Abstract
Whitish hypermelanocytic flake-like lesions on scanning laser ophthalmoscopy (SLO) multicolor posterior pole imaging (PPI) can correspond to several conditions, including simple nevi or shallow choroidal melanomas, paraneoplastic fundus lesions like bilateral diffuse uveal melanocytic proliferation, or choroidal melanocytic lesions found in neurofibromatosis type 1 (NF1). We report three cases with unilateral flake-shaped choroidal lesions on SLO multicolor PPI, similar to choroidal NF1 lesions, monitored their evolution and analyzed their potential nature using multimodal imaging including SLO multicolor and classical PPI, infrared autofluorescence (IRAF), spectral-domain-optical coherence tomography (SD-OCT), enhanced-depth imaging-OCT (EDI-OCT), OCT-angiography as well as fluorescein angiography, and indocyanine green angiography (ICGA). Two oncologic patients and one healthy patient presented unilateral whitish cornflake-shaped lesions on SLO multicolor and IRAF PPI, faintly or not visible on fundus photography, hypofluorescent on the intermediate-phase ICGA, but isofluorescent on the late-phase ICGA corresponding to hyperreflective areas in the choroid immediately under the retinal pigment epithelium on SD-OCT. The lesions were nonevolutive. Multimodal imaging determined that these “nevoid” lesions were melanocytic but could not be assimilated to classical nevi, having a looser structure that allowed some indocyanine green impregnation explaining the isofluorescence on the late-phase ICGA. The lesions were similar to those described in NF1 cases and were unrelated to the oncologic status.
Keywords: Choroidal neurofibromatosis 1, indocyanine green angiography, near-infrared image, scanning laser ophthalmoscope multicolor photographs
INTRODUCTION
The presence of multiple choroidal flake-like lesions on scanning laser ophthalmoscopy (SLO) multicolor fundus picture and infrared autofluorescence (IRAF) in a patient with a history of neoplasia can be a diagnostic problem for the ophthalmologist. Paraneoplastic syndromes should be excluded, such as bilateral diffuse uveal melanocytic proliferation (BDUMP) as well as small melanomas.
Infections and noninfectious posterior uveitis could present with posterior pole lesions, although these lesions are not detected on IRAF.
Multiple choroidal lesions, better visible in Near infrared (NIR) imaging (SLO and IRAF), were also described in patients with neurofibromatosis type 1 (NF1)[1] and added as a supplementary criterion in the diagnosis of NF1 in 2021.[2] These nodules may correspond to ovoid bodies of proliferating, neoplastic Schwann cells arranged in concentric rings around axons, with choroidal melanocytic proliferations.[3] The lesions are unilateral, occupying the posterior pole, and better detected on multicolor SLO imaging and on IRAF. Indocyanine green angiography (ICGA) is another helpful imaging method as the lesions present as dark hypofluorescent spots in the posterior pole. Although these lesions are characteristic for NF1, they were described in healthy individuals by Shelsta et al. in 2012.[4] In 2020, the same group of clinicians presented another series of cases with unilateral multifocal lesions in 11 patients, from whom 10 patients had normal brain magnetic resonance imaging (MRI) and/or normal computed tomography scan (when performed), as well as no medical history. One patient had previously treated Hodgkin lymphoma. Lesions were presumed to be benign, nonprogressive choroidal lymphoid lesions.[5]
In our center, which is specialized in retinal diseases and intraocular inflammations, within 24 months, we examined three women, two with a history of neoplasia treated by chemotherapy and one healthy patient, presenting with the same imaging pattern. To our knowledge, these are the first cases who presented unilateral choroidal lesions similar to choroidal NF1 analyzed by multimodal imaging, with a history of chemotherapy due to neoplastic disease.
CASE REPORTS
Case 1
A 56-year-old woman with a history of neuroendocrine pulmonary cancer was referred to our center for asymptomatic multiple lesions in the choroid of her left eye (OS). She was treated with chemotherapy which was stopped 4 months before the consultation. The best corrected visual acuity (BCVA) was 10/10 in both eyes. Intraocular pressure was normal in both eyes. Slit-lamp (S/L) examination was unremarkable. Unilateral whitish flake-like lesions in the left fundus were identified on SLO multicolor and IRAF images [Figures 1 and 2]. Fundus examination/photographs showed barely visible hyperpigmented areas corresponding to the SLO/IRAF white flakes. Spectral-domain enhanced-depth imaging optical coherence tomography (SD-EDI-OCT) showed hyperreflective fluffy nodules immediately beneath the retinal pigment epithelium (RPE)/Bruch's complex corresponding to the flakes seen on SLO/IRAF frames [Figure 2].
