Summary
Background
Despite remarkable progress in maternal and neonatal health, regional inequalities persist in Peru. In rural areas of Amazonian Loreto, access to quality care is difficult, home births are frequent, and neonatal mortality is high. We conducted a prospective before-and-after study to assess the effect after implementation and over time of a community-based intervention on essential newborn care (ENC).
Methods
Mamás del Río consists of tablet-enhanced educational home visits by Community health workers (CHW) to pregnant women and mothers of newborns, with supportive training on ENC of traditional birth attendants and facility staff. The study area comprised 79 rural communities of three districts in Loreto. Primary outcomes were ENC practices in home births, secondary outcomes were ENC in facility births as well as healthcare seeking, measured at baseline before and at year 2 and year 3 after intervention implementation. Community censuses included questionnaires to women aged 15–49 years with a live birth. We calculated prevalence of outcomes at each time point and estimated adjusted prevalence differences (PD) between time points using post-estimation based on logistic regression.
Findings
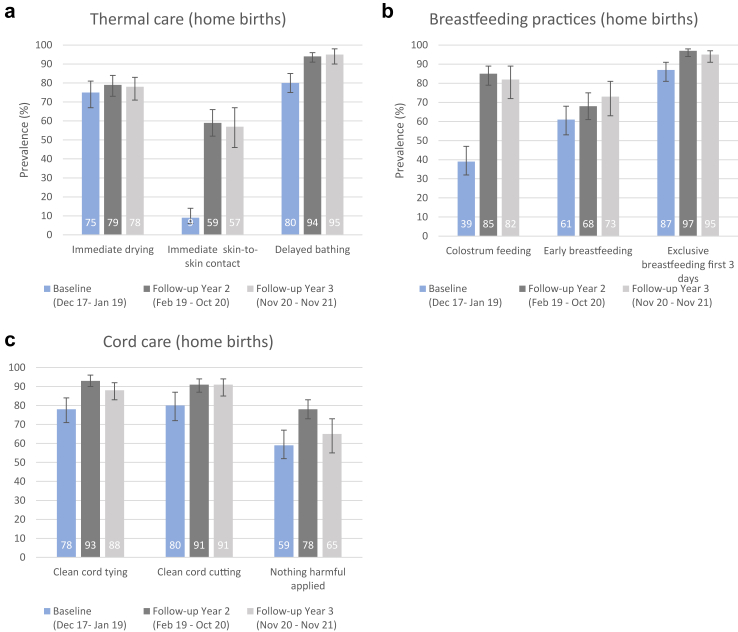
Following implementation early 2019, 97% of communities had a trained CHW. At year 2 follow-up, 63% (322/530) of women received a CHW visit during pregnancy. Seven out of nine ENC indicators among home births improved, with largest adjusted prevalence differences in immediate skin-to-skin contact (50% [95% CI: 42–58], p < 0.0001), colostrum feeding (45% [35–54], p < 0.0001), and cord care (19% [10–28], p = 0.0001). Improvements were maintained at year 3, except for cord care. At year 2, among facility births only three ENC indicators improved, while more women gave birth in a facility. Sensitivity analyses showed ENC prevalence was similar before compared to after onset of Covid-19 lockdown.
Interpretation
ENC practices in home births improved consistently and changes were sustained over time, despite the onset of the Covid-19 pandemic. A community-based approach for behaviour-change in home-based newborn care appears effective. Process evaluation of mechanisms will help to explain observed effects and understand transferability of findings.
Funding
Grand Challenges Canada and Peruvian National Council of Science and Technology.
Keywords: Maternal-neonatal health, Essential newborn care, Community-based intervention, Evaluation, Peru, Indigenous, Amazon
Research in context.
Evidence before this study
Regional health inequalities persist despite national improvements in Peru. In Loreto, located in the Amazon rainforest, neonatal mortality remains high. Hygienic conditions are poor and infections are a leading cause of death in indigenous communities. Most women give birth at home due to difficult geographic access and low quality of care, further exacerbated by the Covid-19 pandemic. Prevalence of essential newborn care (ENC) practices is low, despite being cost-effective, easy to implement, and directly linked to improved survival. Evidence from other countries suggests that community-based interventions can be effective at improving ENC and reducing neonatal mortality. While Peru has a large network of volunteer Community health workers (CHW), our comprehensive literature review covering Embase, Medline, ScieLO, and BVS Peru (see Supplementary Materials 2) suggests that rigorous evaluations are scarce and impact of community-based interventions on maternal-neonatal health outcomes remains unknown.
Added value of this study
This is the first study to rigorously document implementation characteristics and to evaluate the impact of a community-based intervention on ENC and other maternal-neonatal health outcomes in Peru. Responding to the unmet need in an underserved and hard-to-reach indigenous population, we developed Mamás del Río, an intervention covering training of CHW and Traditional birth attendants (TBA), combined with supportive facility strengthening to promote ENC practices and healthcare utilization. We assessed the effect after implementation and changes in effect over time, provided easily interpretable effect sizes adjusted for confounding, and conducted sensitivity analyses to assess the impact of Covid-19 and the unprecedented lockdown on outcomes.
Implications of all the available evidence
We found substantial and consistent improvements across all ENC practices for home births which were maintained over time, suggesting that a community-based approach for behaviour-change in newborn care at home appears effective. While ENC practices at health facilities saw fewer improvements, facility births and newborn check-ups saw small but meaningful increases, despite disruptions by the pandemic. Our findings should encourage Peruvian policy makers to incorporate community-based approaches as part of their maternal-neonatal health strategy in similar settings. Our experience reinforces the importance of community-based approaches as an integral part of the health system, given that CHW and TBAs largely resumed their activities while facility-based care was severely disrupted during the first months of the pandemic. Upcoming process evaluation will help to explain observed changes, understand generalizability to other settings, and generate valuable insights for Peruvian CHW policy.
Introduction
As the world was gripped by the Covid-19 pandemic, child mortality remained unacceptably high. In 2020, 5 million children under the age of five died, half of whom were newborns.1 Peru, a middle-income country of rich geographical, geological, and cultural diversity, has already achieved the Sustainable Development Goals target of reducing neonatal mortality to under 12 per 1000 live births. From 2000 to 2020, neonatal mortality was reduced by more than half, from 16 to 7 per 1000 live births,2 and the coverage gap of key care indicators such as skilled birth attendance and antenatal care (ANC) contacts was largely closed.3 This success was attributed to overall improvements of social determinants of health, cross-cutting antipoverty programmes, and implementation of targeted maternal, neonatal, and child health interventions—all in a context of political stability and economic growth.4,5 Despite this remarkable progress, not all regions in Peru benefited equally. Significant socioeconomic and health inequalities persist, especially among the poorest and those living in rural areas.6,7
Loreto, Peru's largest department located in the Amazon rainforest, home to a large diversity of indigenous populations scattered across vast remote areas,8 is one of the regions with worst maternal and neonatal health indicators. Neonatal mortality estimates for Loreto suggest a rate of 19 per 1000 live births based on 2010–2012 Demographic Health Survey (DHS) data,5 with 55% of neonatal deaths expected to be under-registered.9 Anecdotal evidence suggests that neonatal mortality in indigenous communities might even be higher, with infections presenting the leading cause of death.10 Formative research conducted by our group in rural areas of three underserved districts in Loreto suggests difficult geographic access to health facilities; while facilities are often poorly staffed and perceptions of mistreatment and inadequate care are common.11,12 Based on census data from 2019, we found that two out of every three women give birth at home, with almost complete absence of skilled attendants.13 Essential newborn care (ENC), a set of practices implemented around birth to ensure optimal breastfeeding, thermal, and hygienic care, had a low prevalence. While the coverage gap was most pronounced in home births, coverage was also not universal in facility births, despite ENC being cost-effective, easy to implement, and directly linked to newborn survival.13, 14, 15
Disruption to provision of routine care and economic hardship caused by the Covid-19 pandemic likely further exacerbated access barriers to facility-based maternal-neonatal health care.11 From March 2020, Peru implemented a strict lockdown in response to the Covid-19 pandemic, including police and military-enforced home isolation, a night curfew, school closures and prohibition of non-essential businesses and domestic travel that were only gradually eased from July 2020. While not all of these centralised governmental measures were put into practice in rural Amazon, community isolation and travel restrictions were common. Routine services were frequently suspended in rural health facilities during the first months of the pandemic, while many local Community health workers (CHW) continued their activities. Despite these measures, outbreaks in communities were frequent and fatalities were reported.11
Neonatal deaths that are mostly preventable16 can be reduced through effective interventions across a variety of delivery platforms.15 Evidence from South Asia and Southern Africa suggests that community-based approaches such as counselling and care by CHW can achieve reductions in neonatal mortality of 11–25% and are particularly effective in settings with high mortality and few facility births.17,18 However, as these interventions are complex19 as involving multiple stakeholders, targeted behaviours, and mechanisms of change,20, 21, 22 the degree of impact is highly setting-specific. In Peru, large-scale MNCH interventions involving community actors included the Primary Health Care Strategy,23 the Integrated Management of Childhood Illness programme,24,25 and the Proyecto 2000.26 Although as of 2020 there were more than 34000 health-related and community-based actors registered in Peru,27 so far CHW or traditional birth attendants (TBA) have not played a major role in large-scale programmes. Furthermore, rigorous prospective evaluations are scarce, highlighting an important knowledge gap regarding the impact of community-based interventions on MNCH outcomes, their implementation characteristics, and underlying mechanisms in Peru and the Amazon setting specifically (see comprehensive review—Supplementary Materials 2).
