Abstract
Objective
Chronic disease is the leading cause of morbidity and mortality on a global scale. Recent use of intelligent home environments for remote health monitoring has allowed patients to feel safe at home. By encouraging patient engagement and, if necessary, care delivery, smart home environments may be a useful method for managing chronic diseases at home. The purpose of this study is to synthesize the evidence on the usage of smart healthcare in the home for chronic illness management.
Methods
We conducted a scoping review using the Joanna Briggs Methodology and searched three databases from 2017 to 2022 for original research papers on smart healthcare, smart home technology, home-based technology, home monitoring, and physiological monitoring for chronic illness management. We did a descriptive study on the pertinent data we collected, as well as an analysis of whether the devices met its objectives.
Results
The final analysis included nine papers, the majority of which were randomized controlled trials. All of the studies were carried out in developed countries. The gadgets or smart healthcare in these studies are categorized based on the technology used and the outcomes measured. Respiratory, weight, and ballistocardiograph measurements, as well as changes in questionnaire ratings, hospitalization, activity monitoring, device acceptability, medication adherence, exercise capacity, and body function, were all measured.
Conclusion
Smart healthcare applications boost health by monitoring health and wellness, recording physical activity and rehabilitation, and improving overall quality of life. Not all smart home applications, however, served their intended purpose. As a result, more research into the efficacy of smart healthcare is needed to improve its application for chronic illness treatment.
Keywords: Chronic conditions, home monitoring, smart healthcare, smart home technology, chronic disease, physical monitoring
Introduction
Globally, chronic disease is the primary cause of morbidity and mortality. 1 The World Health Organization (WHO) estimates that 41 million people die each year, accounting for 71% of all mortality globally. 2 Chronic illness risk factors affect people of all ages. According to research, more than 15 million chronic disease-related mortality occur between the ages of 30 and 69. 2 Additional data indicate that approximately 25% of adults have one or more chronic health issues, putting a significant strain on individuals, families, and the healthcare system. 1 Chronic diseases are described broadly as issues which persist a year or longer and necessitate continuing medical attention, impede daily activities, or both. Heart disease, cancer, lung disease, stroke, Alzheimer's disease, diabetes, and chronic kidney disease are examples of chronic diseases, with heart disease, cancer, and diabetes being the primary causes of death and disability in industrialized countries. 3 Chronic disease-related costs are currently increasing at an alarming rate 4 motivating the advancement of home healthcare. Addressing chronic disease is a major challenge for global healthcare systems. 5
Smart home environments have recently been employed to provide remote health monitoring, allowing patients to feel safe at home.6,7 A smart home is a home with a networked sensor and device network that provides intelligence, automation, control, contextual awareness, adaptability, and functionality to improve occupant health and healthcare delivery both remotely and locally. 8 The combination of healthcare and smart homes has given rise to a new term: “smart home healthcare.” Smart home healthcare aims to help users by providing information about their health status and condition. 9 It was first proposed in 1984, and it refers to homes with interactive smart technology including smart home, robotic assistants, also telemonitoring and tele support. Robotic assistants typically do the most fundamental tasks that contribute to increased patient independence. 8 For example, duties such as forgetting to eat, taking medication, or using the restroom are real issues that can be resolved. Monitoring vital signs, monitoring activities of daily living (ADL), monitoring emergency aid, and social contact are the four key areas of concern in telemonitoring.
Smart home healthcare is widely regarded as a cost-effective and technologically advanced solution for enhancing healthcare. 7 The utilization of smart home healthcare involves the regular monitoring of patients’ conditions using various devices such as sensors, cameras, and microphones. 7 These devices are continuously capturing valuable data regarding patients’ health status, interactions, and daily activities within their homes. This information can be leveraged by healthcare professionals through multimodal inputs, including speech and video capture, to provide patients with guidance and support through voice commands, video consultations, or service instructions. 10
Smart home environments offer an effective approach to managing chronic diseases by promoting patient engagement and, when necessary, facilitating care delivery. 11 Many instances of ineffective chronic disease management can be attributed to outdated care delivery models. 12 Recent advancements in home-based wireless devices, applications, and wearables have created opportunities for healthcare systems to closely monitor health indicators and physiological data in almost real time. For instance, wearable devices equipped with finger sensors can monitor cardiovascular and respiratory systems to manage chronic diseases. 13 Additionally, there are smart home healthcare devices that offer a diabetes monitoring system, providing automatic feedback messages and recording crucial data such as blood glucose levels, dietary habits, blood pressure, and physical activity. 14 Leveraging a WeChat account equipped with multiple functional modules can also serve as a proactive prevention platform, offering users a robust tool capable of ensuring an efficient self-monitoring process for managing chronic obesity.15,16
Smart home healthcare technologies offer a foundation for increased patient engagement and introduce a novel care delivery model built upon integrated practice units. These innovations are essential for addressing the evolving healthcare landscape by shifting the focus from a hospital-centric to a patient-centered approach, with the potential to enhance the management of chronic illnesses. 1 Recognizing the need to consolidate and synthesize smart healthcare research and evidence, there arises an opportunity to elevate functionality and broaden the acceptance of smart healthcare, which holds great promise in improving the management of chronic diseases. 17 Consequently, this study embarks on a comprehensive scoping review, aiming to explore the practical applications of smart healthcare within the home setting for individuals managing chronic diseases.
