Abstract
Purpose
The purpose of this in vivo study was to compare the relative efficacy of two different chemical irrigants in achieving the same objective of bacteria decrease in deciduous teeth. The classic needle irrigation system and the EndoVac system were chemical irrigants.
Materials and methods
In this comparative study, 80 deciduous molars in patients aged 3–9 years were chosen according to the selection criteria. The teeth were divided randomly into four groups based on the irrigation system and irrigant used, namely, the group I [2.5% sodium hypochlorite (NaOCl) + conventional needle], group II (2.5% NaOCl + EndoVac), group III [2% chlorhexidine (CHX) + conventional needle], and group IV (2% CHX + EndoVac). Pre and postirrigation microbial samples were collected and transferred for microbial assay. Thereafter, pre and postoperative observations were recorded and a mean reduction of bacterial colony-forming units (CFU)/mL was obtained. The statistical analysis was then performed.
Results
In the intragroup comparison, EndoVac and the conventional system showed a statistically significant (p > 0.05) reduction in mean CFU/mL. In the intergroup comparison, EndoVac showed better results than the conventional needle irrigation system (p > 0.05). There was more reduction in CFU in 2% CHX than in 2.5% NaOCl in both the conventional needle system (p = 0.3056) and the EndoVac system (p = 0.4573), with no significant difference.
Conclusion
In this in vivo study, the efficacy of EndoVac was found to be better among all the tested groups. Around 2% CHX was found superior as compared to 2.5% NaOCl with no significant difference.
Clinical significance
The EndoVac apical negative pressure irrigant system eliminates optimum bacterial load. It significantly cleans more debris from mechanically inaccessible regions of root canals. The use of 2% CHX has shown promising results due to its property of substantivity and acceptability by children.
How to cite this article
Ahmadi M, Govil S. Conventional to EndoVac: A Comparative Evaluation of Two Irrigation Systems in Microbial Reduction of Primary Root Canals Using Chemical Irrigants: An In Vivo Study. Int J Clin Pediatr Dent 2023;16(S-2):S113–S117.
Keywords: Antibacterial efficacy, Chlorhexidine, EndoVac, Microbial reduction, Sodium hypochlorite
Introduction
Pulpal and periapical infections are caused by microorganisms. Endodontic therapy has been advocated as an effective way to eliminate microorganisms from the root canal. This is achieved by optimally cleaning, shaping, and obturating the root canals hermetically, which is the principal purpose of endodontic therapy.1
However, due complexity of the root canal system, microbial penetration into the dentinal tubules and the production of a smear layer during mechanical instrumentation of the root canals make full cleaning and shaping of the canals practically difficult.2 The use of an irrigant becomes necessary in order to thoroughly clean the root canal system.3
A good root canal irrigant should possess the properties of debris removal, breakdown of organic tissue, killing of microorganisms, elimination of microbial byproducts, and removal of smear layer.4 To attain this purpose, various chemicals and therapeutic substances have been tried. The most recommended and effective among these is NaOCl.5 NaOCl in 2.5% concentration is most widely used for irrigation in primary teeth root canals.6,7 It is an efficient tissue solvent with antibacterial properties. Its toxicity to periradicular tissues, corrosive impact on endodontic instruments, and foul odor remain a concern, particularly in children.8 CHX digluconate (2% CHX) has been suggested as an irrigant in endodontic treatment because of its antibacterial activity and lack of cytotoxicity to periradicular tissues in primary teeth.9
The most common technique in endodontics for irrigation is conventional needle irrigation. The irrigant replenishment and exchange in the apical part, lateral canal, and isthmus of the canal are inadequate.10 Additionally, positive pressure may cause postoperative discomfort as well as tissue and permanent tooth bud damage by forcing the irrigant into periradicular tissues. Thus, the conventional needle lags in providing significant quantities of irrigation fluid to the whole root canal and untouchable portions in a safe and effective manner.7
To overcome these drawbacks, newer irrigation systems have been introduced to increase the effectiveness of root canal debridement.4 The EndoVac™ system (Kerr Corp., Orange, California, United States of America) is a novel new irrigation system. It is an apical negative pressure irrigation that delivers irrigants safely to apical parts and unreachable parts of root canals.7
The study was motivated by a dearth of emphasis on irrigation in primary root canal treatment in the dentistry literature. In primary tooth root canal therapy, the impact of various irrigation solutions and delivery techniques has not been adequately studied. There are limited literature for in vivo investigations comparing the microbial reduction of standard needle irrigation and the EndoVac system on primary teeth knowledge. Therefore, this study aimed to evaluate microbial reduction with two irrigation regimens using the conventional needle irrigation method and the EndoVac system with different irrigation solutions in primary molar root canals.
