Abstract
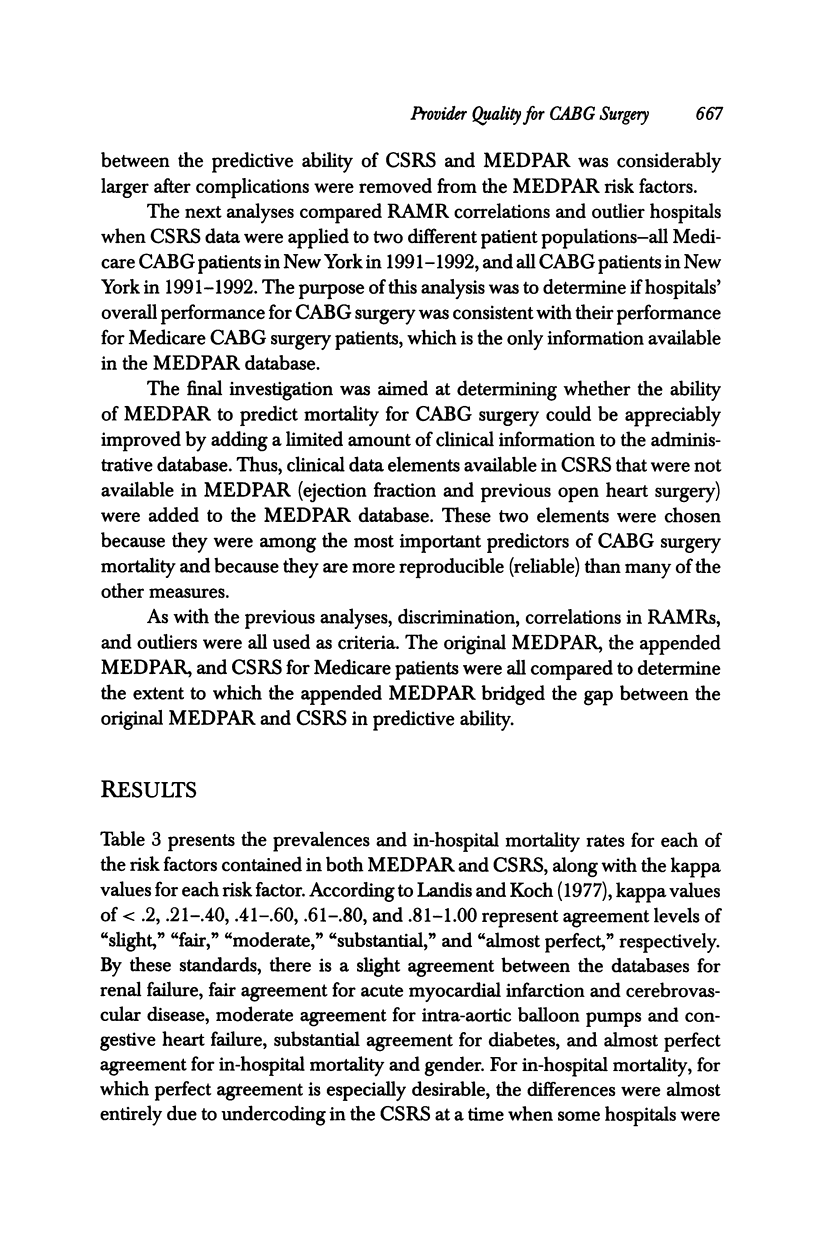
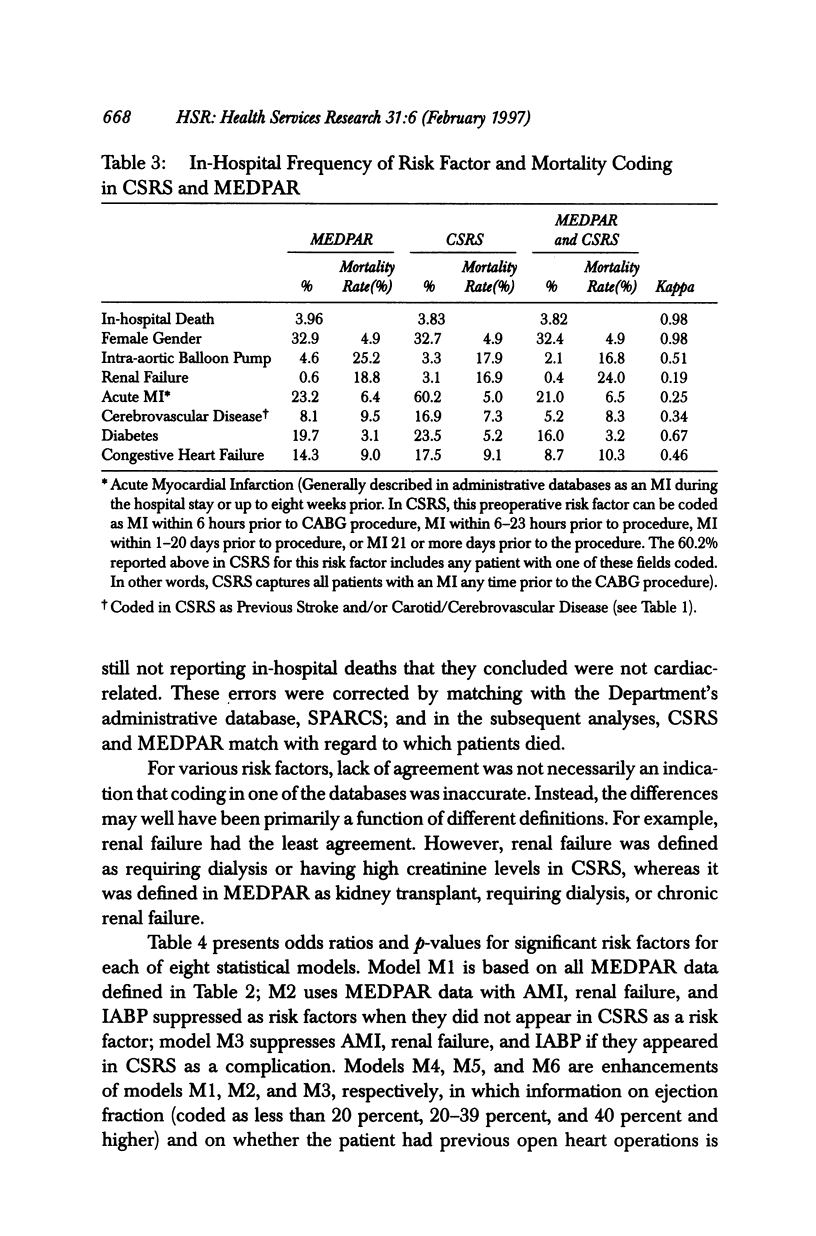
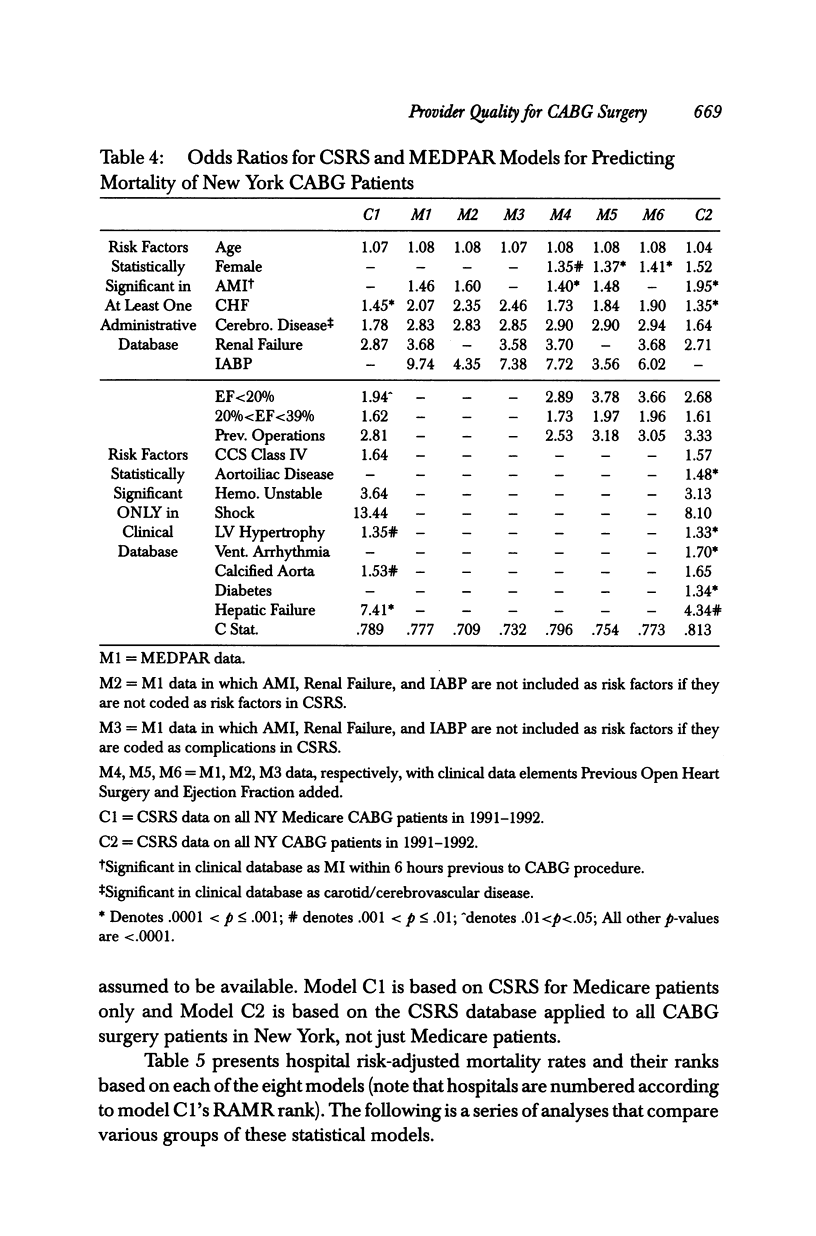
OBJECTIVES: To assess the relative abilities of clinical and administrative data to predict mortality and to assess hospital quality of care for CABG surgery patients. DATA SOURCES/STUDY SETTING: 1991-1992 data from New York's Cardiac Surgery Reporting System (clinical data) and HCFA's MEDPAR (administrative data). STUDY DESIGN/SETTING/SAMPLE: This is an observational study that identifies significant risk factors for in-hospital mortality and that risk-adjusts hospital mortality rates using these variables. Setting was all 31 hospitals in New York State in which CABG surgery was performed in 1991-1992. A total of 13,577 patients undergoing isolated CABG surgery who could be matched in the two databases made up the sample. MAIN OUTCOME MEASURES: Hospital risk-adjusted mortality rates, identification of "outlier" hospitals, and discrimination and calibration of statistical models were the main outcome measures. PRINCIPAL FINDINGS: Part of the discriminatory power of administrative statistical models resulted from the miscoding of postoperative complications as comorbidities. Removal of these complications led to deterioration in the model's C index (from C = .78 to C = .71 and C = .73). Also, provider performance assessments changed considerably when complications of care were distinguished from comorbidities. The addition of a couple of clinical data elements considerably improved the fit of administrative models. Further, a clinical model based on Medicare CABG patients yielded only three outliers, whereas eight were identified using a clinical model