Methods
We used the Joanna Briggs Institute's (JBI) 18 scoping review framework to evaluate, explain, and synthesize the available data on the implementation of smart healthcare in the home for chronic disease patients. The review was then reported on in accordance with the PRISMA-P principles. 19
Search strategy
The research question was: what smart healthcare or smart home application could be used to offer physiological monitoring on patients with chronic disease? This study utilized the phrases “chronic disease” AND “smart healthcare” OR “smart home technology” OR “home-based technology” OR “home monitoring” AND “physiological monitoring.” The Boolean operators “OR” and “AND” were used to connect keywords. PubMed, CINAHL, and ScienceDirect were among the databases used. The study was carried out in December 2022. Original studies written in English, papers published between 2017 and 2022, and research that investigates the deployment of smart healthcare in the home environment, with an emphasis on physiological monitoring (outcomes measured and results), were the inclusion criteria. Table 1 shows the literature search strategy.
Table 1.
Literature search strategy.
| Search | Field | ||
|---|---|---|---|
| Population | Concept | Context | |
| #1 AND #2 AND #3 | Chronic disease | Smart healthcare | Physiological monitoring |
| Smart home technology | |||
| Home-based technology | |||
| Home monitoring | |||
Eligibility criteria and data selection
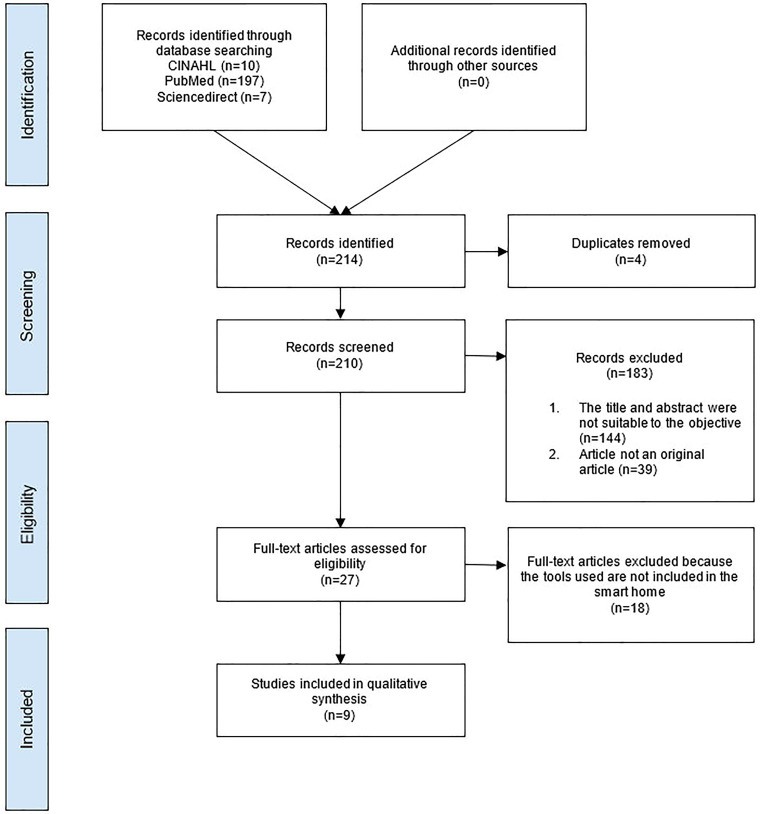
A total of 214 titles were discovered by examining databases. Mendeley was used to filter and choose titles and abstracts. After removing duplicates, 210 titles and abstracts were reviewed for eligibility. One reviewer (IMN) looked at the title and abstract to see if they were relevant to smart home healthcare and chronic disease. ID examined the extraction at random to check its accuracy and applicability. Any disagreements were resolved by discussion. For the full texts, ID and IMN reviewed all 27 publications independently, analyzing each one and discussing any disagreements. Finally, this analysis contained nine papers. The included article must explain the implementation of a smart home device used for physical monitoring of chronically ill patients with measured outcomes. Eighteen papers were discarded because they were not conducted at home or did not measure any result. As a consequence, nine articles were selected for the final scoping review. Figure 1 PRISMA flow diagram depicts the stages and includes articles in each stage (see supplemental file for details).