Materials and Methods
This in vivo study investigated 80 deciduous posterior teeth. The study population included systemically healthy children between the ages of 3 and 9 requiring endodontic treatment. The randomly chosen patients were from the outpatient section of the Department of Pedodontics & Preventive Dentistry, Babu Banarasi Das College of Dental Sciences, Babu Banarasi Das University, Lucknow, Uttar Pradesh, India. It was approved by the institutional ethics and research committee of Babu Banarasi Das College of Dental Sciences, Babu Banarasi Das University, Lucknow, Uttar Pradesh, India. Prior to the inclusion of each child in the study, the purpose of the study was explained to their parents.
Following inclusion and exclusion criteria were used to select the teeth samples:
Inclusion Criteria
Healthy children with no systemic conditions were considered.
The primary teeth should be asymptomatic with necrotic.
The roots should be intact, or less than two-thirds of physiological root resorption should be considered.
Exclusion Criteria
Resorbing and mobile teeth with excessive root resorption.
Any patient with developmental anomalies, periodontal problems, or traumatic injuries requires pulp therapy.
Children with special healthcare needs.
Children who have received antibiotics within the last 3 months before treatment.
Teeth with periodontal pockets.
Teeth that need the operative intervention of the root canals.
Preparation Endodontic of Access Cavity
Complete oral prophylaxis of the dentition and after that, polishing with pumice was done. The tooth was isolated using a rubber dam after being injected with lignocaine containing 1:80000 adrenaline (Lignox, Warren, Mumbai, India). A high-speed air turbine with a round diamond point was used to initiate the root canal access opening, followed by the use of a low-speed engine to gain final access. An inverted cone diamond point was used to modify the cavity walls. The root canal was accessed with a size 10 K-file and the working length was determined. The contents were debrided from the canal walls using circumferential filing.
Sample Collection
Preoperative sterile paper point samples (S1) were placed in the canal for at least 60 seconds at the same level to soak up the fluid in the canal. The saturated paper points were deposited into 10 mL of thioglycolate broth and immediately transferred to the microbiology lab for microbial culture. The working length was estimated.
In all the cases, chemomechanical preparation was completed at the same appointment. Hand nickel-titanium K-files (Mani, Inc., Tochigi, Japan) were used for canal preparation to the working length in a back-and-forth alternating rotation motion using a circumferential technique up to International Organization for Standardization #25 size file. The 20 teeth designated for each group were irrigated with one of the following irrigant and irrigation systems.
Group I: Around 2.5% NaOCl irrigant using a conventional needle.
Group II: Around 2.5% NaOCl irrigant using EndoVac system.
Group III: Around 2% CHX irrigant using a conventional needle.
Group IV: Around 2% CHX irrigant using EndoVac system.
After irrigation, the postoperative paper point samples (S2) were placed for 60 seconds and immediately transferred to the microbiology lab for microbial culture.
Microbiological Processing
The preoperative (S1) and postoperative (S2) paper point samples placed in 10 mL of thioglycolate broth were vortexed in a vortex mixer (Eltek VM 301) for 1 minute. Serial dilution of the broth was done by transferring 10 mL in the first test tube and 9 mL in the rest of the 9 test tubes. These test tubes were autoclaved at 121°C/15 PSI for 15 minutes. The samples were transferred from the test tube to the blood agar media using the micropipettes. The sample test tubes were cultured at 30°C in an incubator for 24–48 hours and CFU was estimated using a microbial colony counter. The observations were laid down using the formula: CFU/mL = (number of colonies × dilution factor)/volume of culture plate and statistical analysis was performed further.