We developed a community-based intervention with CHW and TBA training, combined with supportive facility strengthening to promote ENC practices and healthcare seeking. We conducted a prospective before-and-after study to assess the effect and changes over time of the Mamás del Río intervention on ENC in home births in three districts in Amazonian Peru, two and three years after implementation. We also evaluated ENC in facility births and healthcare utilization in all births as secondary outcomes.
Methods
Study area
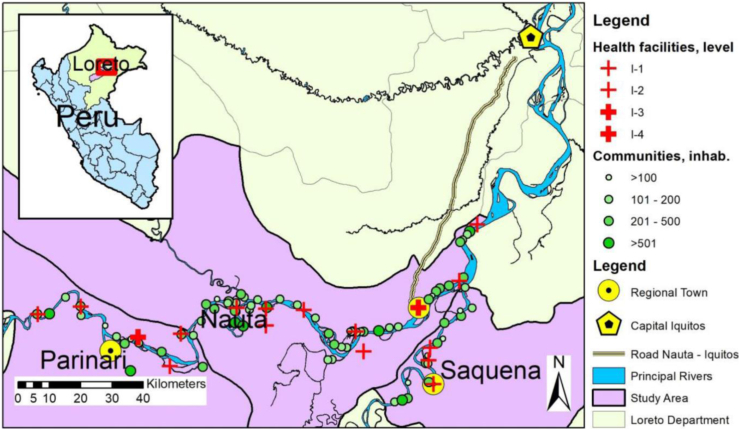
The study area comprised 79 communities in rural areas of three districts (Nauta, Parinari, Saquena) of Loreto, located within the Amazon basin in the north of Peru (Fig. 1). Detailed descriptions of the study setting have been reported previously.11, 12, 13 Briefly, the principal ethnic group in the study areas are the Kokama-Kokamillas, who live in communities dispersed along the Amazon River tributaries within dense tropical rainforest. Most are poor subsistence farmers and fishers with a monthly income of less than 50 USD. Running water, electricity, and sanitation are often lacking and hygienic conditions are poor. A total of 18 health posts and three health centres are situated within the study area. All facilities provide basic routine antenatal and postnatal care but are only capable of attending imminent births. Obstetric emergencies are referred to the largest health centre in Nauta and the regional hospital in Iquitos. There are multi-faceted access barriers to facilities, including difficult geographic access via river and high travel costs, poor staffing and equipment of facilities, and poor perception of services by women. Most communities have their own health promoters (promotores de salud), volunteers trained by church, governmental, and non-governmental organisations; as well as other community-based health actors including TBA (parteras tradicionales), healers (vegetalistas, curanderos, hueseros), and sobadoras who, amongst others, align the baby's position in the uterus.
Fig. 1.
Mamás del Río study area (own assembly, reproduced from Reinders et al., 2020).
Intervention
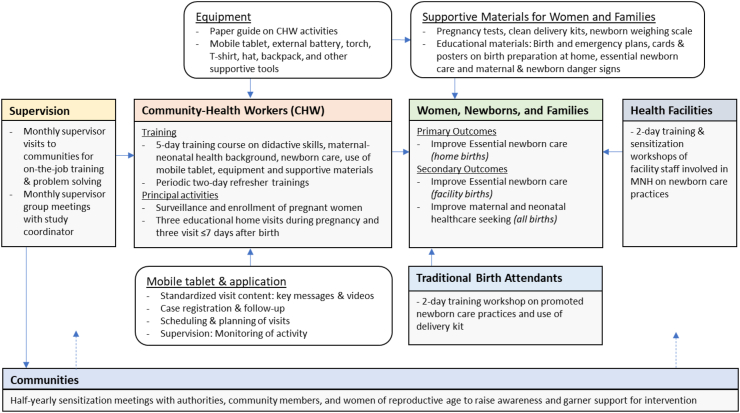
Our formative research11, 12, 13 suggested poor birth and newborn care in a setting with high neonatal mortality. Due to a high proportion of home births that is unlikely to change due to described access barriers to facility care, along with an existing network of CHW without structured activities, we opted to develop a largely community-based intervention. The Mamás del Río intervention is aiming to improve ENC practices and promote healthcare seeking among women and their newborns through educational home visits by CHW supported by electronic tablets as job aids. Supportive components include ENC training of TBA and health facility staff, as well as comprehensive supervision and community sensitizations for awareness raising (Fig. 2). A full description of the intervention can be found in the study protocol.28
Fig. 2.
Conceptual framework of the Mamás del Río intervention.
Community health workers
CHW represent the central element of the intervention. Communities received written invitations to participate in the programme and to select one CHW candidate, who was required to be a trusted male or female resident, parent of own children, with or without prior experience in health, and willing to be trained, to use an electronic tablet, and work as a volunteer.
CHW were trained to identify possible pregnancies through community engagement, confirm pregnancies by administering pregnancy tests, and enrol pregnant women to receive home visits with their verbal permission. CHW were asked to conduct three home visits during pregnancy and three home visits during the first week postpartum to pregnant women, mothers and their newborns, and family members. Schedule and content were adapted based on guidance by WHO/UNICEF29 and the Peruvian Ministry of Health.30 Visits during pregnancy covered promotion of facility birth, ANC visits, and recognition of maternal danger signs. The second and third home visit shortly before birth covered promotion of newborn and immediate birth care practices and distribution of clean delivery kits. Home visits 4 to 6 after birth included weighing and referral of newborn in case of low birth weight, reinforcement of newborn care, and recognition of neonatal danger signs (see Figure S1 for complete visit schedule).
CHW were equipped with internet-capable electronic tablets running the CommCare application (Dimagi Inc. Cambridge, Massachusetts), programmed to represent the logical structure and schedule of home visit. Tablets were intended as job aids to provide standardized visit content and support behaviour-change communication through images and videos, some of which were co-created with the communities,31 scheduling and reminder of visits, registration and follow-up. Other supportive materials included urine-based pregnancy tests, educational cards and posters on newborn care, clean delivery kits, and weighing scales.
Five-day baseline trainings covering theoretical sessions and practical role plays on ENC practices, use of materials, and conduct of home visits were held by two local facilitators with a professional health background and overseen by a member of the study team who developed the materials. After the initial training, periodic two-day refresher and consolidation trainings with CHW were conducted covering selected ENC practices, communication skills, and tablet use. These trainings were subsequently repeated to replace CHW who dropped-out. Written informed consent for participation as a CHW volunteer in the programme and collection of process data was obtained. All participants received small monetary compensation for their travel costs.
TBA and facility staff
TBA were found to be key influencers of ENC practices for home births.13 Communities were invited to select TBA for two-day training workshops covering the importance of ENC, use of clean delivery kits, and practical simulation of care using plastic dolls. Repeat trainings were held periodically. Staff of health facilities in the study area that were involved in maternal-neonatal care participated in two-day training workshops on routine newborn care,32 adapted from the WHO ENC course33 and Peruvian guidelines,34 as well as sensitization on the scope of the intervention and to build collaborations with CHW. Facility staff training was developed, organized, and conducted together with regional health authorities and planned to be repeated half-yearly.
Supervision & community sensitization
The intervention was designed with comprehensive supervision. Supervisors were asked to pay monthly visits to communities to provide support, on-the-job training, and materials to CHW. During their visits, supervisors also meet with community leaders, TBA, and health facility staff to maintain ongoing dialogue and solve any problems. Supervisors were paid staff local to the region, with at least a technical degree in nursing. They were trained during a 5-day workshop and received field-training by the study team covering intervention goals, CHW activities, and supervisory tasks. They attended monthly group meetings with the study coordinator for feedback, planning of visits, and activity monitoring of app data use by CHW. Supervisors also conducted half-yearly community sensitization through townhall meetings to raise awareness and garner support for the intervention.
Study design & participants
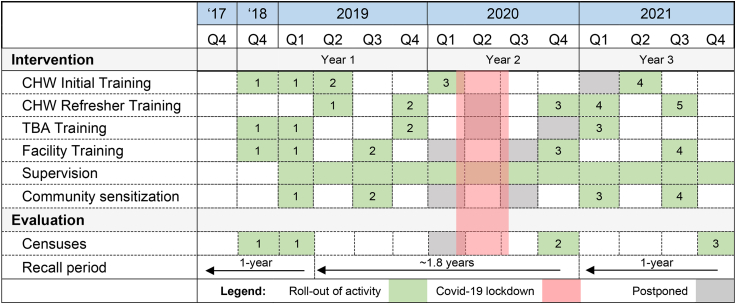
The evaluation of the Mamás del Río programme consists of an outcome and process evaluation.28 As part of the outcome evaluation, we conducted a prospective before-and-after study to assess the effect after implementation and changes over time of the intervention on ENC practices and healthcare utilization. Outcomes were measured through three repeated, cross-sectional household censuses conducted at baseline before implementation in early 2019, and at year 2 and year 3 follow-up after implementation of the intervention (Fig. 3).
Fig. 3.
Implementation of intervention and evaluation activities throughout the study period. Numbers denote separate implementation activities. Baseline CHW training (1) was implemented between December 18 and February 19; repeat trainings to replace dropouts (2, 3, and 4) were implemented thereafter. Intervention kicked-off with start of supervision activities in Feb ‘19 and terminated with last supervision in October 21; for a total duration of 2 years and 8 months. The first census for baseline measurement was conducted between December 18 and January 19, with a 1-year recall period and earliest birth included was in December 17. The second census for follow-up was planned one year after but postponed to November 20 due to Covid-19 with an extended recall period. The third and last follow-up census conducted in November 21 with a regular 1-year recall period.
