Abstract
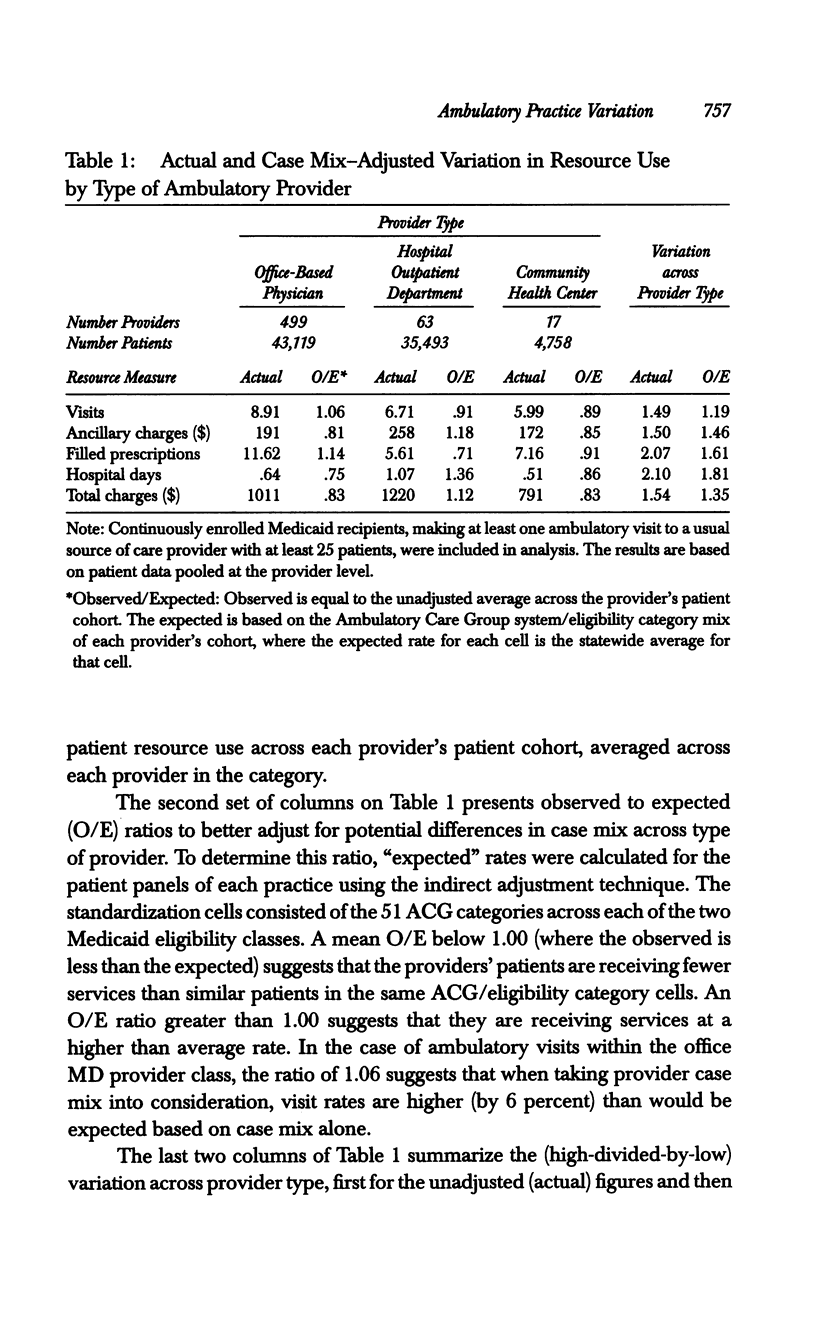
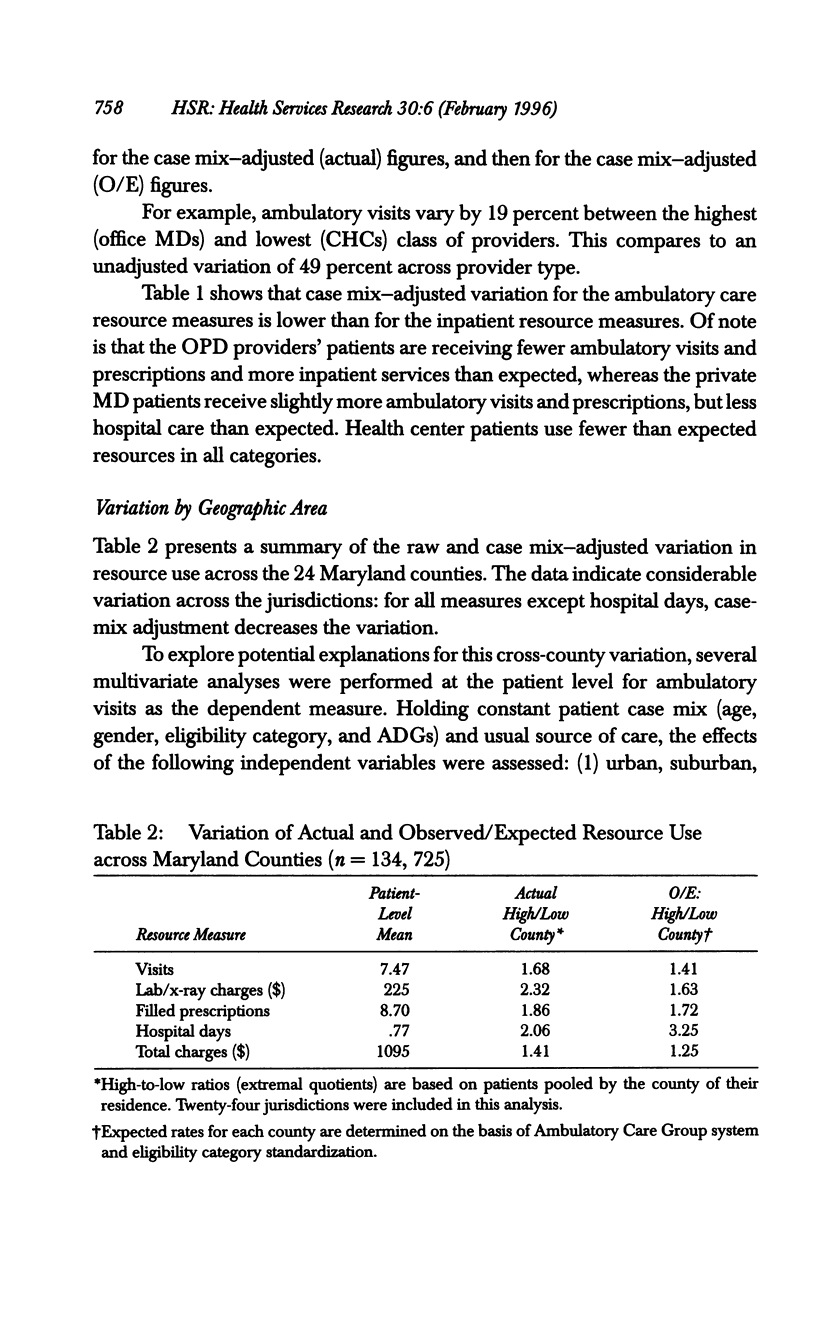
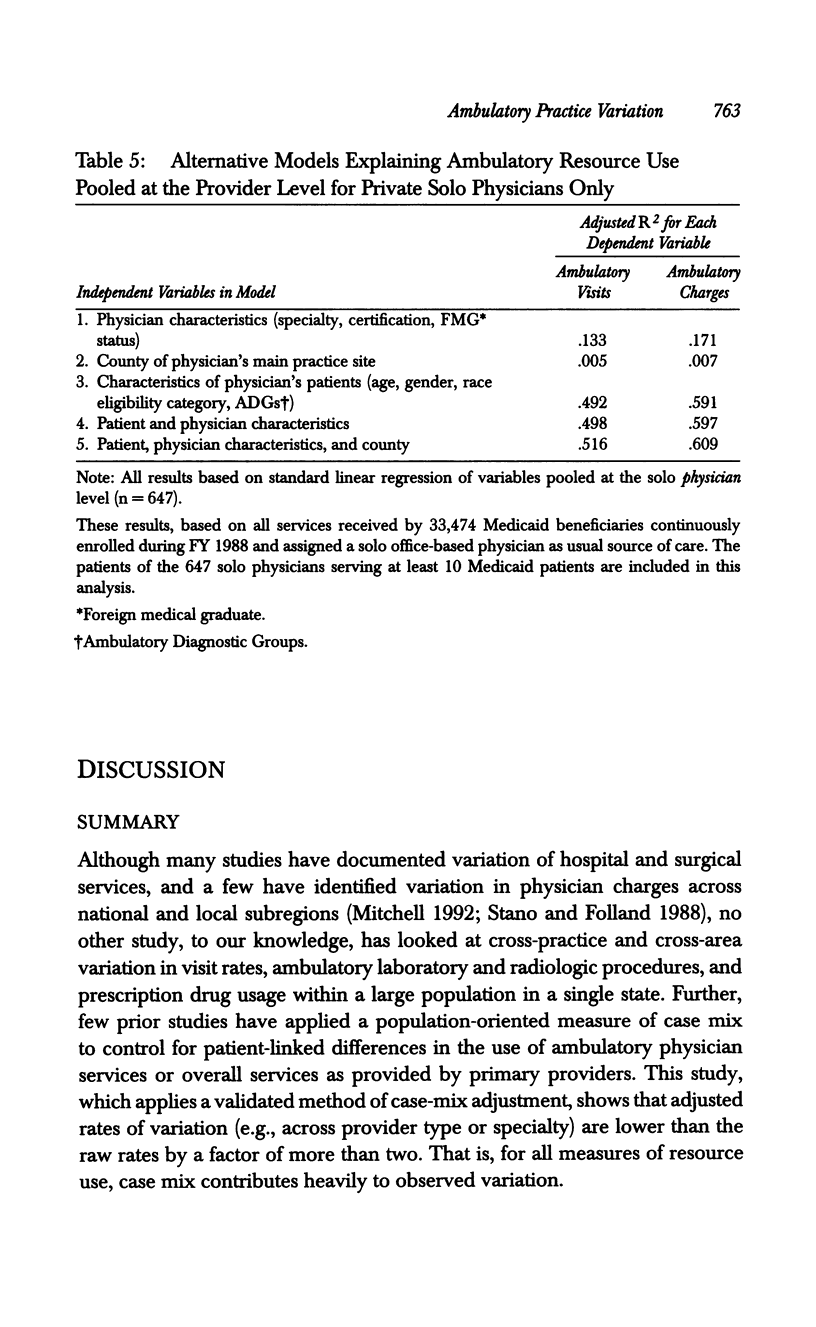
STUDY QUESTIONS: What is the extent of variation in patterns of ambulatory care practice across one state's Medicaid program once case mix is controlled for? How much of this variation in resource consumption is explained by factors linked to the provider, patient, and geographic subarea? DATA SOURCES/STUDY SETTING: Practices of all providers delivering care to persons who were continuously enrolled in the Maryland Medicaid program during FY 1988 were studied. A computerized summary of all services received during this year for 134,725 persons was developed using claims data. We also obtained data from the state's beneficiary and provider files and the American Medical Association's masterfile. Each patient was assigned a "usual source of care" (primary provider) based on the actual patterns of service. The Ambulatory Care Group (ACG) measure was used to help control for case mix. STUDY DESIGN: This was a cross-sectional study based on the universe of continuously enrolled Medicaid enrollees in one state. PRINCIPAL FINDINGS: After controlling for case mix, the variation in patient resource use by type of primary provider was 19 percent for ambulatory visits, 46 percent for ancillary testing, 61 percent for prescriptions, and 81 percent for hospitalizations. Across Maryland counties, comparing the low- to high-use jurisdiction, there was 41 percent variation in case mix-adjusted visit rates, 72 percent variation in pharmacy use, and 325 percent variation in hospital days. At the individual practice level, physician characteristics explain up to 17 percent of ambulatory resource use and geographic area explains only a few percent, while patient characteristics explain up to 60 percent of variation. CONCLUSIONS: