Abstract
Superficial temporal artery pseudoaneurysms are an uncommon vascular pathology that can present after head or facial trauma. Furthermore, they are rarely reported in the pediatric population. Ultrasound can be a useful tool in the diagnosis because it is easily accessible and can be rapidly acquired. We report a case that demonstrates the utility of ultrasound in the diagnosis of a superficial temporal artery pseudoaneurysm.
Keywords: Pediatric vascular surgery, Temporal artery pseudoaneurysm
A pseudoaneurysm due to blunt trauma is a commonly described entity in vascular surgery. However, these are usually seen in larger vessels, such as an iliac or femoral artery. Traumatic superficial temporal artery (STA) pseudoaneurysm is a rare injury that has only been described in case reports or small case series and is even rarer in the pediatric population.1,2 Patients typically present with a painless and pulsatile mass in the temple. The diagnosis is aided by ultrasound or computed tomography angiography. Regardless, STA pseudoaneurysms are often misdiagnosed as cysts or abscesses.3, 4, 5, 6, 7 In the present report, we describe a pediatric case of a STA pseudoaneurysm. The patient's parents provided written informed consent for the report of his case details and imaging studies.
Case report
A 4-year-old boy presented to the emergency department (ED) with a persistent head lesion of his left temporal area after a fall that had occurred 2 weeks prior. At the time of his fall, he had a laceration in the area with bleeding, but the patient did not present to the hospital at that time. After developing induration and swelling to the site, the parents brought the child to the ED. The patient and his parents denied any fevers, chills, erythema, or pain. He had no contributory medical, surgical, or family history. On presentation to the ED, the patient was described as having a 1-cm fluctuant mass of his left anterior temporal region without erythema or warmth (Fig 1), and no pulsatility of the lesion was documented. Concern was expressed for a retained foreign body, seroma, or abscess. An incision and drainage procedure was performed by the ED physicians, and the patient experienced bright red pulsatile bleeding, which was controlled with sutures. At this time, no imaging studies were obtained. The patient was referred to pediatric surgery and was seen 2 weeks later for evaluation of the mass with concern for a pseudoaneurysm. An immediate diagnostic ultrasound of the head and neck showed a partially thrombosed left temporal artery pseudoaneurysm with Doppler flow measuring 11.0 × 7.0 × 9.0 mm (Figs 2 and 3). The patient’s case was discussed with vascular surgery at this time, and the patient was scheduled for surgery the following day. The patient underwent general anesthesia, and surgical excision of the pseudoaneurysm and ligation of the left temporal artery was performed by vascular and pediatric surgery. An ultrasound scan was used preoperatively to identify the artery proximally and distally to the pseudoaneurysm. An elliptical incision was made at the left temporal region overlying the pseudoaneurysm, and dissection was carried down to the pseudoaneurysm. This allowed for easy identification of the proximal and distal ends of the STA pseudoaneurysm, which were subsequently ligated. The pseudoaneurysm was then excised. The patient tolerated the procedure well and was discharged the same day in stable condition. He had no complications on follow-up.
Fig 1.
Left temporal artery pseudoaneurysm after emergency department (ED) incision and drainage.
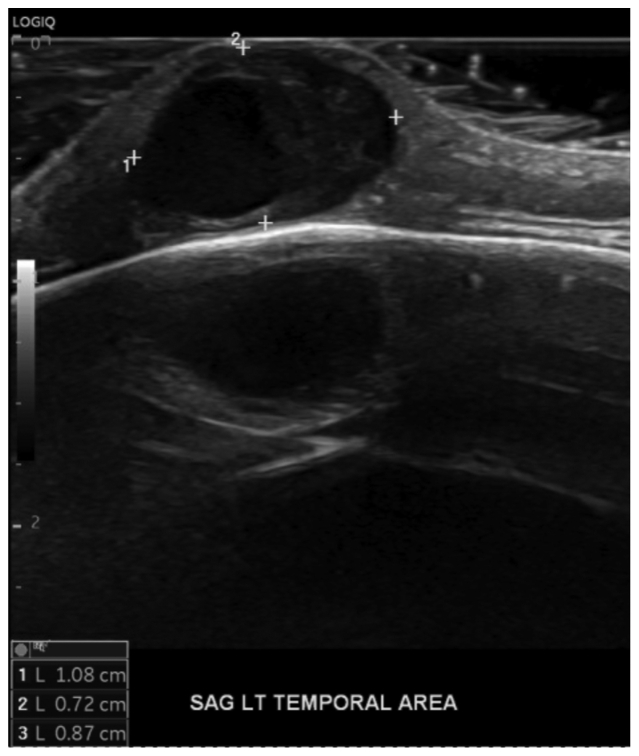
Fig 2.
Sagittal B-mode image of pseudoaneurysm with measurements. LT, Left; SAG, sagittal.