Statistical Analysis
Statistics were tabulated in a Microsoft Excel sheet under the guidance of a statistician. Statistical analysis was conducted using means and standard deviations for each group (Statistical Package for the Social Sciences (SPSS) 22.00 for Windows; SPSS Inc, Chicago, United States of America). The data were analyzed statistically using a one-way analysis of variance for each assessment point. Student t-tests were used to determine the difference between the two groups. A p-value of <0.05 was considered significant.
Result
Table 1 shows the preoperative and postoperative mean CFU of the conventional and EndoVac system. The results show that there is a decrease in the mean CFU from preoperative to postoperative values in conventional as well as EndoVac systems, with statistically significant differences between them (p < 0.05) (Figs 1 234).
Table 1.
Log CFU mean numbers of remaining bacteria among conventional system and EndoVac system
| System | Preoperative | Postoperative | Paired t-test | p-value | ||
|---|---|---|---|---|---|---|
| Mean CFU (*10 6 ) | Standard deviation | Mean CFU (*10 6 ) | Standard deviation | |||
| Conventional system | 3.93 | 0.97 | 1.72 | 0.69 | 11.37 | <0.01* |
| EndoVac system | 4.02 | 0.91 | 1.31 | 0.61 | 13.98 | <0.01* |
| Unpaired t-test | 0.49 | 3.08 | ||||
| p-value | 0.74 | 0.042* | ||||
*Statistically significant
Fig. 1.
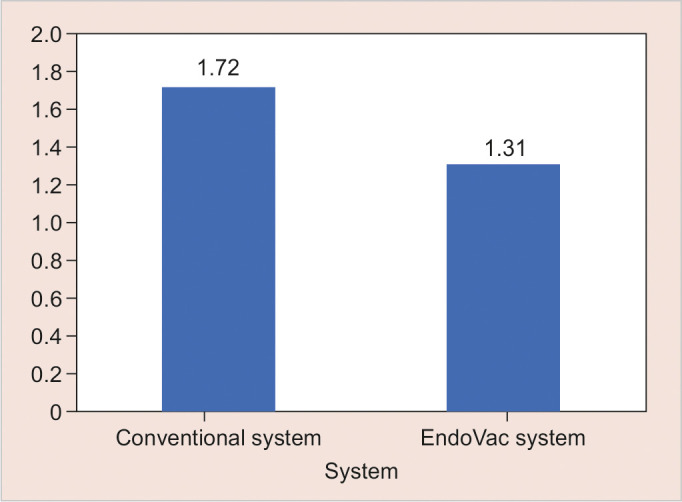
Log CFU mean numbers of remaining bacteria among conventional system and EndoVac system
Fig. 2.
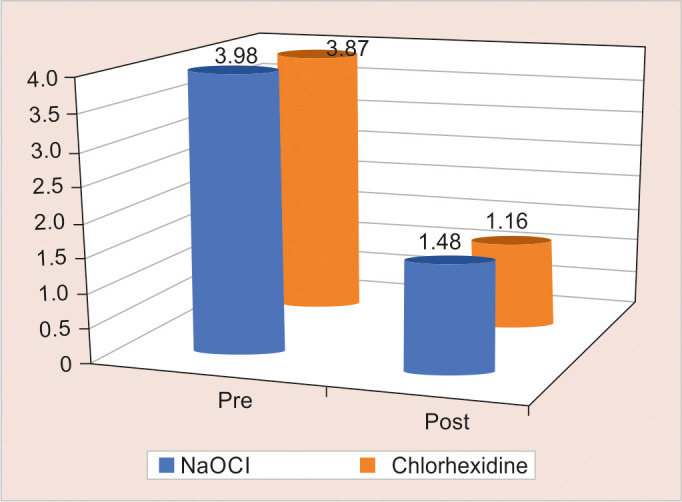
Log CFU mean numbers of remaining bacteria among various irrigants
Fig. 3.
