Abstract
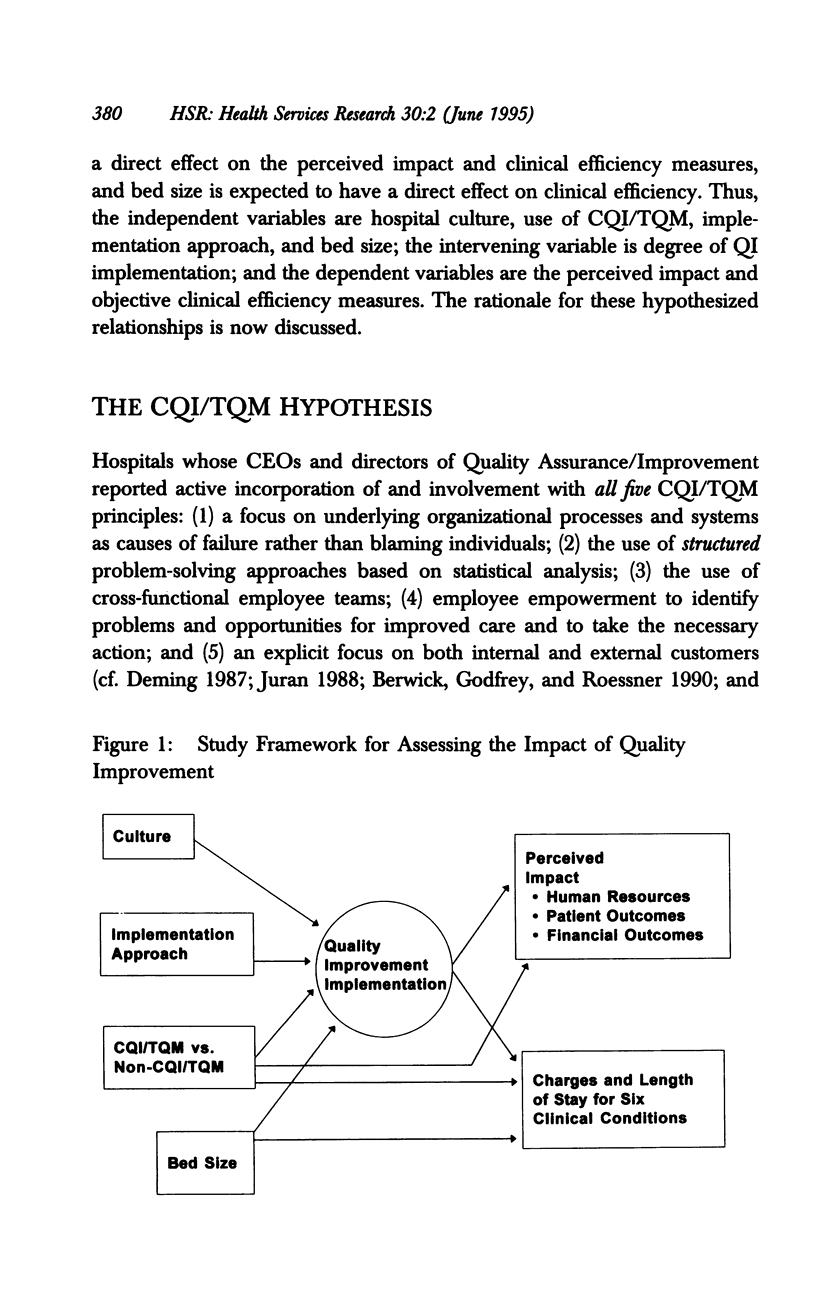
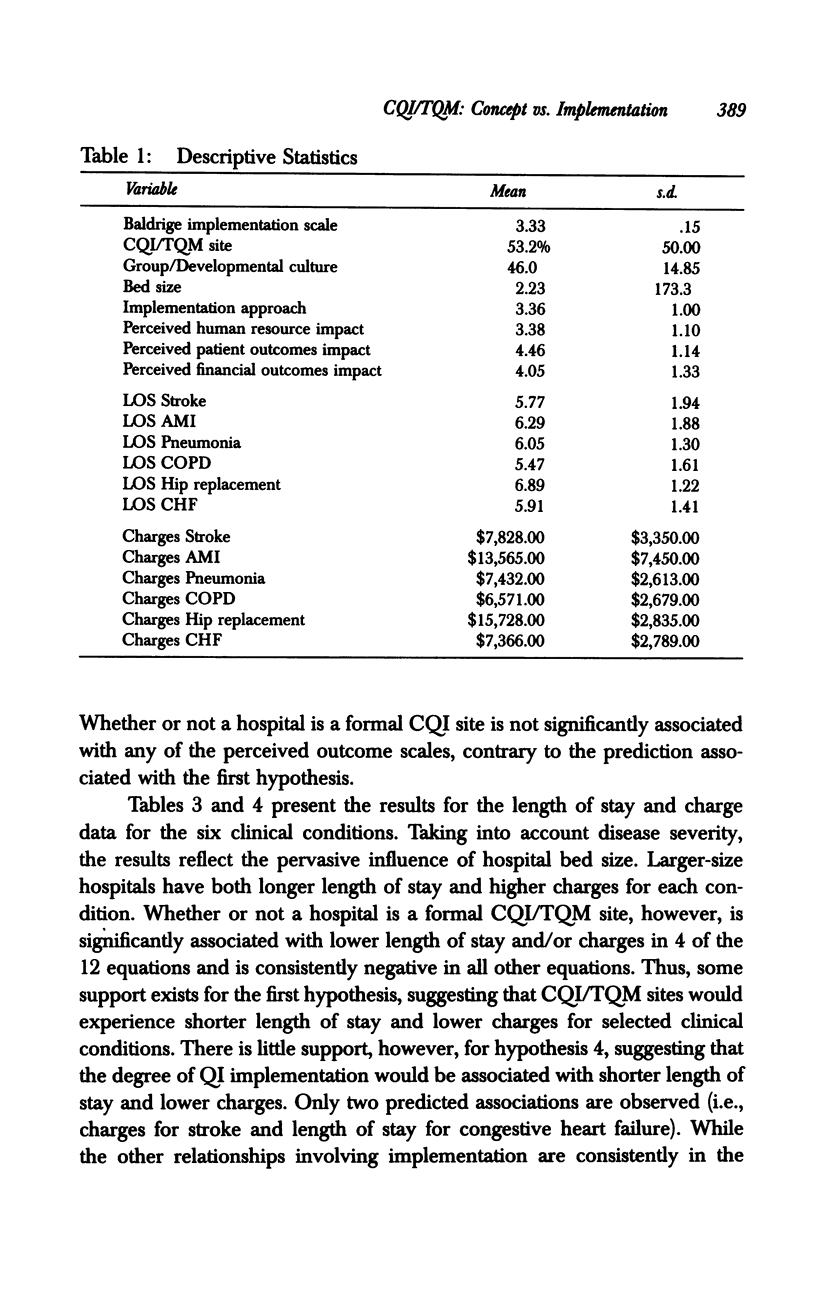
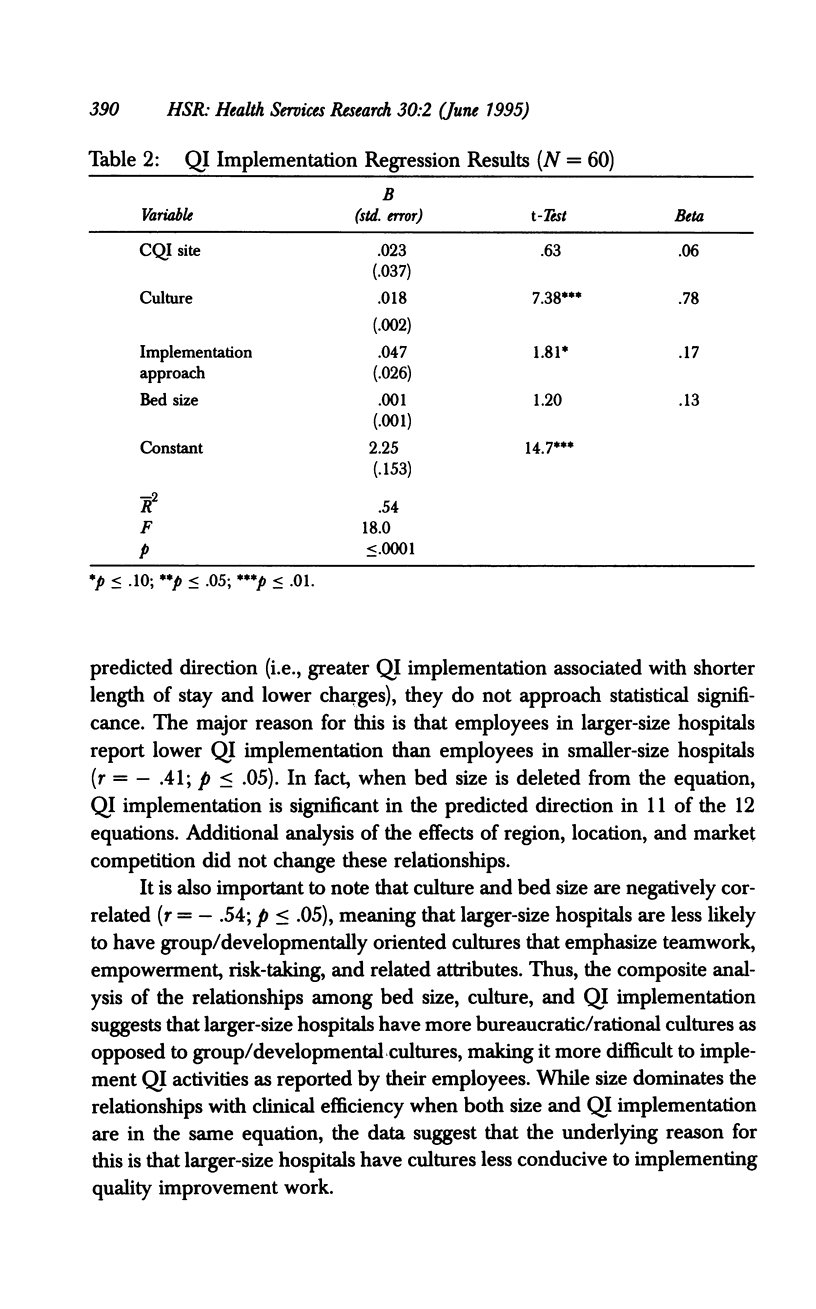
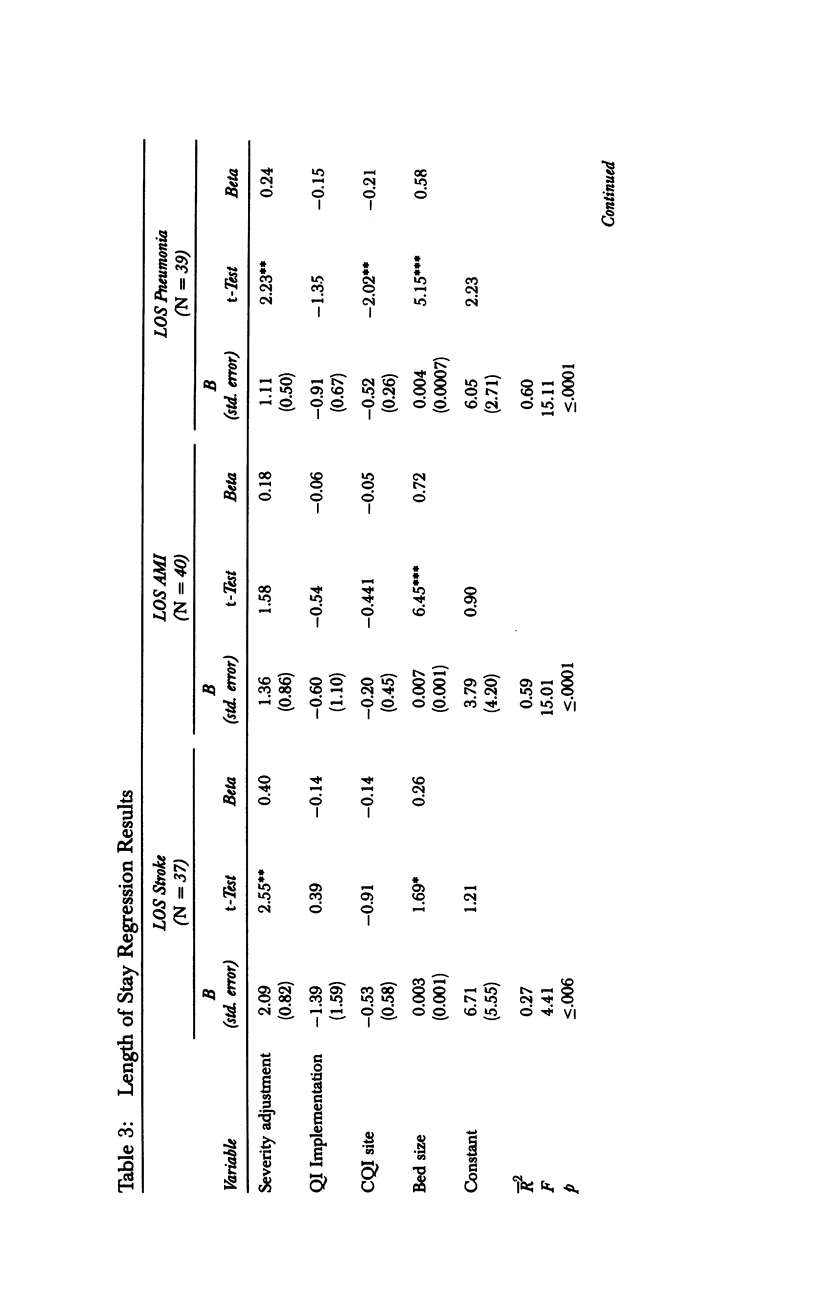
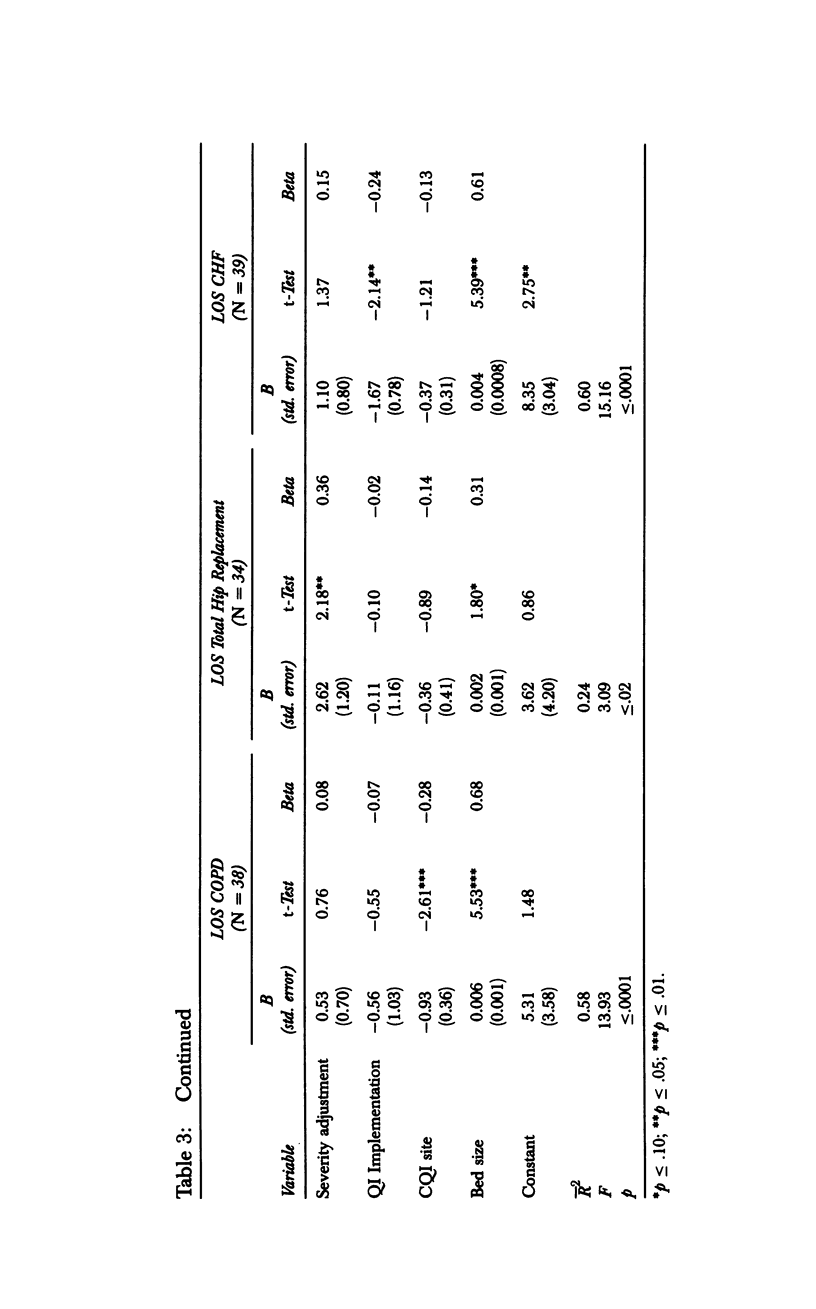
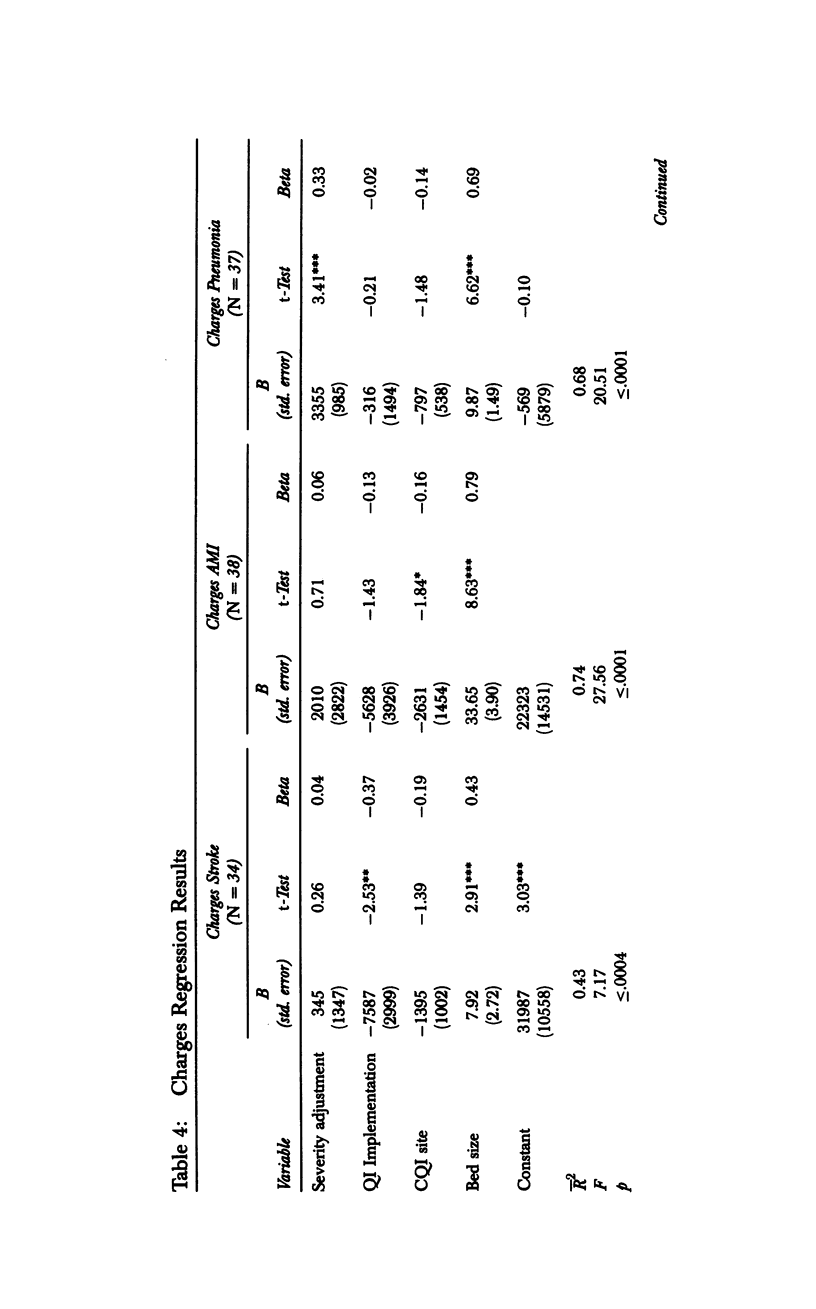
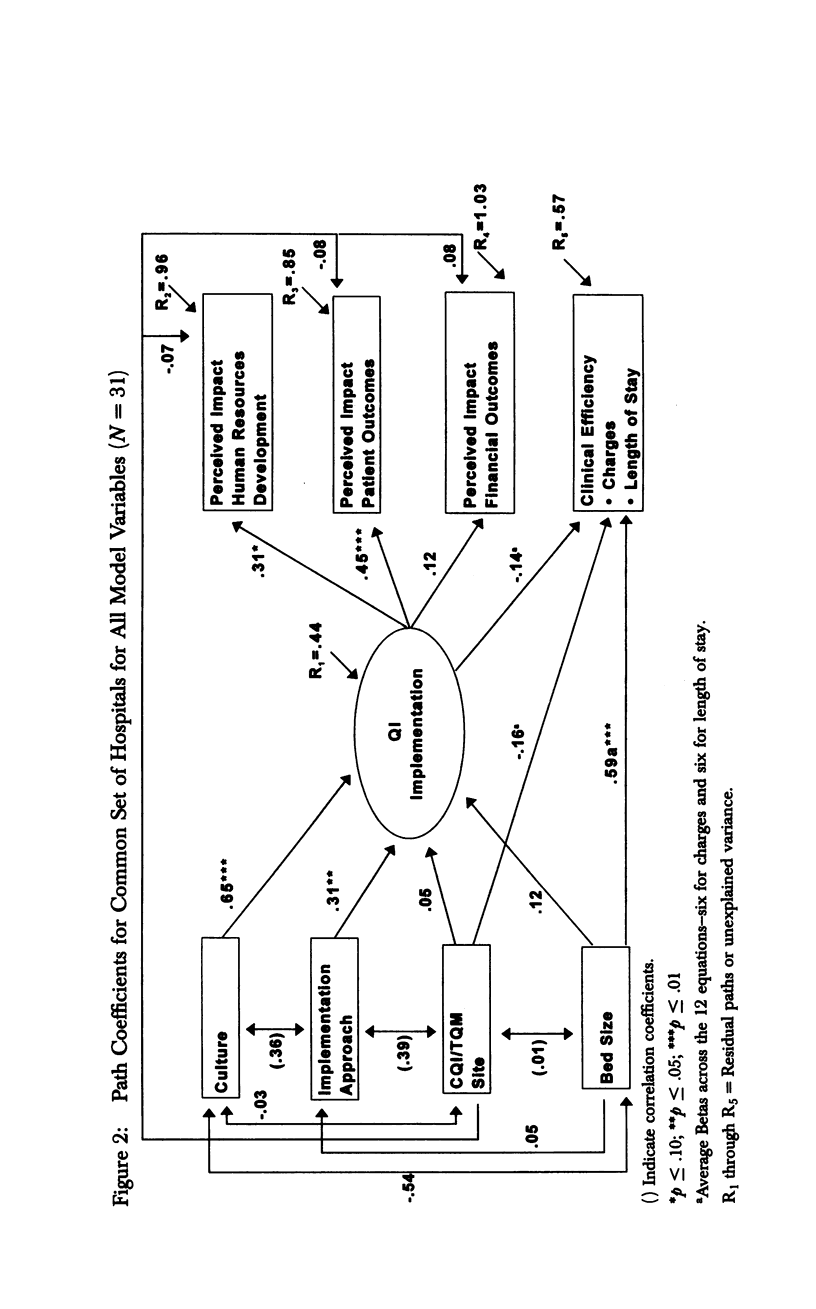
OBJECTIVE: This study examines the relationships among organizational culture, quality improvement processes and selected outcomes for a sample of up to 61 U. S. hospitals. DATA SOURCES AND STUDY SETTING: Primary data were collected from 61 U. S. hospitals (located primarily in the midwest and the west) on measures related to continuous quality improvement/total quality management (CQI/TQM), organizational