Since a large proportion of variation was explained by patient case mix, it is evident that risk adjustment is essential for these types of analyses. However, even after adjustment, resource use varies considerably across types of ambulatory care provider and region, with consequent implications for efficiency of health services delivery.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cherkin D. C., Rosenblatt R. A., Hart L. G., Schneeweiss R., LoGerfo J. The use of medical resources by residency-trained family physicians and general internists. Is there a difference? Med Care. 1987 Jun;25(6):455–469. doi: 10.1097/00005650-198706000-00001. [DOI] [PubMed] [Google Scholar]
- Diehr P., Cain K., Connell F., Volinn E. What is too much variation? The null hypothesis in small-area analysis. Health Serv Res. 1990 Feb;24(6):741–771. [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn A., Powe N. R. Small area variations in health care delivery in Maryland. Health Serv Res. 1995 Jun;30(2):295–317. [PMC free article] [PubMed] [Google Scholar]
- Greenfield S., Nelson E. C., Zubkoff M., Manning W., Rogers W., Kravitz R. L., Keller A., Tarlov A. R., Ware J. E., Jr Variations in resource utilization among medical specialties and systems of care. Results from the medical outcomes study. JAMA. 1992 Mar 25;267(12):1624–1630. [PubMed] [Google Scholar]
- Greenwald H. P., Peterson M. L., Garrison L. P., Hart L. G., Moscovice I. S., Hall T. L., Perrin E. B. Interspecialty variation in office-based care. Med Care. 1984 Jan;22(1):14–29. doi: 10.1097/00005650-198401000-00002. [DOI] [PubMed] [Google Scholar]