for all CABG patients. CONCLUSIONS: If administrative databases are used in outcomes research, (1) efforts to distinguish complications of care from comorbidities should be undertaken, (2) much more accurate assessments may be obtained by appending a limited number of clinical data elements to administrative data before assessing outcomes, and (3) Medicare data may be misleading because they do not reflect outcomes for all patients.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dubois R. W., Brook R. H., Rogers W. H. Adjusted hospital death rates: a potential screen for quality of medical care. Am J Public Health. 1987 Sep;77(9):1162–1166. doi: 10.2105/ajph.77.9.1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher E. S., Whaley F. S., Krushat W. M., Malenka D. J., Fleming C., Baron J. A., Hsia D. C. The accuracy of Medicare's hospital claims data: progress has been made, but problems remain. Am J Public Health. 1992 Feb;82(2):243–248. doi: 10.2105/ajph.82.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannan E. L., Bernard H. R., O'Donnell J. F., Kilburn H., Jr A methodology for targeting hospital cases for quality of care record reviews. Am J Public Health. 1989 Apr;79(4):430–436. doi: 10.2105/ajph.79.4.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannan E. L., Kilburn H., Jr, Lindsey M. L., Lewis R. Clinical versus administrative data bases for CABG surgery. Does it matter? Med Care. 1992 Oct;30(10):892–907. doi: 10.1097/00005650-199210000-00002. [DOI] [PubMed] [Google Scholar]
- Hannan E. L., Kilburn H., Jr, Racz M., Shields E., Chassin M. R. Improving the outcomes of coronary artery bypass surgery in New York State. JAMA. 1994 Mar 9;271(10):761–766. [PubMed] [Google Scholar]