culture, implementation approaches, and degree of quality improvement implementation based on the Baldrige Award criteria. These data were combined with independently collected data on perceived impact and objective measures of clinical efficiency (i.e., charges and length of stay) for six clinical conditions. STUDY DESIGN: The study involved cross-sectional examination of the named relationships. DATA COLLECTION/EXTRACTION METHODS: Reliable and valid scales for the organizational culture and quality improvement implementation measures were developed based on responses from over 7,000 individuals across the 61 hospitals with an overall completion rate of 72 percent. Independent data on perceived impact were collected from a national survey and independent data on clinical efficiency from a companion study of managed care. PRINCIPAL FINDINGS: A participative, flexible, risk-taking organizational culture was significantly related to quality improvement implementation. Quality improvement implementation, in turn, was positively associated with greater perceived patient outcomes and human resource development. Larger-size hospitals experienced lower clinical efficiency with regard to higher charges and higher length of stay, due in part to having more bureaucratic and hierarchical cultures that serve as a barrier to quality improvement implementation. CONCLUSIONS: What really matters is whether or not a hospital has a culture that supports quality improvement work and an approach that encourages flexible implementation. Larger-size hospitals face more difficult challenges in this regard.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Batalden P., Smith S. D., Bovender J. O., Hardison C. D. Quality improvement: the role and application of research methods. J Health Adm Educ. 1989 Summer;7(3):577–583. [PubMed] [Google Scholar]
- Berwick D. M. Continuous improvement as an ideal in health care. N Engl J Med. 1989 Jan 5;320(1):53–56. doi: 10.1056/NEJM198901053200110. [DOI] [PubMed] [Google Scholar]
- Counte M. A., Glandon G. L., Oleske D. M., Hill J. P. Total quality management in a health care organization: how are employees affected? Hosp Health Serv Adm. 1992 Winter;37(4):503–518. [PubMed] [Google Scholar]
