. Forecasting seizure risk in adults with focal epilepsy: a development and validation study. Lancet Neurol. 2021;20:127–35. doi: 10.1016/S1474-4422(20)30396-3.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Baud MO, Kleen JK, Mirro EA, Andrechak JC, King-Stephens D, Chang EF, et al. Multi-day rhythms modulate seizure risk in epilepsy. Nat Commun. 2018;9:88. doi: 10.1038/s41467-017-02577-y.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Beninger RJ, Milner PM. Conditioned reinforcement based on reinforcing electrical stimulation of the brain: chain schedules. Psychobiology. 1977;5:285–9. doi: 10.3758/BF03335332.. [DOI] [Google Scholar]
- 157.Khambhati AN, Shafi A, Rao VR, Chang EF. Long-term brain network reorganization predicts responsive neurostimulation outcomes for focal epilepsy. Sci Transl Med. 2021;13:eabf6588. doi: 10.1126/scitranslmed.abf6588.. [DOI] [PubMed] [Google Scholar]
- 158.Huang Y, Hajnal B, Entz L, Fabó D, Herrero JL, Mehta AD, et al. Intracortical dynamics underlying repetitive stimulation predicts changes in network connectivity. J Neurosci. 2019;39:6122–35. doi: 10.1523/JNEUROSCI.0535-19.2019.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Khambhati AN, Kahn AE, Costantini J, Ezzyat Y, Solomon EA, Gross RE, et al. Functional control of electrophysiological network architecture using direct neurostimulation in humans. Netw Neurosci. 2019;3:848–77. doi: 10.1162/netn_a_00089.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Widge AS, Deckersbach T, Eskandar EN, Dougherty DD. Deep brain stimulation for treatment-resistant psychiatric illnesses: what has gone wrong and what should we do next. Biol Psychiatry. 2016;79:e9–e10. doi: 10.1016/j.biopsych.2015.06.005.. [DOI] [PubMed] [Google Scholar]
- 161.Bagby RM, Ryder AG, Schuller DR, Marshall MB. The hamilton depression rating scale: has the gold standard become a lead weight? AJP. 2004;161:2163–77. doi: 10.1176/appi.ajp.161.12.2163.. [DOI] [PubMed] [Google Scholar]
- 162.Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–9. doi: 10.1192/bjp.134.4.382.. [DOI] [PubMed] [Google Scholar]
- 163.Davidson J, Turnbull CD, Strickland R, Miller R, Graves K. The Montgomery-Åsberg depression scale: reliability and validity. Acta Psychiatr Scandinavica. 1986;73:544–8. doi: 10.1111/j.1600-0447.1986.tb02723.x.. [DOI] [PubMed] [Google Scholar]
- 164.Cuijpers P, Li J, Hofmann SG, Andersson G. Self-reported versus clinician-rated symptoms of depression as outcome measures in psychotherapy research on depression: a meta-analysis. Clin Psychol Rev. 2010;30:768–78. doi: 10.1016/j.cpr.2010.06.001.. [DOI] [PubMed] [Google Scholar]
- 165.Rush AJ, Carmody TJ, Ibrahim HM, Trivedi MH, Biggs MM, Shores-Wilson K, et al. Comparison of self-report and clinician ratings on two inventories of depressive symptomatology. PS. 2006;57:829–37. doi: 10.1176/ps.2006.57.6.829.. [DOI] [PubMed] [Google Scholar]
- 166.Iannuzzo RW, Jaeger J, Goldberg JF, Kafantaris V, Sublette ME. Development and reliability of the HAM-D/MADRS interview: an integrated depression symptom rating scale. Psychiatry Res. 2006;145:21–37. doi: 10.1016/j.psychres.2005.10.009.. [DOI] [PubMed] [Google Scholar]
- 167.van Westen M, Rietveld E, Bergfeld IO, de Koning P, Vullink N, Ooms P, et al. Optimizing deep brain stimulation parameters in obsessive–compulsive disorder. Neuromodulation. 2021;24:307–15. doi: 10.1111/ner.13243.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ramasubbu R, Lang S, Kiss ZHT. Dosing of electrical parameters in deep brain stimulation (DBS) for intractable depression: a review of clinical studies. Front Psychiatry. 2018;9:302. doi: 10.3389/fpsyt.2018.00302.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Boutet A, Madhavan R, Elias GJB, Joel SE, Gramer R, Ranjan M, et al. Predicting optimal deep brain stimulation parameters for Parkinson’s disease using functional MRI and machine learning. Nat Commun. 2021;12:3043. doi: 10.1038/s41467-021-23311-9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Malekmohammadi M, Mustakos R, Sheth S, Pouratian N, McIntyre CC, Bijanki KR, et al. Automated optimization of deep brain stimulation parameters for modulating neuroimaging-based targets. J Neural Eng. 2022;19:046014. doi: 10.1088/1741-2552/ac7e6c.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Butson CR, Noecker AM, Maks CB, McIntyre CC (2007) StimExplorer: deep brain stimulation parameter selection software system. In: Sakas DE, Simpson BA (eds) Operative Neuromodulation: Volume 2: Neural Networks Surgery. Springer, Vienna, pp 569–74. [DOI] [PubMed]