The Covid-19 pandemic and associated lockdown, which occurred about a year into our study, imposed deviations from the original study protocol.28 While we had planned to conduct all three censuses with a one-year recall period, the first follow-up census had to be postponed for almost a year and was conducted with a longer recall period, extending the overall study period to almost three years (Fig. 3). While we had planned to pool follow-up censuses, we finally decided to assess the effect over separate follow-up time points, to account for differential recall periods and possible interference by Covid-19.
Study participants for the evaluation were women between 15 and 49 years with a singleton live birth as the principal beneficiaries of the intervention. While the baseline census and the year 3 follow-up census included women with a live birth within the last year, the extended recall period of the second census meant that all women with a live birth since the baseline census were included (see Fig. 3). Only vaginal births were included for the analysis of ENC at facilities as caesarean births likely had received different treatment and are unable to report on most ENC practices. Ethical approval was received from the Universidad Peruana Cayetano Heredia (16071) and the London School of Hygiene & Tropical Medicine (100419).
Outcomes
Primary outcomes were defined a priori28 as ENC in home births, and included practices related to thermal care (immediate drying, immediate skin-to-skin contact, delayed bathing for the first three days), hygienic cord care (clean cord tying with a new clamp or thread, clean cord cutting with a new scalpel, razor blade or scissors, and no harmful substances applied to cord other than alcohol or water/soap), and optimal breastfeeding (colostrum feeding, early breastfeeding within 1 h after birth, and exclusive breastfeeding within the first three days). Definition and operationalization of primary outcomes can be found in Figure S2. Secondary outcomes were ENC practices among facility births as well as utilization of maternal-neonatal health care at facilities (ANC, facility birth, and postnatal newborn check-up) among all births.
Data collection & procedures
Censuses covering the entire population of the study area were conducted in all communities to evaluate study outcomes, detailed procedures were reported previously.13,28 Briefly, censuses consisted of enumerating households (i.e. systematic listing of all household members) to identify all eligible women for participation in a questionnaire covering women's and household characteristics, healthcare seeking, intervention exposure, and birth and newborn care practices of their last birth. Written informed consent testified by an independent witness was obtained from eligible women willing to participate. Questionnaires were administered electronically using mobile devices by female health professionals who received prior training.
To evaluate implementation characteristics, data was collected from multiple sources. CHW were administered a questionnaire regarding their characteristics, prior experience, and activities. The study coordinator collected data regarding implementation of training activities and retention of CHW throughout the study.
The study area and corresponding number of communities was predetermined based on logistical and budgetary considerations. Power calculations for the initially planned before-and-after analysis based on two time points were conducted for all primary outcomes, using assumptions based on estimates from a pilot survey from 2018. Minimal absolute detectable increases of changes in ENC in home births ranged from 9 to 20% for expected sample sizes and different design effect scenarios,28 which we deemed attainable.
Definition of variables
All outcomes were based on maternal self-report. Operational definitions of ENC indicators and coding of variables have been reported previously.13 Place of birth was defined as at home, at a health facility, during transit, or as ‘other’ if unable to categorize to any prior category. Categories of monthly household income were based on poverty levels for the rural jungle region in Peru.35 ANC contacts were coded into four levels (≥8, 6–7, 1–5, and 0) to reflect WHO recommendations,36 Peruvian recommendations,37 insufficient contact, and no contact, respectively.
Statistical analysis
We cross-tabulated women's characteristics by each census and calculated column percentages. To assess differences between baseline and follow-up censuses, we calculated p-values using Pearson's chi-squared test converted into F statistic together with the ‘svy’ command correcting for survey design,38 accounting for clustering of observations at the community level39 since women from the same community might share similar characteristics or practices.
Women's self-reported receipt of CHW home visits was considered the principal intervention exposure. Coverage of CHW home visits was calculated as proportion of women with any CHW visit during pregnancy or during the first week postpartum, stratified by calendar year quarter based on newborns' birth dates. Coverage of CHW throughout the study was calculated as proportion of CHW among all communities who received baseline training or subsequent training to replace dropouts and were active during each quarter. Coverage of trained TBA among all communities and coverage of health facilities with at least one trained staff were also calculated and reported together with CHW characteristics and coverage to describe the intervention's key implementation characteristics.
To evaluate the effect of the intervention on outcomes, we first compared outcomes between baseline and year 2 follow-up census to assess changes from before to after implementation. Secondly, we compared outcomes between year 2 and year 3 follow-up to assess whether changes were maintained over time. We calculated prevalence of primary and secondary outcomes as proportion of women reporting a specific outcome; cases with “don't know” responses or missing data were omitted from analysis. 95% confidence intervals (95% CI) were calculated based on Taylor-linearized standard errors, also accounting for clustering at the community level.38, 39, 40
To assess for changes between time points, we calculated adjusted prevalence differences (PD)13 using a three-step approach. First, we fitted logistic regression models and used a time variable to estimate the effect of time, representing intervention availability, on outcomes. To adjust for confounding, we then added women's education as a covariate to all models. Education was considered an a priori confounder as being an important determinant of ENC13 and use of facility care41,42; as well as likely changing over time as observed in other rural areas in Peru.35 In addition, we used a stepwise forward selection approach to examine other covariates as potential confounders based on a change-in-estimate criterium of ≥10%. Ethnicity, religion, district, parity, and ANC contacts were additional covariates that qualified for some models, as described in the results section. Using the output from the logistic regression models, we then transformed odds ratios to PD using a post-estimation approach.13 95% CI were calculated using the Taylor linearization and p-values based on the linear test of equivalence between baseline and follow-up prevalence.40,43
To assess the impact of the Covid-19 lockdown on outcomes, we conducted a sensitivity analysis using data from the year 2 follow-up census and stratified outcomes by birth dates of newborns born before and after onset of lockdown on 16 March 2020. All analyses were conducted using Stata 17.0 (Stata Corp, College Station, Texas).
Role of funding source
This manuscript has been prepared as part of the implementation and evaluation of the Mamás del Río program, funded by the National Council of Science and Technology, Grant Number 135-2016 and Grand Challenges Canada, Grant Number 0816-05. The funders had no role in study design, data collection and analysis, decision to publish, preparation of the manuscript, or any other aspect pertinent to the study.
Results
Implementation characteristics
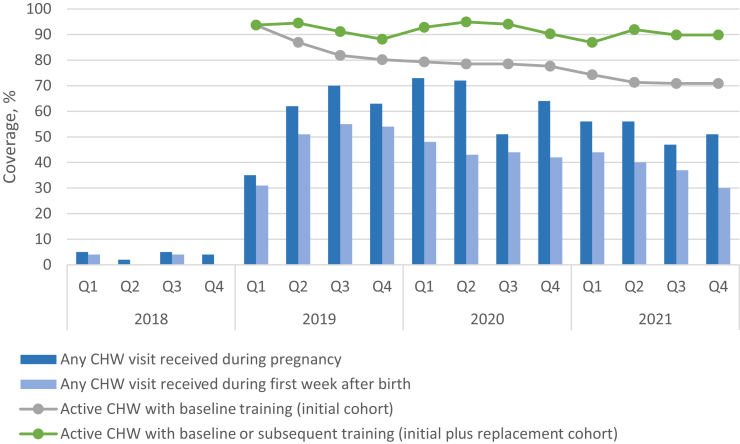
Baseline training of CHW, TBA, health staff, and supervisors was undertaken between December 2018 and February 2019 (Fig. 3). At baseline, n = 77 CHW received training and were active across all communities in the study area (77/79, 97%, see Fig. 4). Questionnaire data was available for 88% (68/77) CHW, of which 79% were male (54/68) and 82% (56/68) were between 30 and 71 years of age (Table S1). Only a quarter (17/68, 25%) had secondary education and few had experience with smartphones (18/68, 27%). About half (33/68, 52%) were actively performing tasks as health promoters in their communities prior to Mamás del Río training, mostly offering treatment or cures to the general population (31/68, 46%). Only 37% (25/68) had received any other training in the last 5 years. Coverage of CHW remained high (71/79, 90%) at the end of study, while 73% (56/77) from the initial cohort were retained as active volunteers.
Fig. 4.
Coverage of CHWhome visits and retainment of active CHW over time. Annotations: Data of CHW visits based on women questionnaire. Data on CHW retainment based on supervisor documentation. Total number of dropouts: 2019 (n = 17), 2020 (n = 5), and 2021 (n = 7); Number of dropouts from the initial cohort: 2019 (n = 14), 2020 (n = 2), and 2021 (n = 5).
At baseline, 67% (53/79) communities had at least one TBA trained, while coverage was lower during subsequent trainings (63%, 51/79 and 42%, 33/79). More than two thirds (71%, 15/21) of facilities had at least one staff trained at baseline, while coverage increased to 86% (18/21) at last training (Table S2). Supervisors started their monthly supervision visits with community sensitization in February 2019, marking the start of the intervention. While trainings were planned at regular intervals throughout the planned study period of two years, the onset of the Covid-19 pandemic led to postponement of several activities anticipated for 2020 (Fig. 3). The study ended with cease of supervision by end of October 2021.
Census
Censuses were completed for all (79/79) communities, and participation among enumerated houses was high (≥99%, Figure S3). A total of 1192 completed questionnaires were available and participation was high for baseline (324/326, 99%), year 2 (532/555, 96%) and year 3 follow-up (336/339, 99%) censuses.