Figure 1.
PRISM flow diagram.
Data extraction and analysis
Data extraction was carried out in accordance with the JBI methodology, and the search strategy was determined using the wide population, concept, and context (PCC) framework recommended by the JBI for Scoping Reviews (as shown in Table 1). The following information was retrieved: author, year of publication, research aims, country and location, study participants, study design, technology used, outcomes measured, and results. We determined the device's effectiveness by determining if each smart home application's function could achieve the desired objective. We conducted a descriptive analysis on the relevant data that we collected. Because this review did not contain any personally identifiable medical information about a living person, the patient's specific consent is not required.
Results
Upon conducting the search using the provided search terms, multiple results were generated. All of the research conducted in this study was limited to developed countries, such as the United States,20–23 France, 24 the Netherlands, 25 China,23,26 Spain,27,28 the United Kingdom, Slovenia, Estonia, and Sweden. 27 No studies conducted in developing countries were identified. According to the year of publication, the majority of articles (33.33%, n = 3) were published in 2018.26–28 The study design of the majority of the studies22,24,26,27 was randomized clinical trials: two studies were longitudinal studies,20,23 one pilot study, 21 one prospective observational study, 25 and one quasi-experimental study. 28 The primary context and objectives of the investigations were identical. The goal of the study is to define, investigate, validate, and evaluate smart health care in the management of chronic disease in patients at home.20–28 The majority of the research were conducted in patients’ homes, with the exception of four studies that were conducted in a combination of medical facility and patient home settings.22,23,26,28
Among the diseases addressed were heart failure, chronic obstructive pulmonary disease (COPD), central congenital hypoventilation syndrome, asthma, chronic cerebrovascular sickness, and hypertension.20–28 The outcomes measured also varied, such as respiratory measurement; weight measurement; ballistocardiograph measurement; change in questionnaire scores; hospitalization; activity tracking; device acceptance; medication adherence; exercise capacity; body function measurement such as respiratory rate, heart rate, lung function, and chronic disease treatment; or control such as sleep apnea diagnosis, obstructive sleep apnea diagnosis, and hypertension control.20–28
Devices or smart healthcare used in these studies had different function, such as alarms, displays, data storage, data transmission, and data recording. Alarm devices include vibrating wristbands (“Feeltact®”, Novitact Lacroix-Saint-Ouen, France), phone applications to trigger vibrating alarms, 24 ECG monitors, 26 and Resmon Pro Diary using forced oscillation technique (FOT) measurement. 27 Display system devices include a remote care management system 21 and cardiologists and monitoring reports. 26 Data storage devices include cellphones from Elephant Medical's heart healthcare cloud service platform. 26 Bed scales, 20 ECG monitors, internet of things (IoT) technology, 26 and a mobile modem 27 were examples of data transmission equipment. Bed scales, 20 activity or smart sensors,21,25,28 the handheld Spirobank, wireless activity tracker, Cohero health smart inhalers, the Emotion Faros 180°, 21 and portable polysomnography22,23 and also spirometer 25 were all examples of data recording devices. However, most of the devices have more than one function. The majority of studies uses automatic sensors for vital sign measurements.20,21,23,25,26,28
Discussion
This research focused on the use of smart healthcare for chronic disease management including heart failure, COPD, central congenital hypoventilation syndrome, asthma, chronic cerebrovascular illness, and hypertension (Table 2). Two major findings emerged from this review. First, the application has a broad scope and has the ability to improve the quality of life of chronic patients. Smart healthcare uses different types of technology (Table 3) for example the IoT, big data, cloud computing, and artificial intelligence to fundamentally revolutionize the old medical system, making healthcare more efficient, convenient, and personalized. 29 Smart healthcare has a great impact on well-being, especially in the management of chronic diseases by facilitating the control of worsening condition and boosting patient safety through disease management assistance. 30 It also gave a positive effect on the management of diabetes, hypertension, and rheumatoid arthritis. 31 These intelligent technologies can aid in the active monitoring of patients’ adherence and are capable of reducing various possible errors. 32
Table 2.
