Abstract
Background:
The American Rescue Plan Act of 2021 awarded $500 million towards scaling “strike teams” to mitigate the impact of Coronavirus Disease 2019 (COVID-19) within nursing homes. The Massachusetts Nursing Facility Accountability and Support Package (NFASP) piloted one such model during the first weeks of the pandemic, providing nursing homes financial, administrative, and educational support. For a subset of nursing homes deemed high-risk, the state offered supplemental, in-person technical infection control support.
Methods:
Using state death certificate data and federal nursing home occupancy data, we examined longitudinal all-cause mortality per 100,000 residents and changes in occupancy across NFASP participants and subgroups that varied in their receipt of the supplemental intervention.
Results:
Nursing home mortality peaked in the weeks preceding the NFASP, with a steeper increase among those receiving the supplemental intervention. There were contemporaneous declines in weekly occupancy. The potential for temporal confounding and differential selection across NFASP subgroups precluded estimation of causal effects of the intervention on mortality.
Conclusions:
We offer policy and design suggestions for future strike team iterations that could inform the allocation of state and federal funding. We recommend expanded data collection infrastructure and, ideally, randomized assignment to intervention subgroups to support causal inference as strike team models are scaled under the direction of state and federal agencies.
Keywords: Nursing homes, COVID-19, strike teams, American Rescue Plan Act of 2021, older adults
Introduction
Nursing homes incurred disproportionate morbidity and mortality during the coronavirus disease 2019 (COVID-19) pandemic. During the first-wave of the pandemic, over half of all-cause deaths in Massachusetts occurred within nursing homes.1 In response, the Massachusetts Executive Office of Health and Human Services partnered with state entities and trade organizations to administer the novel Nursing Facility Accountability and Support Package (NFASP).2,3 This nine-week intervention modeled a multidomain, tiered approach to COVID-19 mitigation within nursing homes statewide. Early analysis of the NFASP demonstrated a decrease in weekly new COVID-19 infections and mortality during the intervention period, but researchers noted the difficulty of isolating intervention effects without randomization.2,3
The NFASP has served as a foundation for the ‘NFASP 2.0,’ which directs an additional $260 and $180 million in respective state and federal funding to COVID-19 mitigation within nursing homes.2 Federally, the American Rescue Plan Act of 2021 (ARPA) awarded $500 million towards the Nursing Home & Long-Term Care Facility Strike Team and Infrastructure Project to scale approaches similar to that of the NFASP.4,5 Evaluating the strengths and limitations of the strike team model is important to the informed allocation of funds to address current and future outbreaks of transmissible diseases within congregate healthcare and residential settings.