Women's characteristics
At baseline, most women (202/324, 62%) with a live birth in the last 12 months were between 20 and 34 years of age (Table 1). Half of women (163/322, 51%) had only primary education and 52% (167/322) lived in extreme poverty. About half (148/313, 47%) were of the Kokama-Kokamilla ethnicity and 52% (162/311) were Catholic. Most women (276/324, 85%) had more than one child, while 35% (114/324) had five or more children. Two thirds (213/324, 66%) lived more than 10 km traveling distance via river from a health centre and only 26% (83/323) had eight or more ANC contacts. About two thirds of women gave birth at home (208/324, 64%) and most births were attended by a TBA (132/324, 40%) or a family member (64/324, 20%). Few children were born in health posts (33/324, 10%), health centres (40/324, 12%) or hospitals in the capital (41/324, 13%); proportion of caesarean section was 8% (25/324).
Table 1.
Characteristics of women between 15 and 49 years with a live birth in the last 12 months at baseline, follow-up year 2, and follow-up year 3.
| Baseline (Dec 2017–Jan 2019, n = 324) |
Follow-up year 2 (Feb 2019–Oct 2020, n = 532) |
p-value | Follow-up year 3 (Nov 2020–Nov 2021, n = 336) |
p-value | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| District | ||||||||
| Nauta | 205 | 63 | 323 | 61 | 0.63 | 191 | 57 | 0.42 |
| Parinari | 66 | 20 | 120 | 23 | 82 | 24 | ||
| Saquena | 53 | 16 | 89 | 17 | 63 | 19 | ||
| Age | ||||||||
| 15–19 | 57 | 18 | 95 | 18 | 0.25 | 72 | 21 | 0.15 |
| 20–34 | 202 | 62 | 354 | 67 | 203 | 60 | ||
| 35–49 | 65 | 20 | 83 | 16 | 61 | 18 | ||
| Highest educationa | ||||||||
| No education | 3 | 1 | 4 | 1 | 0.0031 | 3 | 1 | 0.50 |
| Primary | 163 | 51 | 201 | 38 | 133 | 40 | ||
| Secondary | 149 | 46 | 306 | 58 | 192 | 57 | ||
| Superior | 7 | 2 | 21 | 4 | 7 | 2 | ||
| Household incomeb | ||||||||
| <S/150 extreme poverty | 167 | 52 | 233 | 45 | 0.20 | 165 | 50 | 0.24 |
| S/151–250 poverty | 90 | 28 | 178 | 34 | 116 | 35 | ||
| >S/250 above poverty line | 65 | 20 | 110 | 21 | 49 | 15 | ||
| Ethnicityc | ||||||||
| Kokama-Kokamilla | 148 | 47 | 231 | 47 | 0.54 | 136 | 44 | 0.0020 |
| Mixed-race | 132 | 42 | 195 | 40 | 155 | 50 | ||
| Other/None | 33 | 11 | 64 | 13 | 20 | 6 | ||
| Religiond | ||||||||
| Catholic | 162 | 52 | 239 | 48 | 0.60 | 148 | 45 | 0.0011 |
| Evangelic | 123 | 40 | 215 | 43 | 129 | 39 | ||
| Others | 26 | 8 | 41 | 8 | 54 | 16 | ||
| Birth order | ||||||||
| 1 | 48 | 15 | 136 | 26 | 0.0004 | 80 | 24 | 0.33 |
| 2–4 | 162 | 50 | 257 | 48 | 155 | 46 | ||
| ≥5 | 114 | 35 | 139 | 26 | 101 | 30 | ||
| Distance to health centre | ||||||||
| ≤0–10 km | 111 | 34 | 183 | 34 | 0.95 | 105 | 34 | 0.39 |
| 11–22 km | 104 | 32 | 175 | 33 | 123 | 33 | ||
| 23–51 km | 109 | 34 | 174 | 33 | 106 | 33 | ||
| Antenatal care contactse | ||||||||
| 0 | 25 | 8 | 45 | 9 | 0.58 | 19 | 6 | 0.12 |
| 1–5 | 111 | 34 | 194 | 38 | 143 | 44 | ||
| 6–7 | 104 | 32 | 145 | 29 | 101 | 31 | ||
| ≥8 | 83 | 26 | 122 | 24 | 65 | 20 | ||
| Type of birth | ||||||||
| Vaginal | 299 | 92 | 500 | 94 | 0.26 | 311 | 93 | 0.42 |
| Caesarean | 25 | 8 | 32 | 6 | 25 | 7 | ||
| Place of birth | ||||||||
| Hospital | 41 | 13 | 66 | 12 | 0.027 | 39 | 12 | 0.32 |
| Health centre | 40 | 12 | 91 | 17 | 54 | 16 | ||
| Health post | 33 | 10 | 83 | 16 | 39 | 12 | ||
| At home | 208 | 64 | 286 | 54 | 197 | 59 | ||
| Transit/Other | 2 | 1 | 6 | 1 | 7 | 2 | ||
| Type of birth attendant | ||||||||
| Skilled birth attendant | 128 | 40 | 246 | 46 | 0.11 | 135 | 40 | 0.047 |
| Traditional birth attendant | 132 | 40 | 175 | 33 | 140 | 42 | ||
| Family member/unskilled | 64 | 20 | 111 | 21 | 61 | 18 | ||
| Any MDR CHW home visit | ||||||||
| During pregnancyf | 12 | 4 | 322 | 63 | <0.0001 | 180 | 54 | 0.017 |
| After birthg | 5 | 2 | 255 | 48 | <0.0001 | 128 | 38 | 0.011 |
P-values calculated using F-test accounting for clustering at the community level.
Highest level reached, completed and not completed. Three women responded with “don't know”.
Monthly gross household income. Currency is Peruvian Soles (PEN), at the time of write-up 1 PEN was 0.27 USD, with income categories translating to < 41 USD = extreme poverty, 41–68 USD = poverty, and >68 USD = above poverty line. Eighteen women responded with “don't know”.
Seventy-eight women responded with “don't know”.
Fifty-five women responded with “don't know”.
Thirty-five women responded with “don't know” or had missing values.
Four women responded with “don't know”.
Two women responded with “don't know”.
At year 2 follow-up compared to baseline, more women had secondary education (58% vs 46%, p = 0.0031), were primiparous (26 vs 15%, p = 0.0004), and gave birth in a health centre (17 vs 12%, p = 0.027) or health post (16 vs 10%, p = 0.027; Table 1). At year 3 compared to year 2 follow-up, more women identified themselves as mixed-race (50 vs 40%, p = 0.0020) and pertained to other religions (16 vs 8%, p = 0.0011), while more births were attended by TBA (42 vs 33%, p = 0.047). There were no changes in facility births (Table 1).
Exposure to CHW home visits
The coverage of home visits by trained CHW increased from baseline to year 2 follow-up from 4% to 63% (p < 0.0001) and from 2% to 48% (p < 0.0001) during pregnancy and after birth, respectively (Table 1). From year 2 to year 3 follow-up, visits decreased during pregnancy (63%–54%, p = 0.017) and after birth (48% vs 38%, p = 0.011). Stratification by quarter revealed a steep increase in visits after implementation, a sudden reduction of visits in Q3 2020, and a subtle decline in visits until the end of the study (Fig. 4).
ENC in home births
After implementation, consistent improvements were seen in seven out of nine ENC practices for home births (Fig. 5a–c). From baseline to year 2 follow-up, largest unadjusted PD were found in skin-to-skin contact (PD: 50% [95% CI: 42–58], p < 0.0001; change from 9 to 59%, respectively) and colostrum feeding (PD: 46% [36–55], p < 0.0001; 39–85%), see Table 2. Improvements of intermediate effect size were seen in no application of harmful substances to cord (PD: 19% [10–28], p = 0.0001; 59–78%), cord tying (PD: 15% [8–23], p = 0.0001; 78–93%), and delayed bathing (PD: 14% [9–19], p < 0.0001; 80–94%). Small improvements were found for clean cord cutting (PD: 10% [2–19], p = 0.016; 80–91%) and exclusive breastfeeding during the first 3 days (PD: 10% [5–15], p = 0.0006; 87–97%). Adjustment for education and other covariates (see details in footnote of Table 2) did not alter effect estimates importantly, with only minimal differences in point estimates for clean cord cutting (adjusted PD: 11% [3–20], p = 0.012), colostrum feeding (adjusted PD: 45% [35–54], p < 0.0001), and exclusive breastfeeding (adjusted PD: 11% [5–16], p = 0.0006). From year 2 to year 3 follow-up, no evidence for change in most indicators was found after adjustment (see Table 2); except for a reduction in application of no harmful substances (adjusted PD: −14% [−24 to −4], p = 0.0070) and weak evidence for a reduction of clean cord tying (adjusted PD: −5% [−10 to 0], p = 0.041).
Fig. 5.
a–c: Primary outcomes:thermal care, breastfeeding practices, and cord care reported by women between 15 and 49 years who had a live birth at home—at baseline, follow-up year 2, and follow-up year 3.
Table 2.