Figure 1.
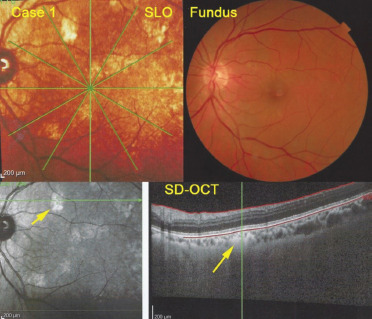
Multimodal imaging of Case 1. SLO of the left eye (top left) showing whitish hyperreflective lesions characteristic for melanocytic lesions, while on classical fundus photographs of the posterior pole hyperpigmented lesions are barely detectable (fundus, top right). On OCT, lesions appear as fluffy hyperreflective lesions just underneath the RPE-Bruch's membrane complex (yellow arrow on SD-OCT) and correspond to whitish areas on infrared frame (bottom left, yellow arrow). SLO: Scanning laser ophthalmoscopy
Figure 2.
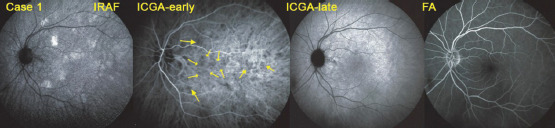
Multimodal imaging of Case 1. The lesions are well identified as whitish flakes on IRAF (left image). On the early frame of ICGA (middle left), hypofluorescent areas corresponding to the IRAF flakes are clearly seen (yellow arrows). On the late ICGA frame (middle right), these areas become isofluorescent. FA is noncontributive (right). FA: Fluorescein angiography, ICGA: Indocyanine green angiography, IRAF: Infrared autofluorescence
Fluorescein angiography (FA) was normal, while ICGA demonstrated hypofluorescent patches in the early/intermediate phase, corresponding to the SLO/IRAF flakes, which disappeared in the late angiographic phase [Figure 2].
To exclude an inflammatory/infectious etiology, blood tests were performed, including QuantiFERON Gold, syphilis serology (Treponema pallidum hemagglutination test and venereal disease research laboratory test), angiotensin-converting enzyme, and lysozyme which were normal. HLA-A29 was absent, and the cerebral MRI was normal.
After 24 months of follow-up, lesions were stable with no progression on the different imaging modalities (SLO, IRAF SD-OCT, and ICGA), and visual function was stable.
Case 2
A 50-year-old woman was addressed to our center for further examination due to unilateral whitish lesions of the right eye (OD) well identified on SLO multicolor images and IRAF [Figures 3 and 4]. She had a history of cancer of the rectum treated with chemotherapy and radiotherapy. She was asymptomatic, and BCVA was 10/10 in both eyes. S/L examination was unremarkable, and the flare was normal at 3.4 ph/ms. Lesions were well delineated on SLO multicolor fundus photographs and on IRAF as whitish hyperreflective flake-like areas corresponding to hyperreflective fluffy nodules immediately beneath the RPE/Bruch's complex on SD-EDI-OCT. These lesions were only faintly visible as discreet hyperpigmented areas on classical fundus photographs. OCT angiography was unremarkable [Figures 3 and 4].
Figure 3.
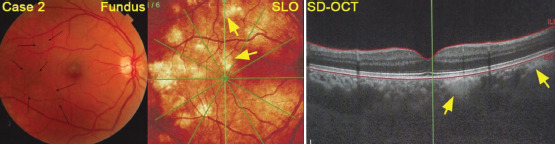
Multimodal imaging of Case 2. Classical color fundus photography of the right eye (left) showing barely visible areas of hyperpigmentation (black arrows), corresponding to the numerous whitish flake-like lesions characteristic of melanocytic lesions depicted on the SLO fundus picture (middle). On SD-EDI-OCT (right), the lesions corresponding to the SLO flakes appear as fluffy loose structures (yellow arrows). SLO: Scanning laser ophthalmoscopy, SD-EDI-OCT: Spectral-domain enhanced-depth imaging optical coherence tomography
FA was normal, while ICGA presented hypofluorescent areas in the early and intermediate phase, which corresponded to the IRAF lesions. The lesions became isofluorescent in the late stages of the ICGA. On microperimetry, the lesions did not affect the retinal sensitivity [Figure 4].
Figure 4.