- Kaluzny A. D., McLaughlin C. P., Jaeger B. J. TQM as a managerial innovation: research issues and implications. Health Serv Manage Res. 1993 May;6(2):78–88. doi: 10.1177/095148489300600202. [DOI] [PubMed] [Google Scholar]
- Kaluzny A. D., McLaughlin C. P., Kibbe D. C. Continuous quality improvement in the clinical setting: enhancing adoption. Qual Manag Health Care. 1992 Fall;1(1):37–44. [PubMed] [Google Scholar]
- Kaluzny A. D., McLaughlin C. P. Managing transitions: assuring the adoption and impact of TQM. QRB Qual Rev Bull. 1992 Nov;18(11):380–384. doi: 10.1016/s0097-5990(16)30559-0. [DOI] [PubMed] [Google Scholar]
- Laffel G., Blumenthal D. The case for using industrial quality management science in health care organizations. JAMA. 1989 Nov 24;262(20):2869–2873. [PubMed] [Google Scholar]
- McLaughlin C. P., Kaluzny A. D. Total quality management in health: making it work. Health Care Manage Rev. 1990 Summer;15(3):7–14. doi: 10.1097/00004010-199001530-00002. [DOI] [PubMed] [Google Scholar]
- Sahney V. K., Warden G. L. The quest for quality and productivity in health services. Front Health Serv Manage. 1991 Summer;7(4):2–56. [PubMed] [Google Scholar]
- Shortell S. M., Levin D. Z., O'Brien J. L., Hughes E. F. Assessing the evidence on CQI: is the glass half empty or half full? Hosp Health Serv Adm. 1995 Spring;40(1):4–24. [PubMed] [Google Scholar]
- Shortell S. M., Zimmerman J. E., Rousseau D. M., Gillies R. R., Wagner D. P., Draper E. A., Knaus W. A., Duffy J. The performance of intensive care units: does good management make a difference? Med Care. 1994 May;32(5):508–525. doi: 10.1097/00005650-199405000-00009. [DOI] [PubMed] [Google Scholar]
- Wakefield D. S., Wakefield B. J. Overcoming the barriers to implementation of TQM/CQI in hospitals: myths and realities. QRB Qual Rev Bull. 1993 Mar;19(3):83–88. doi: 10.1016/s0097-5990(16)30597-8. [DOI] [PubMed] [Google Scholar]
- Ware J. E., Jr, Sherbourne C. D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473–483. [PubMed] [Google Scholar]