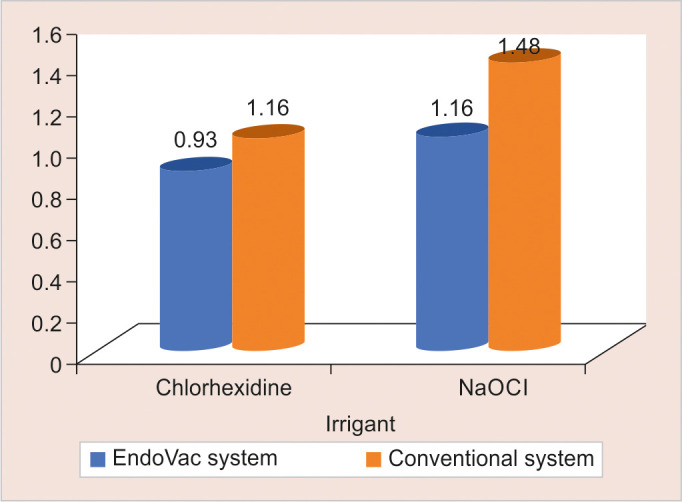
Comparison of CHX and NaOCI in different systems
Fig. 4.
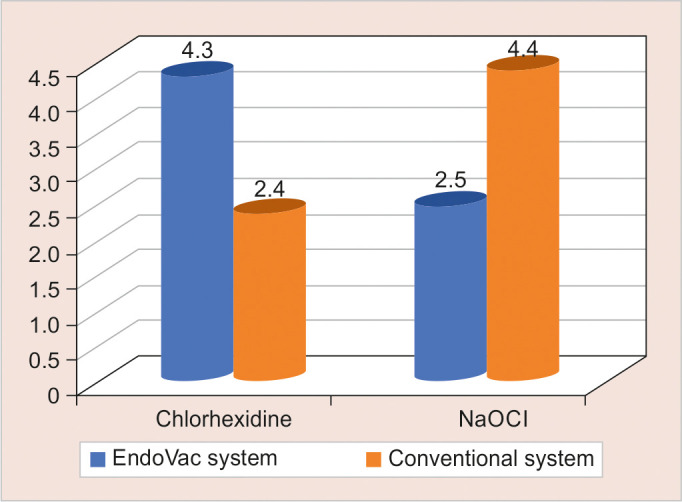
Comparison of EndoVac system and conventional system with respect to CHX and NaOCI
Table 2 shows the comparison of preoperative and postoperative efficacy of various irrigants with respect to log CFU mean numbers of remaining bacteria in the conventional system. The result shows that the mean CFU difference between the various irrigants was statistically significant, with a decrease in mean CFU from preoperative to postoperative value (p < 0.05).
Table 2.
Comparison of preoperative and postoperative efficacy of various irrigants with respect to log CFU mean numbers of remaining bacteria in the conventional system
| Irrigant | Pre | Post | t-test | p-value | ||
|---|---|---|---|---|---|---|
| Mean CFU (*106) | Standard deviation | Mean CFU (*106) | Standard deviation | |||
| NaOCI | 3.98 | 1.03 | 1.48 | 0.51 | 12.19 | <0.01* |
| CHX | 3.87 | 0.96 | 1.16 | 0.54 | 15.24 | <0.01* |
*Statistically significant
Table 3 shows the comparison between CHX and NaOCI in the conventional and EndoVac system. The results show that there was no statistically significant difference between the CHX and NaOCl group mean CFU in both systems (p > 0.05).
Table 3.
Comparison of CHX and NaOCI in different systems
| Irrigant | EndoVac system | Conventional system | ||
|---|---|---|---|---|
| Mean CFU (*106 ) | Standard deviation | Mean CFU (*10 6 ) | Standard deviation | |
| CHX | 0.93 | 0.52 | 1.16 | 0.54 |
| NaOCI | 1.16 | 0.48 | 1.48 | 0.51 |
| t-test | 2.93 | 2.97 | ||
| p-value | 0.055 | 0.052 | ||
Table 4 shows the comparison of the EndoVac system and the Conventional system with respect to CHX and NaOCI. The result shows that the mean CFU was less in the EndoVac system as compared to the conventional system in the various irrigants, with a statistically significant difference among the groups (p < 0.05).
Table 4.