- Hartley R. M., Charlton J. R., Harris C. M., Jarman B. Patterns of physicians' use of medical resources in ambulatory settings. Am J Public Health. 1987 May;77(5):565–567. doi: 10.2105/ajph.77.5.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasper J. D. The importance of type of usual source of care for children's physician access and expenditures. Med Care. 1987 May;25(5):386–398. doi: 10.1097/00005650-198705000-00003. [DOI] [PubMed] [Google Scholar]
- Kelman H. R., Thomas C. Hospital and ambulatory service use by the urban elderly under different health care delivery systems. Med Care. 1988 Aug;26(8):739–749. doi: 10.1097/00005650-198808000-00001. [DOI] [PubMed] [Google Scholar]
- Kravitz R. L., Greenfield S., Rogers W., Manning W. G., Jr, Zubkoff M., Nelson E. C., Tarlov A. R., Ware J. E., Jr Differences in the mix of patients among medical specialties and systems of care. Results from the medical outcomes study. JAMA. 1992 Mar 25;267(12):1617–1623. [PubMed] [Google Scholar]
- McDevitt R. D., Dutton B. Expenditures for ambulatory episodes of care: the Michigan Medicaid experience. Health Care Financ Rev. 1989 Winter;11(2):43–55. [PMC free article] [PubMed] [Google Scholar]
- McPherson K., Wennberg J. E., Hovind O. B., Clifford P. Small-area variations in the use of common surgical procedures: an international comparison of New England, England, and Norway. N Engl J Med. 1982 Nov 18;307(21):1310–1314. doi: 10.1056/NEJM198211183072104. [DOI] [PubMed] [Google Scholar]
- Mitchell J. B. Area variation in Medicare physician spending. Health Aff (Millwood) 1992 Spring;11(1):224–234. doi: 10.1377/hlthaff.11.1.224. [DOI] [PubMed] [Google Scholar]
- Paul-Shaheen P., Clark J. D., Williams D. Small area analysis: a review and analysis of the North American literature. J Health Polit Policy Law. 1987 Winter;12(4):741–809. doi: 10.1215/03616878-12-4-741. [DOI] [PubMed] [Google Scholar]