- 172.Widge AS, Bilge MT, Montana R, Chang W, Rodriguez CI, Deckersbach T, et al. Electroencephalographic biomarkers for treatment response prediction in major depressive illness: a meta-analysis. Am J Psychiatry. 2019;176:44–56. doi: 10.1176/appi.ajp.2018.17121358.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.van der Vinne N, Vollebregt MA, van Putten MJAM, Arns M. Stability of frontal alpha asymmetry in depressed patients during antidepressant treatment. Neuroimage Clin. 2019;24:102056. doi: 10.1016/j.nicl.2019.102056.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Vuga M, Fox NA, Cohn JF, George CJ, Levenstein RM, Kovacs M. Long-term stability of frontal electroencephalographic asymmetry in adults with a history of depression and controls. Int J Psychophysiol. 2006;59:107–15. doi: 10.1016/j.ijpsycho.2005.02.008.. [DOI] [PubMed] [Google Scholar]
- 175.Tenke CE, Kayser J, Alvarenga JE, Abraham KS, Warner V, Talati A, et al. Temporal stability of posterior EEG alpha over twelve years. Clin Neurophysiol. 2018;129:1410–7. doi: 10.1016/j.clinph.2018.03.037.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Trotti R, Parker D, McDowell JE, Pearlson G, Keshavan M, Keedy S, et al. Longitudinal stability of psychosis biomarkers: findings from the bipolar-schizophrenia network for intermediate phenotypes (B-SNIP) Biol Psychiatry. 2021;89:S124. doi: 10.1016/j.biopsych.2021.02.321.. [DOI] [Google Scholar]
- 177.Sellers KK, Stapper N, Astudillo Maya DA, Henderson C, Khambhati AN, Fan JM, et al. Changes in intracranial neurophysiology associated with acute COVID-19 infection. Clin Neurophysiol. 2023;148:29–31. doi: 10.1016/j.clinph.2023.01.012.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Katerndahl D, Ferrer R, Best R, Wang C-P. Dynamic patterns in mood among newly diagnosed patients with major depressive episode or panic disorder and normal controls. Prim Care Companion J Clin Psychiatry. 2007;9:183–7. doi: 10.4088/PCC.v09n0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Bosley HG, Soyster PD, Fisher AJ. Affect dynamics as predictors of symptom severity and treatment response in mood and anxiety disorders: evidence for specificity. J Pers Oriented Res. 2019;5:101–13. doi: 10.17505/jpor.2019.09.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Hosenfeld B, Bos EH, Wardenaar KJ, Conradi HJ, van der Maas HLJ, Visser I, et al. Major depressive disorder as a nonlinear dynamic system: bimodality in the frequency distribution of depressive symptoms over time. BMC Psychiatry. 2015;15:222. doi: 10.1186/s12888-015-0596-5.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Young MA, Fogg LF, Scheftner WA, Fawcett JA. Concordance of symptoms in recurrent depressive episodes. J Affect Disord. 1990;20:79–85. doi: 10.1016/0165-327(90)90120-w.. [DOI] [PubMed] [Google Scholar]
- 182.Roberts RE, Lewinsohn PM, Seeley JR. Symptoms of DSM-III-R major depression in adolescence: evidence from an epidemiological survey. J Am Acad Child Adolesc Psychiatry. 1995;34:1608–17. doi: 10.1097/00004583-199512000-00011.. [DOI] [PubMed] [Google Scholar]
- 183.Chai LR, Khambhati AN, Ciric R, Moore TM, Gur RC, Gur RE, et al. Evolution of brain network dynamics in neurodevelopment. Netw Neurosci. 2017;1:14–30. doi: 10.1162/NETN_a_00001.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Betzel RF, Byrge L, He Y, Goñi J, Zuo X-N, Sporns O. Changes in structural and functional connectivity among resting-state networks across the human lifespan. Neuroimage. 2014;102:345–57. doi: 10.1016/j.neuroimage.2014.07.067. [DOI] [PubMed] [Google Scholar]