Changes in coverage of essential newborn care practices of women between 15 and 49 years who had a live birth at home (primary outcomes) from baseline to follow-up year 2 and follow-up year 3.
| Prevalence difference baseline to Follow-up year 2 |
Prevalence difference follow-up year 2 to follow-up Year 3 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted |
Adjusteda |
Unadjusted |
Adjustedb |
|||||||||
| % | 95% CI | p-value | % | 95% CI | p-value | % | 95% CI | p-value | % | 95% CI | p-value | |
| Thermal care | ||||||||||||
| Immediate drying | 4 | −5 to 12 | 0.38 | 3 | −6 to 11 | 0.52 | −1 | −9 to 7 | 0.83 | −1 | −9 to 8 | 0.88 |
| Immediate skin-to-skin contact | 50 | 42–58 | <0.0001 | 50 | 42–58 | <0.0001 | −3 | −15 to 9 | 0.66 | −3 | −15 to 9 | 0.63 |
| Delayed bathing | 14 | 9–19 | <0.0001 | 14 | 8–20 | <0.0001 | 1 | −4 to 6 | 0.73 | 0 | −5 to 5 | 0.91 |
| Cord care | ||||||||||||
| Clean cord tying | 15 | 8–23 | 0.0001 | 15 | 8–22 | <0.0001 | −5 | −10 to 0 | 0.042 | −5 | −10 to 0 | 0.041 |
| Clean cord cutting | 10 | 2–19 | 0.016 | 11 | 3–20 | 0.012 | 0 | −6 to 6 | 0.99 | 2 | −3 to 7 | 0.41 |
| Nothing harmful applied | 19 | 10–28 | 0.0001 | 19 | 10–28 | 0.0001 | −14 | −24 to −4 | 0.0080 | −14 | −24 to 4 | 0.0070 |
| Breastfeeding | ||||||||||||
| Colostrum feeding | 46 | 36–55 | <0.0001 | 45 | 35–54 | <0.0001 | −3 | −11 to 6 | 0.54 | −2 | −10 to 6 | 0.63 |
| Early breastfeeding | 8 | −2 to 18 | 0.14 | 8 | −2 to 18 | 0.11 | 4 | −6 to 15 | 0.41 | 4 | −6 to 14 | 0.43 |
| Exclusive breastfeeding first 3 days | 10 | 5–15 | 0.0006 | 11 | 5–16 | 0.0006 | −2 | −5 to 1 | 0.20 | −3 | −6 to 1 | 0.10 |
95% Confidence Intervals (95% CI) were calculated based on Taylor-linearized standard errors accounting for clustering at the community level.
All models for baseline and follow-up year 2 comparison were adjusted a priori for education. Additional covariates included based on ≥10% change-in-estimate criterium were ethnicity for of delayed bathing and cord cutting; and ethnicity + religion for of exclusive breastfeeding first 3 days.
All models for follow-up year 2 and year 3 comparison were adjusted a priori for education. Additional covariates included based on ≥10% change-in-estimate criterium were ethnicity for delayed bathing; ethnicity + religion for cord cutting; and religion for exclusive breastfeeding first 3 days.
ENC in facility births
From baseline to year 2 follow-up, among women with vaginal births in health facilities, improvements were seen in delayed bathing (adjusted PD: 32% [20–45], p < 0.0001), colostrum feeding (adjusted PD: 22% [13–30], p < 0.0001), and immediate skin-to-skin contact (adjusted PD: 19% [8–31], p = 0.0015), see Tables S4 and S5 for comprehensive results. From year 2 to year 3 follow-up, some evidence was found for a reduction in skin-to-skin contact (adjusted PD: −12 [−22 to 2], p = 0.028).
Health care seeking
From baseline to year 2 follow-up, the proportion of facility births increased (adjusted PD: 8% [14–1], p = 0.021), more newborns were weighed early (adjusted PD: 15% [7–24], p = 0.0005) and had an early check-up (adjusted PD: 7% [3–11], p = 0.0011), see Tables S6 and S7. Weak evidence for a reduction in ≥6 ANC contacts (PD: −7% [−14 to 1], p = 0.092) was found after adjustment. From year 2 to year 3 follow-up, some evidence was found for a reduction in early weighing of newborns (adjusted PD: −7% [−14 to 0], p = 0.043) while the other indicators remained unchanged.
Subgroup analysis Covid
Post-hoc stratification of year 2 follow-up data by birth dates before and after onset of lockdown showed no substantial changes in coverage levels of ENC outcomes in facility or home births (Tables S8 and S9). While the proportion of facility births remained similar, fewer women had ≥6 ANC visits after onset of lockdown (40% [95% CI: 32–49]) compared to before (59% [53–65]), see Table S10. Fewer newborns were weighed early after (62% [54–69]) compared to before lockdown (74% [68–79]); however, confidence intervals were narrowly overlapping.
Discussion
Key findings
Substantial and consistent improvements were seen across almost all ENC practices for home births at year 2 follow-up, with largest increases in skin-to-skin contact, colostrum feeding, and cord care. Coverage levels of most practices were sustained at year 3 follow-up, except for cord care. These results were achieved in a context of major disruptions due to the Covid-19 pandemic and an unprecedented lockdown. ENC practices among facility births, defined as secondary outcomes, saw fewer and smaller improvements, with only three indicators improving after implementation. There were small increases in facility births and early newborn checkups; while coverage of ≥6 ANC contacts seemed to decrease at year 2 follow-up. Post-hoc stratification showed that while healthcare utilization tended to decrease after start of lockdown, ENC practices for home or facility births were not impacted. About two thirds of women were visited by a CHW during pregnancy after implementation. While visit coverage was only marginally impacted during the first months of lockdown, we observed a subtle downwards trend in visits towards the end of the study.
Comparison to other studies
As far as we know, our study is the first one to document the impact of a community-based intervention on MNCH and specifically on ENC outcomes in Peru. Large cluster-randomized trials from LMIC countries in South Asia and Sub-Saharan Africa have already demonstrated that community-based interventions with CHW home visits can effectively reduce neonatal mortality and improve ENC practices, which amongst others, were intermediate outcomes in all trials.44, 45, 46, 47, 48, 49 Studies that did not find an effect on neonatal mortality and/or ENC cited low home visit coverage49,50 or inadequate targeting of neonatal mortality risk factors.51 Findings from our study are consistent with other non-randomized but larger proof-of-principle studies from LMIC, which documented moderate to large effect sizes in before-and-after comparisons on breastfeeding practices (10–35%),52, 53, 54, 55, 56, 57 hygienic cord care (11–36%),52, 53, 54,56,57 and thermal care (16–41%)45,53, 54, 55, 56, 57, 58 for home and facility births combined.
Implementation characteristics of CHW component
The intervention was designed with CHW as the central element. Following written invitations detailing CHWs' future roles while avoiding hard selection criteria, CHW were chosen by their own communities during investigator-unfacilitated assemblies. CHW who attended trainings were mostly poorly educated, middle-aged, male health promoters. While this ensured an experienced cadre of CHW, their gender might have been an issue—male CHW usually have lower acceptance among female recipients, especially in maternal-neonatal health care covering intimate topics that often require trust for successful interactions; while pre-existing social gender norms can act as further barriers.20, 21, 22,59 Given this, the major effect seen comes somewhat as a surprise and warrants closer examination of the CHW's role in the mechanisms of change and their reception by women in this setting.
About two thirds of eligible women were reached by CHW in the first two years after implementation. Larger proof-of-principle studies from South Asia and Sub-Saharan Africa achieved coverage levels of home visits during pregnancy of 31–83% (median 59%).52, 53, 54, 55, 56, 57, 58,60 While our CHW achieved good coverage at intermediate levels, CHW in reviewed studies had much larger populations to cover (one CHW per 771 to 4367 population) compared to CHW in our study (one CHW per 133 population), where communities are small and each traditionally provide their own CHW. While at the end of our study only about half of eligible women received a visit during pregnancy, 86% reportedly had heard of the programme (data not shown). These findings indicate that CHW did not achieve their full potential, especially towards the end of the study, as they missed an important number of women despite having a comparably low workload.
Coverage of trained and active CHW was almost universal after implementation and remained very high throughout the study due to subsequent trainings replacing dropouts. Three quarters of CHW were retained at the end of the study; a principal reason for dropout being the lack of payment and/or time for volunteering (data not shown). Published data on CHW attrition is scarce and the few available estimates range widely.61,62 Considering that our CHW did not receive any remuneration or major incentives, the attrition rate in our study seems acceptable. While we chose this approach in line with Peru's CHW policy,63 current WHO guidelines recommend, amongst others, financial incentives as part of CHW programmes.64 Achieving long-term sustainability with a volunteering approach in combination with structured activity and supervision, as in our case, might therefore be difficult and needs further appraisal.
Implementation characteristics of TBA component
Consistent and substantial increases across ENC practices in home births in the context of intermediate home visit coverage suggest other causative mechanisms exerting effects. In our setting, TBA attend about two thirds of home births and are therefore key influencers of ENC. Current WHO guidance advocates partnership with TBA and endorses their training in settings where they remain key providers of care at birth.65 This strategy however has been controversial in the past and the role of TBA was marginalized in global health policy for decades as considered detrimental to ensuring skilled attendants for every birth.66,67 In Peru, although participation of the community in the referral and promotion of maternal-neonatal health care at facilities is a goal in the Ministry's of Health latest plan for reduction of maternal and perinatal mortality, TBA are not specifically mentioned.68
In our intervention, we decided to integrate TBA training to align with the reality of our setting, characterized by multi-faceted access barriers for institutional births. After implementation, two-thirds of communities had a trained TBA, who were mostly middle- and older-aged women with experience in attending births. While the inherent profile and role of TBA themselves have long been seen as a barrier to change of practices,66 our experience suggests that TBA training may have been an important factor in improving ENC practices at home. Furthermore, the concern that provision of clean delivery kits could incentivize home births was not substantiated, as we saw increases in facility births. The TBA's exact role in achieving changes as well as their attitudes towards institutional births and new care practices remains to be investigated.