Aim, study setting, study design, and participants involved.
| No | Author (year) | Aim | Study setting | Study design | Participants |
|---|---|---|---|---|---|
| 1 | Harrington et al. (2021) 20 | To validate the technology by comparing Bed scales to ground truth data and demonstrating the feasibility of detecting respiratory pathologies and the real-world durability of the platform | United States; patient's home | Longitudinal study (3 months of in-home monitoring) | Eight patients with heart failure |
| 2 | Tillis et al. (2017) 21 | To assess the feasibility and acceptability of implanting multiple home device sensors in patients with GOLD stage 3 or 4 COPD | United States; patient's home | Pilot study | 24 patients with stage 3 or 4 COPD (age mean = 72) |
| 3 | Bravata et al. (2017) 22 | To determine whether the intervention strategy improved sleep apnea detection, obstructive sleep apnea (OSA) treatment, and hypertension control among patients with chronic cerebrovascular disease and hypertension | United States; medical centers and patient's homes | Randomized controlled strategy trial | 225 patients (intervention group, n = 110; control group, n = 115) |
| 4 | Chang et al. (2019) 23 | To evaluate home sleep apnea testing using a type 3 PM (Nox-T3, Nox Medical Inc., Reykjavik, Iceland) to diagnose OSA in adults with COPD | China and United States; in the laboratory and at the patient's home | Longitudinal study (1 week) with three monitoring methods (HSAT, in-laboratory PM, and in-laboratory PSG); | 90 adult patients with COPD |
| 5 | Attali et al. (2020) 24 | To test the capacity of vibrotactile stimulation transmitted to the wrist bones by a vibrating wristband to awaken healthy individuals and patients requiring home mechanical ventilation during sleep | French; patient's home | clinical trial | 37 patients (healthy subject group, n = 20; CH group, n = 8; COPD group, n = 9) |
| 6 | Kamp et al. (2020) 25 | To investigate whether asthma control can be accurately assessed in the home situation by combining parameters from respiratory physiology sensors | Netherlands; patient's home | Prospective observational study | Sixty children with pediatrician-diagnosed asthma and 30 healthy children between 4 and 14 years old |
| 7 | Li et al. (2018) 26 | To investigate whether home-based cardiac exercise rehabilitation (ER) using (remote ECG monitoring system, REMS) is superior to conventional ER without monitoring in patients with CHF | China; outpatient clinic and patient's home | Prospective, randomized, parallel controlled clinical trial | Patients with a systolic cardiac dysfunction 120 patients between 18–75 years old (conventional group, n = 60; remote monitoring rehabilitation group, n = 60) |
| 8 | Walker et al. (2018) 27 | To evaluate the efficacy of home monitoring of lung mechanics by the forced oscillation technique (FOT) and cardiac parameters in older patients with chronic obstructive pulmonary disease (COPD) and comorbidities | Spain, United Kingdom, Slovenia, Estonia, and Sweden; patient's home | A multicenter, randomized, clinical trial | 312 patients with chronic obstructive pulmonary disease (COPD) aged 60 years old or older (control group, n = 158; intervention group, n = 154) |
| 9 | Naranjo-Hernandez et al. (2018) 28 | To describe the design and implementation of a smart vest for an untethered, low-cost, and comfortable breathing monitoring | Spain; hospital-controlled clinical environment and patient's home | Quasi-experimental studies | 11 subjects (healthy subjects group, n = 2; COPD patients group, n = 9) |
Table 3.