The NFASP pilot offers a unique opportunity to evaluate a potentially scalable strike team model. In this manuscript we describe the NFASP in the context of longitudinal trends in nursing home mortality and occupancy. We illustrate how features of the Massachusetts NFASP design precluded causal inference and provide recommendations about the design of future strike team iterations to improve measurement of their effects. We emphasize that impediments to causal inference were exacerbated by the fragmented nature of nursing home data collection and reporting throughout the COVID-19 pandemic.4,6 Improved state and federal data collection infrastructure has since emerged as a legislative priority for public health preparedness.7,8
Study Data and Methods
Intervention timing and domains
The NFASP is one of several examples of strike team models that originated to support nursing home emergency response during the COVID-19 pandemic.4 The strike team effort encompasses various multidisciplinary public health initiatives undertaken to reduce the adverse consequences of the pandemic within nursing homes.4 We selected the NFASP for further evaluation because of its scale and well-documented procedures. The NFASP consisted of four domains, detailed elsewhere.2,3,9 The first established a 28-item Infection Control Competency Checklist, used as a benchmark during nursing home audits.3,10 The second offered reimbursement premiums to facilities adhering to Checklist standards, financed by $130 million in state funding.3 The third centralized assistance with staffing logistics and the procurement of COVID-19 testing kits and personal protective equipment.3 The fourth involved a tiered intervention, wherein facilities were offered distinct levels of technical support based upon adherence to infection control standards, as a proxy for susceptibility to adverse COVID-related outcomes.3 At a minimum, 237 (of 360) nursing homes were offered weekly virtual educational seminars and question and answer services, herein referred to as the “Base Intervention” (BI). A subset of 123 nursing homes were determined to be at increased risk due to either historical infection control deficiencies or performance below an acceptable score threshold on NFASP audits (Supplementary Figure S1).3 These facilities completed 362 tailored on-site consultations with infection preventionists during the intervention, hereafter referred to as the “Supplemental Intervention” (SI).3
Data sources and analysis
We used data from Massachusetts Death Certificate Records from October 2018-September 2020 to link all-cause mortality to individual nursing homes. We derived daily census information (averaged by week) from the Long-Term Care Facility Staffing Payroll-Based Journal (PBJ). We multiply imputed missing staffing and census values using an expectation-maximization algorithm, which enables maximum likelihood estimation in the presence of latent variables.11,12 We used data from the Massachusetts Center for Health Information and Analytics and Centers for Medicare & Medicaid Services (CMS) Nursing Home Care Compare to obtain additional nursing home characteristics.13,14 We obtained lagged (2019) information on nursing home census composition through linkages to Long Term Care Focus (LTCFocus).15 We removed one nursing home from our sample due to incomplete data regarding daily census and staffing information; this facility was within the BI subgroup. Therefore, our analytic sample was comprised of 359 total nursing homes, with 236 facilities within the BI subgroup and 123 facilities within the SI subgroup.