- 185.Betzel RF, Satterthwaite TD, Gold JI, Bassett DS. Positive affect, surprise, and fatigue are correlates of network flexibility. Sci Rep. 2017;7:520. doi: 10.1038/s41598-017-00425-z.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Mirchi N, Betzel RF, Bernhardt BC, Dagher A, Mišic B. Tracking mood fluctuations with functional network patterns. Soc Cogn Affect Neurosci. 2019;14:47–57. doi: 10.1093/scan/nsy107.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Fan JM, Khambhati AN, Sellers KK, Stapper N, Maya DA, Kunwar E, et al. (2023) Epileptiform discharges triggered with direct electrical stimulation for treatment-resistant depression: Factors that modulate risk and treatment considerations. Brain Stimulation: Basic, Translational, and Clinical Research in Neuromodulation 0: 10.1016/j.brs.2023.02.006. [DOI] [PMC free article] [PubMed]
- 188.Rao VR, Sellers KK, Wallace DL, Lee MB, Bijanzadeh M, Sani OG, et al. Direct electrical stimulation of lateral orbitofrontal cortex acutely improves mood in individuals with symptoms of depression. Curr Biol. 2018;28:3893–3902.e4. doi: 10.1016/j.cub.2018.10.026.. [DOI] [PubMed] [Google Scholar]
- 189.Keller CJ, Huang Y, Herrero JL, Fini ME, Du V, Lado FA, et al. Induction and quantification of excitability changes in human cortical networks. J Neurosci. 2018;38:5384–98. doi: 10.1523/JNEUROSCI.1088-17.2018.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Chiang S, Khambhati AN, Wang ET, Vannucci M, Chang EF, Rao VR. Evidence of state-dependence in the effectiveness of responsive neurostimulation for seizure modulation. Brain Stimul. 2021;14:366–75. doi: 10.1016/j.brs.2021.01.023.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Mohan UR, Watrous AJ, Miller JF, Lega BC, Sperling MR, Worrell GA, et al. The effects of direct brain stimulation in humans depend on frequency, amplitude, and white-matter proximity. Brain Stimul. 2020;13:1183–95. doi: 10.1016/j.brs.2020.05.009.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Patel DM, Walker HC, Brooks R, Omar N, Ditty B, Guthrie BL. Adverse events associated with deep brain stimulation for movement disorders analysis of 510 consecutive cases. Operative Neurosurg. 2015;11:190–9. doi: 10.1227/neu.0000000000000659.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Feldmann LK, Neumann W-J, Faust K, Schneider G-H, Kühn AA. Risk of infection after deep brain stimulation surgery with externalization and local-field potential recordings: twelve-year experience from a single institution. Stereotact Funct Neurosurg. 2021;99:512–20. doi: 10.1159/000516150.. [DOI] [PubMed] [Google Scholar]
- 194.Vergani F, Landi A, Pirillo D, Cilia R, Antonini A, Sganzerla EP. Surgical, medical, and hardware adverse events in a series of 141 patients undergoing subthalamic deep brain stimulation for Parkinson Disease. World Neurosurg. 2010;73:338–44. doi: 10.1016/j.wneu.2010.01.017.. [DOI] [PubMed] [Google Scholar]
- 195.Buhmann C, Huckhagel T, Engel K, Gulberti A, Hidding U, Poetter-Nerger M, et al. Adverse events in deep brain stimulation: a retrospective long-term analysis of neurological, psychiatric and other occurrences. PLoS ONE. 2017;12:e0178984. doi: 10.1371/journal.pone.0178984.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Dang J, King KM, Inzlicht M. Why are self-report and behavioral measures weakly correlated? Trends Cogn Sci. 2020;24:267–9. doi: 10.1016/j.tics.2020.01.007.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Ertugrul IO, Jeni LA, Ding W, Cohn JF. AFAR: A Deep Learning Based Tool for Automated Facial Affect Recognition. In: 2019 14th IEEE International Conference on Automatic Face & Gesture Recognition (FG 2019). pp 1–1. 2019. [DOI] [PMC free article] [PubMed]
- 198.Cohn JF, Okun MS, Jeni LA, Ertugrul IO, Borton D, Malone D, et al. Automated affect detection in deep brain stimulation for obsessive-compulsive disorder: a pilot study. Proc ACM Int Conf Multimodal Interact. 2018;2018:40–44. doi: 10.1145/3242969.3243023.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Hachem LD, Wong SM, Ibrahim GM. The vagus afferent network: emerging role in translational connectomics. Neurosurg Focus. 2018;45:E2. doi: 10.3171/2018.6.FOCUS18216.. [DOI] [PubMed] [Google Scholar]
- 200.FDA Premarket Approval (PMA): VNS Therapy System. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P970003. Accessed 11 Feb 2023.