Comparison of EndoVac system and conventional system with respect to CHX and NaOCI
| Irrigant | EndoVac system | Conventional system | t-test | p-value | ||
|---|---|---|---|---|---|---|
| Mean CFU (*10 6 ) | Standard deviation | Mean CFU (*106) | Standard deviation | |||
| CHX | 0.93 | 0.52 | 1.16 | 0.54 | 2.96 | 0.049* |
| NaOCI | 1.16 | 0.48 | 1.48 | 0.51 | 2.99 | 0.047* |
*Statistically significant
Discussion
Irrigation is an important step during pulpectomy. A favorable environment is needed for successful obturation and clinical success in root canal treatment.9 This can be rendered by irrigation which rids the canal system of bacteria, bacterial products, necrotic pulp tissues, and biofilms, as well as flushes the Dentinal debris.9–20
The antimicrobial effect of the EndoVac system has been examined in permanent teeth by many researchers like Cohenca et al.21 and Pawar et al.22, yet limited in vivo studies have been conducted on primary teeth. A number of studies have found that the EndoVac system is more effective at cleaning root canals than conventional irrigation or ultrasonic irrigation.4,23–25 EndoVac technology has the advantage of being able to deliver irrigant innocuously to working lengths. Clinicians must be cautious about the depth of the needle inserted to avoid any irrigant mishaps. EndoVac system can supply more irrigant till the apical third of the canal through the delivery/evacuation tip. Negative pressure delivers a steady flow of fresh irrigant to the working length while the cannulas are in the canal.4
Our study found that there was a significant difference between conventional irrigation and EndoVac 2.5% NaOCl with EndoVac and 2% CHX with EndoVac showed better results than 2.5% NaOCl and 2% CHX with the conventional needle system, respectively. In contrast, the apical negative pressure irrigation did not differ significantly from needle-and-syringe irrigation according to Pawar et al.22 In our study; it was observed that the use of EndoVac resulted in less spillage of irrigants which reduced the frequency of using suction. This enhanced the visibility of the operating field and ease of work.
A comparison between 2.5% NaOCl with EndoVac and 2% CHX with EndoVac in our study showed that the antimicrobial efficacy of 2% CHX with EndoVac was better, but there was no statistically significant difference. Miranda et al.26 compared the EndoVac system alone or in combination with photodynamic therapy and conventional system. It was as successful as conventional needle irrigation in terms of antibacterial efficacy. Nielsen et al.4 compared the efficacy of the EndoVac irrigation system and needle irrigation to debride root canals. With the EndoVac, debridement was significantly better than with needle irrigation which agrees with our findings.
The most preferred irrigant in pulp therapy universally is NaOCl. It is considered a gold standard,12 which is why it was used in the present study. It has a wide clinical range from 0.5% to 5.25%. Its optimal concentration, however, has not been determined by the literature. In primary root canal treatment, 2.5% NaOCl continuously exchanged in large volumes provides a total removal of viable bacteria in the root canal system.13
Chlorhexidine (CHX) demonstrates a broad-spectrum antimicrobial action.14 It exhibits the property of substantivity; that is, it attaches to human tissues, including dentin and releases slowly, resulting in sustained antimicrobial action.27 This highly potent antiseptic is widely used in chemical plaque control as aqueous solutions of 0.1–0.2%. However, literature on endodontics generally recommends a 2% CHX concentration for the purpose of root canal irrigation.12
Studies done previously have shown that NaOCl presents better antimicrobial activity than CHX.15,16 Also, In the studies by Elakanti et al.16 and Luddin et al.17, there was minimal or no difference in the antimicrobial efficacy of NaOCl and 2% CHX against root canal infection. A study done by Siqueira et al.18 demonstrates that CHX has better antimicrobial activity than NaOCl. In the present in vivo study, the mean CFU count of CHX is 1.16 and 0.93 with conventional and EndoVac systems, respectively. Although CHX has shown better antimicrobial efficacy than NaOCl, it was not statistically significant. This is in contradiction with previous studies like Paiva et al.19 and Salman et al.20 where they reported insignificant quantitative bacterial reduction after a final rinse with 2% CHX as compared to 2.5% NaOCl.