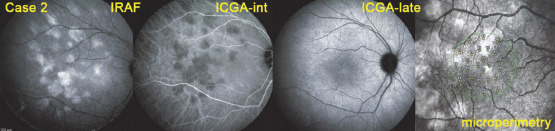
Multimodal imaging of Case 2. IRAF image of the right eye (left picture) demonstrating the whitish flake-like lesions, which are dark hypofluorescent on the intermediate-phase ICGA frame (middle left picture) and become isofluorescent on the late ICGA frame (middle right picture). Microperimetry was not affected (far right). IRAF: Infrared autofluorescence, ICGA: Indocyanine green angiography
Further workup was negative, and the situation was completely stable at 10-month follow-up.
Case 3
A 50-year-old woman was referred to our center for further investigations of asymptomatic choroidal lesions in her OS. She had no history of malignancy but presented a type 2 diabetes.
As shown in Figures 5 and 6, she presented the exact same imaging pattern as Cases 1 and 2. Therefore, no extensive investigations were performed. The situation remained stable on follow-up.
Figure 5.
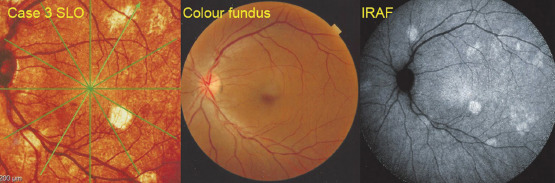
Multimodal imaging of Case 3. SLO multicolor fundus photography (left) shows the whitish hyperreflective fundus lesions characteristic of melanocytic lesions and corresponding to the lesions seen on IRAF (right), while hyperpigmentation cannot be seen on classical fundus photography. (middle). SLO: Scanning laser ophthalmoscopy, IRAF: infrared autofluorescence
Figure 6.
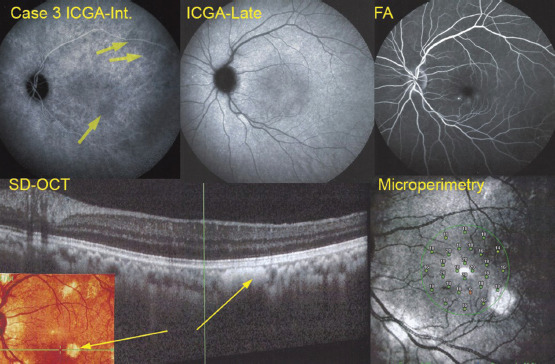
Multimodal imaging of Case 3. The SLO lesions seen on Figure 5 were faintly hypofluorescent in the intermediate phase of ICGA (top left, yellow arrows), but isofluorescent in later angiographic frames (top middle). FA was noncontributive for the pathology, but showed a few pinpoint leaks in connection with her slight diabetic maculopathy. SD-EDI-OCT showed that the flake-like lesions corresponded to fluffy loose hyperreflective nodules situated immediately under the RPE-Bruch's membrane complex. SLO: Scanning laser ophthalmoscopy, EDI: Enhanced-depth imaging, FA: Fluorescein angiography, ICGA: indocyanine green angiography RPE: Retinal pigment epithelium, SD-EDI-OCT: Spectral-domain enhanced-depth imaging optical coherence tomography
We performed in parallel a multimodal analysis of a choroidal nevus [Figure 7]. The main difference that distinguished a classical nevus from the cornflake nevoid lesions were the fact that on ICGA, the lesion remained hypofluorescent during the whole angiographic sequence in the nevus, in contrast to cornflake nevoid lesions, for which the lesion became isofluorescent on late angiographic frames [Table 1]. Second, on SD-OCT, the hyperreflective lesion underneath the RPE-Bruch's membrane complex was dense for nevi [Figure 8], while the lesions were fluffier in cornflake nevoid lesions [Figure 3].
Figure 7.
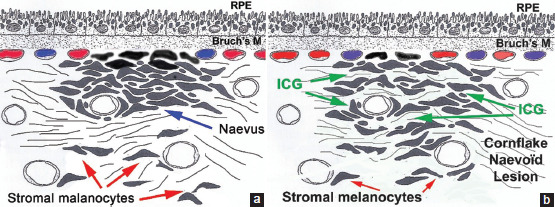
(a) Schematic representation of an inner choroidal nevus. The dense structure of the nevus does not allow infusion of the ICG molecule and remains hypofluorescent during the whole ICGA angiographic sequence. (b) Schematic representation of a cornflake nevoid lesion. Melanocytic cells are more loose and allow infusion of the ICG molecule explaining the late isofluorescence on ICGA, due to a possibly similar loose structure as described in the choroidal lesions of NF1, ICGA: Indocyanine green angiography, ICG: Indocyanine green, RPE: Retinal pigment epithelium, Bruch's M: Bruch's membrane. NF1: neurofibromatosis 1
Table 1.
