Abstract
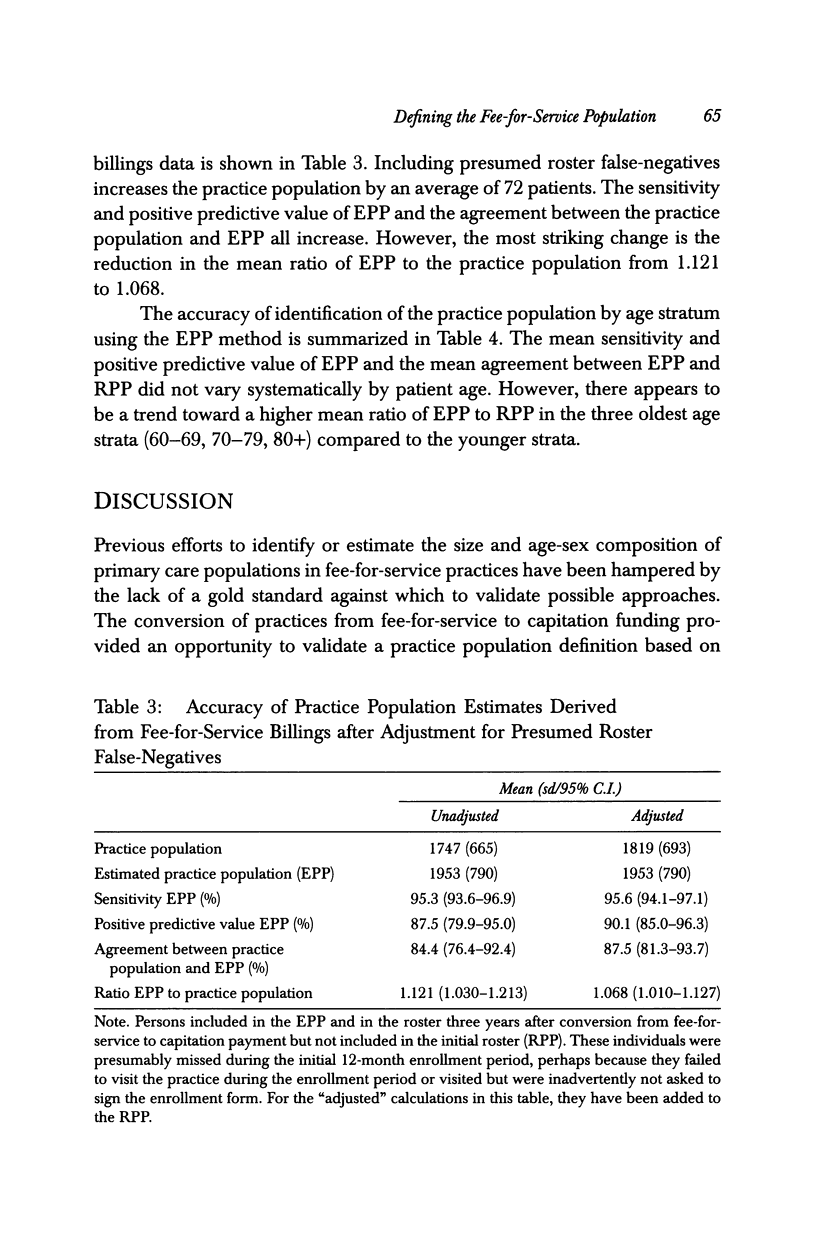
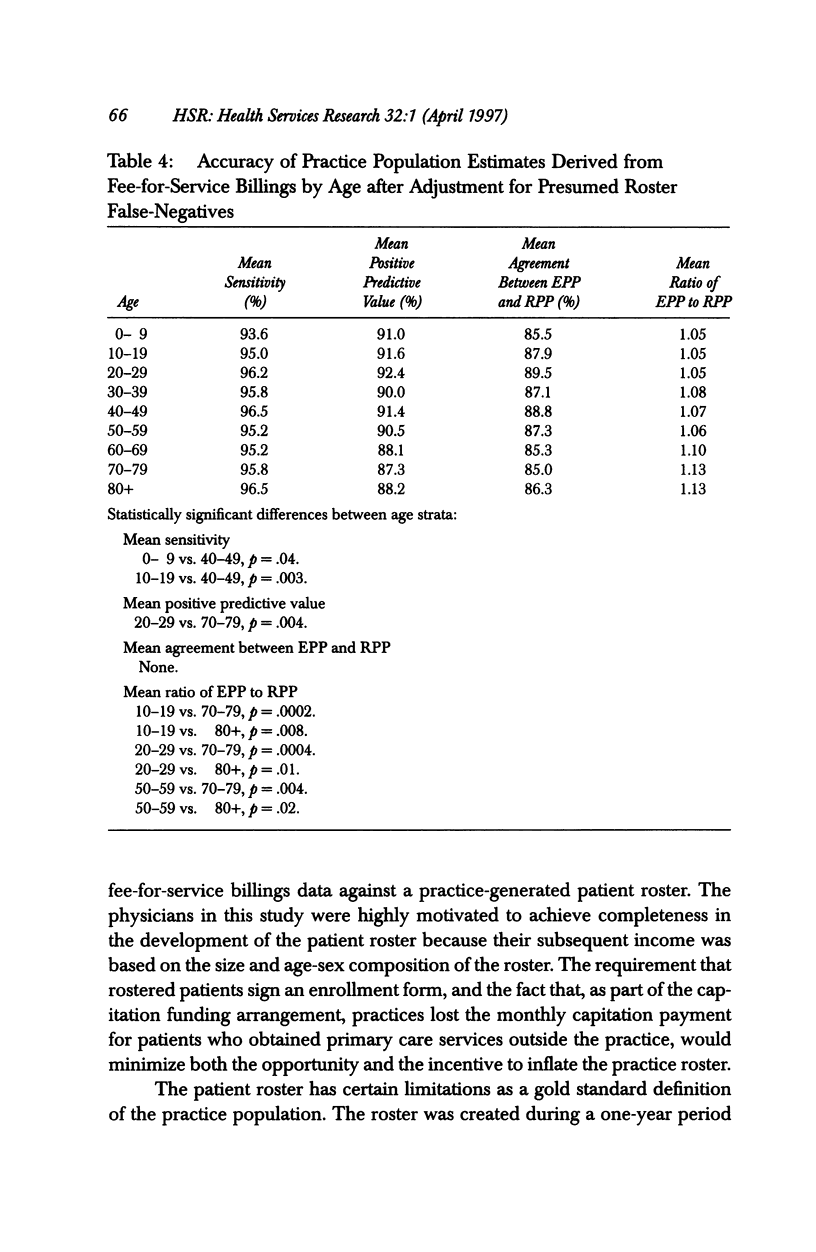
OBJECTIVE: To develop and validate a technique for defining a practice population of discrete individuals based on multiyear family practice fee-for-service billings data. DATA SOURCES/STUDY SETTING: Nineteen family physicians in Ontario, Canada who converted from fee-for-service to capitation payment. Data sources were fee-for-service billings data for the three-year period prior to the conversion from fee-for-service to capitation payment and the rosters of enrolled patients for the first and third years after the change to capitation payment. STUDY DESIGN: The billings-based definition of the physician's practice population was compared against the Year 1 roster. We also compared the billings-based practice population and the Year 1 roster to the physician's Year 3 roster to identify patients who might have been missed during the roster development process. Our principal analyses were an assessment of the sensitivity of the billings-based definition of the practice population (EPP), the positive predictive value of EPP, and the agreement between EPP and the rostered patient population (RPP). We also examined the ratio between EPP and RPP to determine EPP's accuracy in estimating the practice denominator. DATA COLLECTION/EXTRACTION METHODS: The practice population for each physician at the time of conversion from fee-for-service to capitation payment was defined as (a) all persons for whom the physician billed the provincial health insurance plan for at least one visit during the year immediately prior to joining the capitation-funded program; and (b) all additional patients for whom the physician billed the plan for at least one service in each of the two preceding years. Data extraction was carried out within the Ministry of Health in order to preserve the anonymity of patients and physicians. Data were provided to the investigators stripped of patient and physician identifiers. PRINCIPAL FINDINGS: The mean sensitivity and positive predictive value of EPP were 95.3 percent and 87.4 percent, respectively. The level of agreement between EPP and RPP averaged 84.4 percent. The mean ratio of EPP to RPP was 1.21 (95 percent C.I. 1.030-1.213). Correction for roster false-negatives increased the sensitivity, positive predictive value, and agreement between EPP and the practice population, and reduced the mean ratio of EPP to the practice population to 1.068 (95 percent C.I. 1.010-1.127). CONCLUSIONS: The practice population can usefully be defined in fee-for-service family practice on the basis of multiyear fee-for-service billings data. Further research examining alternative encounter-based practice population definitions would be valuable.