Secondary outcomes
Smaller improvements in ENC were seen among facility births. This might be related to the relatively high prevalence of ENC indicators at baseline, making it more difficult to achieve improvements. While coverage of at least one trained staff among facilities was high, we did not have data to assess overall coverage among all staff, which might have been lower. Furthermore, a smaller effect might be attributed to the relatively short training duration of 2 days, inclusion of other training topics competing with ENC content, and heavy staff rotation as many participants were trainees of SERUMS, a national internship programme for recent graduates to counter the shortage of healthcare workers in rural areas of Peru.69
A secondary objective of our intervention was to increase health care utilization, mainly through CHW raising awareness of benefits and thus increasing demand. We detected a small but meaningful increase in facility births, both in health posts and centres but not in hospitals. This was surprising given the profound access barriers and women's preference for home births,12 expected to rather require an intervention fostering structural change by targeting financial incentives, transport systems, quality of care, and cultural competency of facility staff.70, 71, 72 Although this small increase could just depict annual fluctuation, it merits closer examination. While changes in healthcare seeking attitudes through in-migration from urban areas to our study communities in the first year of the pandemic could be a possible explanation, stratification suggests that prevalence tended to be higher before lockdown, coinciding with when the intervention achieved its highest exposure. Preliminary findings from our qualitative work suggest that CHW saw their principal role in incentivizing healthcare utilization and some went over and beyond their roles to actively coordinate and accompany women to facilities, pointing towards a real change.
Impact of Covid-19
The Covid-19 pandemic and associated lockdown affected roll-out of trainings and required adapting the study design. Most facilities suspended routine services and travel restrictions were common.11 Indeed, 53% of women with children born between March and November 2020 reported having problems accessing ANC due to Covid-19 (data not shown), explaining the observed tendency for reduced healthcare utilization after onset of lockdown. Given this, the observed overall increases in facility births and early newborn check-ups are even more meaningful.
Coverage of ENC practices was similar before and after onset of lockdown in the follow-up census at year 2, which would be expected as ENC are mostly behaviour-related and therefore unlikely directly impacted by the lockdown. This is supported by the fact that only 4% of women reported that Covid-19 changed the way they breastfed. Lastly, stratification showed that CHW largely continued their home visits during lockdown, in line with previously reported supervisor-based activity data, promoting ENC practices and distributing clean delivery kit.11
Limitations of the study design
We conducted a before-and-after study without control group, and as such, the results need to be interpreted with caution. While unmeasured secular trends and other external factors can explain changes in uncontrolled studies,73 observed improvements in our study were so extensive that we consider explanations other than intervention effect very unlikely. We adjusted for education as an important known confounder and systematically examined and adjusted all outcomes for other factors with a potential confounding effect; however, confounding seemed not an issue in our study. We are not aware of any relevant co-interventions during the study period besides the national programme Cuna-Más,74 targeting child development through home visits to families with children under three years but only achieving a coverage of 9% as per our last census; and the programme JUNTOS, which could have only impacted ANC contacts which are targeted by monetary incentives.75
Indicators used to measure ENC practices have important limitations in validity as they are solely based on maternal self-report.76, 77, 78, 79, 80 We developed the questionnaires and ENC indicators as rigorously as possible, based on face-to-face interviews and pilot surveys in the target population to test comprehension and carry out cultural adaptation13,28; however, we cannot discard desirability bias causing upward inflation of estimates. Nevertheless, we believe that substantial and consistent improvements in primary outcomes in combination with good implementation strength suggest real changes that are unlikely related to factors other than the intervention itself. However, inherent limitations of the study design still warrant a rigorous appraisal of the underlying mechanisms of change and contextual factors to understand how the intervention worked and generate further evidence for plausibility of effect.
Implications for practice
Rooted in persisting socioeconomic and geographic inequalities and exacerbated by the Covid-19 pandemic, worldwide inflation, and recent political instability, Peru currently faces an unprecedented social crisis. The Mamás del Río intervention targeted one of the poorest, hardest-to-reach, and most underserved regions—the Peruvian Amazon. Our evaluation fills an important knowledge gap in Peru as for the first time we demonstrate that a community approach based on CHW and TBA appears to be effective at improving behaviour-related birth and newborn care outcomes, which should encourage policy makers to incorporate community-based approaches as part of the maternal-neonatal health strategy in similar settings. Activity of CHW volunteers largely continued during the Covid-19 pandemic, reinforcing the importance of community-based approaches as an integral part of the health system and their strengths during major health crisis.81, 82, 83
To confirm the findings of this study and to understand transferability to other settings in Peru as well as sustainability over longer periods of time, mechanisms of change and contextual factors need to be investigated. Key topics for the upcoming qualitative process evaluation are the role of male CHW in a maternal-neonatal health intervention, sustainability of volunteer CHW, and acceptability of ENC practices by TBA and mothers of newborns. Furthermore, while there is evidence linking ENC to reductions in neonatal mortality,13 survival gains associated with the observed improvements seen in our study remain to be quantified.
Conclusions
A community-based approach for behaviour-change in home-based newborn care appears effective in the Amazon setting. Targeted ENC practices in home births improved consistently and changes were sustained over time, despite the onset of an unprecedented pandemic. Detailed process evaluation of mechanisms will examine the link between intervention and observed effects, understand generalizability to other settings, and generate insights for the Peruvian CHW programme.
Contributors
MBB and SR are the lead authors of the manuscript. SR conducted the literature search. SR, CR, and MBB conceived the study and all authors contributed to the study design. SR, AA, and MBB supervised data collection. SR analysed data and MBB verified underlying data. MBB acquired funding for the project. All authors had access to all study data at all times. All authors critically reviewed and gave final approval for publication.
Data sharing statement
De-identified data is available from the corresponding author upon request.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
The authors have no conflicts of interest to declare.
Acknowledgements
The authors would like to thank all CHWs and TBAs for their time and effort to improve the health of their communities.
Footnotes
Translation: For the Spanish translation of the abstract see Supplementary Materials section.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2023.100634.
Appendix A. Supplementary data
References
- 1.United Nations Inter-agency Group for Child Mortality Estimation (UNIGME) 2021. Levels and trends in child mortality.https://cdn.who.int/media/docs/default-source/mca-documents/rmncah/unicef-2021-child-mortality-report.pdf URL: [Google Scholar]
- 2.United Nations Inter-agency Group for Child Mortality Estimation (UNIGME) 2020. Neonatal mortality rate for Peru.https://childmortality.org/data/Peru URL: [Google Scholar]
- 3.UNICEF. Countdown to 2030 . 2022. Women's, children's & adolescents' health. The countdown country profile: a tool for action.https://data.unicef.org/countdown-2030/country/Peru/1/ Peru. URL: [Google Scholar]
- 4.Dickson K.E., Simen-Kapeu A., Kinney M.V., et al. Every newborn: health-systems bottlenecks and strategies to accelerate scale-up in countries. Lancet. 2014;384(9941):438–454. doi: 10.1016/S0140-6736(14)60582-1. [DOI] [PubMed] [Google Scholar]
- 5.Huicho L., Huayanay-Espinoza C.A., Herrera-Perez E., et al. Examining national and district-level trends in neonatal health in Peru through an equity lens: a success story driven by political will and societal advocacy. BMC Public Health. 2016;16(Suppl 2):796. doi: 10.1186/s12889-016-3405-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huicho L., Segura E.R., Huayanay-Espinoza C.A., et al. Child health and nutrition in Peru within an antipoverty political agenda: a countdown to 2015 country case study. Lancet Global Health. 2016;4(6):e414–e426. doi: 10.1016/S2214-109X(16)00085-1. [DOI] [PubMed] [Google Scholar]
- 7.WHO. PAHO/WHO . World Health Organization; 2015; Geneva: 2015. Partnership for maternal, newborn & child health, world bank and alliance for health policy and systems research. Success factors for women's and children's health: Peru. [Google Scholar]