Technology used, outcome measured, and study findings.
| No | Author (year) | Technology used | Outcomes measured | Findings | Study limitation |
|---|---|---|---|---|---|
| 1 | Harrington et al. (2021) 20 | Sensors automatically and continuously collect vital signs for monitoring via non-contact adherence (passive) |
|
|
|
| 2 | Tillis et al. (2017) 21 | Sensors, daily activity measurement via passive motion-sensing technology, and a remote care management system for vital sign symptoms |
|
|
|
| 3 | Bravata et al. (2017) 22 | Automatic devices (passive interaction) for vital sign monitoring |
|
|
|
| 4 | Chang et al. (2019) 23 | Sensors, active and simultaneous, for vital sign measuring |
|
|
|
| 5 | Attali et al. (2020) 24 | Devices with passive interactions for vital sign measurement |
|
|
|
| 6 | Kamp et al. (2020) 25 | Wearable devices with sensors for vital sign measurements |
|
|
|
| 7 | Li et al. (2018) 26 | Sensors and internet of things technology for vital sign measurements |
|
|
|
| 8 | Walker et al. (2018) 27 | Devices and systems for daily live activity and vital sign measurements |
|
Despite the acceptability of the monitoring system to patients, with a high adherence rate, its use did not affect overall TTFH, admission rate, or patient's quality of life assessed by EQ-5D |
|
| 9 | Naranjo-Hernandez et al. (2018) 28 | Automatic sensors for vital sign measurements |
|
|
Not available |
Abbreviations: HF, heart failure; BCG, ballistocardiograph; FOT, forced oscillation technique; TTFH, time to first hospitalization; CAT, COPD assessment tool; PHQ-9, patient health questionnaire; MLHFQ, Minnesota living with heart failure; CHF, congestive heart failure; IHD, ischemic heart disease; QALY, quality-adjusted life years; EQ-5D, EuroQoL 5D; COPD, chronic obstructive pulmonary disease; CH, central hypoventilation; PSG, polysomnography; REMS, remote ECG monitoring system; EEG, electroencephalographic; HERE, home-based exercise rehabilitation with electrocardiogram; 6MWT, 6-min walk test; MQTT, message queue telemetry transport; OSA, obstructive sleep apnea; CPAP, continuous positive airway pressure; ESS, Epworth sleepiness scale; NIHSS, the national institutes of health stroke scale; HSAT, home sleep apnea testing; PM, portable monitor.
The use of smart healthcare in the home from the studies found was mostly for patient with chronic cerebrovascular disease and hypertension (COPD) disease. The technology that used was based on automatic sensor both active and passive motion of patients daily live activity.21,23,27 The vital sign of patients with COPD was also measured using the automatic sensors and a remote care management system.24,28 Another study revealed that the vibrating wristband gadget used to awaken central hypoventilation patients and COPD patients was much less effective than healthy people. 24 Furthermore, researchers discovered that employing a platform that includes a device that monitored within-breath respiratory mechanical impedance had no influence on overall time to first hospitalization, admission rate, or patient quality of life. 27 CHROMED also provides COPD telemonitoring solutions. 27 A device that employed the FOT to measure within-breath respiratory mechanical impedance, a touch-screen computer, and a mobile modem was all part of the platform. 27 Wireless spirometry can also be used to monitor lung health. 25
A smart phone-based handheld wireless spirometer is simple to use and suited for medical diagnostic testing for asthma and COPD at home. 33 Asthma is also the most common chronic respiratory disease in the world after COPD; hence enhancing respiratory assessment is crucial. 22 According to a study conducted in the Netherlands, respiratory physiology sensors such as the Spirobank II Advanced are utilized for respiratory assessment and asthma control. 25 Wearable devices with sensors technology for vital sign was also evidence the use of smart healthcare in patient with asthma chronic disease. 25 Health remote monitoring systems are another way for smart healthcare to monitor important signs that collects patient data via sensors and wearable devices. 34 The activity sensor, which comprises of a communications hub and many sensors installed on household objects, detects patterns of daily activities using passive motion-sensing technology. 21 The employment of a collection of wireless wearable medical equipment and sensors allows for the periodic assessment of a patient's biometric parameters as well as the automatic recognition of the patient's daily physical activity, assuring an effective telemonitoring service for the patient independent of his or her location. 35
Smart healthcare applications for patients with sleep apnea chronic disease provide health monitoring such as bed scales, remote care management systems, portable polysomnography, portable monitor sensors, the handheld Spirobank II Advanced, the two Cohero health smart inhalers, the Emotion Faros 180°, a wearable ECG monitor, and a platform that comprises a device that measures within-breath respiratory and a smart sensor device integrated with a smart vest.20–23,25–28 Bed scales assess not only weight but also breathing rate. 25 Body weight measurements obtained with bed scales may aid in determining fluid status in patients suffering from acute renal damage, which is typically accomplished by monitoring fluid balance. 26 As a patient sleeps in bed, episodic musculoskeletal movements are separated by relatively long movement-free intervals during which low variance physiological signals like respirations can be captured using Bed scales. 20