Conclusion
The present study demonstrates that the EndoVac system performs significantly better than the conventional needle when it comes to eliminating bacteria. Although there was a statistically significant benefit of the EndoVac system over the conventional system, they both have greatly reduced the number of bacteria in the root canal system of primary teeth with hopeful results. The study is one of a kind, where we have conducted the first in vivo study examining the antimicrobial efficacy of both the EndoVac system and conventional needle irrigation system in primary teeth. Using the EndoVac system to treat root canals in primary teeth requires more research, both in vitro and in vivo.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Buldur B, Kapdan A. Comparison of the antimicrobial efficacy of the EndoVac system and conventional needle irrigation in primary molar root canals. J Clin Pediatr Dent. 2017;41(4):284–288. doi: 10.17796/1053-4628-41.4.284. [DOI] [PubMed] [Google Scholar]
- 2.Chandwani M, Mittal R, Chandak S, et al. Effectiveness of Morinda citrifolia juice as an intracanal irrigant in deciduous molars: an in vivo study. Dent Res J (Isfahan) 2017;14(4):246–251. doi: 10.4103/1735-3327.211630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gondim JO, Avaca-Crusca JS, Valentini SR, et al. Effect of a calcium hydroxide/chlorhexidine paste as intracanal dressing in human primary teeth with necrotic pulp against Porphyromonas gingivalis and Enterococcus faecalis. Int J Paediatr Dent. 2012;22(2):116–124. doi: 10.1111/j.1365-263X.2011.01174.x. [DOI] [PubMed] [Google Scholar]
- 4.Nielsen BA, Craig Baumgartner J. Comparison of the EndoVac system to needle irrigation of root canals. J Endod. 2007;33(5):611–615. doi: 10.1016/j.joen.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 5.Siqueira JF Jr, Batista MM, Fraga RC, et al. Antibacterial effects of endodontic irrigants on black-pigmented gram-negative anaerobes and facultative bacteria. J Endod. 1998;24(6):414–416. doi: 10.1016/S0099-2399(98)80023-X. [DOI] [PubMed] [Google Scholar]
- 6.Canoglu H, Tekcicek MU, Cehreli ZC. Comparison of conventional, rotary, and ultrasonic preparation, different final irrigation regimens, and 2 sealers in primary molar root canal therapy. Pediatric dentistry. 2006;28(6):518–523. [PubMed] [Google Scholar]
- 7.Buldur B, Kapdan A. Comparison of the EndoVac system and conventional needle irrigation on removal of the smear layer in primary molar root canals. Niger J Clin Pract. 2017;20(9):1168–1174. doi: 10.4103/1119-3077.181351. [DOI] [PubMed] [Google Scholar]
- 8.Louwakul P, Prucksathamrongkul W. The effect of 2% chlorhexidine as root canal irrigant in pulpectomies of primary molars. Pediatr Dent. 2012;34(7):e192–e196. [PubMed] [Google Scholar]
- 9.Barakat I, ElPatal MA, Abushanan A, et al. Antibacterial effect of metronidazole vs chlorhexidine solutions in treatment of root canals of primary anterior teeth. J Contemp Dent Pract. 2020;21(4):396–399. [PubMed] [Google Scholar]
- 10.Wu MK, van der Sluis LW, Wesselink PR. The capability of two hand instrumentation techniques to remove the inner layer of dentine in oval canals. Int Endod J. 2003;36:218–224. doi: 10.1046/j.1365-2591.2003.00646.x. [DOI] [PubMed] [Google Scholar]
- 11.Walia V, Goswami M, Mishra S, et al. Comparative evaluation of the efficacy of chlorhexidine, sodium hypochlorite, the diode laser and saline in reducing the microbial count in primary teeth root canals - an in vivo study. J Lasers Med Sci. 2019;10(4):268–274. doi: 10.15171/jlms.2019.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siqueira Jr JF, Rôças IN, Favieri A, et al. Chemomechanical reduction of the bacterial population in the root canal after instrumentation and irrigation with 1%, 2.5%, and 5.25% sodium hypochlorite. J Endod. 2000;26(6):331–334. doi: 10.1097/00004770-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Mohammadi Z, Abbott PV. The properties and applications of chlorhexidine in endodontics. Int Endod J. 2009;42(4):288–302. doi: 10.1111/j.1365-2591.2008.01540.x. [DOI] [PubMed] [Google Scholar]