We estimated weekly all-cause mortality per 100,000 nursing home residents and percent-occupancy within the SI and BI groups over four time periods. Time Period 1 (T1) spanned 16 pre-pandemic months (October 1, 2018-February 28, 2020). Time Period 2 (T2) spanned the 8-weeks following the first reported Massachusetts COVID-19 case through the NFASP announcement (February 29, 2020-April 27, 2020). Time Period 3 spanned the 9-weeks of the NFASP intervention (April 28, 2020-July 8, 2020). Time Period 4 (T4) spanned the post-intervention period until the ‘NFASP 2.0’ announcement (July 9, 2020-September 10, 2020).2
Analyses were conducted using R version 4 and the Amelia II package for multiple imputation.
RESULTS
Facilities in the SI and BI groups were comparable with respect to facility ownership, size, and operating margins (Table 1). The SI facilities, however, served a younger patient population, as indicated by both the average age of the resident census and the percentage of residents aged <65-years. SI facilities also cared for a higher percentage of residents primarily insured by Medicaid.
Table 1:
Baseline Facility Characteristics by Intervention Subgroup
| Nursing Home Characteristics (Mean, SD) | Supplemental Intervention (N=123) |
Base Intervention (N=236) |
Standardized Mean Difference |
|---|---|---|---|
| Proprietary ownership (%)a | 96 (78.0%) | 162 (68.6%) | 0.2 |
| Missing | 2 (1.6%) | 0 (0%) | |
| Number of Certified Beds (n)a | 124 (50.1) | 116 (43.0) | −0.2 |
| Missing | 2 (1.6%) | 0 (0%) | |
| Weekly RN hours per patient b | 0.4 (0.2) | 0.5 (0.3) | 0.5 |
| Missing | 0 (0%) | 0 (0%) | |
| Weekly LPN and CNA hours per patient b | 2.9 (0.4) | 3.1 (0.5) | 0.2 |
| Missing | 0 (0%) | 0 (0%) | |
| Medicaid patient-days per year (%)c | 72.0 (14.4) | 66.2 (16.8) | −0.4 |
| Missing | 2 (1.6%) | 2 (0.8%) | |
| Operating margin (%)c | −0.1 (0.1) | −0.1 (0.2) | 0.1 |
| Missing | 2 (1.6%) | 2 (0.8%) | |
| Census RUG Score d | 1.3 (0.14) | 1.3 (0.11) | 0.2 |
| Missing | 4 (3.3%) | 5 (2.1%) | |
| Proportion of Non-Hispanic White residents (%)d | 83.1 (14.9) | 84.9 (16.4) | 0.1 |
| Missing | 5 (4.1%) | 6 (2.5%) | |
| Average age of census (years) d | 78.7 (8.4) | 82.0 (6.8) | 0.4 |
| Missing | 0 (0%) | 0 (0%) | |
| Percent of census aged <65-years (%) | 25.9 (20.3) | 16.8 (15.7) | −0.5 |
| Missing | 19.3% | 19.1% |
RN: Registered Nurse
LPN: Licensed Practical Nurse
CNA: Certified Nursing Assistant
RUG: Resource Utilization Group
Nursing Home Compare 2020 Provider Information
CMS Payroll-Based Journal
Massachusetts Center for Health Information and Analytics 2020 Nursing Home Cost Reports
Long Term Care Focus 2019
Notes: The exhibit displays the facility characteristics for nursing homes within the Base Intervention and Supplemental Intervention groups within the Nursing Facility Accountability and Support Package (NFASP). Staffing measures were derived from the Centers for Medicare & Medicaid Services (CMS) Payroll-Based Journal. Information regarding Medicaid payer-mix and operating margin were derived from the Massachusetts Center for Health Information and Analytics 2020 Nursing Home Cost Reports. Information regarding facility ownership and size (number of certified beds) was derived from CMS Nursing Home Compare. Lagged (2019) information regarding the age and racial and ethnic composition and complexity of residents was derived from the Long-Term Care Focus dataset.