At home, mechanical ventilation can be used to treat persistent respiratory failure. 33 Because of their critical illness, care for a person receiving home mechanical ventilation is extremely complex, requiring technological assistance and skilled nursing services to provide personal care, a variety of daily medical and therapeutic procedures, and educational and psychosocial support for the patient and their family. 36 The research, carried out at the Pitie-Salpetriere respiratory rehabilitation clinic in Paris, discovered that vibrating wristbands provide a good backup to a home mechanical ventilator audio alert for healthy family caregivers. 24 Other than that, a study also carried out the applications of smart healthcare technology use automatically and continuously sensors to collect vital signs for monitoring via non-contact adherence (passive). 20
Smart healthcare applications of patients with cardiac dysfunction were used wearable ECG monitors that can evaluate whether patients reach the intensity based on the heart rate and promptly alert the patients to ensure that exercise intensity is within the preset range. 26 Remote ECG monitoring system (REMS) is used to detect risky arrhythmia and provide an early warning to both the patients and their doctors, which can encourage patients to overcome fear and adhere to exercise. 26 Cardiopulmonary exercise testing (CPET) also can be used to evaluate patient exercise capacity and exertional symptoms and can provide numerous physiological parameters. 26
In addition, smart healthcare for ballistocardiograph (BCG) measurement is a non-invasive method for producing a graphical depiction of the heartbeat-induced repeated motions of the human body. 23 Heartbeat monitoring is especially important today because cardiovascular disease is the leading cause of death worldwide. 37 Bandpass filtering bed scale signals (5 Hz and 50 Hz cut-offs) revealed individual scale BCG morphologies, and the raw BCG signal from each scale was converted into an absolute measure of BCG energy to create a single-peak BCG morphology. 20 Another study discovered that employing miniature springs to transfer matter vibrations to an optical detecting module was an effective method for tracing BCG curves. 38 Monitoring vital signs, which can help assess the health of the human body, is important in many healthcare applications. 39
Some technologies may be used to monitor physical activity as well as for rehabilitation.25,26 Physical activity can also be measured with the ActiGraph wGT3X-BT wireless activity tracker. 25 ActiGraph LLC is a well-known manufacturer of high-performance accelerometers like the wGT3X-BT (with extra battery capacity and wireless Bluetooth features). 40 The ActiGraph wGT3X-BT can store data for up to 43 days and sync wirelessly with the ActiLife mobile application to maximize battery life, and the wireless capability will be disabled. 41 However, we discovered that not all smart home applications served their intended purpose. The use of portable polysomnography revealed that it was less successful in detecting sleep apnea than unattended polysomnography in control patients. 22 Furthermore, in a cohort with well-controlled baseline blood pressure, the intervention using home-based polysomnography did not enhance hypertension control. 22
The studies included in this review also have some limitations due to the small sample size, focused only on certain population, short-term follow-up, and the variation on the pattern of healthcare that may not be generalizable.21,23,26,27 In addition, result bias may found in the smart healthcare system technology measurements according to the non-patient individuals triggering the motion sensor making it impossible to differentiate activity patterns between individuals.20,21 Some of the results were also measured in more than two people that may be slightly different because there was no independent study endpoint committee to review.24,25 Those limitations were worth accepting and provide opportunities for further in-depth research.
However this review also had some limitations. The findings may not have captured all of the evidence in the literature due to the constraints of the keywords, database, and publication year. As a result, we obtained just a restricted number of publications. The research stated above was mostly undertaken in developed nations and may not be applicable in other countries. Nonetheless, this study has the potential to contribute to the mapping of information on smart home healthcare for individuals with chronic diseases.
Conclusion
There are numerous possibilities for smart healthcare in the home for chronic disease management. Smart healthcare applications improve health by monitoring health and well-being, tracking physical activity and rehabilitation, and improving overall quality of life. According to the findings of the study, each study has limitations, and not all smart home applications succeed in meeting their intended purpose. As a result, more research into smart healthcare's efficacy is required to improve its application for chronic disease management.
Supplemental Material
Supplemental material, sj-jpg-1-dhj-10.1177_20552076231218144 for Smart home healthcare for chronic disease management: A scoping review by Inge Dhamanti, Ika M. Nia, Krishnaraj Nagappan and Balaji P. Srikaanth in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076231218144 for Smart home healthcare for chronic disease management: A scoping review by Inge Dhamanti, Ika M. Nia, Krishnaraj Nagappan and Balaji P. Srikaanth in DIGITAL HEALTH
Acknowledgments
The authors would like to express their gratitude and appreciation to all parties involved in this study.