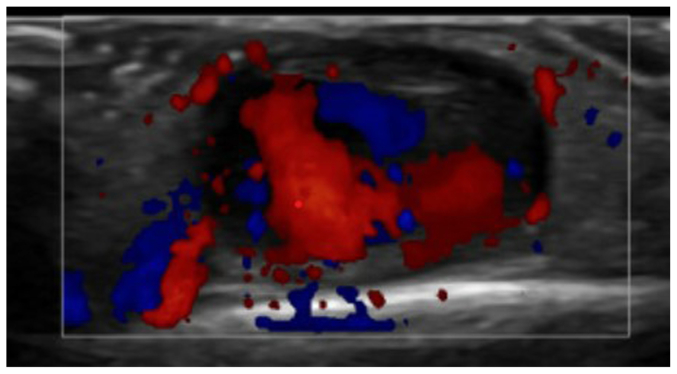
Fig 3.
Color Doppler image of pseudoaneurysm showing flow with partial thrombosis.
Discussion
Pediatric STA pseudoaneurysms are uncommon and rarely described in the literature.1,4,6, 7, 8, 9 Clinicians often fail to consider STA pseudoaneurysms in their differential diagnosis because of its low incidence and other more commonly occurring lesions such as abscesses, lipomas, cysts, hematomas, and enlarged lymph nodes.1,2,7 Other diagnoses such as neuromas, arteriovenous fistulas, Langerhans cell histiocytosis occur but are not as common.7 This can delay proper treatment and lead to unnecessary procedures being performed on children.
The STA is especially susceptible to developing a pseudoaneurysm after a traumatic event because of its superficial location.8 Surgical excision of the pseudoaneurysm and ligation of the temporal artery is the gold standard for treatment.5 A thorough physical examination and high clinical suspicion are crucial for an accurate diagnosis, and persistent post-traumatic temporal masses that are pulsatile and have low clinical suspicion for an infectious etiology should raise concern for a possible STA pseudoaneurysm. Duplex ultrasound can aid in the diagnosis but is rarely performed in the ED for patients presenting with small masses and no other concerning symptoms. Evaluation with duplex ultrasound is recommended in these cases, especially in the pediatric population to avoid exposure to radiation, to accurately diagnose and treat patients in a timely manner.7,9 The current literature on the diagnosis, management, and treatment of an STA pseudoaneurysm is limited and mainly reported in non–vascular surgery journals.4,7, 8, 9 Clinicians could be unaware of vascular surgery's role in the treatment of pediatric patients and, if a STA pseudoaneurysm is encountered, can be considered for consultation, if available. It is also important to keep STA pseudoaneurysms within the differential diagnosis, especially if trauma to the site has occurred. All physicians should remember that the use of ultrasound is advantageous in the diagnosis.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Davis F.M., Eliason J.L., Ganesh S.K., Blatt N.B., Stanley J.C., Coleman D.M. Pediatric nonaortic arterial aneurysms. J Vasc Surg. 2016;63:466–476.e1. doi: 10.1016/j.jvs.2015.08.099. [DOI] [PubMed] [Google Scholar]
- 2.Sarkar R., Coran A.G., Cilley R.E., Lindenauer S.M., Stanley J.C. Arterial aneurysms in children: clinicopathologic classification. J Vasc Surg. 1991;13:47–56. discussion: 56-47. [PubMed] [Google Scholar]
- 3.Namin A., Starnes S.E., Plikaitis C.M. Pediatric craniofacial pseudoaneurysm with a variable history of antecedent trauma. J Craniofac Surg. 2015;26:796–799. doi: 10.1097/SCS.0000000000001425. [DOI] [PubMed] [Google Scholar]
- 4.Quereshy F.A., Choi S., Buma B. Traumatic pseudoaneurysm of the superficial temporal artery in a pediatric patient: a case report. J Oral Maxillofac Surg. 2008;66:133–135. doi: 10.1016/j.joms.2006.05.071. [DOI] [PubMed] [Google Scholar]
- 5.Ruiz-Medina P.E., Narvaez K., Abdul-Hadi A. Post-traumatic true superficial temporal artery aneurysm in a pediatric patient. Am Surg. 2022;88:1317–1318. doi: 10.1177/0003134820942150. [DOI] [PubMed] [Google Scholar]
- 6.Hasegawa H., Tsutsumi S., Yasumoto Y., Inaba T., Ito M. Traumatic pseudoaneurysm arising from the anterior superficial temporal artery in an infant. Childs Nerv Syst. 2011;27:1011–1014. doi: 10.1007/s00381-010-1384-7. [DOI] [PubMed] [Google Scholar]
- 7.Leeman M., Leus A., Ernst C. Post-traumatic pseudoaneurysm of the superficial temporal artery in a pediatric patient. J Belg Soc Radiol. 2023;107:2. doi: 10.5334/jbsr.3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahn H.S., Cho B.M., Oh S.M., Park S.H. Traumatic pseudoaneurysm of the superficial temporal artery in a child: a case report. Childs Nerv Syst. 2010;26:117–120. doi: 10.1007/s00381-009-0953-0. [DOI] [PubMed] [Google Scholar]
- 9.Naija S., Maamouri S., Jameleddine E., et al. Post-traumatic pseudoaneurysm of the superficial temporal artery in a child. J Pediatr Surg Case Rep. 2021;74 [Google Scholar]