- Roos N. P., Roos L. L. High and low surgical rates: risk factors for area residents. Am J Public Health. 1981 Jun;71(6):591–600. doi: 10.2105/ajph.71.6.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stano M., Folland S. Variations in the use of physician services by Medicare beneficiaries. Health Care Financ Rev. 1988 Spring;9(3):51–58. [PMC free article] [PubMed] [Google Scholar]
- Starfield B., Powe N. R., Weiner J. R., Stuart M., Steinwachs D., Scholle S. H., Gerstenberger A. Costs vs quality in different types of primary care settings. JAMA. 1994 Dec 28;272(24):1903–1908. [PubMed] [Google Scholar]
- Starfield B., Weiner J., Mumford L., Steinwachs D. Ambulatory care groups: a categorization of diagnoses for research and management. Health Serv Res. 1991 Apr;26(1):53–74. [PMC free article] [PubMed] [Google Scholar]
- Stuart M. E., Steinwachs D. M. Patient-mix differences among ambulatory providers and their effects on utilization and payments for Maryland Medicaid users. Med Care. 1993 Dec;31(12):1119–1137. doi: 10.1097/00005650-199312000-00005. [DOI] [PubMed] [Google Scholar]
- Stuart M., Steinwachs D., Harlow J., Fox M. Ambulatory practice variation in Maryland: implications for Medicaid cost management. Health Care Financ Rev. 1990 Dec;Spec No:57–67. [PMC free article] [PubMed] [Google Scholar]
- Weiner J. P., Starfield B. H., Steinwachs D. M., Mumford L. M. Development and application of a population-oriented measure of ambulatory care case-mix. Med Care. 1991 May;29(5):452–472. doi: 10.1097/00005650-199105000-00006. [DOI] [PubMed] [Google Scholar]
- Welch W. P., Miller M. E., Welch H. G., Fisher E. S., Wennberg J. E. Geographic variation in expenditures for physicians' services in the United States. N Engl J Med. 1993 Mar 4;328(9):621–627. doi: 10.1056/NEJM199303043280906. [DOI] [PubMed] [Google Scholar]
- Wennberg J., Gittelsohn Small area variations in health care delivery. Science. 1973 Dec 14;182(4117):1102–1108. doi: 10.1126/science.182.4117.1102. [DOI] [PubMed] [Google Scholar]