Footnotes
Contributorship: ID developed the study and was in charge of data collection and analysis. IMN collected and analyzed the data. KN and BPS evaluated the data and revised the manuscript critically. The final version to be published has been approved by all authors.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The ethical approval is not applicable to this study because this research does not contain any studies with human or animal subjects.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Universitas Airlangga (grant number 1266/UN3.15/PT/2022).
Guarantor: ID.
ORCID iD: Inge Dhamanti: https://orcid.org/0000-0003-2347-8771
Supplemental material: Supplemental material for this article is available online.
References
- 1.Xie Y, Lu L, Gao F, et al. Integration of artificial intelligence, Blockchain, and wearable technology for chronic disease management: a new paradigm in smart healthcare. Curr Med Sci 2021; 41: 1123–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Noncommunicable diseases [Internet]. 2021. [cited 2023 Feb 15]. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- 3.Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP) [Internet]. 2022 [cited 2023 Jul 19]. Available from: https://www.cdc.gov/chronicdisease/about/index.htm
- 4.Pulkkinen T, Son YS, Lee J, et al. Progressive monitoring and treatment planning of diabetes mellitus in smart home environment. In: International Conference on Consumer Electronics (ICCE), 2013, pp. 206–207. [Google Scholar]
- 5.Reynolds R, Dennis S, Hasan I, et al. A systematic review of chronic disease management interventions in primary care. BMC Fam Pract 2018; 19: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pham M, Mengistu Y, Do Het al. et al. Delivering home healthcare through a cloud-based smart home environment (CoSHE). Future Gener Comput Syst 2018; 81: 129–140. [Google Scholar]
- 7.Mageroski A, Alsadon A, Withana Cet al. et al. Impact of wireless communications technologies on elder people healthcare: smart home in Australia. Eng J 2017; 21: 263–273. [Google Scholar]
- 8.Bennett J, Rokas O, Chen L. Healthcare in the Smart Home: A study of past, present and future. Sustainability 2017; 9: 840. [Google Scholar]
- 9.Khan MF, Ghazal TM, Said RA, et al. An iomt-enabled smart healthcare model to monitor elderly people using machine learning technique. Comput Intell Neurosci 2021: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hossain MS. Patient status monitoring for smart home healthcare. IEEE international conference on multimedia & expo workshops. 2016;1–6. [Google Scholar]
- 11.Facchinetti G, Petrucci G, Albanesi B, et al. Can smart home technologies help older adults manage their chronic condition? A Systematic Literature Review. Int. J. Environ. Res. Public Health. 2023; 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Milani RV, Bober RM, Lavie CJ. The role of technology in chronic disease care. Prog Cardiovasc Dis 2016; 58: 579–583. [DOI] [PubMed] [Google Scholar]
- 13.Castaneda D, Esparza A, Ghamari M, et al. A review on wearable photoplethysmography sensors and their potential future applications in health care. Int J Biosens Bioelectron 2018; 4: 195-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rghioui A, Lloret J, Harane M, et al. A smart glucose monitoring system for diabetic patient. Electronics 2020; 9: 678 [Google Scholar]
- 15.Jiang Y, Liu F, Guo J, et al. Evaluating an intervention program using WeChat for patients with chronic obstructive pulmonary disease: Randomized controlled trial. J Med Internet Res 2020; 22: e17089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Álvarez R, Torres J, Artola G, et al. Obinter: A holistic approach to catalyse the self-management of chronic obesity. Sensors 2020; 20: 1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim BYB, Lee J. Smart devices for older adults managing chronic disease: A scoping review. JMIR Mhealth Uhealth 2017; 5: e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth 2021; 18 : 3–10. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 20: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harrington N, Bui QM, Wei Z, et al. Passive longitudinal weight and cardiopulmonary monitoring in the home bed. Sci Rep 2021; 11: 24376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tillis W, Bond WF, Svendsen Jet al. et al. Implementation of activity sensor equipment in the homes of chronic obstructive pulmonary disease patients. Telemed e-health 2017; 23: 920–929. [DOI] [PubMed] [Google Scholar]