Figure 1 displays the all-cause mortality rate between September 2018 through September 2020 per 100,000 statewide nursing home residents, and per 100,000 Massachusetts residents whose deaths occurred outside of a nursing home. The all-cause mortality rate within nursing homes exceeded that within other settings throughout the observation period. Statewide nursing home mortality peaked in April 2020, following a regional COVID-19 outbreak and prior to the announcement of the NFASP. Before February 2020 SI facilities experienced a lower mortality rate than BI facilities, followed by a steeper increase in all-cause mortality beginning in March 2020. Mortality reached its lowest point statewide in July 2020, coinciding with a local minimum in COVID-19 infections and the conclusion of the NFASP intervention.
Figure 1. Trends in All-Cause Mortality within Nursing Facility Accountability and Support Package Subgroups.
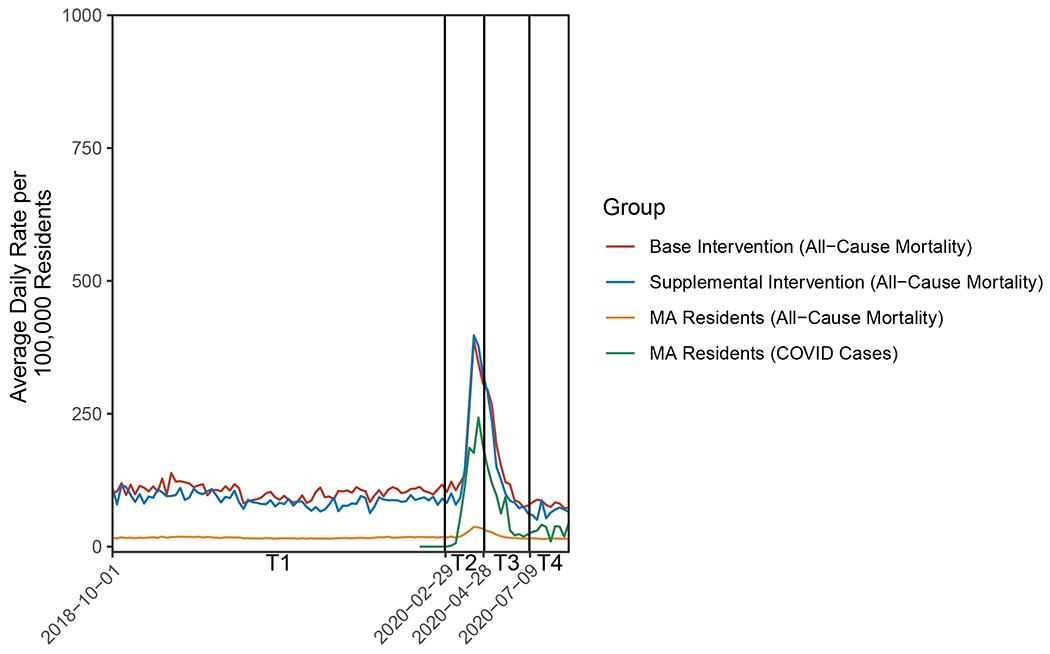
Notes: The exhibit displays all-cause mortality per 100,000 nursing home residents within the Base Intervention (SI) and Supplemental Intervention (SI) groups of the Nursing Home Facility Accountability and Support Package (NFASP). The trend in all-cause mortality per 100,000 Massachusetts residents not residing within nursing homes is provided as a reference. T1 spans the period preceding the first presumptive case of COVID-19 in Massachusetts (October 1, 2018-February 28th, 2020). T2 spans the intervening weeks until the announcement of the NFASP (Feb 29th-April 27th). T3 spans the 9-week NFASP intervention (April 28th-July 8th). T4 spans the weeks following the NFASP until the announcement of the announcement of a renewed statewide intervention, “NFASP 2.0” within Massachusetts nursing homes (July 9th-Sept 10th, 2020).
Figure 2 displays the average occupancy per nursing home in the SI and BI groups. Statewide, nursing homes experienced a sharp decrease in occupancy beginning in February 2020, reaching a nadir in May 2020. SI facilities had lower occupancy throughout all observed time periods, with a minimum of 65% occupied beds during the intervention.
Figure 2. Trends in Nursing Home Occupancy within Nursing Facility Accountability and Support Package Subgroups.
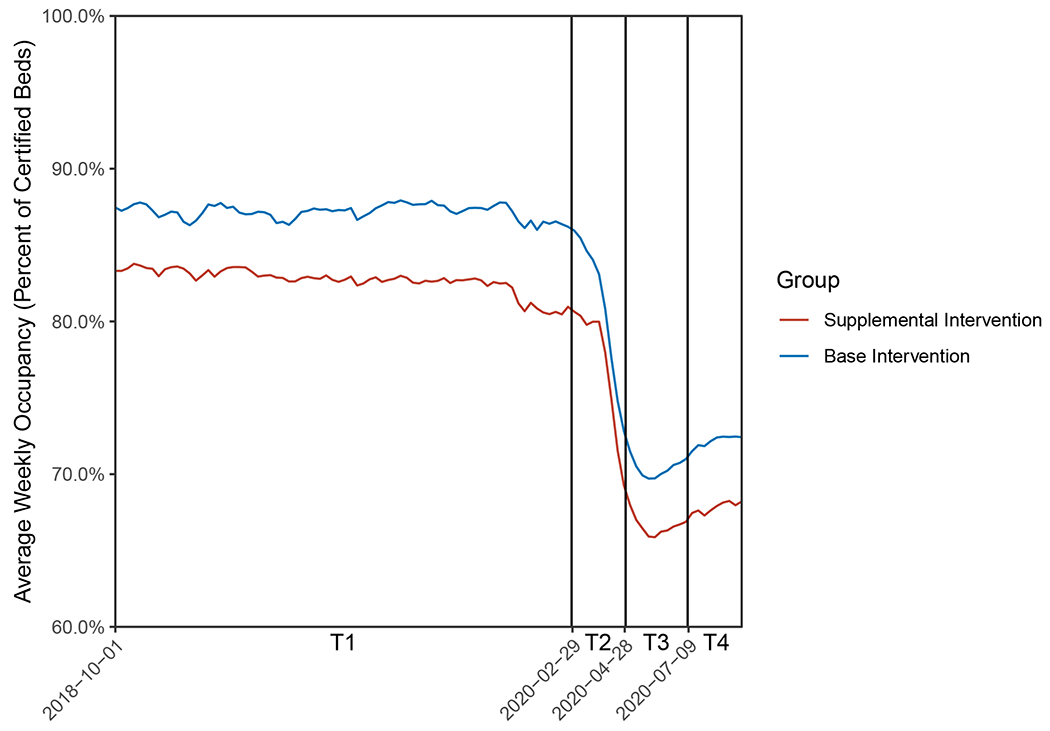
Notes: The exhibit displays the percentage of certified beds occupied within the Base Intervention (SI) and Supplemental Intervention (SI) groups of the Nursing Home Facility Accountability and Support Package (NFASP). T1 spans the period preceding the first presumptive case of COVID-19 in Massachusetts (October 1, 2018-February 28th, 2020). T2 spans the intervening weeks until the announcement of the NFASP (Feb 29th-April 27th). T3 spans the 9-week NFASP intervention (April 28th-July 8th). T4 spans the weeks following the NFASP until the announcement of the announcement of a renewed statewide intervention, “NFASP 2.0” within Massachusetts nursing homes (July 9th-Sept 10th, 2020).