- Hsia D. C., Krushat W. M., Fagan A. B., Tebbutt J. A., Kusserow R. P. Accuracy of diagnostic coding for Medicare patients under the prospective-payment system. N Engl J Med. 1988 Feb 11;318(6):352–355. doi: 10.1056/NEJM198802113180604. [DOI] [PubMed] [Google Scholar]
- Iezzoni L. I., Daley J., Heeren T., Foley S. M., Hughes J. S., Fisher E. S., Duncan C. C., Coffman G. A. Using administrative data to screen hospitals for high complication rates. Inquiry. 1994 Spring;31(1):40–55. [PubMed] [Google Scholar]
- Iezzoni L. I., Foley S. M., Daley J., Hughes J., Fisher E. S., Heeren T. Comorbidities, complications, and coding bias. Does the number of diagnosis codes matter in predicting in-hospital mortality? JAMA. 1992 Apr 22;267(16):2197–2203. doi: 10.1001/jama.267.16.2197. [DOI] [PubMed] [Google Scholar]
- Iezzoni L. I. Using administrative diagnostic data to assess the quality of hospital care. Pitfalls and potential of ICD-9-CM. Int J Technol Assess Health Care. 1990;6(2):272–281. doi: 10.1017/s0266462300000799. [DOI] [PubMed] [Google Scholar]
- Jollis J. G., Ancukiewicz M., DeLong E. R., Pryor D. B., Muhlbaier L. H., Mark D. B. Discordance of databases designed for claims payment versus clinical information systems. Implications for outcomes research. Ann Intern Med. 1993 Oct 15;119(8):844–850. doi: 10.7326/0003-4819-119-8-199310150-00011. [DOI] [PubMed] [Google Scholar]
- Krakauer H., Bailey R. C., Skellan K. J., Stewart J. D., Hartz A. J., Kuhn E. M., Rimm A. A. Evaluation of the HCFA model for the analysis of mortality following hospitalization. Health Serv Res. 1992 Aug;27(3):317–335. [PMC free article] [PubMed] [Google Scholar]