- 14.Ayhan H, Sultan N, Cirak M, et al. Antimicrobial effects of various endodontic irrigants on selected microorganisms. Int Endod J. 1999;32(2):99–102. doi: 10.1046/j.1365-2591.1999.00196.x. [DOI] [PubMed] [Google Scholar]
- 15.Ringel AM, Patterson SS, Newton CW, et al. In vivo evaluation of chlorhexidine gluconate solution and sodium hypochlorite solution as root canal irrigants. J Endod. 1982;8:200–204. doi: 10.1016/S0099-2399(82)80354-3. [DOI] [PubMed] [Google Scholar]
- 16.Elakanti S, Cherukuri G, Rao VG, et al. Comparative evaluation of antimicrobial efficacy of QMixTM 2 in 1, sodium hypochlorite, and chlorhexidine against Enterococcus faecalis and Candida albicans. J Conserv Dent. 2015;18(2):128–131. doi: 10.4103/0972-0707.153067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luddin N, Ahmed HMA. The antibacterial activity of sodium hypochlorite and chlorhexidine against Enterococcus faecalis: a review on agar diffusion and direct contact methods. J Conserv Dent. 2013;16(1):9–16. doi: 10.4103/0972-0707.105291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siqueira JF Jr, Rôças IN, Santos SRL, et al. Efficacy of instrumentation techniques and irrigation regimens in reducing the bacterial population within root canals. J Endod. 2002;28:181–184. doi: 10.1097/00004770-200203000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Paiva SS, Siqueira Jr JF, Rôças IN, et al. Supplementing the antimicrobial effects of chemo-mechanical debridement with either passive ultrasonic irrigation or a final rinse with chlorhexidine: a clinical study. J Endod. 2012;38(9):1202–1206. doi: 10.1016/j.joen.2012.06.023. [DOI] [PubMed] [Google Scholar]
- 20.Salman MI, Schütt-Gerowitt H. Comparisons among three supplementary irrigation techniques and a calcium hydroxide dressing for bacterial elimination after chemomechanical preparation using the self-adjusting file. Future Dental Journal. 2016;2(1):37–40. doi: 10.1016/j.fdj.2016.04.004. [DOI] [Google Scholar]
- 21.Cohenca N, Heilborn C, Johnson JD, et al. Apical negative pressure irrigation versus conventional irrigation plus triantibiotic intracanal dressing on root canal disinfection in dog teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(1):e42–e46. doi: 10.1016/j.tripleo.2009.08.029. [DOI] [PubMed] [Google Scholar]
- 22.Pawar R, Alqaied A, Safavi K, et al. Influence of an apical negative pressure irrigation system on bacterial elimination during endodontic therapy: a prospective randomized clinical study. J Endod. 2012;38(9):1177–1181. doi: 10.1016/j.joen.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 23.Hockett JL, Dommisch JK, Johnson JD, et al. Antimicrobial efficacy of two irrigation techniques in tapered and non-tapered canal preparations: an in vitro study. Journal of Endodontics. 2008;34(11):1374–1377. doi: 10.1016/j.joen.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 24.Gregorio C, Estevez R, Cisneros R, et al. Efficacy of different irrigation and activation systems on the penetration of sodium hypochlorite into simulated lateral canals and up to working length: an in vitro study. Journal of Endodontics. 2010;36(7):1216–1221. doi: 10.1016/j.joen.2010.02.019. [DOI] [PubMed] [Google Scholar]
- 25.Shin S, Kim H, Jung I, et al. Comparison of the cleaning efficacy of a new apical negative pressure irrigating system with conventional irrigation needles in the root canals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(3):479–484. doi: 10.1016/j.tripleo.2009.10.050. [DOI] [PubMed] [Google Scholar]
- 26.Miranda RG, Santos EB, Souto RM, et al. Ex vivo antimicrobial efficacy of the E ndo V ac® system plus photodynamic therapy associated with calcium hydroxide against intracanal E nterococcus faecalis. Int Endod J. 2013;46(6):499–505. doi: 10.1111/iej.12016. [DOI] [PubMed] [Google Scholar]
- 27.Shahsiah S, Azizi A, Moghimipour E, et al. Evaluation of tissue dissolution ability of modified chlorhexidine as a root canal irrigant. Biosci Biotech Res Com. 2017;10(2):40–48. doi: 10.21786/bbrc/10.2/7. [DOI] [Google Scholar]