DISCUSSION
The Massachusetts NFASP pioneered a novel response to COVID-19 within nursing homes and has served as a template for the scaling of similar strike team models, with federal support under ARPA.4,5 Using nursing home occupancy and mortality data, we illustrate challenges in interpreting the effects of the NFASP and its Supplemental Intervention. Trends in statewide nursing home occupancy and mortality suggest time-varying nursing home census composition, and potentially differential changes across the BI and SI groups. Together, these factors preclude a causal estimate of the effects of the overall and tiered interventions on all-cause mortality. As has been noted in a prior evaluation of the NFASP,3 statistical methods cannot overcome the lack of randomization without strong assumptions. Below, we describe opportunities to design future strike team iterations to facilitate program evaluation, which may enhance the impact of state and federal investment in scaling this model.
When Randomization is Difficult
It may have been difficult to randomize an intervention such as the NFASP due to both ethical and practical considerations in the early weeks of a public health emergency.16 An inability to randomize, however, would not preclude rigorous assessment if well-designed data collection infrastructure were folded into program design and supported at the state and federal levels. For example, a stepped-wedge cluster design could enable researchers to differentiate programmatic from selection effects.17 An alternative and complementary approach could include pairing strike team models with infrastructure to capture time-varying aspects of census composition. We suggest that future strike team interventions capture real-time mortality and resident characteristics that are meaningful predictors of mortality, such as age, comorbidities, and cognitive and functional status.18 This information could both enhance program evaluation (by enabling researchers to capture time-varying confounders) and inform risk-stratification. Although resources such as the Minimum Data Set measure such characteristics, standard quarterly assessments are too infrequent to detect changes in the context of a time-limited public health intervention.19 Measuring compositional changes in the nursing home census is especially important when early mortality has the potential to select for a younger and or healthier surviving nursing home population. Considering census composition at the outset of nonrandomized interventions, moreover, may enhance the effectiveness of resource allocation by capturing dimensions of resident susceptibility to hospitalization or mortality that are not reflected in facility process measures.20
Although more intensive data collection procedures should enhance the evaluation of strike team models, it would be impractical for nursing home staff to primarily assume these responsibilities. Indeed, nursing homes care for a complex and heterogeneous population, while navigating competing regulatory requirements and structural challenges that include high staff turnover.21,22 The COVID-19 pandemic exacerbated these preexisting challenges by superimposing acute shortages of staffing and personal protective equipment.23 Partnerships with qualified third-parties to support intensive data collection may enhance the evaluation of nursing home interventions, without detracting from the primary patient care responsibilities of staff. The Long-Term Care Data Cooperative, a collaboration linking electronic health record information to nursing home census and facility characteristics, provides one model for future data collection efforts.24
When Randomization is Feasible
The first iteration of the NFASP illustrates the challenges inherent in selecting a risk-stratification approach to allocate scarce resources. Stratification using infection control process measures produced NFASP subgroups with comparable structural characteristics but unexpectedly sorted facilities with a younger census and lower antecedent and subsequent mortality rates into the Supplemental Intervention. This suggests that the process measures used to classify nursing homes, including historical CMS Health Inspection performance were not effective risk-stratification instruments. This finding is consistent with research suggesting that traditional CMS process measures were not meaningful predictors of COVID-19 cases during the initial weeks of the pandemic.25
In the absence of a definitive standard for differentiating high-risk nursing homes, randomizing tiered support should position administrators and policymakers to garner actionable information. First, randomization would eliminate selection bias, though the treatment and control groups could be unbalanced with small sample sizes. Second, randomization would permit evaluating the relative impact of tiered intervention components when the potential for temporal confounding can be addressed. Third, randomization would reduce the need for the intensive data collection resources and infrastructure required to capture granular information regarding nursing home census composition at repeated intervals.