- 22.Bravata DM, McClain V, Austin C, et al. Diagnosing and managing sleep apnea in patients with chronic cerebrovascular disease: A randomized trial of a home-based strategy. Sleep Breath 2017; 21: 713–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chang Y, Xu L, Han F, et al. Validation of the NOX-T3 portable monitor for diagnosis of obstructive sleep apnea in patients with chronic obstructive pulmonary disease. J Clin Sleep Med 2019; 15: 587–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Attali V, Lavault S, Guerder A, et al. Awakening efficacy of a vibrotactile device in patients on home nocturnal ventilatory assistance and healthy subjects as family caregiver proxies. Chron Respir Dis 2020; 17: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Der Kamp MR, Klaver EC, Thio BJ, et al. WEARCON: Wearable home monitoring in children with asthma reveals a strong association with hospital based assessment of asthma control. BMC Med Inform Decis Mak 2020; 20: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li J, Yang P, Fu D, et al. Effects of home-based cardiac exercise rehabilitation with remote electrocardiogram monitoring in patients with chronic heart failure: A study protocol for a randomised controlled trial. BMJ Open 2018; 9: e023923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walker PP, Pompilio PP, Zanaboni P, et al. Telemonitoring in chronic obstructive pulmonary disease (chromed) a randomized clinical trial. Am J Respir Crit Care Med 2018; 198: 620–628. [DOI] [PubMed] [Google Scholar]
- 28.Naranjo-Hernández D, Talaminos-Barroso A, Reina-Tosina J, et al. Smart vest for respiratory rate monitoring of copd patients based on non-contact capacitive sensing. Sensors 2018; 18: 2144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tian S, Yang W, Le Grange JM, et al. Smart healthcare: making medical care more intelligent. J Glob Health 2019; 3: 62–65. [Google Scholar]
- 30.Facchinetti G, Petrucci G, Albanesi B, et al. Can smart home technologies help older adults manage their chronic condition? A systematic literature review. Int J Environ Res Public Health 2023: 1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ma Y, Zhao C, Zhao Y, et al. Telemedicine application in patients with chronic disease: A systematic review and meta-analysis. BMC Med Inform Decis Mak 2022; 22: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pal P, Sambhakar S, Dave V, et al. A review on emerging smart technological innovations in healthcare sector for increasing patient’s medication adherence. Global Health Journal 2021; 5: 183–189. [Google Scholar]
- 33.Mucchi L, Jayousi S, Gant A, et al. Tele-monitoring system for chronic diseases management: requirements and architecture. Int J Environ Res Public Health 2021; 18: 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen S, Tan F, Lyu Wet al. et al. Ballistocardiography monitoring system based on optical fiber interferometer aided with heartbeat segmentation algorithm. Biomed Opt Express 2020; 11: 5458–5469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schaepe C, Ewers M. I see myself as part of the team” - family caregivers’ contribution to safety in advanced home care. BMC Nurs 2018; 17: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tucker S, Bramante C, Conroy M, et al. The most undertreated chronic disease: Addressing obesity in primary care settings. Current obesity reports 2021; 10: 396–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sadek I, Biswas J, Abdulrazak B. Ballistocardiogram signal processing: A review. Health Information Science and Systems 2019; 7: 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Windisch W, Geiseler J, Simon K, et al. German National guideline for treating chronic respiratory failure with invasive and non-invasive ventilation: revised edition 2017 - part 1. Respiration 2018; 96: 66–97. [DOI] [PubMed] [Google Scholar]
- 39.Poureslami I, Shum J, Kopec J, et al. Development and pretesting of a new functional-based health literacy measurement tool for chronic obstructive pulmonary disease (COPD) and asthma management. International Journal of COPD 2020; 15: 613–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mc Namara K, Alzubaidi H, Jackson JK. Cardiovascular disease as a leading cause of death: how are pharmacists getting involved? Integr Pharm Res Pract 2019; 8: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.López-Ruiz N, Escobedo P, Ruiz-García I, et al. Digital optical ballistocardiographic system for activity, heart rate, and breath rate determination during sleep. Sensors 2022; 22; 4112. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-jpg-1-dhj-10.1177_20552076231218144 for Smart home healthcare for chronic disease management: A scoping review by Inge Dhamanti, Ika M. Nia, Krishnaraj Nagappan and Balaji P. Srikaanth in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076231218144 for Smart home healthcare for chronic disease management: A scoping review by Inge Dhamanti, Ika M. Nia, Krishnaraj Nagappan and Balaji P. Srikaanth in DIGITAL HEALTH