- Landis J. R., Koch G. G. The measurement of observer agreement for categorical data. Biometrics. 1977 Mar;33(1):159–174. [PubMed] [Google Scholar]
- O'Connor G. T., Plume S. K., Olmstead E. M., Coffin L. H., Morton J. R., Maloney C. T., Nowicki E. R., Levy D. G., Tryzelaar J. F., Hernandez F. Multivariate prediction of in-hospital mortality associated with coronary artery bypass graft surgery. Northern New England Cardiovascular Disease Study Group. Circulation. 1992 Jun;85(6):2110–2118. doi: 10.1161/01.cir.85.6.2110. [DOI] [PubMed] [Google Scholar]
- Pryor D. B., Califf R. M., Harrell F. E., Jr, Hlatky M. A., Lee K. L., Mark D. B., Rosati R. A. Clinical data bases. Accomplishments and unrealized potential. Med Care. 1985 May;23(5):623–647. doi: 10.1097/00005650-198505000-00020. [DOI] [PubMed] [Google Scholar]
- Romano P. S., Roos L. L., Luft H. S., Jollis J. G., Doliszny K. A comparison of administrative versus clinical data: coronary artery bypass surgery as an example. Ischemic Heart Disease Patient Outcomes Research Team. J Clin Epidemiol. 1994 Mar;47(3):249–260. doi: 10.1016/0895-4356(94)90006-x. [DOI] [PubMed] [Google Scholar]
- Roos L. L., Jr, Cageorge S. M., Austen E., Lohr K. N. Using computers to identify complications after surgery. Am J Public Health. 1985 Nov;75(11):1288–1295. doi: 10.2105/ajph.75.11.1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu J. V., Jaglal S. B., Naylor C. D. Multicenter validation of a risk index for mortality, intensive care unit stay, and overall hospital length of stay after cardiac surgery. Steering Committee of the Provincial Adult Cardiac Care Network of Ontario. Circulation. 1995 Feb 1;91(3):677–684. doi: 10.1161/01.cir.91.3.677. [DOI] [PubMed] [Google Scholar]