Limitations
Our analysis has several limitations. First, we were unable to account for deaths that occurred outside nursing homes, including deaths that followed transfer to a hospital or to hospice in a setting other than nursing homes. Therefore, the true number of deaths among nursing home residents is larger than captured within our analysis. We recommend that future analyses use longitudinal data sources that accommodate tracking individuals across care settings and over time. Second, we quantify trends, rather than the impact of the overall intervention because of the potential for temporal confounding that could not be addressed without an appropriate external control group or available information on time-varying census composition. The absence of available, real-time resident characteristics in a period with substantial changes in occupancy meant we were unable to quantify differences in risk-adjusted or excess mortality among comparable populations. Third, our analysis required that we impute daily census data for facilities with reporting gaps during the COVID-19 pandemic, in part, due to CMS’ relaxing reporting requirements to reduce the data collection burden.26,27 Census information for 25% of facility-days was missing during the first quarter of 2020; by comparison it was less than 5% in other quarters. Fourth, although we suggest that future interventions consider risk-stratifying facilities using census characteristics that are predictive of adverse resident outcomes, it remains unclear whether this approach would be subject to regression to the mean if sustained over time.28 Furthermore, the risk factors that most predispose to adverse outcomes with novel pathogens are uncertain and may, therefore, complicate preemptive risk stratification. Lastly, we were unable to discern whether nursing home residents’ site of death was concordant with their previously documented wishes, as potentially indicated by do-not-hospitalize orders or receipt of end-of-life care.29 Deaths within nursing homes, may present a goal-concordant outcome for residents and families wishing to minimize burdensome transfers near the end of life.30
CONCLUSION
We suggest that expanded data collection infrastructure and, ideally, randomized assignment to intervention subgroups will enhance the evaluation of strike team models, as these are scaled under the direction of state and federal agencies.
Supplementary Material
Supplementary Figure S1: Nursing Facility Accountability and Support Package Subgroup Assignments (please see Supplementary Materials file)
Key Points
This study illustrates obstacles to measuring the effect of a novel infection control initiative on all-cause mortality within Massachusetts nursing homes during the COVID-19 pandemic.
As federal funds are directed towards the scaling of infection-control mitigation efforts within nursing homes, improved support for data collection should enhance program implementation and evaluation.
Why does this matter?
The Massachusetts Nursing Facility Accountability and Support Package (NFASP) pioneered a state-led approach to COVID-19 mitigation within nursing homes. The NFASP and similar models have provided a framework for the broader state and federal dissemination of infection control interventions. We illustrate how potential temporal confounding and differential selection preclude estimation of program effects. We suggest adaptations that could better support future program evaluation as state and federal funds are deployed.
Disclosures:
Dr. Festa was supported by a training grant from the National Institute on Aging (T32AG019134) and the Clinical and Translational Science Awards Program (TL1TR001864) from the National Center for Advancing Translational Science (NCATS). Dr. Hsu, Dr. Grabowski, Dr. Newhouse, and Dr. Normand were supported by the National Institutes of Health grants P01AG032952 and U01AG076478. Dr. Hsu, Dr. Newhouse, and Dr. Normand were also supported by the National Institutes of Health grant R01AG062282.
Footnotes
Sponsor’s Role: The sponsor did not have a role in the design, methods, subject recruitment, data collections, analysis, or preparation of the paper.