Similarities and differences of the “cornflake” lesions and differential diagnosis
| Findings | IRAF | SLO-infrared | ICGA early-intermediate | ICGA late | SD-EDI-OCT | FA |
|---|---|---|---|---|---|---|
| Cornflake nevoid lesions | Whitish-hyperreflective | Whitish | Hypofluorescence/masking | Isofluorescence | Hyperreflective lesions | Normal |
| Nevi | Whitish-hyperreflective | Whitish | Hypofluorescence/masking | Hypofluorescence/masking | Hyperreflective lesion | Normal |
| Choroidal NF1 | Whitish-hyperreflective | Whitish | Hypofluorescence/masking | ? | Hyperreflective lesions | Normal |
| BDUMP | Not visible | Not visible | Hyperfluorescence/pooling | Hyperfluorescence | Thickness/subretinal fluid | Hyperfluorescence |
IRAF: Infrared autofluorescence, SLO: Scanning laser ophthalmoscopy, ICGA: Indocyanine green angiography, SD-EDI-OCT: Spectral-domain enhanced-depth imaging optical coherence tomography, FA: Fluorescein angiography, NF1: Neurofibromatosis type 1, BDUMP: Bilateral diffuse uveal melanocytic proliferation
Figure 8.
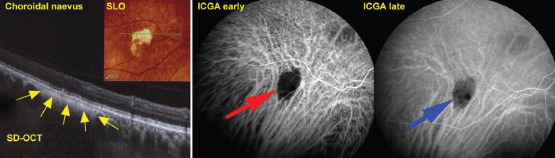
Choroidal nevus. The nevus appears as white on the SLO fundus photograph as is the case for shallow choroidal melanocytic lesions (insert of the left picture). On SD-EDI-OCT, the hyperreflective lesion situated immediately under the RPE-Bruch's membrane complex is much more compact (yellow arrows). On ICGA, the melanocytic lesion (nevus) remains hypofluorescent throughout the angiographic sequence (middle picture red arrow and right picture blue arrow). SLO: Scanning laser ophthalmoscopy, EDI: Enhanced-depth imaging, ICGA: Indocyanine green angiography, RPE: Retinal pigment epithelium, SD-EDI-OCT: Spectral-domain enhanced-depth imaging optical coherence tomography
The possible explanation for these diverse appearances in multimodal imaging analysis is the fact that classical choroidal nevi are more dense and do not allow gradual infiltration of the indocyanine green (ICG) molecule [Figure 7a], while the more loose structure of the cornflake nevoid lesion allows slow infiltration of ICG, explaining the late ICGA isofluorescence [Figure 7b].
DISCUSSION
The presence of whitish lesions on SLO multicolor fundus imaging and on IRAF characteristic of melanocytic lesions in two patients with a history of neoplasia pushed us to exclude a relation with the neoplasia, the chemotherapy, or a paraneoplastic syndrome. BDUMP was excluded because it affects the choroid with subsequent involvement of the RPE and the retina, which is visible on FA and ICGA as hyperfluorescent areas due to exudative retinal detachments and on OCT with hyporeflective areas beneath the sensory retina.[6]
Inflammatory noninfectious and infectious conditions were eliminated; thanks to broad blood test investigations. Lymphoma was also excluded as multimodal imaging was not compatible, and the cerebral MRI was normal.
Therefore, the benign character of these nonevolutive lesions could be supposed, and the presence of similar lesions in a healthy patient was another element toward benign nevus-like lesions. Using multimodal imaging, we tried to analyze the nature of these lesions, which distinguished themselves from classical nevi. Indeed, SLO, IRAF, and SD-OCT were compatible with imaging signs of a nevus. However, ICGA indicated that these “nevoid” structures were hypofluorescent on the early and intermediate frames as expected but isofluorescent on late ICGA frames. This was an indication that these melanocytic lesions were probably histologically looser than a classical nevus, allowing slow infiltration of the ICGA dye. This is supported by the fluffy loose appearance of the lesions on SD-OCT. On the contrary, in classical nevi, ICGA remains hypofluorescent until the late phase and has a more dense structure on SD-OCT.