- 8.INEI . Instituto Nacional de Estadística e Informática (INEI); Lima, Diciembre de: 2018. III Censo de Comunidades nativas 2017. Resultados definitivos. Tomo 1. Instituto Nacional de Estadistica e Informatica.https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1598/TOMO_01.pdf URL: [Google Scholar]
- 9.Ministerio de Salud (MINSA) 2013. Ministerio de Salud, Dirección General de Epidemiología. Mortalidad Neonatal en el Peru y sus departamentos 2011-2012.http://www.dge.gob.pe/portal/docs/Mortalidad_neonatal11_12.pdf Lima, Peru. URL: [Google Scholar]
- 10.Warren J., Lambert W., Fu R., Anderson J., Edelman A. Global neonatal and perinatal mortality: a review and case study for the Loreto Province of Peru. Dove Medical Press. 2012;2012(2):103–113. [Google Scholar]
- 11.Reinders S., Alva A., Huicho L., Blas M.M. Indigenous communities' responses to the COVID-19 pandemic and consequences for maternal and neonatal health in remote Peruvian Amazon: a qualitative study based on routine programme supervision. BMJ Open. 2020;10(12) doi: 10.1136/bmjopen-2020-044197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Del Mastro N.I., Tejada-Llacsa P.J., Reinders S., et al. Home birth preference, childbirth, and newborn care practices in rural Peruvian Amazon. PLoS One. 2021;16(5) doi: 10.1371/journal.pone.0250702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reinders S., Blas M.M., Neuman M., Huicho L., Ronsmans C. Prevalence of essential newborn care in home and facility births in the Peruvian Amazon: analysis of census data from programme evaluation in three remote districts of the Loreto region. Lancet Reg Health Am. 2023;18 doi: 10.1016/j.lana.2022.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mason E., McDougall L., Lawn J.E., et al. From evidence to action to deliver a healthy start for the next generation. Lancet. 2014;384(9941):455–467. doi: 10.1016/S0140-6736(14)60750-9. [DOI] [PubMed] [Google Scholar]
- 15.Darmstadt G.L., Bhutta Z.A., Cousens S., et al. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365(9463):977–988. doi: 10.1016/S0140-6736(05)71088-6. [DOI] [PubMed] [Google Scholar]
- 16.Liu L., Oza S., Hogan D., et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388(10063):3027–3035. doi: 10.1016/S0140-6736(16)31593-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanson C., Kujala S., Waiswa P., Marchant T., Schellenberg J. Community-based approaches for neonatal survival: meta-analyses of randomized trial data. Bull World Health Organ. 2017;95(6):453–464C. doi: 10.2471/BLT.16.175844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gogia S., Sachdev H.P. Home-based neonatal care by community health workers for preventing mortality in neonates in low- and middle-income countries: a systematic review. J Perinatol. 2016;36(Suppl 1):S55–S73. doi: 10.1038/jp.2016.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Craig P., Dieppe P., Macintyre S., et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kok M.C., Dieleman M., Taegtmeyer M., et al. Which intervention design factors influence performance of community health workers in low- and middle-income countries? A systematic review. Health Pol Plann. 2015;30(9):1207–1227. doi: 10.1093/heapol/czu126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kok M.C., Kane S.S., Tulloch O., et al. How does context influence performance of community health workers in low- and middle-income countries? Evidence from the literature. Health Res Pol Syst. 2015;13:13. doi: 10.1186/s12961-015-0001-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glenton C., Colvin C.J., Carlsen B., et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Syst Rev. 2013;2013(10) doi: 10.1002/14651858.CD010414.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.ESAN. Escuela de Administracion de Negocios para Graduados . 1985. Problematica de organizacion y gestion en atencion primaria de salud.https://www.grade.org.pe/en/publicaciones/13266-problematica-de-organizacion-y-gestion-en-atencion-primaria-de-salud/ URL: [Google Scholar]
- 24.Huicho L., Davila M., Gonzales F., Drasbek C., Bryce J., Victora C.G. Implementation of the integrated management of childhood Illness strategy in Peru and its association with health indicators: an ecological analysis. Health Pol Plann. 2005;20(Suppl 1):i32–i41. doi: 10.1093/heapol/czi052. [DOI] [PubMed] [Google Scholar]
- 25.Huicho L., Davila M., Campos M., Drasbek C., Bryce J., Victora C.G. Scaling up integrated management of childhood illness to the national level: achievements and challenges in Peru. Health Pol Plann. 2005;20(1):14–24. doi: 10.1093/heapol/czi002. [DOI] [PubMed] [Google Scholar]
- 26.MINSA-USAID . La Experiencia del PCMI. Programa de Capacitacion Materno Infantil; 2001. Ministerio de Salud (MINSA), USAID. Proyecto 2000.https://www.gob.pe/institucion/minsa/informes-publicaciones/353908-la-experiencia-del-pcmi-programa-de-capacitacion-materno-infantil ULR: [Google Scholar]
- 27.Congreso-Peru . Proyecto de Ley No 6130/2020-CR; 2020. Ley que fortalece la labor de los agentes comunitarios de salud como personal de la primera linea a nivel naciona, priorizando, a las regiones andino-amazonicas.http://www.leyes.congreso.gob.pe/Documentos/2016_2021/Proyectos_de_Ley_y_de_Resoluciones_Legislativas/PL06130-20200904.pdf URL: [Google Scholar]
- 28.Reinders S., Blas M.M., Lange I.L., Ronsmans C. London School of Hygiene & Tropical Medicine; London: 2021. Study protocol: evaluation of the Mamás del Río programme - a community-based, maternal and neonatal health intervention in Rural Amazonian Peru. Report No.: 10.17037/PUBS.04661899. [Google Scholar]
- 29.WHO . 2015. Caring for the newborn at home. Caring for newborns and children in the community. [Google Scholar]
- 30.Ministerio de Salud Peru . Ministerio de Salud, Dirección General de Promoción de la Salud; Lima, Peru: 2009. Documento técnico: preparando al agente comunitario de salud para el cuidado integral de la salud y nutrición de las gestantes y de las niñas y niños menores de 5 años. El manual del agente comunitario de salud; p. 174. [Google Scholar]
- 31.Limaye N.P., Rivas-Nieto A.C., Carcamo C.P., Blas M.M. Nuestras Historias- designing a novel digital story intervention through participatory methods to improve maternal and child health in the Peruvian Amazon. PLoS One. 2018;13(11) doi: 10.1371/journal.pone.0205673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gabrysch S., Civitelli G., Edmond K.M., et al. New signal functions to measure the ability of health facilities to provide routine and emergency newborn care. PLoS Med. 2012;9(11) doi: 10.1371/journal.pmed.1001340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.WHO . 2010. Essential newborn care course.http://www.who.int/maternal_child_adolescent/documents/newborncare_course/en/ URL: [Google Scholar]
- 34.MINSA . 2007. Ministerio de Salud. Dirección general de Salud de las Personas. Guía técnica: guÍAS de práctica clínica para la atención del recién nacido.http://bvs.minsa.gob.pe/local/minsa/1027_dgsp198.pdf URL: [Google Scholar]
- 35.Instituto Nacional de Estadística e Informática (INEI) INEI; Lima-Perú: 2021. Encuesta demográfica y de salud familiar (ENDES) 2020.https://proyectos.inei.gob.pe/endes/2020/INFORME_PRINCIPAL_2020/INFORME_PRINCIPAL_ENDES_2020.pdf URL: [Google Scholar]
- 36.WHO. World Health Organization . 2016. WHO recommendations on antenatal care for a positive pregnancy experience.https://www.who.int/publications/i/item/9789241549912 URL: [PubMed] [Google Scholar]
- 37.MINSA . Ministerio de Salud Peru (MINSA); 2014. Norma técnica de salud para la atención integral de salud materna. NTS N° 105 - minsa/dgsp.V.01.http://bvs.minsa.gob.pe/local/minsa/3281.pdfftp://ftp.minsa.gob.pe/sismed/ftp_carga/KIT_PROGRAMAS_PRESUPUESTALES/PP_PROPORCIONADOS_POR_OGPPM/Revisi%F3n%20PF%20de%20PP%202018/Normatividad%20de%20las%20intervenciones%20sanitarias%20MINSA-DGIESP%2010-08-18/NORMAS%20DESARE/NT%20Salud%20Materna%20precisada%20por%20RM%20159%202014.doc Available from: [Google Scholar]
- 38.StataCorp . StataCorp LLC. Svy — The survey prefix command; College Station, TX: 2021. Stata: release 17. Statistical software. [Google Scholar]
- 39.Bottomley C., Kirby M.J., Lindsay S.W., Alexander N. Can the buck always be passed to the highest level of clustering? BMC Med Res Methodol. 2016;16:29. doi: 10.1186/s12874-016-0127-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wolter K.M. 2nd ed. Springer; New York: 2007. Introduction to variance estimation. [Google Scholar]
- 41.Gabrysch S., Campbell O.M. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009;9:34. doi: 10.1186/1471-2393-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Simkhada B., Teijlingen E.R., Porter M., Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2008;61(3):244–260. doi: 10.1111/j.1365-2648.2007.04532.x. [DOI] [PubMed] [Google Scholar]
- 43.Norton E.C., Miller M.M., Kleinman L.C. Computing adjusted risk ratios and risk differences in Stata. STATA J. 2013;13(3):492–509. [Google Scholar]
- 44.Kirkwood B.R., Manu A., ten Asbroek A.H., et al. Effect of the Newhints home-visits intervention on neonatal mortality rate and care practices in Ghana: a cluster randomised controlled trial. Lancet. 2013;381(9884):2184–2192. doi: 10.1016/S0140-6736(13)60095-1. [DOI] [PubMed] [Google Scholar]
- 45.Baqui A.H., El-Arifeen S., Darmstadt G.L., et al. Effect of community-based newborn-care intervention package implemented through two service-delivery strategies in Sylhet district, Bangladesh: a cluster-randomised controlled trial. Lancet. 2008;371(9628):1936–1944. doi: 10.1016/S0140-6736(08)60835-1. [DOI] [PubMed] [Google Scholar]
- 46.Kumar V., Mohanty S., Kumar A., et al. Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet. 2008;372(9644):1151–1162. doi: 10.1016/S0140-6736(08)61483-X. [DOI] [PubMed] [Google Scholar]
- 47.Bhutta Z.A., Soofi S., Cousens S., et al. Improvement of perinatal and newborn care in rural Pakistan through community-based strategies: a cluster-randomised effectiveness trial. Lancet. 2011;377(9763):403–412. doi: 10.1016/S0140-6736(10)62274-X. [DOI] [PubMed] [Google Scholar]