Conflict of Interest Disclosures: The authors report no conflicts of interest.
Disclaimer: The contents of this manuscript are the sole responsibility of the authors and do not represent the views of the NIA or NCATS.
References
- 1.Chidambaram P. State Reporting of Cases and Deaths Due to COVID-19 in Long-Term Care Facilities.; 2020. Accessed April 20, 2022. https://www.kff.org/coronavirus-covid-19/issue-brief/state-reporting-of-cases-and-deaths-due-to-covid-19-in-long-term-care-facilities/
- 2.Karanovich B. Baker-Polito Administration Announces New Nursing Facility Accountability and Supports.; 2020. Accessed April 16, 2022. https://www.mass.gov/news/baker-polito-administration-announces-new-nursing-facility-accountability-and-supportsounces-new-nursing-facility-accountability-and-supports
- 3.Lipsitz LA, Lujan AM, Dufour A, et al. Stemming the Tide of COVID-19 Infections in Massachusetts Nursing Homes. J Am Geriatr Soc. Published online September 21, 2020:jgs.16832. doi: 10.1111/jgs.16832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Academies of Sciences E and M. The National Imperative to Improve Nursing Home Quality: Honoring Our Commitment to Residents, Families, and Staff. Natl Imp to Improv Nurs Home Qual Honor Our Commit to Resid Fam Staff. Published online April 6, 2022:1–578. doi: 10.17226/26526 [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Nursing Home & Long-Term Care Facility Strike Team and Infrastructure Project Guidance: Project E—Emerging Issues.; 2021. https://www.cdc.gov/ncezid/dpei/pdf/guidance-nursing-home-ltc-facility-strike-team-and-infastructure-508.pdf
- 6.Grimm CA. CMS’s COVID-19 Data Include Required Information From The Vast Majority of Nursing Homes, But CMS Could Take Actions to Improve Completeness and Accuracy of the Data.; 2021. Accessed June 3, 2022. https://oig.hhs.gov
- 7.Underwood L. H.R.8481 – 117th Congress (2021-2022): Improving DATA in Public Health Act. United States Congress.; 2022. Accessed October 8, 2022. http://www.congress.gov/ [Google Scholar]
- 8.Government Accountability Office. COVID-19: Federal Efforts Could Be Strengthened by Timely and Concerted Actions.; 2020. Accessed October 4, 2020. https://www.gao.gov/reports/GAO-20-701/
- 9.Finlaw S. Baker-Polito Administration Announces Further Support, Resources, and Accountability Measures for Nursing Facilities, Funding for Congregate Care Facilities During COVID-19.; 2020. Accessed April 16, 2022. https://www.mass.gov/news/baker-polito-administration-announces-further-support-resources-and-accountability-measures-for-nursing-facilities-funding-for-congregate-care-facilities-during-covid-19
- 10.Massachusetts Department of Public Health. COVID-19 Response Reporting | Mass.gov. Published 2021. https://www.mass.gov/info-details/covid-19-response-reporting
- 11.Centers for Medicare & Medicaid Services. Staffing Data Submission Payroll Based Journal (PBJ). Accessed June 1, 2022. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Staffing-Data-Submission-PBJ
- 12.Honaker J, King G, Blackwell M. Journal of Statistical Software Amelia II: A Program for Missing Data. 2011;45(7). Accessed August 15, 2022. http://www.jstatsoft.org/ [Google Scholar]
- 13.Centers for Medicare & Medicaid Services. Provider Information | Provider Data Catalog. Accessed December 27, 2021. https://data.cms.gov/provider-data/dataset/4pq5-n9py
- 14.Massachusetts Center for Health Information and Analytics. Information for Data Submitters: Nursing Facility Cost Reports. Accessed June 1, 2022. https://www.chiamass.gov/nursing-facility-cost-reports-2/
- 15.LTCFocus Public Use Data sponsored by the National Institute on Aging (P01 AG027296) through a cooperative agreement with the Brown University School of Public Health. doi: 10.26300/h9a2-2c26 [DOI]