Reviewing the literature, we found that these choroidal lesions resemble the manifestations of choroidal NF1.[1] In NF1, the origin of the lesions is due to Schwann cells arranged in concentric rings around axons with a substantial proliferation of choroidal melanocytes.[7] Their similarities on SLO and infrared imaging are astonishing, possibly because lesions could have a similar content of melanocytes in a similarly loose tissue texture as described for NF1-related choroidal lesions.[8,9,10] On ICGA, the choroidal NF1 lesion presented as hypofluorescent, but unfortunately, there was no mention of the late-phase angiographic frames. For all the three patients, NF1 could be excluded as they presented none of the diagnostic criteria (neurofibromas, café-au-lait cutaneous lesions, and Lisch nodules in iris), and they had a mean age of 52 years.
As evidenced in our third case, similar lesions can occur in patients with a normal medical history. As mentioned before, Carroll WJ et al. presented a case series of 11 patients with unilateral lesions of the choroid, which presented whitish IRAF images and hypofluorescent in ICGA.[5] Conversely to our theory, they putatively attributed these lesions to a low-grade lymphocytic process on the benign end of intraocular lymphocytic diseases, with no effect on the visual acuity nor infiltration of the vitreous nor orbit nor conjunctival, nor systemic.[5]
In conclusion, we describe a new type of benign melanocytic choroidal lesion with a flake pattern, which can be distinguished from classical choroidal nevi and which we called “cornflake nevoid” lesions. Their structure is probably less dense than classical choroidal nevi, resembling the tissue structure of choroidal lesions of NF1.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rao RC, Choudhry N. Enhanced depth imaging spectral-domain optical coherence tomography findings in choroidal neurofibromatosis. Ophthalmic Surg Lasers Imaging Retina. 2014;45:466–8. doi: 10.3928/23258160-20140818-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Legius E, Messiaen L, Wolkenstein P, Pancza P, Avery RA, Berman Y, et al. Revised diagnostic criteria for neurofibromatosis type 1 and legius syndrome: An international consensus recommendation. Genet Med. 2021;23:1506–13. doi: 10.1038/s41436-021-01170-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kurosawa A, Kurosawa H. Ovoid bodies in choroidal neurofibromatosis. Arch Ophthalmol. 1982;100:1939–41. doi: 10.1001/archopht.1982.01030040919010. [DOI] [PubMed] [Google Scholar]
- 4.Shelsta HN, Jampol LM, Weinberg DV. Indolent nonprogressive multifocal choroidal lesions. Retina. 2012;32:289–92. doi: 10.1097/IAE.0b013e318219e6e3. [DOI] [PubMed] [Google Scholar]
- 5.Carroll WJ, Deak G, J Daily M, Cunha de Souza E, Shelsta HN, Barbante Casella AM, et al. Indolent, nonprogressive, multifocal choroidal lesions: A Presumed Benign Choroidal Lymphoid Disease. Retina. 2020;40:1980–7. doi: 10.1097/IAE.0000000000002865. [DOI] [PubMed] [Google Scholar]
- 6.Jansen JC, Van Calster J, Pulido JS, Miles SL, Vile RG, Van Bergen T, et al. Early diagnosis and successful treatment of paraneoplastic melanocytic proliferation. Br J Ophthalmol. 2015;99:943–8. doi: 10.1136/bjophthalmol-2014-305893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ueda-Consolvo T, Miyakoshi A, Ozaki H, Houki S, Hayashi A. Near-infrared fundus autofluorescence-visualized melanin in the choroidal abnormalities of neurofibromatosis type 1. Clin Ophthalmol. 2012;6:1191–4. doi: 10.2147/OPTH.S35321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wolter JR, Gonzales-Sirit R, Mankin WJ. Neuro-fibromatosis of the choroid. Am J Ophthalmol. 1962;54:217–25. [PubMed] [Google Scholar]
- 9.Wolter JR. Nerve fibrils in ovoid bodies. Arch Ophthalmol. 1965;73:696–9. doi: 10.1001/archopht.1965.00970030698019. [DOI] [PubMed] [Google Scholar]
- 10.Vagge A, Capris P, Traverso CE. Choroidal abnormalities detected by Near-Infrared Imaging (NIR) in pediatric patients with neurofibromatosis type 1 (NF1) Invest Ophthalmol Vis Sci. 2016;57:774. doi: 10.1167/iovs.15-18603. [DOI] [PubMed] [Google Scholar]