- 48.Bhandari N., Mazumder S., Taneja S., Sommerfelt H., Strand T.A., Group I.E.S. Effect of implementation of Integrated Management of Neonatal and Childhood Illness (IMNCI) programme on neonatal and infant mortality: cluster randomised controlled trial. BMJ. 2012;344:e1634. doi: 10.1136/bmj.e1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Waiswa P., Pariyo G., Kallander K., et al. Effect of the Uganda Newborn Study on care-seeking and care practices: a cluster-randomised controlled trial. Glob Health Action. 2015;8 doi: 10.3402/gha.v8.24584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hanson C., Manzi F., Mkumbo E., et al. Effectiveness of a home-based counselling strategy on neonatal care and survival: a cluster-randomised trial in six districts of rural Southern Tanzania. PLoS Med. 2015;12(9) doi: 10.1371/journal.pmed.1001881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Darmstadt G.L., Choi Y., Arifeen S.E., et al. Evaluation of a cluster-randomized controlled trial of a package of community-based maternal and newborn interventions in Mirzapur, Bangladesh. PLoS One. 2010;5(3) doi: 10.1371/journal.pone.0009696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Baqui A., Williams E.K., Rosecrans A.M., et al. Impact of an integrated nutrition and health programme on neonatal mortality in rural northern India. Bull World Health Organ. 2008;86(10):796–804. doi: 10.2471/BLT.07.042226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hodgins S., McPherson R., Suvedi B.K., et al. Testing a scalable community-based approach to improve maternal and neonatal health in rural Nepal. J Perinatol. 2010;30(6):388–395. doi: 10.1038/jp.2009.181. [DOI] [PubMed] [Google Scholar]
- 54.McPherson R.A., Khadka N., Moore J.M., Sharma M. Are birth-preparedness programmes effective? Results from a field trial in Siraha district, Nepal. J Health Popul Nutr. 2006;24(4):479–488. [PMC free article] [PubMed] [Google Scholar]
- 55.Callaghan-Koru J.A., Nonyane B.A., Guenther T., et al. Contribution of community-based newborn health promotion to reducing inequities in healthy newborn care practices and knowledge: evidence of improvement from a three-district pilot program in Malawi. BMC Public Health. 2013;13:1052. doi: 10.1186/1471-2458-13-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bhutta Z.A., Memon Z.A., Soofi S., Salat M.S., Cousens S., Martines J. Implementing community-based perinatal care: results from a pilot study in rural Pakistan. Bull World Health Organ. 2008;86(6):452–459. doi: 10.2471/BLT.07.045849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Memon Z.A., Khan G.N., Soofi S.B., Baig I.Y., Bhutta Z.A. Impact of a community-based perinatal and newborn preventive care package on perinatal and neonatal mortality in a remote mountainous district in Northern Pakistan. BMC Pregnancy Childbirth. 2015;15:106. doi: 10.1186/s12884-015-0538-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Callaghan-Koru J.A., Estifanos A.S., Sheferaw E.D., et al. Practice of skin-to-skin contact, exclusive breastfeeding and other newborn care interventions in Ethiopia following promotion by facility and community health workers: results from a prospective outcome evaluation. Acta Paediatr. 2016;105(12):e568–e576. doi: 10.1111/apa.13597. [DOI] [PubMed] [Google Scholar]
- 59.Steege R., Taegtmeyer M., McCollum R., et al. How do gender relations affect the working lives of close to community health service providers? Empirical research, a review and conceptual framework. Soc Sci Med. 2018;209:1–13. doi: 10.1016/j.socscimed.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 60.Edmond K.M., Yousufi K., Anwari Z., et al. Can community health worker home visiting improve care-seeking and maternal and newborn care practices in fragile states such as Afghanistan? A population-based intervention study. BMC Med. 2018;16(1):106. doi: 10.1186/s12916-018-1092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nkonki L., Cliff J., Sanders D. Lay health worker attrition: important but often ignored. Bull World Health Organ. 2011;89(12):919–923. doi: 10.2471/BLT.11.087825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.de Vries D.H., Pool R. The influence of community health resources on effectiveness and sustainability of community and lay health worker programs in lower-income countries: a systematic review. PLoS One. 2017;12(1) doi: 10.1371/journal.pone.0170217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.MINSA . Resolucion Ministerial No411 - 2014/MINSA; 2014. Orientaciones para el fortalecimiento de labor del agente comuntario en salud. Docmento technico.http://bvs.minsa.gob.pe/local/MINSA/3154.pdf URL: [Google Scholar]
- 64.WHO . 2018. WHO guideline on health policy and system support to optimize community health worker programmes.https://www.who.int/publications/i/item/9789241550369 URL: [PubMed] [Google Scholar]
- 65.WHO . 2015. World Health Organization recommendations on health promotion interventions for maternal and newborn health.https://www.who.int/publications/i/item/9789241508742 URL: [PubMed] [Google Scholar]
- 66.MacDonald M.E. In: Anthropologies of global maternal and reproductive health: from policy spaces to sites of practice. Wellcome trust-funded monographs and book chapters. Wallace L.J., MacDonald M.E., Storeng K.T., editors. 2022. The place of traditional birth attendants in global maternal health: policy retreat, ambivalence and return; pp. 95–115. Cham (CH) [PubMed] [Google Scholar]
- 67.WHO . 2005. Making pregnancy safer: the critical role of the skilled attendant. A joint statement by WHO, ICM and FIGO.https://apps.who.int/iris/bitstream/handle/10665/42955/9241591692.pdf?sequence=1&isAllowed=y URL: [Google Scholar]
- 68.MINSA. Ministerio de Salud Peru . 2009. Documento tecnico: plan estratégico nacional para la reducción de la Mortalidad materna y perinatal 2009-2015.http://bvs.minsa.gob.pe/local/DGSP/481_DGSP240.pdf Lima. URL: [Google Scholar]
- 69.Miranda J.J., Diez-Canseco F., Lema C., et al. Stated preferences of doctors for choosing a job in rural areas of Peru: a discrete choice experiment. PLoS One. 2012;7(12) doi: 10.1371/journal.pone.0050567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lee A.C., Lawn J.E., Cousens S., et al. Linking families and facilities for care at birth: what works to avert intrapartum-related deaths? Int J Gynaecol Obstet. 2009;107(Suppl 1):S65-S85–S66-S8. doi: 10.1016/j.ijgo.2009.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Camara B.S., Delamou A., Grovogui F.M., et al. Interventions to increase facility births and provision of postpartum care in sub-Saharan Africa: a scoping review. Reprod Health. 2021;18(1):16. doi: 10.1186/s12978-021-01072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Metcalfe R., Adegoke A.A. Strategies to increase facility-based skilled birth attendance in South Asia: a literature review. Int Health. 2013;5(2):96–105. doi: 10.1093/inthealth/ihs001. [DOI] [PubMed] [Google Scholar]
- 73.Habicht J.P., Victora C.G., Vaughan J.P. Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. Int J Epidemiol. 1999;28(1):10–18. doi: 10.1093/ije/28.1.10. [DOI] [PubMed] [Google Scholar]
- 74.MEF. Ministerio de Economia y Finanzas (MEF) 2016. Resultados de la evaluación de impacto del Servicio de Acompañamiento a Familias del Programa Nacional Cuna Más. Septiembre 12, 2016.https://www.mef.gob.pe/contenidos/presu_publ/ppr/eval_indep/informe_resultados_cuna_mas.pdf URL: [Google Scholar]
- 75.MIDIS . 2017. Ministerio de Desarrollo e Inclusión Social. Evaluación de Impacto del programa JUNTOS - resultados finales.http://evidencia.midis.gob.pe/wp-content/uploads/2018/05/Informe_Final_13.pdf URL: [Google Scholar]
- 76.Blanc A.K., Warren C., McCarthy K.J., Kimani J., Ndwiga C., RamaRao S. Assessing the validity of indicators of the quality of maternal and newborn health care in Kenya. J Glob Health. 2016;6(1) doi: 10.7189/jogh.06.010405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stanton C.K., Rawlins B., Drake M., et al. Measuring coverage in MNCH: testing the validity of women's self-report of key maternal and newborn health interventions during the peripartum period in Mozambique. PLoS One. 2013;8(5) doi: 10.1371/journal.pone.0060694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bhattacharya A.A., Allen E., Umar N., et al. Monitoring childbirth care in primary health facilities: a validity study in Gombe State, northeastern Nigeria. J Glob Health. 2019;9(2) doi: 10.7189/jogh.09.020411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McCarthy K.J., Blanc A.K., Warren C.E., Kimani J., Mdawida B., Ndwidga C. Can surveys of women accurately track indicators of maternal and newborn care? A validity and reliability study in Kenya. J Glob Health. 2016;6(2) doi: 10.7189/jogh.06.020502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ameen S., Siddique A.B., Peven K., et al. Survey of women's report for 33 maternal and newborn indicators: EN-BIRTH multi-country validation study. BMC Pregnancy Childbirth. 2021;21(Suppl 1):238. doi: 10.1186/s12884-020-03425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Peretz P.J., Islam N., Matiz L.A. Community health workers and covid-19 - addressing social determinants of health in times of crisis and beyond. N Engl J Med. 2020;383(19) doi: 10.1056/NEJMp2022641. [DOI] [PubMed] [Google Scholar]
- 82.Moscibrodzki P., Li J., Peeling R.W., et al. Social innovation in health: a critical but overlooked component of the COVID-19 pandemic response. BMJ. 2021;7(3):523–525. [Google Scholar]
- 83.Bezbaruah S., Wallace P., Zakoji M., Padmini Perera W., Kato M. Roles of community health workers in advancing health security and resilient health systems: emerging lessons from the COVID-19 response in the South-East Asia Region. WHO South East Asia J Public Health. 2021;10(3):41–48. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.