- 16.Sugarman J, Califf RM. Ethics and Regulatory Complexities for Pragmatic Clinical Trials. JAMA. 2014;311(23):2381–2382. doi: 10.1001/JAMA.2014.4164 [DOI] [PubMed] [Google Scholar]
- 17.Ford I, Norrie J. Pragmatic Trials. N Engl J Med. 2016;375(5):454–463. doi: 10.1056/NEJMRA1510059/SUPPL_FILE/NEJMRA1510059_DISCLOSURES.PDF [DOI] [PubMed] [Google Scholar]
- 18.Panagiotou OA, Kosar CM, White EM, et al. Risk Factors Associated With All-Cause 30-Day Mortality in Nursing Home Residents With COVID-19. JAMA Intern Med. Published online January 4, 2021. doi: 10.1001/jamainternmed.2020.7968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Medicare & Medicaid Services. MDS 3.0 Frequency Report.; 2021. Accessed November 30, 2022. https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/Minimum-Data-Set-3-0-Public-Reports/Minimum-Data-Set-3-0-Frequency-Report
- 20.Islam N, Shkolnikov VM, Acosta RJ, et al. Excess deaths associated with covid-19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. BMJ. 2021;373. doi: 10.1136/BMJ.N1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ouslander JG, Grabowski DC. Rehabbed to Death Reframed: In Response to “Rehabbed to Death: Breaking the Cycle.” J Am Geriatr Soc. 2019;67(11):2225–2228. doi: 10.1111/jgs.16127 [DOI] [PubMed] [Google Scholar]
- 22.Geng F, Stevenson DG, Grabowski DC. Daily nursing home staffing levels highly variable, often below CMS expectations. Health Aff. 2019;38(7):1095–1100. doi: 10.1377/hlthaff.2018.05322 [DOI] [PubMed] [Google Scholar]
- 23.McGarry BE, Grabowski DC, Barnett ML. Severe Staffing And Personal Protective Equipment Shortages Faced By Nursing Homes During The COVID-19 Pandemic. Health Aff. Published online August 20, 2020:10.1377/hlthaff. doi: 10.1377/hlthaff.2020.01269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dore DD, Myles L, Recker A, et al. The Long-Term Care Data Cooperative: The Next Generation of Data Integration. J Am Med Dir Assoc. 2022;23(12):2031–2033. doi: 10.1016/J.JAMDA.2022.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Konetzka RT, White EM, Pralea A, Grabowski DC, Mor V. A systematic review of long-term care facility characteristics associated with COVID-19 outcomes. J Am Geriatr Soc. 2021;69(10):2766–2777. doi: 10.1111/JGS.17434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Medicare & Medicaid Services. Long Term Care Facilities: CMS Flexibilities to Fight COVID-19.; 2021. Accessed April 27, 2022. www.cms.gov/covidvax.
- 27.Centers for Medicare and Medicaid Services. Changes to Staffing Information and Quality Measures Posted on the Nursing Home Compare Website and Five Star Quality Rating System Due to the COVID19 Public Health Emergency.; 2020. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf,
- 28.Finkelstein A, Zhou A, Taubman S, Doyle J. Health Care Hotspotting — A Randomized, Controlled Trial. N Engl J Med. 2020;382(2):152–162. doi: 10.1056/NEJMSA1906848/SUPPL_FILE/NEJMSA1906848_DATA-SHARING.PDF [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ernecoff NC, Zimmerman S, Mitchell SL, et al. Concordance between Goals of Care and Treatment Decisions for Persons with Dementia. J Palliat Med. 2018;21(10):1442–1447. doi: 10.1089/jpm.2018.0103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Polniaszek Susan, Walsh Edith G., Wiener Joshua M.. Hospitalizations of Nursing Home Residents: Background and Options.; 2011. Accessed December 7, 2021. https://aspe.hhs.gov/reports/hospitalizations-nursing-home-residents-background-options-0
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure S1: Nursing Facility Accountability and Support Package Subgroup Assignments (please see Supplementary Materials file)