Full text
PDF










Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson J. E., Gancher W. A., Bell P. W. Validation of the patient roster in a primary care practice. Health Serv Res. 1985 Aug;20(3):301–314. [PMC free article] [PubMed] [Google Scholar]
- Anderson J. E., Willan A. R. Estimating the size of family practice populations. Quadratic Odds Estimation. Med Care. 1988 Dec;26(12):1228–1233. doi: 10.1097/00005650-198812000-00011. [DOI] [PubMed] [Google Scholar]
- Anderson J. E., Willan A. R., Gancher W. A. The negative binomial model and the denominator problem in a rural family practice. Fam Pract. 1986 Sep;3(3):174–183. doi: 10.1093/fampra/3.3.174. [DOI] [PubMed] [Google Scholar]
- Boyle R. M., Rockhold F. W., Mitchell G. S., Jr, VanHorn S. The Age/Sex Register: estimation of the practice population. J Fam Pract. 1977 Dec;5(6):999–1003. [PubMed] [Google Scholar]
- Cherkin D. C., Berg A. O., Phillips W. R. In search of a solution to the primary care denominator problem. J Fam Pract. 1982 Feb;14(2):301–309. [PubMed] [Google Scholar]
- Cherkin D. C. Learning to live without practice denominators. J Fam Pract. 1984 Oct;19(4):437–439. [PubMed] [Google Scholar]
- Cherkin D. C., Phillips W. R., Berg A. O. A method for estimating the population at risk in primary care practices by applying correction factors to the active patient census. J Fam Pract. 1984 Sep;19(3):355–363. [PubMed] [Google Scholar]
- Fraser R. C. Patient movements and the accuracy of the age--sex register. J R Coll Gen Pract. 1982;32(243):615–622. [PMC free article] [PubMed] [Google Scholar]
- Fraser R. C. The reliability and validity of the age-sex register as a population denominator in general practice. J R Coll Gen Pract. 1978 May;28(190):283–286. [PMC free article] [PubMed] [Google Scholar]
- Hannay D. R., Maddox E. J. Missing patients on a health centre file. Community Health (Bristol) 1977 May;8(4):210–216. [PubMed] [Google Scholar]
- Heward J., Clayton D. G. The point accuracy of paediatric population registers. J R Coll Gen Pract. 1980 Jul;30(216):412–416. [PMC free article] [PubMed] [Google Scholar]
- Hutchison B., Birch S., Hurley J., Lomas J., Stratford-Devai F. Do physician-payment mechanisms affect hospital utilization? A study of Health Service Organizations in Ontario. CMAJ. 1996 Mar 1;154(5):653–661. [PMC free article] [PubMed] [Google Scholar]
- Mayo F., Marsland D., Wood M., Mosteller M., Miller G. W., Johnson R. E., Munson P. J. Denominator definition by the utilization correction factor method. Fam Pract. 1986 Sep;3(3):184–191. doi: 10.1093/fampra/3.3.184. [DOI] [PubMed] [Google Scholar]
- Rose G., Barker D. J. Epidemiology for the uninitiated. Rates. Br Med J. 1978 Sep 30;2(6142):941–942. doi: 10.1136/bmj.2.6142.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B. W. The Quadratic Odds Estimation (QOE) method for calculating practice denominators. Med Care. 1988 Dec;26(12):1234–1237. doi: 10.1097/00005650-198812000-00012. [DOI] [PubMed] [Google Scholar]


